Age Variation in Patients with Troponin Level Elevation Without Obstructive Culprit Lesion or Suspected Myocardial Infarction with Non-Obstructive Coronary Arteries—Long-Term Data Covering over Decade
Abstract
1. Introduction
2. Material and Methods
2.1. Study Population and Definition of Troponin Level Elevation Without Obstructive CAD
2.2. Definition of Troponin Level Elevation Without an Obstructive Culprit Lesion
2.3. High-Sensitivity Troponin I
2.4. Outcomes
2.5. Statical Analysis
3. Results
3.1. Baseline Characteristics According to Age
3.2. In-Hospital Complications Presented According to Age
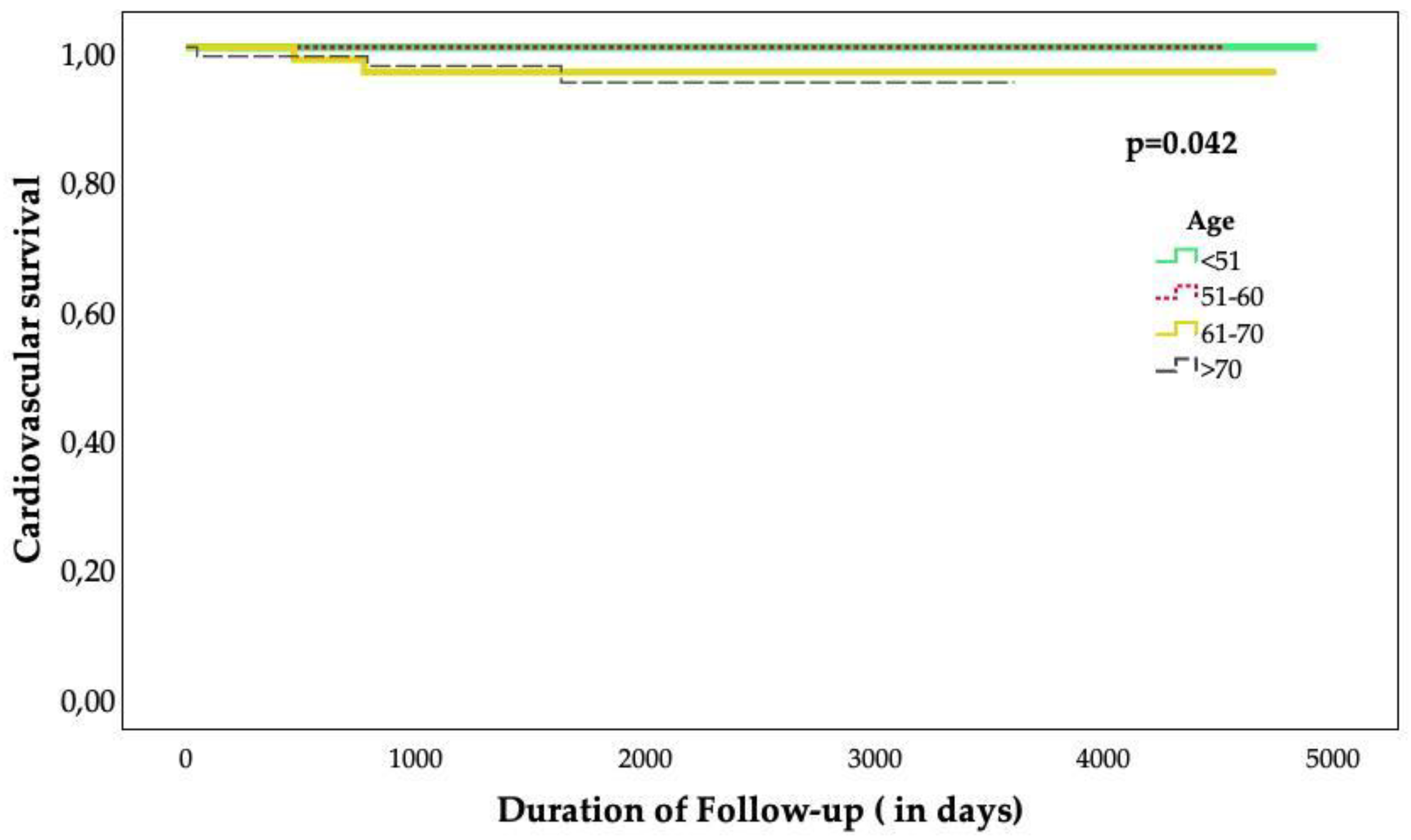
3.3. LVEF and Clinical Outcomes Presented According to Age at Long-Term Follow-Up
4. Discussion
5. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tamis-Holland, J.E.; Jneid, H.; Reynolds, H.R.; Agewall, S.; Brilakis, E.S.; Brown, T.M.; Lerman, A.; Cushman, M.; Kumbhani, D.J.; Arslanian-Engoren, C.; et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation 2019, 139, e891–e908. [Google Scholar] [CrossRef] [PubMed]
- Scalone, G.; Niccoli, G.; Crea, F. Editor’s Choice- Pathophysiology, diagnosis and management of MINOCA: An update. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, D. Myocardial Infarction With Nonobstructive Coronary Arteries: A Call for Individualized Treatment. J. Am. Heart Assoc. 2019, 8, e013361. [Google Scholar] [CrossRef] [PubMed]
- Choo, E.H.; Chang, K.; Lee, K.Y.; Lee, D.; Kim, J.G.; Ahn, Y.; Kim, Y.J.; Chae, S.C.; Cho, M.C.; Kim, C.J.; et al. Prognosis and Predictors of Mortality in Patients Suffering Myocardial Infarction With Non-Obstructive Coronary Arteries. J. Am. Heart Assoc. 2019, 8, e011990. [Google Scholar] [CrossRef]
- Lindahl, B.; Baron, T.; Erlinge, D.; Hadziosmanovic, N.; Nordenskjold, A.; Gard, A.; Jernberg, T. Medical Therapy for Secondary Prevention and Long-Term Outcome in Patients With Myocardial Infarction With Nonobstructive Coronary Artery Disease. Circulation 2017, 135, 1481–1489. [Google Scholar] [CrossRef]
- Planer, D.; Mehran, R.; Ohman, E.M.; White, H.D.; Newman, J.D.; Xu, K.; Stone, G.W. Prognosis of patients with non-ST-segment-elevation myocardial infarction and nonobstructive coronary artery disease: Propensity-matched analysis from the Acute Catheterization and Urgent Intervention Triage Strategy trial. Circ. Cardiovasc. Interv. 2014, 7, 285–293. [Google Scholar] [CrossRef]
- Armillotta, M.; Amicone, S.; Bergamaschi, L.; Angeli, F.; Rinaldi, A.; Paolisso, P.; Stefanizzi, A.; Sansonetti, A.; Impellizzeri, A.; Bodega, F.; et al. Predictive value of Killip classification in MINOCA patients. Eur. J. Intern. Med. 2023, 117, 57–65. [Google Scholar] [CrossRef]
