Allograft Bone Screw in a Comminuted Hawkins III Talar Neck Fracture: Case Report
Abstract
1. Introduction
2. Case Study
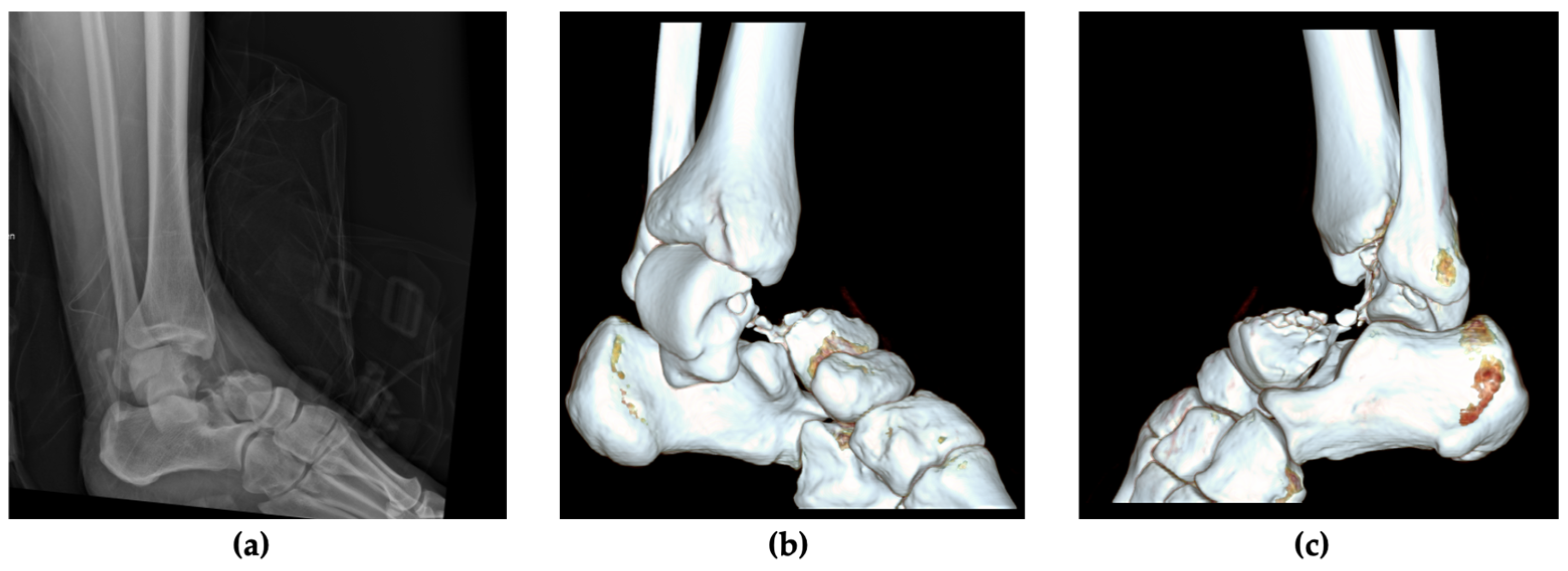
2.1. Patient Information, Clinical Findings and Diagnostic Assessment
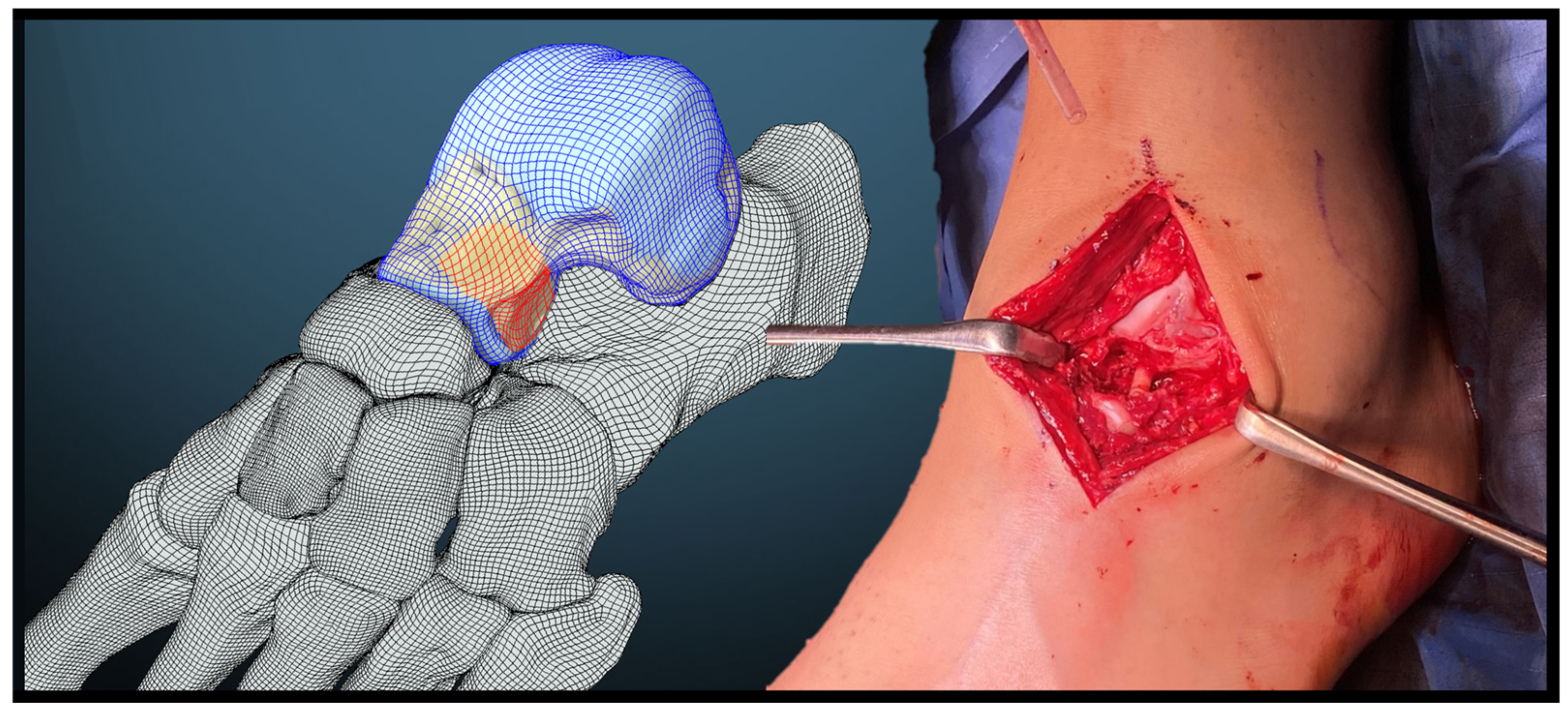
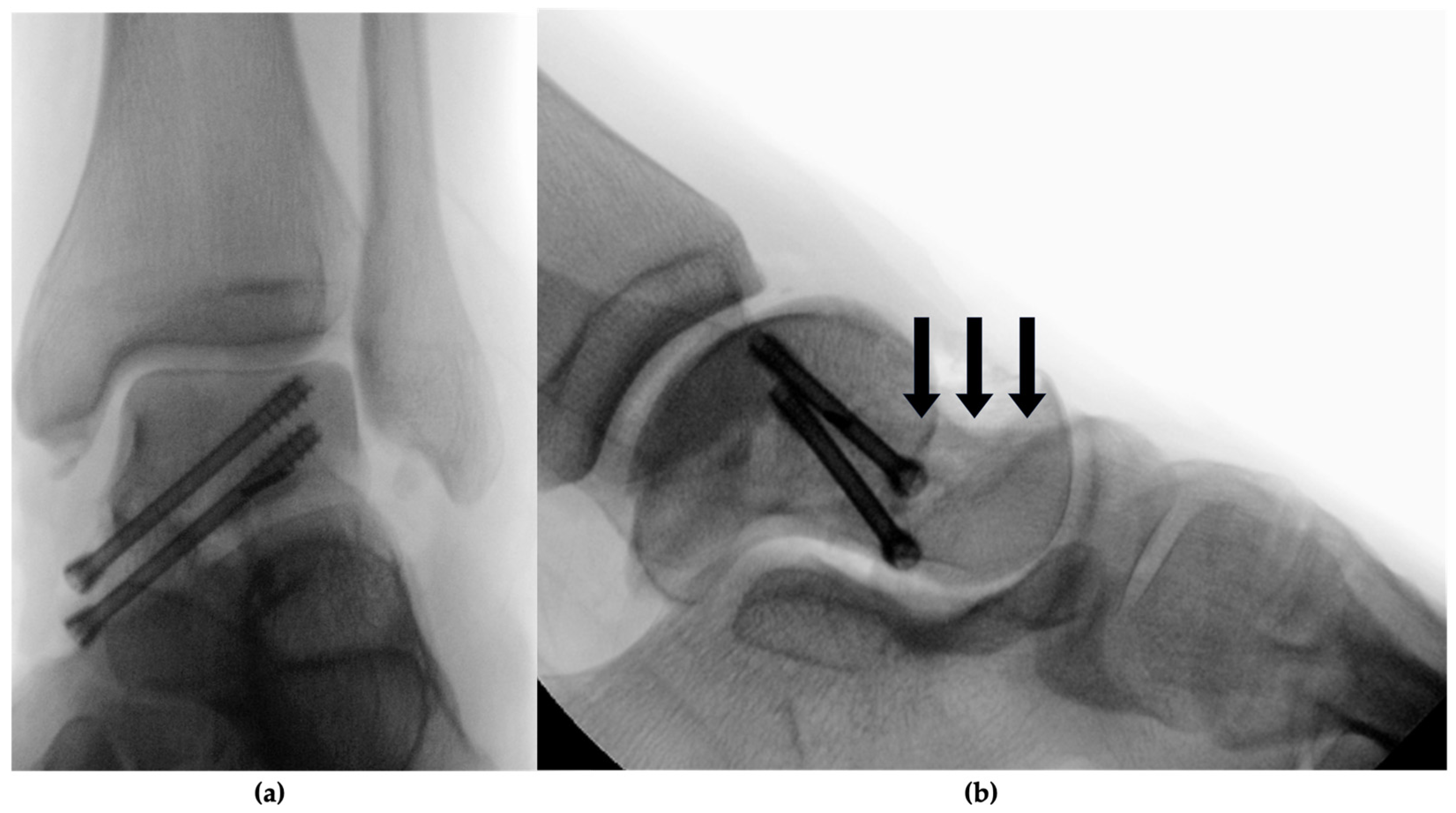
2.2. Therapeutic Intervention
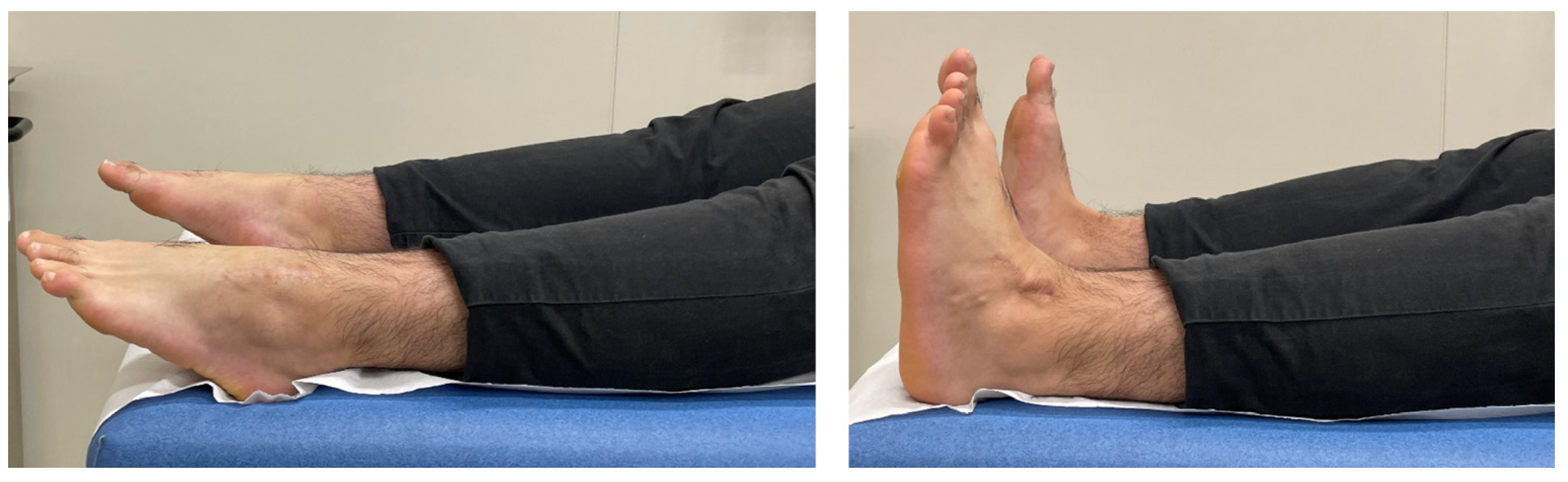
3. Follow-Up and Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fortin, P.T.; Balazsy, J.E. Talus fractures: Evaluation and treatment. JAAOS-J. Am. Acad. Orthop. Surg. 2001, 9, 114–127. [Google Scholar] [CrossRef] [PubMed]
- HAWKINS, L.G. Fractures of the neck of the talus. JBJS 1970, 52, 991–1002. [Google Scholar] [CrossRef]
- Alton, T.; Patton, D.J.; Gee, A.O. Classifications in Brief: The Hawkins Classification for Talus Fractures. Clin. Orthop. Relat. Res. 2015, 473, 3046–3049. [Google Scholar] [CrossRef] [PubMed]
- Vallier, H.A.; Nork, S.E.; Barei, D.P.; Benirschke, S.K.; Sangeorzan, B.J. Talar neck fractures: Results and outcomes. JBJS 2004, 86, 1616–1624. [Google Scholar] [CrossRef]
- Whitaker, C.; Turvey, B.; Illical, E.M. Current concepts in talar neck fracture management. Curr. Rev. Musculoskelet. Med. 2018, 11, 456–474. [Google Scholar] [CrossRef] [PubMed]
