State of the Art in Rehabilitation Strategies After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Extraction and Quality Assessment
2.3. Quality and Risk of Bias Evaluation
2.4. Selection of Articles
3. Results
3.1. Summary of Results
3.2. Manual Therapy
3.3. Aquatic Program
3.4. Stretching
3.5. Strengthening, Core, Balance, and Proprioception
3.6. Cardiovascular Training
3.7. Return to Sport
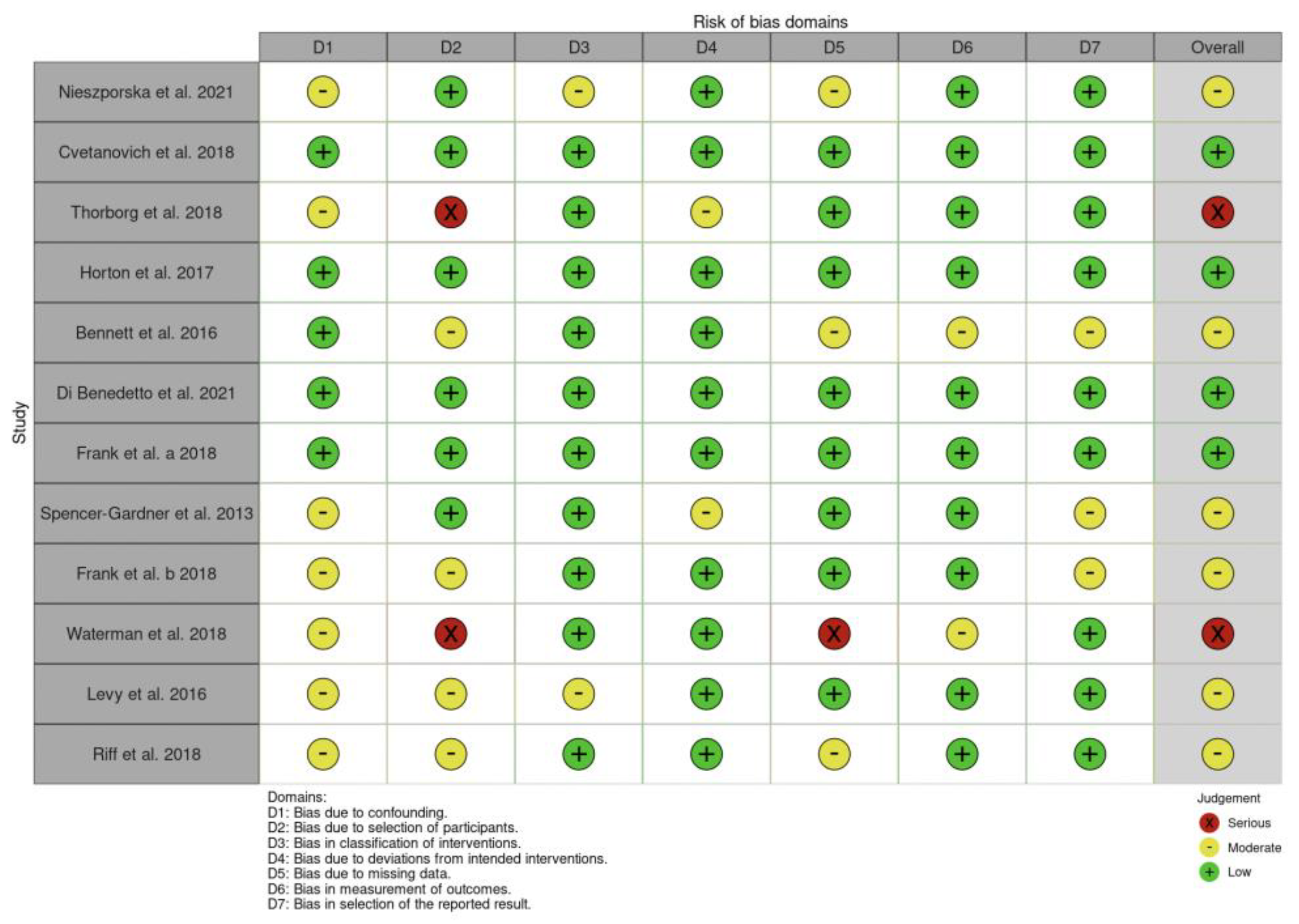
3.8. Risk of Bias and Quality of Evidence
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Müller-Torrente, A.; Puig-Torregrosa, J.; Montero-Navarro, S.; Sanz-Reig, J.; Morera-Balaguer, J.; Más-Martínez, J.; Sánchez-Mas, J.; Botella-Rico, J.M. Benefits of a Specific and Supervised Rehabilitation Program in Femoroacetabular Impingement Patients Undergoing Hip Arthroscopy: A Randomized Control Trial. J. Clin. Med. 2021, 10, 3125. [Google Scholar] [CrossRef] [PubMed]
- Riff, A.J.; Ukwuani, G.; Clapp, I.; Movassaghi, K.; Kelly, D.M.; Nho, S.J. High Rate of Return to High-Intensity Interval Training After Arthroscopic Management of Femoroacetabular Impingement Syndrome. Am. J. Sports Med. 2018, 46, 2594–2600. [Google Scholar] [CrossRef] [PubMed]
- Cvetanovich, G.L.; Weber, A.E.; Kuhns, B.D.; Alter, J.; Harris, J.D.; Mather, R.C., 3rd; Nho, S.J. Hip Arthroscopic Surgery for Femoroacetabular Impingement with Capsular Management: Factors Associated with Achieving Clinically Significant Outcomes. Am. J. Sports Med. 2018, 46, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Cheatham, S.W.; Kolber, M.J. Rehabilitation after hip arthroscopy and labral repair in a high school football athlete. Int. J. Sports Phys. Ther. 2012, 7, 173–184. [Google Scholar]
- Frank, R.M.; Ukwuani, G.; Chahla, J.; Batko, B.; Bush-Joseph, C.A.; Nho, S.J. High Rate of Return to Swimming After Hip Arthroscopy for Femoroacetabular Impingement. Arthroscopy 2018, 34, 1471–1477. [Google Scholar] [CrossRef] [PubMed]
- Palmer, A.J.; Malak, T.T.; Broomfield, J.; Holton, J.; Majkowski, L.; Thomas, G.E.; Taylor, A.; Andrade, A.J.; Collins, G.; Watson, K.; et al. Past and projected temporal trends in arthroscopic hip surgery in England between 2002 and 2013. BMJ Open Sport Exerc. Med. 2016, 21, e000082. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bistolfi, A.; Guidotti, C.; Aprato, A.; Sabatini, L.; Artiaco, S.; Massè, A.; Ferracini, R. Rehabilitation Protocol After Hip Arthroscopy: A 2015-2020 Systematic Review. Am. J. Phys. Med. Rehabil. 2021, 100, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Maimaitimin, M.; Yang, F.; Huang, H.J.; Xu, Y.; Zhang, X.; Ao, Y.F.; Wang, J.Q. Outcomes after hip arthroscopy for femoroacetabular impingement syndrome in Chinese patients: A minimum 2-year follow-up study. Orthop. J. Sports Med. 2022. [Google Scholar] [CrossRef]
- Griffin, D.R.; Dickenson, E.J.; Wall, P.D.H.; Achana, F.; Donovan, J.L.; Griffin, J.; Hobson, R.; Hutchinson, C.E.; Jepson, M.; Parsons, N.R.; et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): A multicentre randomised controlled trial. Lancet 2018, 391, 2225–2235. [Google Scholar] [CrossRef]
