Using Virtual Reality Pablo Gaming in the Post-Operative Rehabilitation of Breast Cancer Patients: Randomized Controlled Trial
Abstract
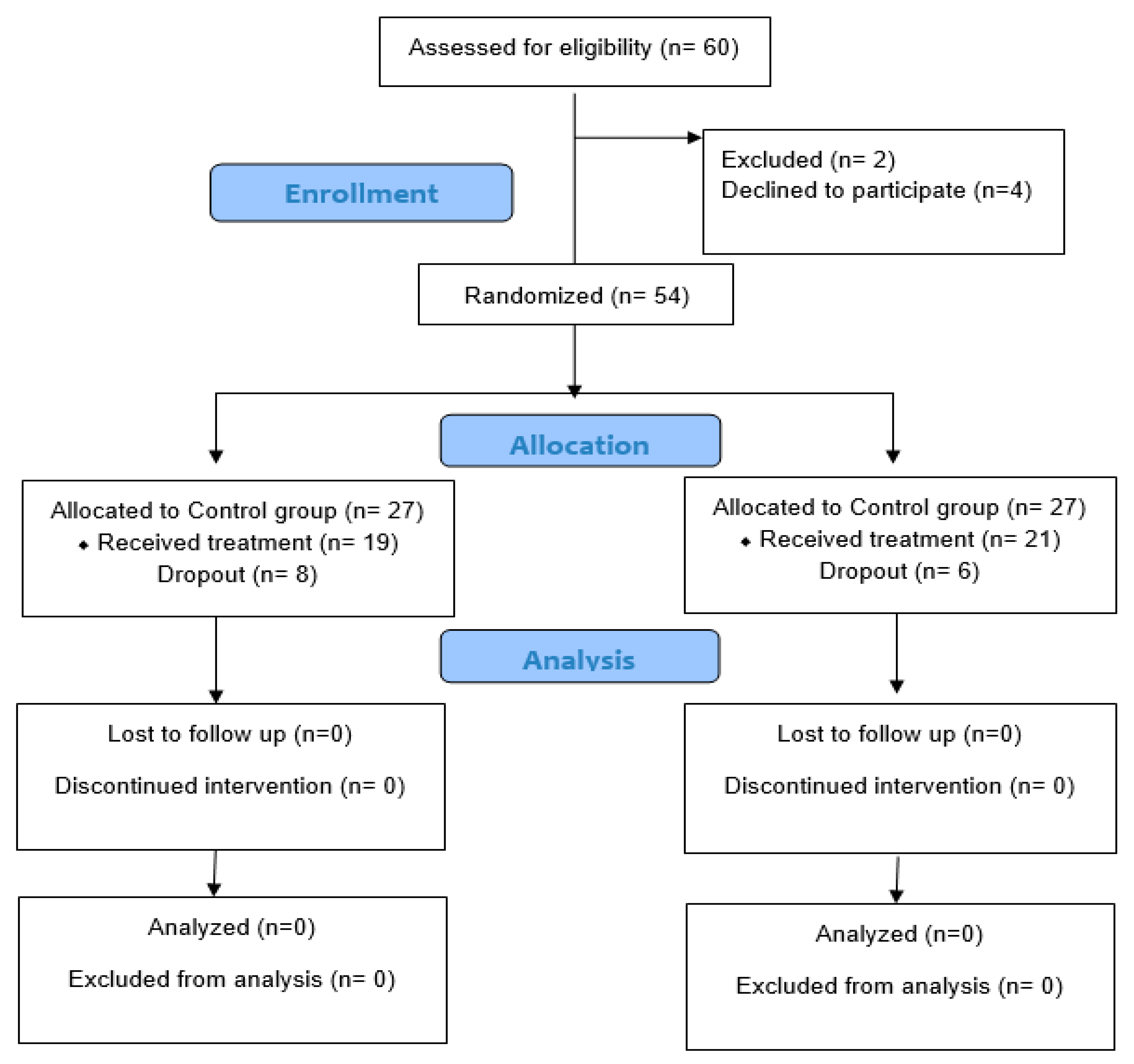
1. Introduction
2. Methods
2.1. Participants
2.2. Sample Size
2.3. Interventions
2.3.1. Exercises
2.3.2. Intermittent Compression
2.3.3. Pablo© Handle Training
2.4. Outcome Measures
2.4.1. Upper Limb Functioning
2.4.2. Fatigue
2.4.3. Pain Intensity
2.4.4. Activities of Daily Living (ADLs)
2.4.5. Anxiety
2.5. Allocation, Concealment, and Blinding
2.6. Statistical Analysis
3. Results
3.1. Between-Group Comparison
3.2. Within-Group Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buche, H.; Michel, A.; Piccoli, C.; Blanc, N. Contemplating or Acting? Which Immersive Modes Should Be Favored in Virtual Reality During Physiotherapy for Breast Cancer Rehabilitation. Front. Psychol. 2021, 12, 631186. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.B.; Lang, J.J.; Compton, K.; Xu, R.; Acheson, A.R.; Henrikson, H.J.; Kocarnik, J.M.; Penberthy, L.; Aali, A.; Abbas, Q. The global burden of cancer attributable to risk factors, 2010–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022, 400, 563–591. [Google Scholar] [CrossRef] [PubMed]
- Iddrisu, M.; Aziato, L.; Dedey, F. Psychological and physical effects of breast cancer diagnosis and treatment on young Ghanaian women: A qualitative study. BMC Psychiatry 2020, 20, 353. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.K.; Ismail, S. Side effects of chemotherapy among cancer patients in a Malaysian general hospital: Experiences, perceptions and informational needs from clinical pharmacists. Asian Pacific J. Cancer Prev. 2014, 15, 5305–5309. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, P.; Baumann, F.T. Physical Activity, Exercise and Breast Cancer—What Is the Evidence for Rehabilitation, Aftercare, and Survival? A Review. Breast Care 2018, 13, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Fors, E.A.; Bertheussen, G.F.; Thune, I.; Juvet, L.K.; Elvsaas, I.Ø.; Oldervoll, L.; Anker, G.; Falkmer, U.; Lundgren, S.; Leivseth, G. Psychosocial interventions as part of breast cancer rehabilitation programs? Results from a systematic review. Psychooncology 2011, 20, 909–918. [Google Scholar] [CrossRef]
- Hussein, H.M.; Maher, A.; Gabr, M.; Fadulelmulla, I.A.; Aldemery, A.A.; Marzouk, M.; Ragab, M. Systematic review/Meta-analysis Impact of low-level laser therapy on upper limb lymphoedema secondary to breast cancer: A systematic review and meta-analysis. Arch. Med. Sci. 2024, 1–8. [Google Scholar] [CrossRef]