- Huber, T.; Hofstätter, S.G.; Fiala, R.; Hartenbach, F.; Breuer, R.; Rath, B. The application of an allogenic bone screw for stabilization of a modified chevron osteotomy: A prospective analysis. J. Clin. Med. 2022, 11, 1384. [Google Scholar] [CrossRef] [PubMed]
- Pastl, K.; Pastl, E.; Flöry, D.; Borchert, G.H.; Chraim, M. Arthrodesis and defect bridging of the upper ankle joint with allograft bone chips and allograft cortical bone screws (Shark Screw®) after removal of the salto-prosthesis in a multimorbidity patient: A case report. Life 2022, 12, 1028. [Google Scholar] [CrossRef] [PubMed]
- Sailer, S.; Lechner, S.; Floßmann, A.; Wanzel, M.; Habeler, K.; Krasny, C.; Borchert, G.H. Treatment of scaphoid fractures and pseudarthroses with the human allogeneic cortical bone screw. A multicentric retrospective study. J. Orthop. Traumatol. 2023, 24, 6. [Google Scholar] [CrossRef] [PubMed]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef] [PubMed]
- Saravi, B.; Lang, G.; Ruff, R.; Schmal, H.; Südkamp, N.; Ülkümen, S.; Zwingmann, J. Conservative and surgical treatment of talar fractures: A systematic review and meta-analysis on clinical outcomes and complications. Int. J. Environ. Res. Public Health 2021, 18, 8274. [Google Scholar] [CrossRef] [PubMed]
- Maher, M.H.; Chauhan, A.; Altman, G.T.; Westrick, E.R. The acute management and associated complications of major injuries of the talus. JBJS Rev. 2017, 5, e2. [Google Scholar] [CrossRef] [PubMed]
- Chateau, P.F.; Brokaw, D.; Jelen, B.; Scheid, D.; Weber, T. Plate fixation of talar neck fractures: Preliminary review of a new technique in twenty-three patients. J. Orthop. Trauma 2002, 16, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Maceroli, M.A.; Wong, C.; Sanders, R.W.; Ketz, J.P. Treatment of comminuted talar neck fractures with use of minifragment plating. J. Orthop. Trauma 2016, 30, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Schulze, W.; Richter, J.; Russe, O.; Ingelfinger, P.; Muhr, G. Surgical treatment of talus fractures. Acta Orthop. Scand. 2002, 73, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Swords, M.; Lakehomer, H.; McDonald, M.; Patel, J. Plate fixation of talus fractures: Where, when, and how? Indian J. Orthop. 