Abstract
Background: The World Health Organization (WHO) estimates that 180,000 patients die from burns every year, which is considered a serious public health issue. Patients with burns require immediate pre-hospital care and transport to specialized treatment facilities. The aim of this study was to outline the profile of the burn patient from the perspective of the Polish Medical Air Rescue (PMAR), as well as to analyze the medical procedures being implemented. Methods: The study includes 2154 interventions by air emergency medical teams (AEMS) which provided aid for burn patients. The analysis covered the period from 2018 to 2022, including nationwide data made available from the IT systems of the PMAR. Statistical design was used, allowing for correlations of variables, at a significance level of p < 0.05. Results: Patients’ ages ranged from 1 month to 96 years (mean 35.05; SD ± 26.88). Adult patients (n = 1409; 65.41%) constituted the vast majority. The number of interventions to children below 1-year-old was noticeable (n = 394; 18.29%). Men were the most likely to suffer burns, up to three times more often than women (n = 1574, 73.07% vs. n = 570, 26.46%. T29—burns to multiple body areas (n = 890)—and T21—burns to the trunk (n = 255)—were most frequently reported as diagnoses according to the ICD-10 classification. A statistically significant association was found between age group and ICD-10 diagnosis (p < 0.001). The vast majority of patients were transported from the scene directly to Burn Treatment Centers (n = 1373; 63.74%). Treatment of pain by helicopter emergency medical services (HEMS) crews appeared to be effective (p < 0.001), and other interventions consisted of administering medications—ketamine (23.72%), rocuronium bromide (15.78%), propofol (14.02%)—and procedures such as sedation (30.87%), as well as intubation (13.42%) and mechanical ventilation (13.23%). Conclusions: The burn patient profile indicates men with a mean age of 35 years. Nevertheless, HEMS crews often carry out missions to infants and newborns. The most common diagnosis was extensive body burns. In 63.74% of the missions, patients were transported to the Burn Treatment Center. The HEMS crews implement effective pharmacological analgesia, and handle rescue medications and procedures to stabilize the patient’s condition.
1. Introduction
Tissue injuries caused by factors such as temperature, chemicals, radiation, friction, and electricity cause burns [1]. The World Health Organization (WHO) estimates that 180,000 patients die from burns every year, which remains a major public health burden [2]. This phenomenon mainly affects low- and middle-income countries, but globally, non-fatal burns are a common cause of morbidity, long-term hospitalization, body disfigurement, and disability. However, the aesthetic-related aspects cause stigma and psychological problems in burn patients. In developed countries, there has been a tendency toward treating patients in specialized medical center settings, allowing for shorter hospital stay as well as improved outcomes [3].
Classifying burns based on their extent and depth is a key part of diagnostics and treatment planning. The commonly used Abbreviated Burn Severity Index (ABSI) procedure is a five-variable scale to help assess burn severity. The variables considered are sex, age, presence of inhalation injury, presence of a full-thickness burn, and percentage of total body surface area burned. Third-degree burns (depth—deep dermal; color—blotchy red) and, sometimes distinguished, fourth-degree burns (depth—full thickness; color—white) are the most serious injuries, involving destruction of the dermis along with deep tissue. This is the condition wherein necrotic and sometimes charred areas are formed. Hospitalization is essential in this case, and treatment often requires skin and tissue replantation to restore lost structures. The treatment process is extremely long and expensive. Optimal burn management requires a comprehensive clinical analysis that not only includes the extent of tissue damage, but also the patient’s characteristics and disease burden. Individualization of care is key, and the age of the patient affects the time of recovery [4]. The procedure of HEMS teams in Poland is described in the internal procedure for burn patients and was prepared according to the recommendations of the American Burn Association (ABA).
