Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection and Data Collection Processes
2.3. Data Items
2.4. Study Risk of Bias Assessment
2.5. Assessment of the Certainty of the Evidence
2.6. Data Extraction and Method of Analysis
- dCAS group: Surgical navigation technology with real-time tracking of the intraoperative position of the surgical instrument and the patient on CBCT images.
- sCAS group: Surgical templates fabricated using stereolithographic computer-aided design and manufacturing (CAD-CAM) techniques from virtual simulations of the MS placement on 3D models reconstructed from CBCT or CT images.
- Radiographic guide group: Wire guides, grids, or any other partially guided devices used as radiopaque references in preoperative evaluation, regardless of whether the guide was used during the surgical procedure.
2.7. Statistical Analysis
3. Results
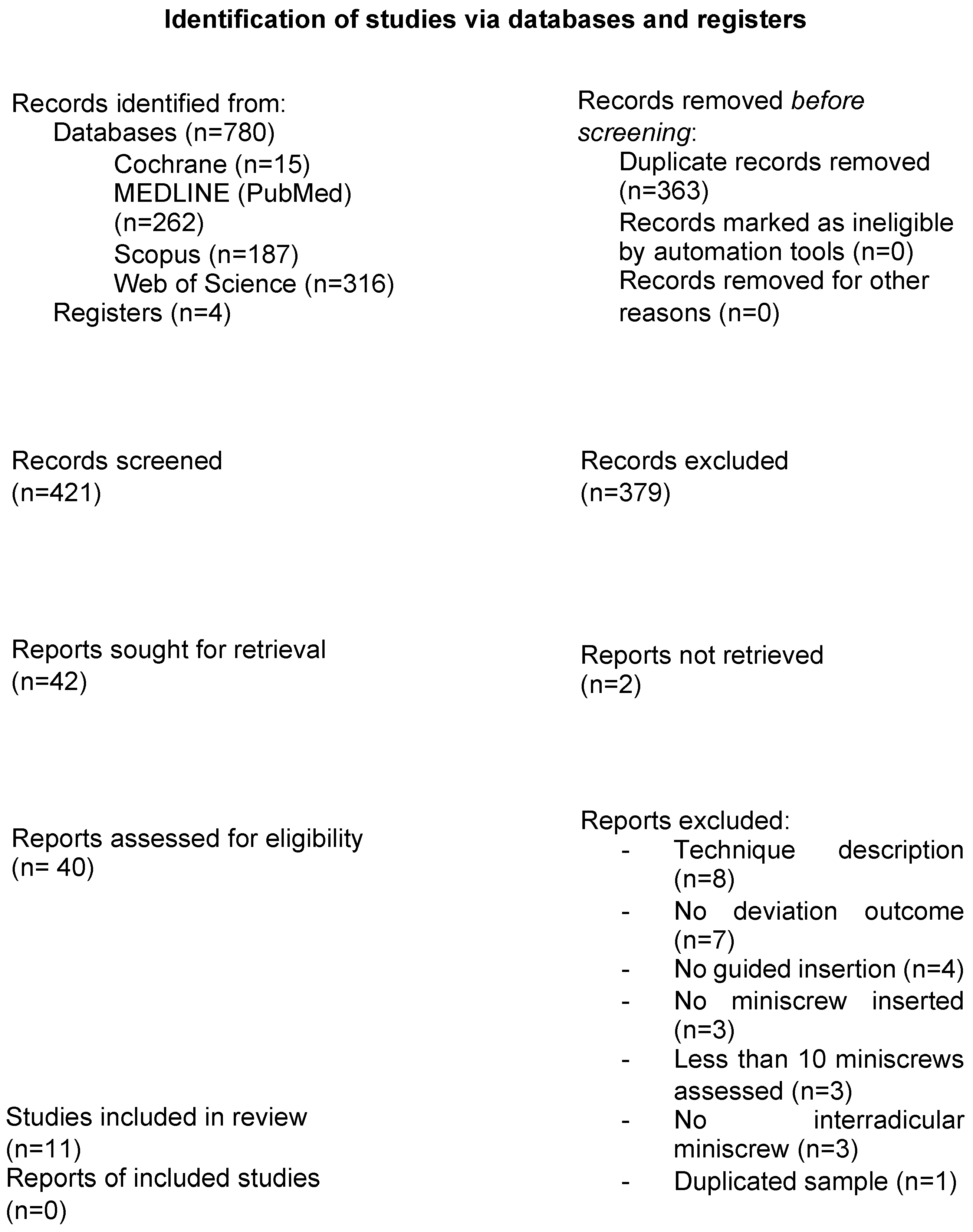
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias and Quality Assessment
3.4. Qualitative Synthesis
3.5. Assessment of the Certainty of the Evidence
3.6. Quantitative Synthesis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Padmini, M.; Bharathi, S.; Smitha, R.; Hamsa, P.R. Mini screws as temporary anchorage device in orthodontics: A narrative review. IOSR J. Dent. Med. Sci. 2016, 15, 55–62. [Google Scholar]
- Alkadhimi, A.; Al-Awadhi, E.A. Miniscrews for orthodontic anchorage: A review of available systems. J. Orthod. 2018, 45, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Jambi, S.; Walsh, T.; Sandler, J.; Benson, P.E.; Skeggs, R.R.; O’Brien, K.D. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database Syst. Rev. 2014, 2014, CD005098. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.M.; Yamamoto, T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am. J. Orthod. Dentofacial Orthop. 2007, 131, S68–S73. [Google Scholar] [CrossRef] [PubMed]
- Chun, Y.S.; Lee, S.K.; Wikesjö, U.M.; Lim, W.H. The interdental gingiva, a visible guide for placement of mini-implants. Orthod. Craniofac Res. 2009, 12, 20–24. [Google Scholar] [CrossRef]
- Landin, M.; Jadhav, A.; Yadav, S.; Tadinada, A. A comparative study between currently used methods and small volume-cone beam tomography for surgical placement of mini implants. Angle Orthod. 2015, 85, 446–453. [Google Scholar] [CrossRef]