- Abumayyaleh, M.; El-Battrawy, I.; Kummer, M.; Pilsinger, C.; Sattler, K.; Kuschyk, J.; Aweimer, A.; Mugge, A.; Borggrefe, M.; Akin, I. Comparison of the prognosis and outcome of heart failure with reduced ejection fraction patients treated with sacubitril/valsartan according to age. Future Cardiol. 2021, 17, 1131–1142. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Agewall, S.; Beltrame, J.F.; Reynolds, H.R.; Niessner, A.; Rosano, G.; Caforio, A.L.; De Caterina, R.; Zimarino, M.; Roffi, M.; Kjeldsen, K.; et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur. Heart J. 2017, 38, 143–153. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, N.A.; Neumann, J.T.; Ojeda, F.; Giannitsis, E.; Spanuth, E.; Blankenberg, S.; Westermann, D.; Zeller, T. Diagnostic Evaluation of a High-Sensitivity Troponin I Point-of-Care Assay. Clin. Chem. 2019, 65, 1592–1601. [Google Scholar] [CrossRef] [PubMed]
- Wildi, K.; Nelles, B.; Twerenbold, R.; Rubini Gimenez, M.; Reichlin, T.; Singeisen, H.; Druey, S.; Haaf, P.; Sabti, Z.; Hillinger, P.; et al. Safety and efficacy of the 0 h/3 h protocol for rapid rule out of myocardial infarction. Am. Heart J. 2016, 181, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthelemy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Lakatta, E.G. Age-associated cardiovascular changes in health: Impact on cardiovascular disease in older persons. Heart Fail. Rev. 2002, 7, 29–49. [Google Scholar] [CrossRef]
- Gabaldon-Perez, A.; Bonanad, C.; Garcia-Blas, S.; Marcos-Garces, V.; D’Gregorio, J.G.; Fernandez-Cisnal, A.; Valero, E.; Minana, G.; Merenciano-Gonzalez, H.; Mollar, A.; et al. Clinical Predictors and Prognosis of Myocardial Infarction with Non-Obstructive Coronary Arteries (MINOCA) without ST-Segment Elevation in Older Adults. J. Clin. Med. 2023, 12, 1181. [Google Scholar] [CrossRef]
- Pasupathy, S.; Air, T.; Dreyer, R.P.; Tavella, R.; Beltrame, J.F. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation 2015, 131, 861–870. [Google Scholar] [CrossRef]
- Canton, L.; Fedele, D.; Bergamaschi, L.; Foa, A.; Di Iuorio, O.; Tattilo, F.P.; Rinaldi, A.; Angeli, F.; Armillotta, M.; Sansonetti, A.; et al. Sex- and age-related differences in outcomes of patients with acute myocardial infarction: MINOCA vs. MIOCA. Eur. Heart J. Acute Cardiovasc. Care 2023, 12, 604–614. [Google Scholar] [CrossRef]
- Safdar, B.; Spatz, E.S.; Dreyer, R.P.; Beltrame, J.F.; Lichtman, J.H.; Spertus, J.A.; Reynolds, H.R.; Geda, M.; Bueno, H.; Dziura, J.D.; et al. Presentation, Clinical Profile, and Prognosis of Young Patients With Myocardial Infarction With Nonobstructive Coronary Arteries (MINOCA): Results From the VIRGO Study. J. Am. Heart Assoc. 2018, 7, e009174. [Google Scholar] [CrossRef]