All scientific opinions agree that burn-related complications can be minimized by proper and prompt first aid [5]. In addition to the actions taken by witnesses to the incident (including interrupting the process causing the burn, cooling with water), further medical management both in the pre-hospital settings and the performance of specialized procedures and treatment in medical facilities is crucial. The primary role is played by the time between the incident and the initiation of therapy. With that in mind, there are protocols developed for emergency services to conduct an initial examination, secure injuries, provide pain management, and allocate the patient to a dedicated hospital [6]. These tasks are usually performed by emergency medical services, which in Europe most often operate as ground-based emergency medical services (EMS) [7] and air emergency medical services (AEMS) [8]. In Poland, AEMS carry out HEMS missions [9]. AEMS crews consist of a professional medical team (medical doctor and paramedic/nurse), as well as a pilot [10]. The specifics of ground teams, which most often do not include a doctor, are different [11,12,13].
Currently, there are 22 AEMS bases in Poland (including one seasonal base) ready to carry out HEMS missions with EC135 helicopters. The HEMS team crew consists of a pilot, a paramedic/nurse, and a physician. In addition, AEMS has two jet aircraft for long-distance transport and Robinson R-44 helicopters. HEMS missions are ordered by medical dispatchers. Decisions on transporting a patient to a dedicated medical facility are made by the crew physician. There are 11 burn treatment centers in Poland, the list of which and the current number of vacancies are posted on the website www.lpr.com.pl (accessed on 1 December 2024). Additionally, some hospitals perform shifts and have a burn unit in their resources.
The authors attempted in this study to outline the profile of a burn patient from an HEMS perspective, as well as to identify the medical procedures implemented and the transport to hospital. Both the medical activities carried out at the scene by the medical team and the target transport site were analyzed, including the Burn Centers (BC).
2. Materials and Methods
The study material consisted of medical and operational records of the AEMS of 1 January 2018 to 31 December 2022. The scope included all missions performed in the country for burn patients. The approval of the unit’s administrator, as well as the ethics committee No. 4/2024 of the University of Siedlce, were obtained. The data were anonymized and processed digitally. The inclusion criteria were missions containing the term “burn” in the AEMS digital database—both in the documentation description and the diagnosis according to the ICD-10 classification. Cases in which the analyzed criteria were not described in the medical documentation were not included.
Statistical processing—results, relationships, and correlations were developed using spreadsheet Microsoft Excel 365 and Statistica 13.3. Sociodemographic data on patients, technical data on HEMS flights, and medical procedures implemented were compiled using counts and percentages for qualitative variables and descriptive statistics (mean, standard deviation, median, mode, minimum and maximum). Pearson’s Chi-square test was used to test the relationship between the two qualitative variables. Fisher’s exact test was chosen interchangeably when the expected counts were less than 5. Welch’s test was used to compare two groups and more than two groups—in several cases the distribution of the dependent variable was significantly different from normal, this was checked by the W Shapiro–Wilk test, but with the large groups (n > 30), a parametric test was chosen. The variances in the compared groups were heterogeneous. On the other hand, the Wilcoxon test was used to compare two dependent samples—the dependent variable in this case was ordinal. The significance level was set at p = 0.05.
3. Results
3.1. Characteristics of the Study Group
The total number of missions included in the analysis was 2154, selected from a digital database run by the Polish Medical Air Rescue. Patient ages ranged from 1 month to 96 years (mean 35.05; SD ± 26.88). Adult patients (n = 1409; 65.41%) constituted the vast majority. The number of interventions to children below 1-year-old—as many as 394 cases, or nearly one-fifth of all missions (18.29%)—is noticeable. Men suffered burns as much as three times more often than women (n = 1574, 73.07% vs. n = 570, 26.46%), as shown in Table 1.

Table 1.
Characteristics of burn patients during HEMS missions.