- Ibrahim, A.A.; Gabr Ali, A.M.M.; Fadulelmulla, I.A.; Ragab, M.M.M.; Aldemery, A.A.; Mohamed, A.R.; Dewir, I.M.; Hakami, H.A.; Hussein, H.M. Using Inspiratory Muscle Training to Improve Respiratory Strength, Functional Capacity, Fatigue, and Stress in Breast Cancer Patients Undergoing Surgery. J. Multidiscip. Healthc. 2024, 17, 1931–1941. [Google Scholar] [CrossRef]
- Cipresso, P.; Giglioli, I.A.C.; Raya, M.A.; Riva, G. The past, present, and future of virtual and augmented reality research: A network and cluster analysis of the literature. Front. Psychol. 2018, 9, 2086. [Google Scholar] [CrossRef]
- Karamians, R.; Proffitt, R.; Kline, D.; Gauthier, L.V. Effectiveness of virtual reality-and gaming-based interventions for upper extremity rehabilitation poststroke: A meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 885–896. [Google Scholar] [CrossRef]
- Ayed, I.; Ghazel, A.; Jaume-i-Capo, A.; Moya-Alcover, G.; Varona, J.; Martínez-Bueso, P. Vision-based serious games and virtual reality systems for motor rehabilitation: A review geared toward a research methodology. Int. J. Med. Inform. 2019, 131, 103909. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yu, F.; Shi, D.; Shi, J.; Tian, Z.; Yang, J.; Wang, X.; Jiang, Q. Application of virtual reality technology in clinical medicine. Am. J. Transl. Res. 2017, 9, 3867. [Google Scholar] [PubMed]
- Mouatt, B.; Smith, A.E.; Mellow, M.L.; Parfitt, G.; Smith, R.T.; Stanton, T.R. The Use of Virtual Reality to Influence Motivation, Affect, Enjoyment, and Engagement During Exercise: A Scoping Review. Front. Virtual Real. 2020, 1, 564664. [Google Scholar] [CrossRef]
- Zhang, H.; Xu, H.; Zhang, Z.X.; Zhang, Q. Efficacy of virtual reality-based interventions for patients with breast cancer symptom and rehabilitation management: A systematic review and meta-analysis. BMJ Open 2022, 12, e051808. [Google Scholar] [CrossRef] [PubMed]
- Czech, O.; Siewierska, K.; Krzywińska, A.; Skórniak, J.; Maciejczyk, A.; Matkowski, R.; Szczepańska-Gieracha, J.; Malicka, I. Virtual Therapy Complementary Prehabilitation of Women Diagnosed with Breast Cancer—A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 722. [Google Scholar] [CrossRef]
- Chirico, A.; Maiorano, P.; Indovina, P.; Milanese, C.; Giordano, G.G.; Alivernini, F.; Iodice, G.; Gallo, L.; De Pietro, G.; Lucidi, F.; et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiol. 2020, 235, 5353–5362. [Google Scholar] [CrossRef]