- Pais, J.L.; Izquierdo Coronel, B.; Galan Gil, D.; Espinosa Pascual, M.J.; Martinez Peredo, C.G.; Awamleh Garcia, P.; Gorriz Magana, J.; Mata Caballero, R.; Fraile Sanz, A.; Muniz, J.; et al. Psycho-emotional disorders as incoming risk factors for myocardial infarction with non-obstructive coronary arteries. Cardiol. J. 2018, 25, 24–31. [Google Scholar] [CrossRef]
- Lopez-Pais, J.; Izquierdo Coronel, B.; Raposeiras-Roubin, S.; Alvarez Rodriguez, L.; Vedia, O.; Almendro-Delia, M.; Sionis, A.; Martin-Garcia, A.C.; Uribarri, A.; Blanco, E.; et al. Differences Between Takotsubo and the Working Diagnosis of Myocardial Infarction With Nonobstructive Coronary Arteries. Front. Cardiovasc. Med. 2022, 9, 742010. [Google Scholar] [CrossRef] [PubMed]
- He, C.J.; Zhu, C.Y.; Han, B.; Hu, H.Z.; Wang, S.J.; Zhai, C.L.; Hu, H.L. Association between anxiety and clinical outcomes in Chinese patients with myocardial infarction in the absence of obstructive coronary artery disease. Clin. Cardiol. 2020, 43, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Cammann, V.L.; Szawan, K.A.; Stahli, B.E.; Kato, K.; Budnik, M.; Wischnewsky, M.; Dreiding, S.; Levinson, R.A.; Di Vece, D.; Gili, S.; et al. Age-Related Variations in Takotsubo Syndrome. J. Am. Coll. Cardiol. 2020, 75, 1869–1877. [Google Scholar] [CrossRef] [PubMed]
- Tornvall, P.; Gerbaud, E.; Behaghel, A.; Chopard, R.; Collste, O.; Laraudogoitia, E.; Leurent, G.; Meneveau, N.; Montaudon, M.; Perez-David, E.; et al. Myocarditis or “true” infarction by cardiac magnetic resonance in patients with a clinical diagnosis of myocardial infarction without obstructive coronary disease: A meta-analysis of individual patient data. Atherosclerosis 2015, 241, 87–91. [Google Scholar] [CrossRef]
- Pizzi, C.; Xhyheri, B.; Costa, G.M.; Faustino, M.; Flacco, M.E.; Gualano, M.R.; Fragassi, G.; Grigioni, F.; Manzoli, L. Nonobstructive Versus Obstructive Coronary Artery Disease in Acute Coronary Syndrome: A Meta-Analysis. J. Am. Heart Assoc. 2016, 5, e004185. [Google Scholar] [CrossRef]
- Almeida, A.G. MINOCA and INOCA: Role in Heart Failure. Curr. Heart Fail. Rep. 2023, 20, 139–150. [Google Scholar] [CrossRef]
- Abdu, F.A.; Liu, L.; Mohammed, A.Q.; Luo, Y.; Xu, S.; Auckle, R.; Xu, Y.; Che, W. Myocardial infarction with non-obstructive coronary arteries (MINOCA) in Chinese patients: Clinical features, treatment and 1 year follow-up. Int. J. Cardiol. 2019, 287, 27–31. [Google Scholar] [CrossRef]
- Ishii, M.; Kaikita, K.; Sakamoto, K.; Seki, T.; Kawakami, K.; Nakai, M.; Sumita, Y.; Nishimura, K.; Miyamoto, Y.; Noguchi, T.; et al. Characteristics and in-hospital mortality of patients with myocardial infarction in the absence of obstructive coronary artery disease in super-aging society. Int. J. Cardiol. 2020, 301, 108–113. [Google Scholar] [CrossRef]