- Hanish, S.; Muhammed, M.; Kelly, S.; DeFroda, S. Postoperative Rehabilitation for Arthroscopic Management of Femoroacetabular Impingement Syndrome: A Contemporary Review. Curr. Rev. Musculoskelet. Med. 2023, 16, 381–391. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ryan, R.; Hill, S. How to GRADE the Quality of the Evidence; Cochrane Consumers and Communication Group: London, UK, 2016. [Google Scholar]
- Bennell, K.L.; Spiers, L.; Takla, A.; O’Donnell, J.; Kasza, J.; Hunter, D.J.; Hinman, R.S. Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: A randomised controlled trial (FAIR). BMJ Open 2017, 23, e014658. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nieszporska, O.; Truszczyńska-Baszak, A. Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI-Femoroacetabular Impingement: A Case-Control Study and Preliminary Report. J. Clin. Med. 2021, 10, 1023. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thorborg, K.; Kraemer, O.; Madsen, A.D.; Hölmich, P. Patient-Reported Outcomes Within the First Year After Hip Arthroscopy and Rehabilitation for Femoroacetabular Impingement and/or Labral Injury: The Difference Between Getting Better and Getting Back to Normal. Am. J. Sports Med. 2018, 46, 2607–2614. [Google Scholar] [CrossRef] [PubMed]
- Horton, B.S.; Marland, J.D.; West, H.S.; Wylie, J.D. Transition to Telehealth Physical Therapy After Hip Arthroscopy for Femoroacetabular Impingement: A Pilot Study with Retrospective Matched-Cohort Analysis. Orthop. J. Sports Med. 2021, 9, 1–6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bennett, A.N.; Nixon, J.; Roberts, A.; Barker-Davies, R.; Villar, R.; Houghton, J.M. Prospective 12-month functional and vocational outcomes of hip arthroscopy for femoroacetabular impingement as part of an evidence-based hip pain rehabilitation pathway in an active military population. BMJ Open Sport. Exerc. Med. 2016, 9, e000144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Di Benedetto, P.; Vidi, D.; Buttironi, M.M.; Mancuso, F.; Ricciarelli, M.; Causero, A. Outcomes in arthroscopic surgery and proposal rehabilitative treatment in femoral acetabular impingement syndrome. Acta Biomed. 2022, 92, e2021575. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frank, R.M.; Ukwuani, G.; Clapp, I.; Chahla, J.; Nho, S.J. High Rate of Return to Cycling After Hip Arthroscopy for Femoroacetabular Impingement Syndrome. Sports Health 2018, 10, 259–265. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Spencer-Gardner, L.; Eischen, J.J.; Levy, B.A.; Sierra, R.J.; Engasser, W.M.; Krych, A.J. A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 848–859. [Google Scholar] [CrossRef] [PubMed]
- Waterman, B.R.; Ukwuani, G.; Clapp, I.; Malloy, P.; Neal, W.H.; Nho, S.J. Return to Golf After Arthroscopic Management of Femoroacetabular Impingement Syndrome. Arthroscopy 2018, 34, 3187–3193.e1. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.M.; Kuhns, B.D.; Frank, R.M.; Grzybowski, J.S.; Campbell, K.A.; Brown, S.; Nho, S.J. High Rate of Return to Running for Athletes After Hip Arthroscopy for the Treatment of Femoroacetabular Impingement and Capsular Plication. Am. J. Sports Med. 2017, 45, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.R.; Larson, C.M.; Bedi, A. Indications for Hip Arthroscopy. Sports Health 2017, 9, 402–413. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mora, R.; Soldini, A.; Raschellà, F.; Paparella, F.; Belluati, A.; Basile, G. Primitive synovial chondromatosis of the hip joint. Ital. J. Orthop. Traumatol. 1992, 18, 231–239. [Google Scholar] [PubMed]