Statistical analysis showed significant differences in age between patients according to ICD10 diagnoses (p < 0.001). It turned out that patients with the lowest age had a diagnosis of T21—thermal and chemical burn of the torso (Me = 1 year). In contrast, the oldest victims experienced thermal and chemical burns of the respiratory tract (Me = 51 years), as well as thermal burns classified by the extent of the body surface covered (Me = 45 years). Tukey’s post hoc test confirmed that age was significantly higher for T27 diagnoses and significantly lower for T21 than for most other diagnoses.
A statistically significant association was found between age group and ICD-10 diagnosis (p < 0.001). Pediatric patients were significantly more likely to experience thermal and chemical burns of the torso, i.e., T21 (27.19%), than adult patients (5.11%). In contrast, adults were far more likely to be diagnosed with T27: Thermal and chemical burns of the respiratory tract (5.11%), as well as T29—thermal and chemical burns to numerous areas of the body (47.13%). The results of the analysis are shown in Table 2.

Table 2.
ICD-10 diagnoses among burn patients receiving AEMS intervention by age group.
3.2. Transport
The on-scene management of the air emergency medical team included not only transport to the treatment facility (n = 1679; 77.95%), but also the possibility of leaving the patient at the scene (n = 48; 2.23%), handing over to another AEMS team (n = 53; 2.46%), Polish Medical Air Rescue medical airplane (n = 36; 1.57%), and ground teams. This is related to ensuring the patient’s continuity of professional medical care in the pre-hospital setting, as well as the allocation of sometimes long distances for transfer to a higher referral center (Table 3).

Table 3.
Handing over patients during HEMS missions.
The vast majority of patients were transported from the scene directly to Burn Treatment Centers (n = 1373; 63.74%), and slightly less than a third to another treatment facility (30.22%). An analysis by age was also performed, and it was found that as many as 77.86% of adult patients ended up in a Burn Treatment Center, while this percentage was significantly lower among pediatric patients, at 33.14% (Chi2 p < 0.001) (Table 4).

Table 4.
HEMS missions by target hospital in terms of age group.
3.3. Pharmacological Treatment
Analysis of the NRS pain rating scale showed that the pain level of burn patients decreased significantly as a result of the treatment implementation by the Polish Medical Air Rescue (p < 0.001). Before treatment, the median pain score among patients was 2, and after treatment introduction, it was 0 (Figure 1).
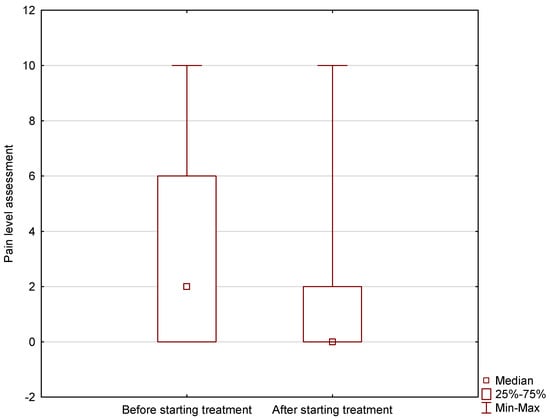
Figure 1.
Pain level of burn patients before and after treatment implementation in AEMS settings.
In addition to anesthetic drugs, a number of other preparations were used in 43.13% of burn patients; the most common of which were ketamine (23.72%), rocuronium bromide (15.78%), and propofol (14.02%). A summary of the medications that the AEMS crew was authorized to administer is provided in Table 5.

Table 5.
Medications administered to burn patients during HEMS missions.
3.4. Emergency Procedures
The list of procedures for which a medical doctor is authorized in Poland was selected to avoid discrepancies in the competence of representatives of other medical professions operating in the pre-hospital emergency system. The authors included missions that HEMS crews performed independently or by taking over a patient from a ground medical rescue team, who may have implemented some rescue procedures beforehand. Slightly less than half of burn patients (43.55%) required specialized medical treatments implemented by the HEMS team. The AEMS physician most often made the decision to perform the following: sedation (30.87%), as well as intubation (13.42%), mechanical ventilation (13.23%), and relaxation (8.40%). A detailed summary is provided in Table 6. In 22 cases, sudden cardiac arrest (SCA) was diagnosed, and resuscitation was implemented. In 7 patients (31.82%) with SCA, a mechanical chest compression device was used in the HEMS setting.