- Quesada, O.; Yildiz, M.; Henry, T.D.; Okeson, B.K.; Chambers, J.; Shah, A.; Stanberry, L.; Volpenhein, L.; Aziz, D.; Lantz, R.; et al. Characteristics and Long-term Mortality in Patients with ST-Segment Elevation Myocardial Infarction with Non-Obstructive Coronary Arteries (STE-MINOCA): A High Risk Cohort. medRxiv 2023. [Google Scholar] [CrossRef]
- Pelliccia, F.; Pasceri, V.; Niccoli, G.; Tanzilli, G.; Speciale, G.; Gaudio, C.; Crea, F.; Camici, P.G. Predictors of Mortality in Myocardial Infarction and Nonobstructed Coronary Arteries: A Systematic Review and Meta-Regression. Am. J. Med. 2020, 133, 73–83.e4. [Google Scholar] [CrossRef]


| Variables | All Patients n = 373 | <51 n = 78 | 51–60 n = 72 | 61–70 n = 81 | >70 n = 142 | p Value |
|---|---|---|---|---|---|---|
| Age—years, mean ± SD | 63 ± 15.6 | 40 ± 9.3 | 56 ± 3 | 65 ± 3 | 78 ± 5 | <0.001 |
| Male—n (%) | 185 (49.6) | 55 (70.5) | 42 (58.3) | 36 (44.4) | 52 (36.6) | <0.001 |
| BMI—kg/m2, mean ± SD | 27.6 ± 5.6 | 27.8 ± 6 | 28.4 ± 6 | 27.3 ± 5 | 27.3 ± 5 | 0.502 |
| Duration of hospitalization—days, mean ± SD | 10 ± 8.5 | 8 ± 5 | 10.2 ± 8 | 11 ± 12 | 10.7 ± 8 | 0.060 |
| Symptoms—n (%) | ||||||
| Angina pectoris | 226 (61.6) | 55 (71.4) | 41 (58.6) | 49 (60.5) | 81 (58.3) | 0.252 |
| Dyspnea | 164 (44.4) | 18 (23.4) | 34 (47.2) | 39 (48.2) | 73 (52.5) | <0.001 |
| Palpations | 45 (12.3) | 12 (15.6) | 7 (10) | 9 (11.1) | 17 (12.2) | 0.750 |
| Clinic parameter, mean ± SD | ||||||
| Systolic BP, mmHg | 146.6 ± 64.4 | 137.1 ± 26 | 146.2 ± 31 | 154.3 ± 126 | 147 ± 26 | 0.553 |
| Diastolic BP, mmHg | 84.8 ± 18.1 | 58.7 ± 17 | 90.9 ± 24 | 81.4 ± 14 | 83.2 ± 17 | 0.026 |
| Heart rate, bpm | 89.8 ± 28.6 | 88.3 ± 24 | 93.8 ± 27 | 88.1 ± 33 | 89.6 ± 29 | 0.609 |
| ECG—n (%) | ||||||
| ST elevation | 55 (14.8) | 25 (32.1) | 7 (9.7) | 7 (8.6) | 16 (11.3) | <0.001 |
| Inversed T-Waves | 183 (49.2) | 27 (34.6) | 33 (45.8) | 44 (54.3) | 79 (56) | 0.015 |
| Medical history—n (%) | ||||||
| Current Smoking | 85 (23.1) | 31 (40.3) | 18 (25.4) | 25 (30.9) | 11 (7.9) | <0.001 |
| Obesity | 112 (30) | 23 (29.5) | 24 (34.3) | 25 (30.9) | 40 (28.2) | 0.887 |
| Arterial hypertension | 253 (68.2) | 33 (42.3) | 36 (51.4) | 66 (81.5) | 118 (83.1) | <0.001 |
| Dyslipidemia | 99 (26.6) | 16 (20.5) | 19 (26.8) | 22 (27.2) | 42 (29.6) | 0.547 |
| Diabetes Mellitus | 65 (17.5) | 8 (10.3) | 10 (14.1) | 13 (16.1) | 34 (23.9) | 0.054 |
| COPD | 47 (12.6) | 0 (0) | 8 (11.3) | 18 (22.2) | 21 (14.8) | <0.001 |
| Bronchial Asthma | 33 (8.9) | 7 (9) | 10 (14.1) | 5 (6.2) | 11 (7.7) | 0.344 |
| Malignancy | 47 (12.7) | 2 (2.6) | 2 (2.9) | 12 (15) | 31 (21.8) | <0.001 |
| Kidney disease | 53 (14.3) | 5 (6.4) | 5 (7) | 12 (14.8) | 31 (21.8) | 0.003 |
| Neurological disease | 90 (24.3) | 11 (14.1) | 12 (17.1) | 19 (23.5) | 48 (33.8) | 0.004 |