- Barros, E.S.; Janson, G.; Chiqueto, K.; Garib, D.G. Two-dimensional radiographic and clinical references of the tooth crown for orthodontic mini-implant insertion: A guide-free technique. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, e8–e16. [Google Scholar] [CrossRef]
- Suzuki, E.Y.; Buranastidporn, B. An adjustable surgical guide for miniscrew placement. J. Clin. Orthod. 2005, 39, 588–590. [Google Scholar]
- Cousley, R.R.J.; Parberry, D.J. Surgical stents for accurate miniscrew insertion. J. Clin. Orthod. 2006, 40, 412–417. [Google Scholar]
- Choi, H.J.; Kim, T.W.; Kim, H.W. A precise wire guide for positioning interradicular miniscrews. J. Clin. Orthod. 2007, 41, 258–261. [Google Scholar]
- Cassetta, M.; Altieri, F.; Di Giorgio, R.; Barbato, E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: Description of a technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, D.; Wang, G.; Wang, C.; Zhao, Z. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 728.e1–728.e10. [Google Scholar] [CrossRef] [PubMed]
- Retana, A.; Emery, R.W.; Keir, V. Removal of impacted supernumerary teeth using a dynamic surgical navigation system: A case report. J. Oral Maxillofac. Surg. 2019, 77, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Emery, R.W.; Korj, O.; Agarwal, R. A review of in-office dynamic image navigation for extraction of complex mandibular third molars. J. Oral Maxillofac. Surg. 2017, 75, 1591–1600. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Furuki, T. Application of computer-assisted navigation systems in oral and maxillofacial surgery. Jpn. Dent. Sci. Rev. 2018, 54, 139–149. [Google Scholar] [CrossRef]
- Landaeta-Quinones, C.G. Computer-assisted surgery: Applications in dentistry and oral and maxillofacial surgery. Dent. Clin. N. Am. 2018, 62, 403–420. [Google Scholar] [CrossRef]
- Mihit, F.Z.; Zubizarreta-Macho, Á.; Montiel-Company, J.M.; Albaladejo Martínez, A. Systematic review and network meta-analysis of the accuracy of orthodontic mini-implants placed in the inter-radicular space by image-guided techniques. BMC Oral Health 2023, 23, 383. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024). Cochrane. 2024. Available online: www.training.cochrane.org/handbook (accessed on 1 September 2024).