Table 6.
Emergency procedures performed on burn patients during HEMS missions.
In a detailed analysis, the authors noted some correlations (Table 7). Adult patients were intubated almost seven times more often (18.15%) than pediatric patients (2.71%). The differences shown were statistically significant (p < 0.001). Statistical analysis showed a significant association between sex and intubation (p = 0.013). Men were intubated significantly more often than women (10.99% vs. 5.34%). The observed differences were found to be statistically significant (p < 0.001). RTS (p < 0.001) and GCS (p < 0.001) scores were significantly lower in burn patients who were intubated. Furthermore, intubation was used significantly more often in subjects with abnormal ECG (p < 0.001), dyspnea (p < 0.001), cyanosis (p = 0.001), and pale skin (p < 0.001).

Table 7.
The use of intubation in patients during HEMS missions.
4. Discussion
Individuals with body injuries constitute a significant group of patients requiring the aid of emergency medical teams [14]. Burns, due to their nature, are among the injuries that often generate the need to implement specialized treatments as early as possible in the pre-hospital settings, and then organize transfer to dedicated treatment centers. The authors analyzed a number of variables obtained from several years of medical records of a nationwide emergency unit in Poland—the Polish Medical Air Rescue [15].
The profile of the burn patient from the AEMS perspective indicated male sex (n = 1574; 73.07%) and a mean age of 35.05 years (SD ± 26.88). The study by Wejnarski et al. [16] confirms the results obtained, indicating significantly more frequent AEMS interventions to adult patients. However, it is important to stress the noted significant number of missions to infants and newborns, which accounted for as many as 394 cases (18.29% of all missions). The data suggest that HEMS crews are much more likely to be dispatched to the scene if the burn patient is a child under 1-year-old. In the study by Nicholson B. et al., HEMS intervention rates for burnt children were shown to be as high as 18.1% [17]. It should be noted that helicopter rescue flights are associated with risk. In the case of night time, dense development, and bad weather conditions, there is a risk for both the crew and the patient being transported. The lack of sufficient infrastructure sometimes causes the need for additional ambulance transport from the helicopter to the hospital building (no landing pad at the hospital).
Patients showed extensive body burns, as suggested by the ICD-10 code (T29—multiple body areas), which was diagnosed in 890 cases, code T21 (trunk) diagnosed in 255 cases, and T31 (extensive) in 243 cases. The AEMS physician diagnosed respiratory burns (T27) only in 3.62% of the missions (n = 78). Patients with such injuries usually show a more severe general condition and require the implementation of mechanical ventilation, as confirmed by a study by Cachafeiro et al. [18]. During statistical analysis, a significant relationship was found between the age group and the ICD-10 diagnosis (p < 0.001). The study showed that pediatric patients were significantly more likely to experience thermal and chemical burns of the torso than adult patients (5.11%). Adults, on the other hand, were significantly more likely to suffer respiratory burns than children. Having considered the foregoing, it can be concluded that inhalation burns are the domain of adult patients.
As already mentioned, maintaining treatment continuity by providing transportation to a higher reference center has an important role in rescue missions for burn patients. Some hospitals have the status of Burn Treatment Center in Poland. These dedicated treatment facilities were used in 63.74% of the cases analyzed. There are literature sources confirming the important role of air ambulance teams in allocating patients to dedicated medical facilities [19,20,21,22]. Our results confirmed this strategy to be effective, yet it is worth considering the reasons behind not transferring a patient to the Burn Treatment Center. The factors influencing this relationship are based on a number of variables, ranging from the physician’s decision at the scene to the hospital’s ability to accommodate a helicopter, which requires having an active helipad in the facility’s infrastructure. Roman J. et al. pointed out another problem concerning the economics of dispatching HEMS teams for minor burns [23]. The cost of a rescue helicopter intervention is significantly higher compared to a ground ambulance; therefore, the necessity of dispatching should always be considered.