| Autoimmune disease | 17 (4.6) | 5 (6.4) | 2 (2.8) | 3 (3.7) | 7 (5) | 0.733 |
| Psychiatric disease | 39 (10.5) | 6 (7.7) | 10 (14.1) | 14 (17.3) | 9 (6.3) | 0.041 |
| Pacemaker | 14 (3.8) | 0 (0) | 1 (1.4) | 2 (2.5) | 11 (7.8) | 0.012 |
| History of Malignant cardiac arrhythmias *—n (%) | 8 (2.2) | 0 (0) | 0 (0) | 2 (2.5) | 6 (7.8) | 0.101 |
| Bradycardiac arrhythmias | 6 (1.6) | 0 (0) | 0 (0) | 1 (1.2) | 5 (3.6) | 0.123 |
| -AV block 2 Mobitz | 3 (0.8) | 0 (0) | 0 (0) | 1 (1.2) | 2 (1.4) | 0.567 |
| -AV block 3 | 3 (0.8) | 0 (0) | 0 (0) | 0 (0) | 3 (2.1) | 0.179 |
| -Asystole | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Ventricular arrhythmias | 1 (0.3) | 0 (0) | 0 (0) | 1 (1.2) | 0 (0) | 0.311 |
| -sustained | 1 (0.3) | 0 (0) | 0 (0) | 1 (1.2) | 0 (0) | 0.311 |
| -non-sustained | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| -ventricular fibrillation | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Torsades de pointes | 1 (0.3) | 0 (0) | 0 (0) | 0 (0) | 1 (0.7) | 0.658 |
| Atrial fibrillation * | 57 (15.4) | 1 (1.3) | 6 (8.6) | 13 (16.1) | 37 (26.1) | <0.001 |
| Laboratory values, mean ± SD | ||||||
| Troponin (µg/L) | 2.1 ± 8.4 | 2.8 ± 5.8 | 2.7 ± 12.1 | 1.3 ± 7.3 | 1 ± 5 | 0.234 |
| Creatin Phosphokinase (U/L) | 288.6 ± 548.9 | 352.2 ± 407 | 427.4 ± 943 | 235.4 ± 340 | 215 ± 418 | 0.030 |
| BNP (pg/ml) | 433.5 ± 1004.5 | 175 ± 390 | 432 ± 1286 | 560 ± 987 | 514 ± 1070 | 0.181 |
| Creatinine (mg/dl) | 3.3 ± 30.9 | 0.9 ± 0.2 | 12.9 ± 70.6 | 1.1 ± 0.4 | 1.1 ± 0.4 | 0.040 |
| TSH (mU/l) | 2 ± 1.7 | 2 ± 1.2 | 2.3 ± 2.4 | 1.8 ± 1.8 | 1.9 ± 1.4 | 0.986 |
| fT3 (pmol/l) | 5.2 ± 1 | 5.5 ± 1 | 5.2 ± 1 | 5.2 ± 1.1 | 4.8 ± 0.9 | 0.861 |
| fT4 (ng/l) | 10.6 ± 2.8 | 10.2 ± 1.8 | 9.1 ± 1.5 | 10.6 ± 3.1 | 12 ± 3.3 | 0.941 |
| Echocardiography data, n (%) | ||||||
| LVEF %, (on admission), mean ± SD | 36.9 ± 25.7 | 46.7 ± 23 | 37.5 ± 25 | 34.4 ± 27 | 32.6 ± 25 | <0.001 |
| -LVEF > 50 % | 170 (66.9) | 52 (82.5) | 29 (60.4) | 35 (67.3) | 54 (59.3) | 0.016 |
| -LVEF 40–49 % | 31 (12.2) | 3 (4.8) | 9 (18.8) | 5 (9.6) | 14 (15.4) | 0.096 |
| -LVEF < 40 % | 52 (20.5) | 8 (12.7) | 10 (20.8) | 11 (21.2) | 23 (25.3) | 0.305 |
| Left ventricular hypertrophy | 103 (29.1) | 15 (32.5) | 20 (30.3) | 23 (29.5) | 45 (33.8) | 0.177 |
| Tricuspid valve regurgitation | 89 (24.2) | 7 (9) | 15 (21.4) | 21 (26.3) | 46 (32.9) | 0.001 |
| -mild | 63 (17.1) | 6 (7.7) | 11 (15.7) | 14 (17.5) | 32 (22.9) | 0.041 |
| -moderate | 23 (6.3) | 1 (1.3) | 4 (5.7) | 6 (7.5) | 12 (8.6) | 0.187 |
| -severe | 3 (0.8) | 0 (0) | 0 (0) | 1 (1.3) | 2 (1.4) | 0.564 |
| Mitral valve regurgitation | 106 (28.8) | 7 (9) | 16 (22.9) | 21 (26.3) | 62 (44.3) | <0.001 |
| -mild | 77 (20.9) | 6 (7.7) | 12 (17.1) | 17 (21.3) | 42 (29.8) | 0.001 |