- Kelly, B.T.; Williams, R.J., 3rd; Philippon, M.J. Hip arthroscopy: Current indications, treatment options, and management issues. Am. J. Sports Med. 2003, 31, 1020–1037. [Google Scholar] [CrossRef] [PubMed]
- Edelstein, J.; Ranawat, A.; Enseki, K.R.; Yun, R.J.; Draovitch, P. Post-operative guidelines following hip arthroscopy. Curr. Rev. Musculoskelet. Med. 2012, 5, 15–23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Voight, M.L.; Robinson, K.; Gill, L.; Griffin, K. Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health 2010, 2, 222–230. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wahoff, M.; Ryan, M. Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin. Sports Med. 2011, 30, 463–482. [Google Scholar] [CrossRef] [PubMed]
- Dimitrakopoulou, A.; English, B.; Kartsonaki, C.; Gledhill, A.; Schilders, E. The effectiveness of hydrotherapy on return to play in sports following hip arthroscopic surgery: A comparative study. Hip Int. 2024, 34, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Kuhns, B.D.; Weber, A.E.; Batko, B.; Nho, S.J.; Stegemann, C. A Four-Phase Physical Therapy Regimen for Returning Athletes to Sport Following Hip Arthroscopy for Femoroacetabular Impingement with Routine Capsular Closure. Int. J. Sports Phys. Ther. 2017, 12, 683–696. [Google Scholar] [PubMed] [PubMed Central]
- Weber, A.E.; Nakata, H.; Mayer, E.N.; Bolia, I.K.; Philippon, M.J.; Snibbe, J.; Romano, R.; Tibone, J.E.; Gamradt, S.C. Return to Sport After Hip Arthroscopy for Femoroacetabular Impingement Syndrome in NCAA Division I Athletes: Experience at a Single Institution. Orthop. J. Sports Med. 2020, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]

| Authors | Study Design | Patients Total | Age | Population | Surgical Techniques | Treatment | Main findings |
|---|---|---|---|---|---|---|---|
| Bennel et al. 2017 [14] | RCT | 30 | 31 ± 7 and 28.6 ± 8.1 | Elite and recreational athletes | Labral repair, femoral osteochondroplasty | PT group: seven 30 min individual appointments with a study physiotherapist: one preoperative visit (after baseline assessment) within 2 weeks prior to surgery and six postoperative visits commencing at week two (approximately 2, 4, 6, 8, 10 and 12 weeks postsurgery). Control group: received no physiotherapist-prescribed rehabilitation programme | 14 and 24 week post-surgery. At week 14, PT group showed significantly greater improvements on the iHOT-33 and HOS-SS (p < 0.05) |
| Müller-Torrente et al. 2021 [1] | RCT | 100 | 41.3± 10.2 (41.8 ± 12.4, 40.9 ± 7.6) | Recreational athletes | Hip arthroscopic with an inside-out technique | PT group: physiotherapy session of 45 min each, once every two weeks for a total of 7 sessions (weeks 2, 4, 6, 8, 10, 12 and 14 post-surgery) Control Group: usual care | 4 and 14 week post-surgery. The experimental group achieved statistically significant improvement over the control group in terms of: diagnostic tests, ROM, VAS (p < 0.001) and mHHS (p < 0.001) at 14 weeks |