Further results demonstrated the forms of patient transfer from the helicopter to ground medical rescue teams, which accounted for 315 cases. It can be inferred that this solution was used precisely because of the inability to land directly at the Burn Treatment Center.
The study conducted also included the burn patient treatment from the perspective of the Polish Medical Air Rescue. It was proven that effective analgesic treatment was implemented, achieving a statistically significant reduction in pain levels (p < 0.001). This confirms that adequate analgesia forms the basis of medical care for trauma patients [24,25,26,27]. The authors also presented the use of other pharmacological agents, including achieving sedation, relaxation, or administering pressure amines. It is reasonable to believe that the most commonly used medications (ketamine, rocuronium bromide, propofol) were used by the HEMS crew to perform RSI (rapid sequence intubation).
The AEMS physician is also qualified and authorized to perform advanced emergency procedures [28,29]. Sedation, endotracheal intubation, and mechanical ventilation were among the most commonly performed specialist procedures. The database obtained by the authors did not allow determining from which type of ground team (with or without a physician) the HEMS crew took over the patient. One may conclude that the incidents to which the rescue helicopter was called by the emergency medical team took over the patient from both teams with a physician and those only with paramedics; the latter are not yet certified to perform RSI [30]. The authors recommend further research to assess this correlation, as the number of intubations performed by HEMS crews (n = 289; 13.42%) appears to be significant, given that the vast majority of flights are supposed to support ground teams. Hall K. et al., in a retrospective review of burn patient records from a large Australian Helicopter Ambulance Service, found that intubation was performed in 60 of 490 cases, which is 12.24% [31]. The result is comparable to that obtained by the authors of the present study. In cases of sudden cardiac arrest, both Polish medical doctors and paramedics perform endotracheal intubation, greatly improving airway security in trauma patients [32,33]. Further training and development of local authorizations for medical personnel appear to be necessary, in order to provide professional medical assistance regardless of emergency medical team type [34,35].
Limitations of the study
The data analyzed partially covered the COVID-19 pandemic period. The authors recognize the possibility that the state of the epidemic might have affected the actual number and the true nature of incidents involving trauma patients, including those suffering burns, which required AEMS intervention [36,37]. The medical records had some information missing (e.g., determining the patient’s age), resulting in limited data in 72 cases in the patient profile section. The database also did not provide detailed information on the purpose of the patient’s transfer to the ground-based EMS team or the police. This information could be supplemented by conclusions covering the organizational and transportation activities of HEMS crews. The authors limited the analysis to medications and procedures performed exclusively by a medical doctor. Standard procedures (e.g., fluid therapy, application of topical dressings) that can also be performed by paramedics were omitted.
5. Conclusions
HEMS crews are more likely to have to intervene to men suffering burns than women. The predominant age group is adults; yet there is a special role for helicopter crews demonstrated for children under 1-year-old. Both pediatric and adult patients were most often diagnosed with extensive body burns, which raises the need to implement additional medical measures. In 63.74% of the missions, patients were transported to the Burn Treatment Center. The cooperation of the HEMS with ground emergency medical teams during transportation to the hospital seems to be crucial for safe, prompt and effective transfer. HEMS crews implement effective pharmacological analgesia, and handle rescue medications and procedures to stabilize the patient’s condition. The authors suggest that the results obtained should form the basis for analyzing the possibility of expanding higher-referral facilities with helipads for HEMS crews, which could significantly speed up the transfer of patients without the need for an additional transfer by ambulance.