| -moderate | 19 (5.2) | 1 (1.3) | 2 (2.9) | 3 (3.8) | 13 (9.2) | 0.041 |
| -severe | 10 (2.7) | 0 (0) | 2 (2.9) | 1 (1.3) | 7 (5) | 0.137 |
| Aortic valve regurgitation | 39 (10.6) | 0 (0) | 7 (10) | 3 (3.8) | 29 (20.7) | <0.001 |
| -mild | 31 (8.4) | 0 (0) | 5 (7.1) | 3 (3.8) | 23 (16.4) | <0.001 |
| -moderate | 4 (1.1) | 0 (0) | 2 (2.8) | 0 (0) | 2 (1.4) | 0.271 |
| -severe | 4 (1.1) | 0 (0) | 0 (0) | 0 (0) | 4 (2.9) | 0.086 |
| Drugs on admission, n (%) | ||||||
| ß-Blocker | 131 (35.2) | 8 (10.3) | 20 (28.2) | 32 (39.5) | 71 (50.7) | <0.001 |
| ACE inhibitor | 121 (32.6) | 14 (17.9) | 17 (23.9) | 35 (43.2) | 55 (39) | <0.001 |
| Sartans | 57 (15.3) | 4 (5.1) | 9 (12.7) | 11 (13.6) | 33 (23.6) | 0.003 |
| Ca-Blocker | 74 (19.9) | 6 (7.7) | 8 (11.3) | 16 (19.8) | 44 (31.4) | <0.001 |
| Diuretics | 101 (27.2) | 8 (10.3) | 14 (19.7) | 16 (19.8) | 63 (45) | <0.001 |
| Statin | 281 (76.8) | 78 (27.1) | 75 (25.2) | 61 (21.3) | 41 (18.1) | <0.001 |
| Anticoagulants ** | 58 (15.6) | 1 (1.3) | 2 (2.8) | 17 (21) | 38 (27.1) | <0.001 |
| Aspirin | 79 (21.2) | 7 (9) | 12 (16.9) | 23 (28.4) | 37 (26.4) | 0.006 |
| Clopidogrel | 18 (4.8) | 2 (2.6) | 2 (2.8) | 6 (7.4) | 8 (5.7) | 0.416 |
| Prasugrel | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Antiarrhythmics *** | 10 (2.7) | 0 (0) | 3 (4.2) | 3 (3.7) | 4 (2.9) | 0.375 |
| Variables | All Patients n = 373 | <51 n = 78 | 51–60 n = 72 | 61–70 n = 81 | >70 n = 142 | p Value |
|---|---|---|---|---|---|---|
| ß-Blocker, n (%) | 270 (72.4) | 50 (64.1) | 54 (75) | 63 (77.8) | 103 (72.5) | 0.252 |
| ACE inhibitor, n (%) | 224 (60.1) | 46 (59) | 47 (65.3) | 51 (63) | 80 (56.3) | 0.584 |
| Sartans, n (%) | 62 (16.6) | 6 (7.7) | 10 (13.9) | 15 (18.5) | 31 (21.8) | 0.049 |
| Ca Blocker, n (%) | 100 (26.8) | 12 (15.4) | 15 (20.8) | 24 (29.6) | 49 (34.5) | 0.011 |
| Diuretics, n (%) | 166 (44.5) | 13 (16.7) | 29 (40.3) | 34 (42) | 90 (63.4) | <0.001 |
| Statin, n (%) | 206 (55.2) | 21 (26.9) | 32 (44.4) | 41 (50.6) | 73 (51.4) | <0.001 |
| Anticoagulants *, n (%) | 104 (27.9) | 3 (3.9) | 17 (23.6) | 25 (30.9) | 59 (41.5) | <0.001 |
| Aspirin, n (%) | 175 (46.9) | 27 (34.6) | 32 (44.4) | 46 (56.8) | 70 (49.3) | 0.038 |
| Clopidogrel, n (%) | 68 (18.2) | 14 (18) | 11 (15.3) | 20 (24.7) | 23 (16.2) | 0.381 |
| Prasugrel, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Antiarrhythmics **, n (%) | 26 (7) | 1 (1.3) | 7 (9.7) | 5 (6.2) | 13 (9.2) | 0.119 |
| Variables | All Patients n = 373 | <51 n = 78 | 51–60 n = 72 | 61–70 n = 81 | >70 n = 142 | p Value |
|---|---|---|---|---|---|---|
| Adverse event, n (%) | 132 (35.5) | 12 (15.4) | 26 (36.1) | 27 (33.3) | 67 (47.2) | <0.001 |
| CPR | 7 (1.9) | 0 (0) | 3 (4.2) | 1 (1.2) | 3 (2.1) | 0.290 |