- Feyzioğlu, Ö.; Dinçer, S.; Akan, A.; Algun, Z.C.; Jin, A.A.; Chen, X.X.; Zhang, X.X.; Chen, J. Design and clinical application of rehabilitation VR system for breast cancer patients. Chin. Gen. Pract. 2018, 28, 2987. [Google Scholar]
- Hartwig, M. Fun and evidence-computer based arm rehabilitation with the Pablo Plus System. Prod. Profile 2011, 1, 1–5. [Google Scholar]
- Chaudhary, P.; Hamdani, N.; Sharma, P. The effects of visuomotor training using Pablo System on hand grip strength and wrist movements in adults and elderly. Iran. Rehabil. J. 2019, 17, 215–223. [Google Scholar] [CrossRef]
- Nica, A.S.; Brailescu, C.M.; Scarlet, R.G. Virtual reality as a method for evaluation and therapy after traumatic hand surgery. Annu. Rev. Cybertherapy Telemed. 2013, 191, 48–52. [Google Scholar]
- House, G.; Burdea, G.; Grampurohit, N.; Polistico, K.; Roll, D.; Damiani, F.; Hundal, J.; Demesmin, D. A feasibility study to determine the benefits of upper extremity virtual rehabilitation therapy for coping with chronic pain post-cancer surgery. Br. J. Pain 2016, 10, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.S.; Zeng, D.; Leung, J.H.T.; Ooi, B.S.Y.; Kong, K.T.; Yeo, Y.H.; Goo, J.T.T.; Chia, C.L.K. Measuring upper limb function and patient reported outcomes after major breast cancer surgery: A pilot study in an Asian cohort. BMC Surg. 2020, 20, 108. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, E.B.; Ahmad, M.; Bani Mohammad, E.; Ahmad, M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: A randomized control trial. Palliat. Support. Care 2019, 17, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Tian, Q.; Xu, M.; Yu, L.; Yang, S.; Zhang, W. The Efficacy of Virtual Reality-Based Interventions in Breast Cancer-Related Symptom Management: A Systematic Review and Meta-analysis. Cancer Nurs. 2023, 46, E276–E287. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.D.; Gopman, J.M.; Salzberg, C.A. The evolution of mastectomy surgical technique: From mutilation to medicine. Gland Surg. 2018, 7, 308. [Google Scholar] [CrossRef]
- Kaidar-Person, O.; Offersen, B.V.; Boersma, L.J.; de Ruysscher, D.; Tramm, T.; Kühn, T.; Gentilini, O.; Mátrai, Z.; Poortmans, P. A multidisciplinary view of mastectomy and breast reconstruction: Understanding the challenges. Breast 2021, 56, 42–52. [Google Scholar] [CrossRef]
- Hess, L.M.; Smith, D.; Cui, Z.L.; Montejano, L.; Liepa, A.M.; Schelman, W.; Bowman, L. The relationship between Eastern Cooperative Oncology Group performance status and healthcare resource utilization among patients with advanced or metastatic colorectal, lung or gastric cancer. J. Drug Assess. 2021, 10, 10–17. [Google Scholar] [CrossRef]
