Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Design
2.2.1. Forms of Compression
2.2.2. Survey
2.3. Statistical Analysis
3. Results
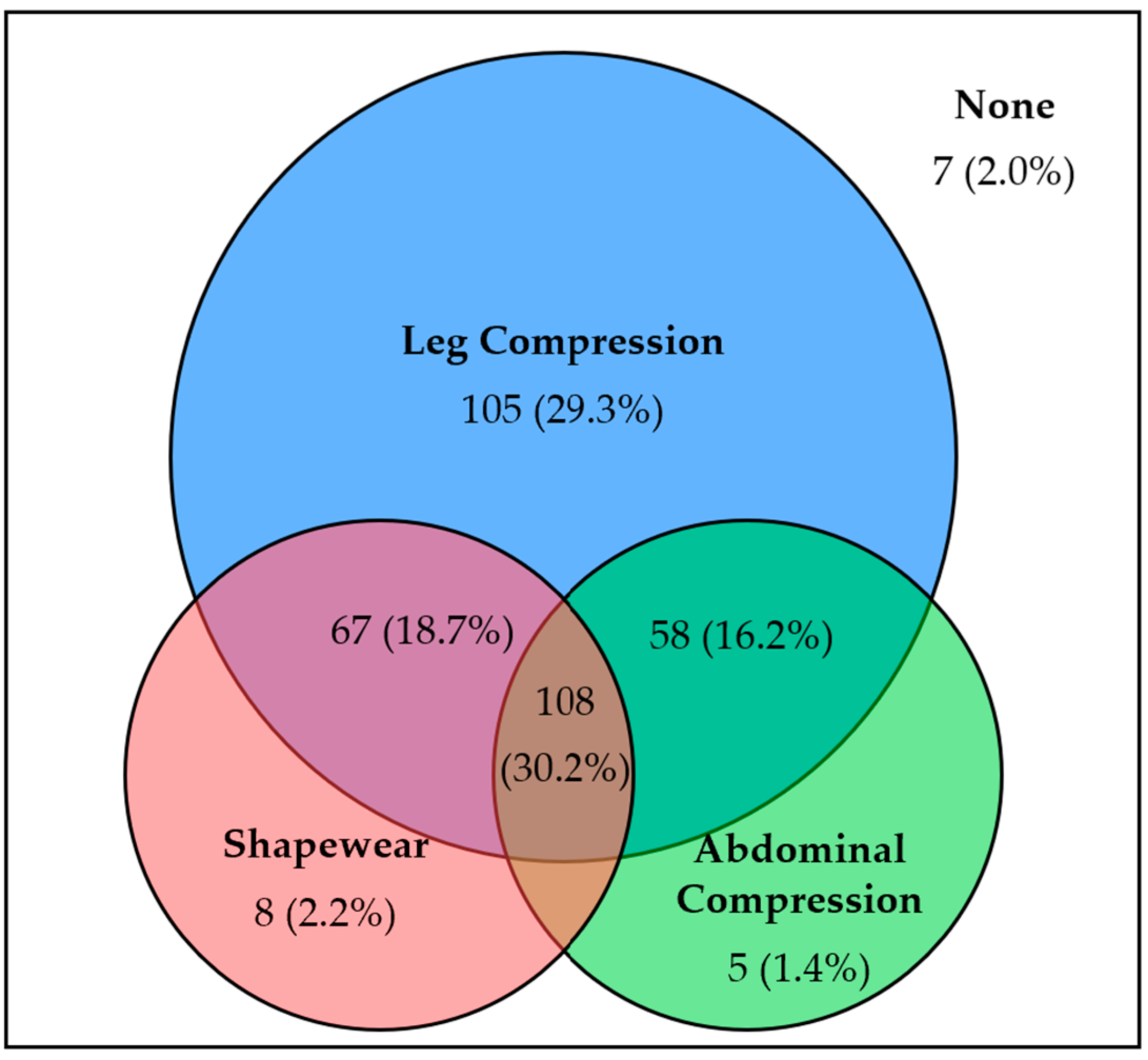
3.1. Forms of Compression Garments
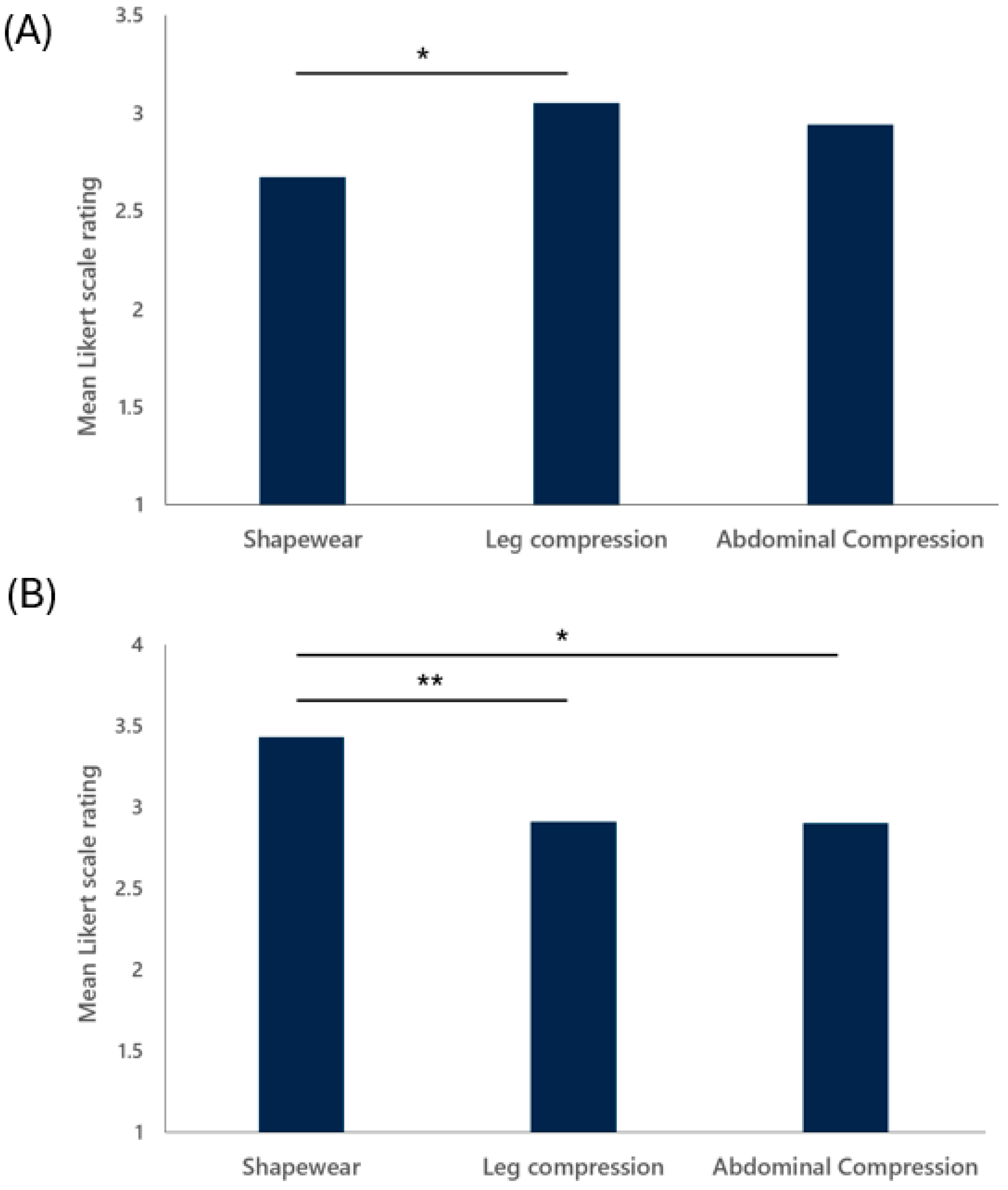
3.2. Product Feature Ratings
3.3. Different Treatment Approaches
4. Discussion
4.1. Main Findings
4.2. Compression Garments for POTS and nOH Patients
4.3. Compliance to Compression Therapy
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Abdominal Compression Garments | Leg Compression Garments | Shapewear | p-Value | |
|---|---|---|---|---|
| Comfort | 0.0299 | |||
| Mean (SD) | 2.94 (1.08) | 3.05 (1.11) | 2.67 (0.93) | |
| Aesthetic appeal | 0.606 | |||
| Mean (SD) | 2.63 (1.12) | 2.50 (1.09) | 2.63 (0.97) | |
| Concealability | 0.00246 | |||
| Mean (SD) | 2.90 (1.22) | 2.91 (1.08) | 3.43 (1.21) | |
| Ease of use | 0.945 | |||
| Mean (SD) | 3.21 (1.03) | 3.15 (1.09) | 3.15 (0.93) | |
| Durability | 0.592 | |||
| Mean (SD) | 3.65 (1.06) | 3.52 (0.92) | 3.47 (0.84) | |
| Cost effectiveness | 0.028 | |||
| Mean (SD) | 3.15 (0.92) | 2.73 (1.05) | 2.90 (1.02) | |
| Consistency | 0.779 | |||
| Mean (SD) | 3.33 (1.12) | 3.35 (1.21) | 3.24 (1.23) |
References
- Sebastian, S.A.; Co, E.L.; Panthangi, V.; Jain, E.; Ishak, A.; Shah, Y.; Vasavada, A.; Padda, I. Postural Orthostatic Tachycardia Syndrome (POTS): An Update for Clinical Practice. Curr. Probl. Cardiol. 2022, 47, 101384. [Google Scholar] [CrossRef] [PubMed]
- Garland, E.M.; Celedonio, J.E.; Raj, S.R. Postural Tachycardia Syndrome: Beyond Orthostatic Intolerance. Curr. Neurol. Neurosci. Rep. 2015, 15, 60. [Google Scholar] [CrossRef] [PubMed]
- Robertson, D. The Epidemic of Orthostatic Tachycardia and Orthostatic Intolerance. Am. J. Med. Sci. 1999, 317, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Hamrefors, V.; Spahic, J.M.; Nilsson, D.; Senneby, M.; Sutton, R.; Melander, O.; Fedorowski, A. Syndromes of orthostatic intolerance and syncope in young adults. Open Heart 2017, 4, e000585. [Google Scholar] [CrossRef]