Author Contributions
Conceptualisation, A.W., P.K.L., M.B., M.M., K.M., D.S., P.R., R.G. and L.M.; methodology, A.W., P.K.L., M.B., M.M. and P.R.; software, A.W., M.B. and M.M.; validation, A.W., P.K.L., M.B., M.M., K.M., D.S., P.R., R.G. and L.M.; formal analysis, A.W., P.K.L., M.B. and M.M.; investigation, A.W., P.K.L., M.B. and M.M.; resources, A.W., P.K.L., M.B., M.M., K.M., D.S., P.R., R.G. and L.M.; data curation, A.W., P.K.L., M.B., M.M., P.R. and R.G.; writing—original draft preparation, A.W., P.K.L., M.B. and M.M.; writing—review and editing, A.W., K.M., D.S., P.R., R.G. and L.M.; visualisation, A.W., P.K.L., M.B. and M.M.; supervision, A.W., P.K.L., M.B., M.M., K.M., D.S., P.R., R.G. and L.M.; project administration, A.W., P.K.L., M.B., M.M., K.M., D.S., P.R., R.G. and L.M. All authors have read and agreed to the published version of the manuscript.
Funding
No fund was received related to this study.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethics committee No. 4/2024 of the University of Siedlce.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gomez, R.; Cancio, L.C. Management of Burn Wounds in the Emergency Department. Emerg. Med. Clin. N. Am. 2007, 25, 135–146. [Google Scholar] [CrossRef] [PubMed]
- WHO. Burn. Available online: https://www.who.int/en/news-room/fact-sheets/detail/burns (accessed on 24 September 2024).
- Smolle, C.; Cambiaso-Daniel, J.; Forbes, A.A.; Wurzer, P.; Hundeshagen, G.; Branski, L.K.; Huss, F.; Kamolz, L.P. Recent trends in burn epidemiology worldwide: A systematic review. Burns 2017, 43, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Stylianou, N.; Buchan, I.; Dunn, K.W. A review of the international Burn Injury Database (iBID) for England and Wales: Descriptive analysis of burn injuries 2003–2011. BMJ Open 2015, 5, e006184. [Google Scholar] [CrossRef] [PubMed]
- Fadeyibi, I.O.; Ibrahim, N.A.; Mustafa, I.A.; Ugburo, A.O.; Adejumo, A.O.; Buari, A. Practice of first aid in burn related injuries in a developing country. Burns 2015, 41, 1322–1332. [Google Scholar] [CrossRef] [PubMed]
- Wejnarski, A.; Leszczyński, P.; Świeżewski, S.; Podgórski, M.; Farkowski, M.M.; Sterliński, M.; Panczyk, M.; Gotlib, J.; Rabczenko, D.; Gałązkowski, R.M. Characteristics of aeromedical transport, both inter-hospital and directly from the scene of the incident, in patients with acute myocardial infarction or acute trauma between 2011–2016 in Poland: A case-control study. Adv. Clin. Exp. Med. 2019, 28, 1495–1505. [Google Scholar] [CrossRef]
- Leszczyński, P.K.; Sobolewska, P.; Muraczyńska, B.; Gryz, P.; Kwapisz, A. Impact of COVID-19 Pandemic on Quality of Health Services Provided by Emergency Medical Services and Emergency Departments in the Opinion of Patients: Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 1232. [Google Scholar] [CrossRef]
- Chappelle, C.; Li, C.; Vascik, P.D.; Hansman, R.J. Opportunities to enhance air emergency medical service scale through new vehicles and operations. In Proceedings of the 2018 Aviation Technology, Integration, and Operations Conference, Atlanta, Georgia, 25–29 June 2018. 2883. [Google Scholar] [CrossRef]
- Świeżewski, S.P.; Rzońca, P.; Panczyk, M.; Leszczyński, P.K.; Gujski, M.; Michalak, G.; Fronczak, A.; Gałązkowski, R. Polish Helicopter Emergency Medical Service (HEMS) Response to Stroke: A Five-Year Retrospective Study. Med. Sci. Monit 2019, 25, 6547–6553. [Google Scholar] [CrossRef] [PubMed]