- Shao, Y.; Qi, K.; Zhou, Q.-H.; Zhong, D.-S. Intermittent pneumatic compression pump for breast cancer-related lymphedema: A systematic review and meta-analysis of randomized controlled trials. Oncol. Res. Treat. 2014, 37, 170–174. [Google Scholar] [CrossRef]
- Alotaibi, N.M.; Aljadi, S.H.; Alrowayeh, H.N. Reliability, validity and responsiveness of the Arabic version of the Disability of Arm, Shoulder and Hand (DASH-Arabic). Disabil. Rehabil. 2016, 38, 2469–2478. [Google Scholar] [CrossRef]
- Harrington, S.; Michener, L.A.; Kendig, T.; Miale, S.; George, S.Z. Patient-reported upper extremity outcome measures used in breast cancer survivors: A systematic review. Arch. Phys. Med. Rehabil. 2014, 95, 153–162. [Google Scholar] [CrossRef]
- Smets, E.M.A.; Garssen, B.; de Bonke, B.; De Haes, J. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J. Psychosom. Res. 1995, 39, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. STOP, THAT and One Hundred Other Sleep Scales; Springer: Berlin/Heidelberg, Germany, 2012; pp. 1–406. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. JAAOS Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P. The validity and reliability of pain measures in adults with cancer. J. Pain 2003, 4, 2–21. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Barros, V.; Bassi-Dibai, D.; Guedes, C.L.R.; Morais, D.N.; Coutinho, S.M.; de Oliveira Simões, G.; Mendes, L.P.; da Cunha Leal, P.; Dibai-Filho, A.V. Barthel Index is a valid and reliable tool to measure the functional independence of cancer patients in palliative care. BMC Palliat. Care 2022, 21, 124. [Google Scholar] [CrossRef]
- Morishima, T.; Sato, A.; Nakata, K.; Matsumoto, Y.; Koeda, N.; Shimada, H.; Maruhama, T.; Matsuki, D.; Miyashiro, I. Barthel Index-based functional status as a prognostic factor in young and middle-aged adults with newly diagnosed gastric, colorectal and lung cancer: A multicentre retrospective cohort study. BMJ Open 2021, 11, e046681. [Google Scholar] [CrossRef]
- Julian, L.J. Measures of anxiety: State-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and Hospital anxiety and Depression scale-anxiety (HADS-A). Arthritis Care Res. 2011, 63, S467–S472. [Google Scholar] [CrossRef]
- Beikmoradi, A.; Najafi, F.; Roshanaei, G.; Esmaeil, Z.P.; Khatibian, M.; Ahmadi, A. Acupressure and anxiety in cancer patients. Iran. Red Crescent Med. J. 2015, 17, e25919. [Google Scholar] [CrossRef]
- Stein, J.; Bishop, L.; Gillen, G.; Helbok, R. Robot-assisted exercise for hand weakness after stroke: A pilot study. Am. J. Phys. Med. Rehabil. 2011, 90, 887–894. [Google Scholar] [CrossRef]