- Arnold, A.C.; Ng, J.; Raj, S.R. Postural tachycardia syndrome—Diagnosis, physiology, and prognosis. Auton. Neurosci. 2018, 215, 3–11. [Google Scholar] [CrossRef]
- Raj, S.R.; Biaggioni, I.; Yamhure, P.C.; Black, B.K.; Paranjape, S.Y.; Byrne, D.W.; Robertson, D. Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation 2005, 111, 1574–1582. [Google Scholar] [CrossRef]
- Olufsen, M.S.; Ottesen, J.T.; Tran, H.T.; Ellwein, L.M.; Lipsitz, L.A.; Novak, V. Blood pressure and blood flow variation during postural change from sitting to standing: Model development and validation. J. Appl. Physiol. 2005, 99, 1523–1537. [Google Scholar] [CrossRef]
- Jacob, G.; Biaggioni, I.; Mosqueda-Garcia, R.; Marie Robertson, R.; Robertson, D. Relation of Blood Volume and Blood Pressure in Orthostatic Intolerance. Am. J. Med. Sci. 1998, 315, 95–100. [Google Scholar] [CrossRef]
- Okamoto, L.E.; Raj, S.R.; Peltier, A.; Gamboa, A.; Shibao, C.; Diedrich, A.; Black, B.K.; Robertson, D.; Biaggioni, I. Neurohumoral and haemodynamic profile in postural tachycardia and chronic fatigue syndromes. Clin. Sci. 2012, 122, 183–192. [Google Scholar] [CrossRef]
- Gibbons, C.H.; Bonyhay, I.; Benson, A.; Wang, N.; Freeman, R. Structural and functional small fiber abnormalities in the neuropathic postural tachycardia syndrome. PLoS ONE 2013, 8, e84716. [Google Scholar] [CrossRef]
- Gibbons, C.H.; Schmidt, P.; Biaggioni, I.; Frazier-Mills, C.; Freeman, R.; Isaacson, S.; Karabin, B.; Kuritzky, L.; Lew, M.; Low, P.; et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J. Neurol. 2017, 264, 1567–1582. [Google Scholar] [CrossRef] [PubMed]
- Palma, J.A.; Kaufmann, H. Epidemiology, Diagnosis, and Management of Neurogenic Orthostatic Hypotension. Mov. Disord. Clin. Pract. 2017, 4, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.R.; Guzman, J.C.; Harvey, P.; Richer, L.; Schondorf, R.; Seifer, C.; Thibodeau-Jarry, N.; Sheldon, R.S. Canadian Cardiovascular Society Position Statement on Postural Orthostatic Tachycardia Syndrome (POTS) and Related Disorders of Chronic Orthostatic Intolerance. Canadian J. Cardiol. 