| Left ventricular thrombus | 3 (0.8) | 1 (1.3) | 1 (1.4) | 0 (0) | 1 (0.7) | 0.754 |
| Thromboembolic event | 3 (0.8) | 0 (0) | 0 (0) | 1 (1.2) | 2 (1.4) | 0.564 |
| Pulmonary edema | 9 (2.7) | 1 (1.3) | 2 (2.8) | 2 (2.5) | 4 (2.8) | 0.906 |
| Cardiogenic shock | 9 (2.7) | 1 (1.3) | 2 (2.8) | 2 (2.5) | 4 (2.8) | 0.906 |
| Invasive ventilation | 29 (7.8) | 4 (5.1) | 8 (11.1) | 6 (7.4) | 11 (7.8) | 0.597 |
| Non-invasive ventilation | 11 (3) | 0 (0) | 1 (1.4) | 4 (4.9) | 6 (4.3) | 0.180 |
| Stroke | 1 (0.3) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 0.243 |
| Malignant cardiac arrhythmias *, n (%) (on admission/in hospital) | 39 (10.5) | 8 (10.3) | 11 (15.3) | 5 (6.2) | 15 (10.6) | 0.339 |
| Bradycardiac arrhythmias | 13 (3.5) | 3 (3.8) | 1 (1.4) | 1 (1.2) | 8 (5.6) | 0.248 |
| -AV block 2 Mobitz | 3 (0.8) | 2 (2.6) | 0 (0) | 0 (0) | 1 (0.7) | 0.234 |
| -AV block 3 | 1 (0.3) | 0 (0) | 0 (0) | 0 (0) | 1 (0.7) | 0.655 |
| -Asystole | 10 (2.7) | 2 (2.6) | 1 (1.4) | 1 (1.2) | 6 (4.2) | 0.494 |
| Ventricular arrhythmias | 14 (3.8) | 2 (2.6) | 5 (6.9) | 4 (4.9) | 5 (3.5) | 0.438 |
| -sustained | 8 (2.2) | 2 (2.6) | 2 (2.8) | 0 (0) | 4 (2.8) | 0.524 |
| -non-sustained | 6 (1.6) | 0 (0) | 4 (5.6) | 1 (1.3) | 1 (0.7) | 0.027 |
| -ventricular fibrillation | 16 (4.3) | 3 (3.8) | 7 (9.7) | 3 (3.7) | 3 (2.1) | 0.075 |
| Torsades de pointes | 2 (0.5) | 0 (0) | 1 (1.4) | 0 (0) | 1 (0.7) | 0.598 |
| Supraventricular arrhythmias *, n (%) | 85 (22.8) | 3 (3.8) | 11 (15.3) | 19 (23.5) | 52 (36.6) | <0.001 |
| Atrial fibrillation | 77 (20.6) | 3 (3.8) | 8 (11.1) | 15 (18.5) | 51 (35.9) | <0.001 |
| -first appearance | 43 (11.5) | 3 (3.8) | 5 (6.9) | 6 (7.4) | 29 (20.4) | <0.001 |
| -recurrens | 34 (9.1) | 0 (0) | 3 (4.2) | 9 (11.1) | 22 (15.5) | <0.001 |
| Atrial flutter | 9 (2.4) | 0 (0) | 3 (4.2) | 4 (4.9) | 2 (1.4) | 0.129 |
| -first appereance | 9 (2.4) | 0 (0) | 3 (4.2) | 4 (4.9) | 2 (1.4) | 0.129 |
| -recurrens | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| In-hospital death, n (%) | 10 (2.7) | 0 (0) | 3 (4.2) | 2 (2.5) | 5 (3.5) | 0.371 |
| Cardiac caused death | 6 (1.6) | 0 (0) | 2 (2.8) | 1 (1.3) | 3 (2.1) | 0.535 |
| Non-cardiac caused death | 4 (1.1) | 0 (0) | 1 (1.4) | 1 (1.3) | 2 (1.4) | 0.783 |
| Variables | All Patients n = 373 | <51 n = 78 | 51–60 n = 72 | 61–70 n = 82 | >70 n = 142 | p Value |
|---|---|---|---|---|---|---|
| FU EF (%), mean ± SD | 49 ± 14.7 | 58.1 ± 11 | 48.4 ± 17 | 42.3 ± 14 | 43.1 ± 12 | <0.001 |
| -LVEF ≥ 50 %, n (%) | 184 (49.3) | 33 (42.3) | 21 (30) | 15 (19.5) | 31 (23) | 0.005 |
| -LVEF 40-49 %, n (%) | 100 (27.8) | 3 (3.9) | 7 (10) | 5 (6.5) | 12 (8.9) | 0.457 |
| -LVEF < 40 %, n (%) | 27 (7.5) | 5 (6.4) | 10 (14.3) | 10 (13) | 25 (18.5) | 0.106 |
| Cardioversion, n (%) | 50 (13.9) | 5 (6.4) | 14 (19.4) | 17 (21.3) | 28 (19.7) | 0.042 |