| Nieszporska et al. 2021 [15] | Case-Control | 12 | 40.1 ± 9.7 | Adult patients | Standard surgery | Rehabilitation program lasting between 4 and 6 months | 21.2 months. After surgery, 67% of patients returned to exercise at the same or higher level. The mean HHS results were good, with values of 88.00 ± 11.48. The SF-36 scores were >50 |
| Cvetanovich et al 2018 [3] | Case-Control | 386 | 33.3 ± 12.1 | General population with high percentage of sports/hobbies (71.5%) | Labral repair, acetabular rim trimming, femoral osteochondroplasty, capsular repair, and acetabular delamination | 4-phase rehabilitation protocol lasting between 24 and 32 weeks | 2 years minimum. At minimum 2-yr follow-up, patients had statistically significant (p < 0.001) improvements in all PROs with a 1.2% rate of revision surgery and 1.7% rate of conversion to THA. MCID was achieved by 78.8% of patients. |
| Thorborg et al. 2018 [16] | Cohort Study | 97 158 | 37.5 39 | Patients undergoing hip arthroscopy | Standard 2-portal technique (anterolateral and inferior midanterior), labral reapair | 4-phase rehabilitation program (mobility, stability, strength and return to sport/competition) supervised by the local physiotherapist | 3, 6 and 12 months. Improvements for all HAGOS subscales and mHHS results were seen at 3 months (p < 0.001). Were seen only improvements for HAGOS Sport and Recreation (Sport/Rec) and Participation in Physical Activities (PA) subscales between 3 and 12 months (p < 0.05) but not for HAGOS Pain, Symptoms, Activities of Daily Living (ADL), or Hip-Related Quality of Life (QOL) subscales or the mHHS |
| Horton et al. 2021 [17] | Cohort study | 51 | 33.94 ± 10.4 33.8 ± 10.3 33.5 ± 10.2 | Patients with primary hip arthroscopy | Femoroplasty, labral repair, chondrolabaral debriment, acetabuloplasty | Intervention group: patients undergoing initial in-person visits followed by a transition to telehealth physical therapy for 3 months postoperatively. the telehealth visits consisted of up to 22 minutes of guided exercise program. Comparison group 1: patients undergoing in-person physical therapy with the same physical therapy team as the telehealth group Comparison group 2: and patients undergoing in-person therapy with a different therapy team at the same facility | 3 months. There was no difference in preoperative, postoperative, or the change in iHOT-12. All groups had a significant improvement in iHOT-12 from preoperatively to the 3-month postoperative evaluation. |
| Bennett et al. 2016 [18] | Observational study | 101 | 33 | Active military population | - | Patients undergoing a progressive rehabilitation program by the military rehabilitation team | 2, 6 and 12 months. There were significant improvements, compared with baseline, at 12-month follow-up for all measurement scales: VAS (p << 0.001), NHAS (p < 0.001) and FAA (p < 0.001) |
| Di Benedetto et al. 2021 [19] | Observational study | 19 | 37 ± 3.8 | Young adult population | Arthroscopic acetabular rim trimming and osteochondroplasty of the femoral head-neck junction | The rehabilitation process was divided into 3 phases: Phase I or protection (0 to 2 weeks p.o.)Phase II or middle (2 to 4 weeks p.o.) Phase III or advanced (4 to 6 weeks p.o.) | 6 week and 3 months. Six weeks after surgery T0 and T1, there is a pain reduction of 36.04%, while at the 3-month follow-up the reduction is 33.44%. WOCMAN scale had a statistically significant improvement in activities of daily living and general performance [p (T0–T1) = 0.0219], p (T0–T2) = 0.0227] |