2018, 52, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Labmayr, V.; Huber, E.; Wenzel-Schwarz, F.; Holweg, P.; Ornig, M.; Jakob, G.; Palle, W.; Borchert, G.H.; Pastl, K. Non-Union Treatment in the Foot, Ankle, and Lower Leg: A Multicenter Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®). J. Pers. Med. 2024, 14, 352. [Google Scholar] [CrossRef] [PubMed]
- Brcic, I.; Pastl, K.; Plank, H.; Igrec, J.; Schanda, J.E.; Pastl, E.; Werner, M. Incorporation of an allogenic cortical bone graft following arthrodesis of the first metatarsophalangeal joint in a patient with hallux rigidus. Life 2021, 11, 473. [Google Scholar] [CrossRef] [PubMed]
- Sangeorzan, B.J.; Wagner, U.A.; Harrington, R.M.; Tencer, A.F. Contact characteristics of the subtalar joint: The effect of talar neck misalignment. J. Orthop. Res. 1992, 10, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J. General principles of reconstruction. In Fractures and Dislocations of the Talus and Calcaneus: A Case-Based Approach; Springer: Cham, Switzerland, 2020; pp. 333–337. [Google Scholar]
- Ohl, X.; Harisboure, A.; Hemery, X.; Dehoux, E. Long-term follow-up after surgical treatment of talar fractures: Twenty cases with an average follow-up of 7.5 years. Int. Orthop. 2011, 35, 93–99. [Google Scholar] [CrossRef] [PubMed]