2020, 36, 357–372. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.J.; Raj, S.R. Pharmacotherapy for postural tachycardia syndrome. Auton. Neurosci. 2018, 215, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Thijs, R.D.; Wieling, W.; Kaufmann, H.; Claydon, V.E.; Van Wijnen, V.K.; Harms, M.P.M.; Juraschek, S.P.; Thijs, R.D. Diagnosis and treatment of orthostatic hypotension. Lancet Neurol. 2022, 21, 735–746. [Google Scholar]
- Fedorowski, A. Postural orthostatic tachycardia syndrome: Clinical presentation, aetiology and management. J. Intern. Med. 2019, 285, 352–366. [Google Scholar] [CrossRef]
- Denq, J.; Opfer-Gehrking, T.; Giuliani, M.; Convertino, V.; Low, P.; Low, P.A. Efficacy of compression of different capacitance beds in the amelioration of orthostatic hypotension. Clin. Auton. Res. 1997, 7, 321–326. [Google Scholar] [CrossRef]
- Smit, A.A.J.; Wieling, W.; Fujimura, J.; Denq, J.C.; Opfer-Gehrking, T.L.; Akarriou, M.; Karemaker, J.M.; Low, P.A. Use of lower abdominal compression to combat orthostatic hypotension in patients with autonomic dysfunction. Clin. Auton. Res. 2004, 14, 167–175. [Google Scholar] [CrossRef]
- Bourne, K.M.; Sheldon, R.S.; Hall, J.; Lloyd, M.; Kogut, K.; Sheikh, N.; Jorge, J.; Ng, J.; Exner, D.V.; Tyberg, J.V.; et al. Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients with Postural Orthostatic Tachycardia Syndrome. J. Am. Coll. Cardiol. 2021, 77, 285–296. [Google Scholar] [CrossRef]
- Coniglio, A.C.; Kittipibul, V.; Pelligra, R.; Richardson, E.S.; Holley, C.L.; Fudim, M. One Small Step for a Patient, One Giant Leap for Orthostatic Hypotension. Cureus 2022, 14, e31612. [Google Scholar] [CrossRef]
- Tani, H.; Singer, W.; McPhee, B.R.; Opfer-Gehrking, T.L.; Haruma, K.; Kajiyama, G.; Low, P.A. Splanchnic-mesenteric capacitance bed in the postural tachycardia syndrome (POTS). Auton. Neurosci. 2000, 86, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.J.; Singer, W.; Sandroni, P.; Sletten, D.M.; Gehrking, T.L.; Gehrking, J.A.; Low, P.; Basford, J.R. Effects of patient-controlled abdominal compression on standing systolic blood pressure in adults with orthostatic hypotension. Arch. Phys. Med. Rehabil. 2015, 96, 505–510. [Google Scholar] [CrossRef] [PubMed]