- Sterne, J.; Savović, J.; Page, M.; Elbers, R.; Blencowe, N.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, 4898. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, B.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, USA, 2011. [Google Scholar]
- Montagner, A.F.; Sarkis-Onofre, R.; Pereira-Cenci, T.; Cenci, M.S. MMP inhibitors on dentin stability: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 733–743. [Google Scholar] [CrossRef]
- AlShwaimi, E.; Bogari, D.; Ajaj, R.; Al-Shahrani, S.; Almas, K.; Majeed, A. In vitro antimicrobial effectiveness of root canal sealers against Enterococcus faecalis: A systematic review. J. Endod. 2016, 42, 1588–1597. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Skupien, J.A.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thompson, S. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Patsopoulos, N.A.; Evangelou, E.; Ioannidis, J.P.A. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008, 37, 1148–1157. [Google Scholar] [CrossRef]
- Suzuki, E.Y.; Suzuki, B. Accuracy of miniscrew implant placement with a 3-dimensional surgical guide. J. Oral Maxillofac. Surg. 2008, 66, 1245–1252. [Google Scholar] [CrossRef]
- Estelita, S.S.; Janson, G.; Chiqueto, K.; Janson, M.; de Freitas, M.R. Predictable drill-free screw positioning with a graduated 3-dimensional radiographic-surgical guide: A preliminary report. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 722–735. [Google Scholar] [CrossRef]
- Morea, C.; Hayek, J.E.; Oleskovicz, C.; Dominguez, G.C.; Chilvarquer, I. Precise insertion of orthodontic miniscrews with a stereolithographic surgical guide based on cone beam computed tomography data: A pilot study. Int. J. Oral Maxillofac. Implant. 2011, 26, 860–865. [Google Scholar]
- Qiu, L.; Xu, H.; Feng, P.; Sha, X.; Zhang, H. Clinical effectiveness of orthodontic miniscrew implantation guided by a novel cone beam CT image-based CAD-CAM template. Ann. Transl. Med. 2021, 9, 1025. [Google Scholar] [CrossRef]
- Bae, M.J.; Kim, J.Y.; Park, J.T.; Cha, J.Y.; Kim, H.J.; Yu, H.S.; Hwang, C.-J. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 893–901. [Google Scholar] [CrossRef]
- Yu, J.J.; Kim, G.T.; Choi, Y.S.; Hwang, E.H.; Paek, J.; Kim, S.H.; Huang, J.C. Accuracy of a cone beam computed tomography-guided surgical stent for orthodontic mini-implant placement. Angle Orthod. 2012, 82, 275–283. [Google Scholar] [CrossRef]
- Qiu, L.; Haruyama, N.; Suzuki, S.; Yamada, D.; Obayashi, N.; Kurabayashi, T.; Moriyama, K. Accuracy of orthodontic miniscrew implantation guided by stereolithographic surgical stent based on cone-beam CT-derived 3D images. Angle Orthod. 2012, 82, 284–293. [Google Scholar] [CrossRef]
- Riad-Deglow, E.; Toledano-Gil, S.; Zubizarreta-Macho, Á.; Bufalá-Pérez, M.; Rodríguez Torres, P.; Tzironi, G.; Albaladejo-Martínez, A.; López-Román, A.; Hernández-Montero, S. Influence of the computer-aided static navigation technique and mixed reality technology on the accuracy of the orthodontic micro-screws placement. An in vitro study. J Pers Med. 2021, 11, 964. [Google Scholar] [CrossRef] [PubMed]
- Thakur, A.; Toshniwal, N.; Misal, A.; Mathur, A. Comparison of accuracy of various positioning guides used for determination of implant placement site using RVG. J. Indian. Orthod. Soc. 2012, 46, 70–76. [Google Scholar] [CrossRef]