- Burdea, G.C.; Coiffet, P. Virtual Reality Technology; John Wiley & Sons: Hoboken, NJ, USA, 2003; ISBN 0471360899. [Google Scholar]
- Feyzioğlu, Ö.; Dinçer, S.; Akan, A.; Algun, Z.C. Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery? Support. Care Cancer 2020, 28, 4295–4303. [Google Scholar] [CrossRef]
- Atef, D.; Elkeblawy, M.M.; El-Sebaie, A.; Abouelnaga, W.A.I. A quasi-randomized clinical trial: Virtual reality versus proprioceptive neuromuscular facilitation for postmastectomy lymphedema. J. Egypt. Natl. Cancer Inst. 2020, 32, 29. [Google Scholar] [CrossRef]
- Chirico, A.; Lucidi, F.; De Laurentiis, M.; Milanese, C.; Napoli, A.; Giordano, A. Virtual reality in health system: Beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J. Cell. Physiol. 2016, 231, 275–287. [Google Scholar] [CrossRef] [PubMed]
| PG | CG | MD | t-Value | p-Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||||
| Age (years) | 47 ± 3.94 | 48 ± 4.60 | −1 | −0.56 | 0.57 | |
| BMI (kg/m2) | 28.05 ± 3.04 | 28.80 ± 2.84 | −0.75 | −0.81 | 0.42 | |
| Type of surgery, n (%) | ||||||
| Radical mastectomy | 8 (38%) | 5 (26%) | χ2 = 0.63 | 0.43 | ||
| Modified radical mastectomy | 13 (62%) | 14 (74%) | ||||
| Tumor stage, n (%) | ||||||
| Stage I | 11 (52%) | 12 (63%) | χ2 = 0.47 | 0.49 | ||
| Stage II | 10 (48%) | 7 (37%) | ||||
| lymph node involvement, n (%) | ||||||
| N0 | 9 (43%) | 11 (58%) | χ2 = 0.94 | 0.63 | ||
| N1 | 8 (38%) | 5 (26%) | ||||
| N2 | 4 (19%) | 3 (16%) | ||||
| Adjuvant therapy, n (%) | ||||||
| Radiation | 7 (33%) | 6 (32%) | χ2 = 2.98 | 0.22 | ||
| Chemotherapy | 4 (19%) | 8 (42%) | ||||
| Radiation + chemotherapy | 10 (48%) | 5 (26%) | ||||
| Outcomes | PG | CG | MD | 95% CI | p-Value * | ηp2 | ||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Lower Bound | Upper Bound | |||||
| Pain (VAS) | Pre-treatment | 6.95 ± 1.07 | 6.79 ± 1.23 | 0.16 | −0.57 | 0.90 | 0.65 | 0.005 |
| Post-treatment | 4.33 ± 0.91 | 5.26 ± 1.20 | −0.93 | −1.61 | −0.25 | 0.008 | 0.17 | |
| Follow-up | 2.71 ± 1.01 | 4.42 ± 0.96 | −1.71 | −2.34 | −1.07 | 0.001 | 0.44 | |
| Function (DASH) | Pre-treatment | 59.29 ± 5.62 | 57.42 ± 3.58 | 1.87 | −1.19 | 4.92 | 0.22 | 0.03 |
| Post-treatment | 38.10 ± 4.16 | 49.16 ± 3.72 | −11.06 | −13.60 | −8.53 | 0.001 | 0.67 | |
| Follow-up | 29.05 ± 4.49 | 46.26 ± 3.43 | −17.21 | −19.79 | −14.64 | 0.001 | 0.82 | |
| Anexity (SAI) | Pre-treatment | 37.05 ± 4.62 | 35.26 ± 5.36 | 1.79 | −1.41 | 4.98 | 0.26 | 0.03 |