| 6 Months | 1 Year | 2 Years | |
|---|---|---|---|
| AOFAS | 85/100 | 88/100 | 100/100 |
| FAAM | 69/84 (82%) | 79/84 (94%) | 83/84 (99%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huetter, K.; Holweg, P.; Ornig, M.; Labmayr, V. Allograft Bone Screw in a Comminuted Hawkins III Talar Neck Fracture: Case Report. J. Clin. Med. 2024, 13, 7457. https://doi.org/10.3390/jcm13237457
Huetter K, Holweg P, Ornig M, Labmayr V. Allograft Bone Screw in a Comminuted Hawkins III Talar Neck Fracture: Case Report. Journal of Clinical Medicine. 2024; 13(23):7457. https://doi.org/10.3390/jcm13237457
Chicago/Turabian StyleHuetter, Konstanze, Patrick Holweg, Martin Ornig, and Viktor Labmayr. 2024. "Allograft Bone Screw in a Comminuted Hawkins III Talar Neck Fracture: Case Report" Journal of Clinical Medicine 13, no. 23: 7457. https://doi.org/10.3390/jcm13237457
APA StyleHuetter, K., Holweg, P., Ornig, M., & Labmayr, V. (2024). Allograft Bone Screw in a Comminuted Hawkins III Talar Neck Fracture: Case Report. Journal of Clinical Medicine, 13(23), 7457. https://doi.org/10.3390/jcm13237457