- Kalra, S.; Tripathi, T.; Rai, P.; Kanase, A. Evaluation of orthodontic mini-implant placement: A CBCT study. Prog. Orthod. 2014, 15, 61. [Google Scholar] [CrossRef]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe zones”: A guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar]
- Alharbi, F.; Almuzian, M.; Bearn, D. Miniscrews failure rate in orthodontics: Systematic review and meta-analysis. Eur. J. Orthod. 2018, 40, 519–530. [Google Scholar] [CrossRef]
- Cheng, S.J.; Tseng, I.Y.; Lee, J.J.; Kok, S.H. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int. J. Oral Maxillofac. Implant. 2004, 19, 100–106. [Google Scholar]
- Park, H.S.; Jeong, S.H.; Kwon, O.W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 18–25. [Google Scholar] [CrossRef]
- Deguchi, T.; Nasu, M.; Murakami, K.; Yabuuchi, T.; Kamioka, H.; Takano-Yamamoto, T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 721.e7–721.e12. [Google Scholar] [CrossRef]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Kyung, H.M.; Park, H.S.; Bae, S.M.; Sung, J.H.; Kim, I.B. Development of orthodontic micro-implants for intraoral anchorage. J. Clin. Orthod. 2003, 37, 321–328. [Google Scholar]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 416–435. [Google Scholar] [CrossRef] [PubMed]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery: A review. Int. J. Oral Maxillofac. Implant. 2006, 21, 855–863. [Google Scholar]
- Wexler, A.; Tzadok, S.; Casap, N. Computerized navigation surgery for the safe placement of palatal implants. Am. J. Orthod. Dentofac. Orthop. 2007, 131 (Suppl. S4), S100–S105. [Google Scholar] [CrossRef] [PubMed]
- Brilli, D.; Cauli, I.; Cassetta, M. How palatal vault morphology and screw length influence the accuracy of dynamic computer-guided orthodontic miniscrew insertion: A prospective clinical study. J. Dent. 2024, 146, 105093. [Google Scholar] [CrossRef]
- Prager, T.; Karapetian, V.; Muller-Hartwich, R.; Zoller, J.E.; Mischkowski, R. Application of a computer navigation system for the placement of orthodontic anchorage screws. Int. J. Comput. Dent. 2008, 11, 201–212. [Google Scholar]

| Variable | Definition | ||
|---|---|---|---|
| Primary outcome | Safety | Risk of root contact or damage during the surgical procedure | |
| Secondary outcome | Accuracy | Angular deviation | Difference in the angulation of the MS compared to the planned insertion angle |
| Coronal deviation | Difference in the MS position from the planned position at the coronal level | ||
| Apical deviation | Difference in the MS position from the planned position at the apical level | ||
| Authors (Year) | Country | Design | No. of Subjects MSs | MS Type and Dimensions | Groups | Pre-Operative Planning Method | Post-Operative Planning Method |
|---|---|---|---|---|---|---|---|
| Bae et al. (2013) [30] | South Korea | Cadaver study | 12–45 | BMK; Biomaterials Korea, Seoul, Republic of Korea (1.5 × 7 mm) |
|
| Pre and post CBCT overlapping + 3D analysis program |
| Estelita et al. (2009) [27] | Brazil | Cohort prospective study | 6–10 | SH 1514-07, Absoanchor, Dentos, Daegu, Republic of Korea (1.5 × 7 mm) | Radiographic guide | Intraoral radiograph | Intraoral radiograph |