| Post-treatment | 30.48 ± 4.49 | 33.84 ± 5.07 | −3.36 | −6.43 | −0.31 | 0.03 | 0.12 | |
| Follow-up | 25.81 ± 3.54 | 30.89 ± 4.70 | −5.08 | −7.73 | −2.44 | 0.001 | 0.28 | |
| Fatigue (MFI) | Pre-treatment | 51.81 ± 7.09 | 52.26 ± 7.50 | −0.45 | −5.13 | 4.22 | 0.84 | 0.001 |
| Post-treatment | 40.24 ± 4.83 | 46.42 ± 7.14 | −6.18 | −10.05 | −2.32 | 0.003 | 0.22 | |
| Follow-up | 29.48 ± 4.80 | 41.53 ± 6.65 | −12.05 | −15.74 | −8.36 | 0.001 | 0.54 | |
| Barthel Index for (ADLs) | Pre-treatment | 61.43 ± 5.73 | 62.89 ± 8.05 | −1.46 | −5.91 | 2.97 | 0.51 | 0.01 |
| Post-treatment | 79.76 ± 6.22 | 72.63 ± 7.52 | 7.13 | 2.73 | 11.53 | 0.002 | 0.22 | |
| Follow-up | 86.19 ± 4.98 | 75 ± 6.87 | 11.19 | 7.38 | 15.00 | 0.001 | 0.48 | |
| Flexion ROM | Pre-treatment | 77.67 ± 2.56 | 78.79 ± 2.25 | −1.12 | −2.67 | 0.43 | 0.15 | 0.05 |
| Post-treatment | 84.43 ± 2.18 | 84.47 ± 2.29 | −0.04 | −1.48 | 1.39 | 0.95 | 0.001 | |
| Follow-up | 87.43 ± 1.75 | 83.74 ± 2.26 | 3.69 | 2.41 | 4.98 | 0.001 | 0.47 | |
| Extension ROM | Pre-treatment | 72.19 ± 2.96 | 73.16 ± 3.15 | −0.97 | −2.92 | 0.99 | 0.32 | 0.02 |
| Post-treatment | 79.14 ± 3.99 | 78.42 ± 2.79 | 0.72 | −1.51 | 2.95 | 0.51 | 0.01 | |
| Follow-up | 81.05 ± 3.11 | 78.79 ± 2.87 | 2.26 | 0.33 | 4.18 | 0.02 | 0.13 | |
| Grip strength | Pre-treatment | 13.90 ± 1.73 | 13.21 ± 1.13 | 0.69 | −0.25 | 1.64 | 0.15 | 0.05 |
| Post-treatment | 21.62 ± 2.27 | 17.89 ± 1.49 | 3.73 | 2.48 | 4.97 | 0.001 | 0.49 | |
| Follow-up | 23.71 ± 2 | 18.89 ± 1.41 | 4.82 | 3.70 | 5.94 | 0.001 | 0.67 | |
| Outcome | Pre-Treatment vs. Post-Treatment | Pre-Treatment vs. Follow-Up | Post-Treatment vs. Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | 95% CI | p Value * | MD | 95% CI | p Value * | MD | 95% CI | p Value * | ||||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||||
| Pain (VAS) | 2.62 | 2.12 | 3.12 | 0.001 | 4.24 | 3.64 | 4.84 | 0.001 | 1.62 | 1.19 | 2.05 | 0.001 |
| Function (DASH) | 21.19 | 18.68 | 23.70 | 0.001 | 30.24 | 27.53 | 32.95 | 0.001 | 9.05 | 7.52 | 10.58 | 0.001 |
| Anxiety (SAI) | 6.57 | 4.67 | 8.48 | 0.001 | 11.24 | 9.26 | 13.21 | 0.001 | 4.67 | 3.24 | 6.10 | 0.001 |
| Fatigue (MFI) | 11.57 | 8.81 | 14.34 | 0.001 | 22.33 | 18.16 | 26.51 | 0.001 | 10.76 | 7.77 | 13.75 | 0.001 |
| Barthel Index for (ADLs) | −18.33 | −21.92 | −14.74 | 0.001 | −24.76 | −28.13 | −21.40 | 0.001 | −6.43 | −8.36 | −4.50 | 0.001 |
| Flexion ROM | −6.76 | −8.22 | −5.31 | 0.001 | −9.76 | −11.41 | −8.12 | 0.001 | −3 | −4.21 | −1.79 | 0.001 |
| Extension ROM | −6.95 | −8.73 | −5.18 | 0.001 | −8.86 | −10.44 | −7.28 | 0.001 | −1.91 | −2.73 | −1.08 | 0.001 |