- McGregor, G.; Hee, S.W.; Eftekhari, H.; Holliday, N.; Pearce, G.; Sandhu, H.; Simmonds, J.; Joshi, S.; Kavi, L.; Bruce, J.; et al. Protocol for a randomised controlled feasibility trial of exercise rehabilitation for people with postural tachycardia syndrome: The PULSE study. Pilot. Feasibility Stud. 2020, 6, 157. [Google Scholar] [CrossRef] [PubMed]
- Dahm, K.T.; Myrhaug, H.T.; Strømme, H.; Fure, B.; Brurberg, K.G. Effects of preventive use of compression stockings for elderly with chronic venous insufficiency and swollen legs: A systematic review and meta-analysis. BMC Geriatr. 2019, 19, 76. [Google Scholar] [CrossRef] [PubMed]
- Partsch, H.; Partsch, B.; Braun, W. Interface pressure and stiffness of ready made compression stockings: Comparison of in vivo and in vitro measurements. J. Vasc. Surg. 2006, 44, 809–814. [Google Scholar] [CrossRef]
- Faisal Sh Adnan, M.; Antonin, H.; Tanveer, H. Effect of elastane linear density on compression pressure of V-shaped compression socks. Ind. Textila 2018, 69, 118–127. [Google Scholar] [CrossRef]
- Fu, Q.; Levine, B.D. Exercise and non-pharmacological treatment of POTS. Auton. Neurosci. 2018, 215, 20–27. [Google Scholar] [CrossRef]
- Harper, D.; Chandler, B. Splanchnic circulation. BJA Educ. 2016, 16, 66–71. [Google Scholar] [CrossRef]
- Pelling, M.M.; Brown, M.T.; Gilliland, C.A.; Cutchins, A. Left Common Iliac Vein Stenting in a Case of Postural Orthostatic Tachycardia Syndrome/Pelvic Pain Overlap. Cureus 2024, 16, e53974. [Google Scholar] [CrossRef]
- Wigg, J.; Lee, N. Use of compression shorts in the management of lymphoedema and lipoedema. Br. J. Community Nurs. 2014, 19, S30–S35. [Google Scholar] [CrossRef]