- Świeżewski, S.P.; Wejnarski, A.; Leszczyński, P.K.; Wojak, A.; Fronczak, A.; Darocha, T.; Gałązkowski, R.; Opolski, G.; Rzońca, P. Characteristics of urban vs rural utilization of helicopter emergency medical service in patients with ST-elevation myocardial infarction in Poland. Kardiol. Pol. 2020, 78, 284–291. [Google Scholar] [CrossRef]
- Mitura, K.; Snarska, J.; Celiński, D.; Maślach, D.; Leszczyński, P.K.; Binkowska, A.; Szpakowski, L.; Szajda, S.D. ICD-10 Classification in the Practice of Emergency Medical Teams: New Insights. Emer. Med. Inter. 2024, 2024, 8506561. [Google Scholar] [CrossRef] [PubMed]
- Trochimiak, P.; Leszczyński, P.K.; Świniarski, P. Comparative analysis of pharmacotherapy used by Emergency Medical Services in Poland. Crit. Care Innov. 2020, 3, 20–30. [Google Scholar] [CrossRef]
- Zdzieborska, P.; Sholokhova, D.; Zalewski, R. Characteristics of emergency medical service (EMS) calls to mentally disabled residents of a social welfare home. Crit. Care Innov. 2023, 6, 1–12. [Google Scholar] [CrossRef]
- Ramzee, A.F.; El-Menyar, A.; Asim, M.; Kanbar, A.; Ahmed, K.; Daoud, B.; Mathradikkal, S.; Kloub, A.; Al-Thani, H.; Rizoli, S. The impact of emergency department length of stay on the outcomes of trauma patients requiring hospitalization: A retrospective observational study. World J. Emerg. Med. 2023, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- Rzońca, P.; Gałązkowski, R.; Wójcik-Fatla, A.; Panasiuk, L.; Gotlib, J. Missions of the helicopter emergency medical service in rural and urban areas in Poland-a comparative retrospective analysis. Ann. Agric. Environ Med. 2019, 26, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Wejnarski, A.; Podgórski, M.; Kamecki, A.; Świeżewski, S.P. The role of the Polish Medical Air Rescue in optimization of transport time of patients. Anest. Rat. 2016, 10, 34–45. [Google Scholar]
- Nicholson, B.; Dhindsa, H. Helicopter transport in regionalized burn care: One program’s perspective. Air Med. J. 2016, 35, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Cachafeiro, L.; Sanchez, M.; Herrero, E.; Fernández, L.; Irazabal, M.; Hernandez, M.; Agrifoglio, A.; Garcia de Lorenzo, A.; Lendinez, M. Inhalation injury in critical burn patients. Crit. Care 2013, 17, 118. [Google Scholar] [CrossRef][Green Version]
- Kunecka, Z.; Marel, M. Analiza i ocena możliwości operacyjnych lotniczego pogotowia ratunkowego w ujęciu krajowym. J. Translog. 2021, 7, 39–52. [Google Scholar] [CrossRef]
- Gaździńska, A.; Jagielski, P.; Gałązowski, R. Assessment of physical activity of members of the helicopter emergency medical service (HEMS). Emerg. Med. Serv. 2020, 6, 91–98. [Google Scholar]
- Wejnarski, A.; Leszczyński, P.K.; Świeżewski, S.P.; Gałązkowski, R. Analiza profilu pacjentów transportowanych w lotach międzyszpitalnych realizowanych przez HEMS w Polsce w latach 2011-2015. Anest. Ratow. 2017, 11, 28. [Google Scholar]
- Rzońca, E.; Świeżewski, S.P.; Gałązkowski, R.; Bień, A.; Kosowski, A.; Leszczyński, P.; Rzońca, P. Neonatal transport in the practice of the crews of the polish medical air rescue: A retrospective analysis. Inter. J. Environ. Res. Public Health 2020, 17, 705. [Google Scholar] [CrossRef]