| Grip strength | −7.72 | −8.98 | −6.45 | 0.001 | −9.81 | −11.02 | −8.60 | 0.001 | −2.9 | −2.72 | −1.47 | 0.001 |
| Outcome | Pre-Treatment vs. Post-Treatment | Pre-Treatment vs. Follow-Up | Post-Treatment vs. Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | 95% CI | p Value * | MD | 95% CI | p Value * | MD | 95% CI | p Value * | ||||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||||
| Pain (VAS) | 1.53 | 1.00 | 2.05 | 0.001 | 2.39 | 1.74 | 3.00 | 0.001 | 0.86 | 0.39 | 1.29 | 0.001 |
| Function (DASH) | 8.26 | 5.62 | 10.90 | 0.001 | 11.16 | 8.31 | 14.01 | 0.001 | 2.9 | 1.29 | 4.50 | 0.001 |
| Anxiety (SAI) | 1.42 | −0.58 | 3.42 | 0.25 | 4.37 | 2.29 | 6.45 | 0.001 | 2.95 | 1.45 | 4.45 | 0.001 |
| Fatigue (MFI) | 5.84 | 2.93 | 8.75 | 0.001 | 10.73 | 6.35 | 15.13 | 0.001 | 4.89 | 1.75 | 8.04 | 0.001 |
| Barthel Index for (ADLs) | −9.74 | −13.51 | −5.96 | 0.001 | −12.11 | −15.64 | −8.57 | 0.001 | −2.37 | −4.40 | −0.34 | 0.001 |
| Flexion ROM | −5.68 | −7.22 | −4.15 | 0.001 | −4.95 | −6.68 | −3.22 | 0.001 | 0.73 | −0.53 | 2.01 | 0.46 |
| Extension ROM | −5.26 | −7.13 | −3.40 | 0.001 | −5.63 | −7.29 | −3.97 | 0.001 | −0.37 | −1.23 | 0.50 | 0.87 |
| Grip strength | −4.68 | −6.02 | −3.35 | 0.001 | −5.68 | −6.96 | −4.41 | 0.001 | −1 | −1.66 | −0.34 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelmoniem Ibrahim, A.; Aly, S.M.; Youssef, A.S.A.; Ragab, M.M.M.; Hussein, H.M. Using Virtual Reality Pablo Gaming in the Post-Operative Rehabilitation of Breast Cancer Patients: Randomized Controlled Trial. J. Clin. Med. 2024, 13, 7609. https://doi.org/10.3390/jcm13247609
Abdelmoniem Ibrahim A, Aly SM, Youssef ASA, Ragab MMM, Hussein HM. Using Virtual Reality Pablo Gaming in the Post-Operative Rehabilitation of Breast Cancer Patients: Randomized Controlled Trial. Journal of Clinical Medicine. 2024; 13(24):7609. https://doi.org/10.3390/jcm13247609
Chicago/Turabian StyleAbdelmoniem Ibrahim, Ahmed, Sobhy M. Aly, Ahmed S. A. Youssef, Mohamed Marzouk Mohamed Ragab, and Hisham M. Hussein. 2024. "Using Virtual Reality Pablo Gaming in the Post-Operative Rehabilitation of Breast Cancer Patients: Randomized Controlled Trial" Journal of Clinical Medicine 13, no. 24: 7609. https://doi.org/10.3390/jcm13247609
APA StyleAbdelmoniem Ibrahim, A., Aly, S. M., Youssef, A. S. A., Ragab, M. M. M., & Hussein, H. M. (2024). Using Virtual Reality Pablo Gaming in the Post-Operative Rehabilitation of Breast Cancer Patients: Randomized Controlled Trial. Journal of Clinical Medicine, 13(24), 7609. https://doi.org/10.3390/jcm13247609