| Kalra et al. (2014) [35] | India | RCT split-mouth | 13–40 | DB Orthodontics Limited, West Yorkshire, UK (1.5 × 9 mm) |
|
| CBCT without overlapping |
| Liu et al. (2010) [12] | China | Cohort prospective study | 11–34 | Beici Medical Company, Ningbo, China (1.6 × 11mm) | sCAS | CBCT + 3D planning software | Pre and post CBCT overlapping + 3D analysis program |
| Morea et al. (2011) [28] | Brazil | Cohort prospective study | 4–10 | Dentaurum, Ispringen, Germany (NR × 6–8 mm) | sCAS | CBCT + 3D planning software | Pre and post CBCT overlapping + 3D analysis program |
| Qiu et al. (2012) [32] | China | In vitro study | 3–30 | Ortholution, Seoul, Republic of Korea (1.8 × 7 mm) |
| CBCT + 3D planning software | Pre and post CBCT overlapping + 3D analysis program |
| Qiu et al. (2021) [29] | China | Cohort prospective study | 10–24 | Ningbo Cibei Medical Equipment Co. LTD., China (1.6 × 9 mm) | sCAS | CBCT + 3D planning software | Pre and post CBCT overlapping + 3D analysis program |
| Riad et al. (2021) [33] | Spain | In vitro study | 14–207 | Dual Top® Anchor System, JEIL Medical Corporation, Guro-gu, Seoul, Republic of Korea (1.3 × 8 mm) |
| CBCT + 3D planning software | Pre and post CBCT overlapping + 3D analysis program |
| Suzuki et al. (2008) [26] | Thailand | Cohort retrospective study | NR–220 | NR |
| Intraoral radiograph | Intraoral radiograph |
| Thakur et al. (2012) [34] | India | Cohort prospective study | 21–21 | NR (1.3 × 8 mm) |
| Intraoral radiograph | Intraoral radiograph |
| Yu et al. (2012) [31] | South Korea | Animal study | 4–32 | C-implant, C-implant Company, Seoul, Republic of Korea (1.8 × 8.5 mm) | Radiographic guide | CBCT and manually transferring the planning to the surgical stent | CBCT without overlapping |
| Study | Selection | Comparability | Outcome | NOS Score and Overall Quality Assessment |
|---|---|---|---|---|
| Estelita et al. [27] | ** | N/A | ** | 4 (low quality) |
| Liu et al. [12] | *** | N/A | ** | 5 (low quality) |
| Morea et al. [28] | *** | N/A | ** | 5 (low quality) |
| Suzuki et al. [26] | **** | - | ** | 6 (medium quality) |
| Thakur et al. [34] | ** | - | ** | 4 (low quality) |
| Qiu et al. [29] | *** | N/A | ** | 5 (low quality) |
| Study | Control | Sample Size Calculation | Randomization | Allocation Concealment | Same Experimental Conditions | Properly Described Intervention |
|---|---|---|---|---|---|---|
| Bae et al. [30] | Y | N | N | N | N | Y |
| Qiu et al. [32] | Y | N | N | N | Y | Y |
| Riad et al. [33] | Y | N | Y | N | Y | Y |
| Yu et al. [31] | N | N | N/A | N/A | N/A | Y |
| Study | Same Operator | Blinding Operator | Blinding Outcome Assessor | Incomplete Outcome | Overall Assessment | |
| Bae et al. [30] | Unclear | N | Unclear | Unclear | High risk | |
| Qiu et al. [32] | Unclear | N | Unclear | Unclear | High risk | |
| Riad et al. [33] | Y | N | Unclear | Unclear | Medium risk | |
| Yu et al. [31] | N | N | Unclear | Unclear | High risk | |
| Authors (Year) | Studied Variables | No. of Root Contacts | Deviations |
|---|---|---|---|
| Bae et al. [30] | 3D angular deviations (°) and 3D distance (coronal and apical) deviations (mm); root contact or damage | sCAS: 4/25 (contact) FH: 6/20 (contact) and 4/20 (damage) | 3D coronal deviations *:
|
| Liu et al. [12] | Angular (°) and lineal (mm) deviations measured at the apex and placement sites (reported in 3 directions: distomesial, vertical, and buccopalatal) | NR– All deviations of the miniscrews were in the safe zone (less than 0.86 ± 0.125 mm) | Coronal deviation:
|
| Morea et al. [28] | 3D angular (°) deviation and distance (coronal, central, and apical) deviations, root contact | 0/10 | 3D coronal deviation: 0.86 ± 0.57 mm 3D central deviation: 0.71 ± 0.34 mm 3D apical deviation: 0.87 ± 0.54 mm Angular deviation: 1.76 ± 0.93° |
| Qiu et al. [32] | Angular (°) and lineal (mm) deviations measured at the apex and placement sites (reported in two directions: mesiodistal and vertical), root contact | FH: 4/10 sCAS: 0/20 | Coronal deviations:
|
| Qiu et al. [29] | 3D distance (coronal and apical) deviations (mm); root contact | 0/24 |
|
| Riad et al. [33] | 3D angular (°) deviation and distance (coronal and apical) deviations (mm); root contacts | sCAS: 0/69 Mixed-reality: 0/69 FH: 12/69 | 3D coronal deviation *:
3D apical deviation *:
3D angular deviation *:
|
| Authors (Year) | Studied Variables | No. of Roots Contacts | Deviations |
|---|---|---|---|
| Estelita et al. [27] | Miniscrew centralization degree, inaccuracy degree, and risk index | NR | Mesiodistal lineal deviation (inaccuracy degree): 0.17 ± 0.11 mm |
| Kalra et al. [35] | Height deviation (mm), angular mesiodistal (°), and distance mesiodistal deviations (mm) measured at the coronal and apical areas; root contact | Radiographic guide: 3/20 FH: 0/20 | Height deviation:
|
| Suzuki et al. [26] | Angular deviation (°) and distance deviation (mm) measured at the head and tip | Radiographic guide 1 (custom-made sleeve guide): 0/180 (damage) Radiographic guide 2 (wire guide): 0/20 (damage) FH: NR | 2D Coronal deviation *:
|
| Thakur et al. [34] | Horizontal distances: PDL-PDL, PIP-GC, PIP-nearest root, AIP-GC, AIP-nearest root; vertical distance: PIP-AC, AIP-AC; number of radiographs required Pre, post, and differences between pre-post | Radiographic guide 1 (grid): 0/7 Radiographic guide 2 (X-ray pin): 0/7 Radiographic guide 3 (wire eye): 0/7 NR– All deviations of the miniscrews were in the safe zone | Horizontal distance PIP-GC (preoperative) *
|
| Yu et al. [31] | Vertical and horizontal angulation between prescribed and final mini-implant positions | NR |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santmartí-Oliver, M.; Jorba-García, A.; Moya-Martínez, T.; de-la-Rosa-Gay, C.; Camps-Font, O. Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 7697. https://doi.org/10.3390/jcm13247697
Santmartí-Oliver M, Jorba-García A, Moya-Martínez T, de-la-Rosa-Gay C, Camps-Font O. Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(24):7697. https://doi.org/10.3390/jcm13247697
Chicago/Turabian StyleSantmartí-Oliver, Margalida, Adrià Jorba-García, Tania Moya-Martínez, Cristina de-la-Rosa-Gay, and Octavi Camps-Font. 2024. "Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 24: 7697. https://doi.org/10.3390/jcm13247697
APA StyleSantmartí-Oliver, M., Jorba-García, A., Moya-Martínez, T., de-la-Rosa-Gay, C., & Camps-Font, O. (2024). Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(24), 7697. https://doi.org/10.3390/jcm13247697