- Hill, J.A.; Howatson, G.; van Someren, K.A.; Davidson, S.; Pedlar, C.R. The variation in pressures exerted by commercially available compression garments. Sports Eng. 2015, 18, 115–121. [Google Scholar] [CrossRef]
- Lee, N.; Wigg, J. Getting the right fit: Made-to-measure garments for lymphoedema management. Br. J. Community Nurs. 2013, 18, S28–S33. [Google Scholar] [CrossRef] [PubMed]
- Chitambira, F. Patient perspectives: Explaining low rates of compliance to compression therapy. Wound Pract. Res. 2019, 27, 168–174. [Google Scholar] [CrossRef]
- Deb, A.; Morgenshtern, K.; Culbertson, C.J.; Wang, L.B.; Hohler, A.D. A Survey-Based Analysis of Symptoms in Patients with Postural Orthostatic Tachycardia Syndrome. Bayl. Univ. Med. Cent. Proc. 2015, 28, 157–159. [Google Scholar] [CrossRef] [PubMed]


| Product Feature | Description |
|---|---|
| Comfort | Are you comfortable while wearing the garment? |
| Aesthetic appeal | Does the garment fit into your existing wardrobe? |
| Concealability | Is the garment visible underneath clothing? |
| Ease of use | Can the garment easily be donned and doffed? |
| Durability | Can the garment withstand many usages? |
| Cost-effectiveness | Is the garment fairly priced considering its purpose? |
| Consistency | Does the garment reliably and consistently apply therapeutic pressure? |
| nOH (N = 28) | POTS (N = 330) | Overall (N = 358) | p-Value | |
|---|---|---|---|---|
| Age (Years) | 0.00011 | |||
| Mean (SD) | 49.6 (14.8) | 36.9 (11.4) | 37.9 (12.2) | |
| Gender | 0.4317 | |||
| F | 26 (92.9%) | 314 (95.2%) | 340 (95.0%) | |
| M | 2 (7.1%) | 8 (2.4%) | 10 (2.8%) | |
| Other | 0 | 8 (2.4%) | 8 (2.3%) | |
| Ethnicity | 0.9231 | |||
| Black or African American | 0 (0%) | 3 (0.9%) | 3 (0.8%) | |
| White | 27 (96.4%) | 297 (90.0%) | 324 (90.5%) | |
| Other | 1 (3.6%) | 30 (9.1%) | 31 (8.7%) | |
| BMI | 0.0110 | |||
| Mean (SD) | 24.5 (5.87) | 27.7 (7.69) | 27.5 (7.60) | |
| Tried shapewear | 0.6052 | |||
| N | 15 (53.6%) | 160 (48.5%) | 175 (48.9%) | |
| Y | 13 (46.4%) | 170 (51.5%) | 183 (51.1%) | |
| Tried abdominal compression | 0.1531 | |||
| N | 11 (39.3%) | 176 (53.3%) | 187 (52.2%) | |