- Roman, J.; Shank, W.; Demirjian, J.; Tang, A.; Vercruysse, G.A. Overutilization of helicopter transport in the minimally burned—A healthcare system problem that should be corrected. J. Burn. Care Res. 2020, 41, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Latos, M.; Ladowska, D. The usage of morphine in daily practice by emergency medical services (ems). A pilot study. Emerg. Med. Serv. 2016, 3, 88–92. [Google Scholar]
- Szyller, J.; Koral, M.; Zyśko, D. Analysis of the paramedic administration of opioids in paramedical rescue teams. Anest. Ratow. 2013, 7, 165–172. [Google Scholar]
- Garrick, J.F.; Kidane, S.; Pointer, J.E.; Sugiyama, W.; Van Luen, C.; Clark, R. Analysis of the paramedic administration of fentanyl. J. Opioid. Manag. 2011, 7, 229–234. [Google Scholar] [CrossRef]
- Weldon, E.R.; Ariano, R.E.; Grierson, R.A. Comparison of Fentanyl and Morphine in the Prehospital Treatment of Ischemic Type Chest Pain. Prehosp. Emerg. Care 2016, 20, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Leszczyński, P.; Mioduski, M.; Gałązkowski, R. The NACA score as a predictor of ventricular cardiac arrhythmias—A retrospective six-year study. Am. J. Emerg. Med. 2020, 38, 2249–2253. [Google Scholar] [CrossRef]
- Leszczyński, P.; Wejnarski, A.; Rzońca, P.; Gajowniczek, A.; Gałązkowski, R.; Mitura, K.; Sholokhova, D. Arrhythmias in children occurring during HEMS intervention: A retrospective cohort study. Emerg. Med. Int. 2023, 2974648. [Google Scholar] [CrossRef]
- Szymczuk, P. Mortality in OHCA during resuscitation by rescue teams without a doctor. Crit. Care Innov. 2019, 2, 1–10. [Google Scholar] [CrossRef]
- Hall, K.; Burns, B. A review of the burns caseload of a physician-based helicopter emergency medical service. Emerg. Med. Australas. 2017, 29, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Rea, T.; Kudenchuk, P.J.; Sayre, M.R.; Doll, A.; Eisenberg, M. Out of hospital cardiac arrest: Past, present, and future. Resuscitation 2021, 165, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Scquizzato, T.; Gamberini, L.; D’Arrigo, S.; Galazzi, A.; Babini, G.; Losiggio, R.; Imbriaco, G.; Fumagalli, F.; Cucino, A.; Landoni, G.; et al. Incidence, characteristics, and outcome of out-of-hospital cardiac arrest in Italy: A systematic review and meta-analysis. Resusc. Plus 2022, 12, 100329. [Google Scholar] [CrossRef] [PubMed]
- Leszczyński, P.; Charuta, A.; Kołodziejczak, B.; Roszak, M. Evaluation of virtual environment as a form of interactive resuscitation exam. J. New Rev. Hyper. Multi. 2017, 23, 265–276. [Google Scholar] [CrossRef]
- Leszczyński, P.; Charuta, A.; Zacharuk, T. Cadaver as an educational tool increasing the effectiveness of Combat Application Tourniquet use in extremity injuries. Turk. J. Trauma Emerg. Surg. 2021, 27, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Ayvat, P. Distribution of papers on COVID-19 in the field of anesthesiology in individual countries and journals. Crit. Care Innov. 2021, 4, 8–22. [Google Scholar] [CrossRef]
- Kanchana, K.T.G.; Youhasan, P. Impact of sanitary restrictions related to the COVID-19 pandemic on the quality of life of the Sri Lankan population. Crit. Care Innov. 2022, 5, 29–39. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).