| Pacemaker, n (%) | 64 (17.2) | 2 (2.6) | 8 (11.1) | 5 (6.2) | 9 (6.3) | 0.208 |
| LifeVest, n (%) | 24 (6.5) | 5 (6.4) | 4 (5.6) | 1 (1.2) | 2 (1.4) | 0.097 |
| All Patients n = 288 | <51 n = 62 | 51–60 n = 51 | 61–70 n = 61 | >70 n = 114 | p Value | |
|---|---|---|---|---|---|---|
| Adverse event, n (%) | 100 (34.8) | 4 (6.5) | 11 (21.6) | 16 (26.2) | 69 (61.1) | 0.126 |
| Stroke | 10 (4.2) | 2 (3.9) | 1 (2.1) | 1 (2) | 6 (6.8) | 0.797 |
| Thromboembolic event | 6 (2.5) | 2 (3.2) | 0 (0) | 1 (1.9) | 3 (4) | 0.385 |
| Recurrence of Troponin-positive with non-obstructive CAD | 3 (1.3) | 0 (0) | 1 (2.1) | 1 (1.9) | 1 (1.4) | 0.981 |
| Cardiac arrest | 4 (1.7) | 0 (0) | 1 (2.1) | 1 (1.9) | 2 (2.7) | 0.900 |
| Percutaneous coronary intervention | 17 (7.2) | 2 (3.2) | 3 (6.3) | 3 (5.7) | 9 (12.3) | 0.352 |
| Death, n (%) | 69 (24.1) | 0 (0) | 6 (11.8) | 12 (20) | 51 (45.1) | 0.067 |
| -cardiac caused death | 5 (2.1) | 0 (0) | 0 (0) | 2 (3.9) | 3 (4.2) | 0.042 |
| -non-cardiac caused death | 12 (5.1) | 0 (0) | 4 (8.2) | 2 (3.9) | 6 (8.5) | 0.075 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abumayyaleh, M.; Schlettert, C.; Materzok, D.; Mügge, A.; Hamdani, N.; Akin, I.; Aweimer, A.; El-Battrawy, I. Age Variation in Patients with Troponin Level Elevation Without Obstructive Culprit Lesion or Suspected Myocardial Infarction with Non-Obstructive Coronary Arteries—Long-Term Data Covering over Decade. J. Clin. Med. 2024, 13, 7685. https://doi.org/10.3390/jcm13247685
Abumayyaleh M, Schlettert C, Materzok D, Mügge A, Hamdani N, Akin I, Aweimer A, El-Battrawy I. Age Variation in Patients with Troponin Level Elevation Without Obstructive Culprit Lesion or Suspected Myocardial Infarction with Non-Obstructive Coronary Arteries—Long-Term Data Covering over Decade. Journal of Clinical Medicine. 2024; 13(24):7685. https://doi.org/10.3390/jcm13247685
Chicago/Turabian StyleAbumayyaleh, Mohammad, Clara Schlettert, Daniel Materzok, Andreas Mügge, Nazha Hamdani, Ibrahim Akin, Assem Aweimer, and Ibrahim El-Battrawy. 2024. "Age Variation in Patients with Troponin Level Elevation Without Obstructive Culprit Lesion or Suspected Myocardial Infarction with Non-Obstructive Coronary Arteries—Long-Term Data Covering over Decade" Journal of Clinical Medicine 13, no. 24: 7685. https://doi.org/10.3390/jcm13247685
APA StyleAbumayyaleh, M., Schlettert, C., Materzok, D., Mügge, A., Hamdani, N., Akin, I., Aweimer, A., & El-Battrawy, I. (2024). Age Variation in Patients with Troponin Level Elevation Without Obstructive Culprit Lesion or Suspected Myocardial Infarction with Non-Obstructive Coronary Arteries—Long-Term Data Covering over Decade. Journal of Clinical Medicine, 13(24), 7685. https://doi.org/10.3390/jcm13247685