| Y | 17 (60.7%) | 154 (46.7%) | 171 (47.8%) | |
| Tried leg compression | 0.6287 | |||
| N | 1 (3.6%) | 19 (5.8%) | 20 (5.6%) | |
| Y | 27 (96.4%) | 311 (94.2%) | 338 (94.4%) | |
| Most used garment | 0.6909 | |||
| Shapewear | 7 (25.0%) | 65 (19.7%) | 72 (20.1%) | |
| Abdominal compression | 5 (17.9%) | 43 (13.0%) | 48 (13.4%) | |
| Leg compression | 16 (57.1%) | 218 (66.1%) | 234 (65.4%) | |
| None | 0 (0%) | 4 (1.2%) | 4 (1.1%) |
| nOH (N = 28) | POTS (N = 330) | Overall (N = 358) | p-Value | |
| Fluid and salt intake | 0.509 | |||
| N | 10 (35.7%) | 139 (42.1%) | 149 (41.6%) | |
| Y | 18 (64.3%) | 191 (57.9%) | 209 (58.4%) | |
| Exercise | 0.633 | |||
| N | 24 (85.7%) | 258 (78.2%) | 282 (78.8%) | |
| Y | 4 (14.3%) | 72 (21.8%) | 76 (21.2%) | |
| Compression | 0.7287 | |||
| N | 26 (92.9%) | 300 (90.9%) | 326 (91.1%) | |
| Y | 2 (7.1%) | 30 (9.1%) | 32 (8.9%) | |
| Pharmacotherapy | 0.9894 | |||
| N | 16 (57.1%) | 189 (57.3%) | 205 (57.3%) | |
| Y | 12 (42.9%) | 141 (42.7%) | 153 (42.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitra, K.; Kunte, S.; Taube, S.; Tian, W.; Richardson, E.; Frazier-Mills, C.; Fudim, M. Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension. J. Clin. Med. 2024, 13, 7304. https://doi.org/10.3390/jcm13237304
Mitra K, Kunte S, Taube S, Tian W, Richardson E, Frazier-Mills C, Fudim M. Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension. Journal of Clinical Medicine. 2024; 13(23):7304. https://doi.org/10.3390/jcm13237304
Chicago/Turabian StyleMitra, Kishen, Sameer Kunte, Sara Taube, William Tian, Eric Richardson, Camille Frazier-Mills, and Marat Fudim. 2024. "Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension" Journal of Clinical Medicine 13, no. 23: 7304. https://doi.org/10.3390/jcm13237304
APA StyleMitra, K., Kunte, S., Taube, S., Tian, W., Richardson, E., Frazier-Mills, C., & Fudim, M. (2024). Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension. Journal of Clinical Medicine, 13(23), 7304. https://doi.org/10.3390/jcm13237304