| Frank et al. 2018 [20] | Case series | 58 | 30 ± 7.1 | Recreational Athletes (cycling) | Labral repair, femoral osteochondroplasty, capsular closure, acetabular rim trimming | 4-phase rehabilitation protocol: 1: protect the hip joint 2: noncompensatory gait progression 3: return to preinjury function 4: return to sport | minimum 2 years after surgery. 97% of cyclist returned to sport, on average 4.5 months after surgery. 91% ± 13% satisfaction rate in all PROs (p < 0.0001) |
| Spencer-Gardner et al. 2013 [21] | Case series | 52 | 39.2 ± 12.2 | Young adult population | - | Five-phase rehabilitation: Phase 1: day 1 to week 4 (1-2 times for week) Phase 2: weeks 4-8 (e times for week) Phase 3: weeks 8-12 (2-3 times for week) Phase 4: weeks 12-16 (1-2 times for week) Phase 5: weeks 16-24 (return to full activity/sport) | Minimum 1 year. Mean MHHS, HOS-ADL, and HOS-sport scores at a mean 12.5 (range 12–15) months were 80.1 ± 19.9 (0–100), 83.6 ± 19.2 (13.2–100), and 70.3 ± 27.0 (0–100), respectively. |
| Frank et al. 2018 [5] | Case series | 26 | 31.1 ± 7.2 | Recreational athletes (swimming) | Labral repair, femoral osteochondroplasty, acetabular rim trimming (T-capsulotomy) | 4-phase rehabilitation protocol lasting an average of 32 weeks | 2 years minimum. 100% of patients returned to swimming, on average 3.4 ± 1.7 months after surgery (54% higher level, 38% same level as before, 7% lower level). All patients showed significant improvements in PROs (p < 0.05). |
| Waterman et al. 2018 [22] | Case series | 29 | 36 ± 11.9 | Recreational athletes (golf) | Labral repair, femoral osteochondroplasty, acetabular rim trimming, capsular closure | 16 to 20 weeks of a 4-phased postoperative rehabilitation program | 2 years minimum. 97% of golf players returned to sports, and 55% of them noted improvement from preinjury performances. |
| Levy et al. 2016 [23] | Case series | 51 | 26.3 ± 7.8 | Amateur athletes (running) | Labral repair, femoral osteochondroplasty, acetabular rim trimming | 4-phase rehabilitation protocol lasting 32 weeks | Minimum 2 years. 94% of patients returned to running, on average 8.5 months after surgery.Significant improvement of HOS-ADL (p < 0.001), HOS-SS (p > 0.001), and mHHS (p < 0.001). |
| Riff et al. 2018 [2] | Case series | 32 | 34.7 ± 6.9 | Amateur athletes (fitness) | Labral repair, femoral osteochondroplasty, acetabular rim trimming, and capsular closure | 4-phase rehabilitation protocol lasting a mean of 32 weeks. | 2 years minimum (27 +/− 6 months). 88% of patients returned to sport, and 44% of them noted improvement from preinjury performances. All patients demonstrated significant improvements in PROs (p < 0.05). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monselli, C.; Bianco Prevot, L.; Accetta, R.; Tronconi, L.P.; Bolcato, V.; Basile, G. State of the Art in Rehabilitation Strategies After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: A Systematic Review. J. Clin. Med. 2024, 13, 7302. https://doi.org/10.3390/jcm13237302
Monselli C, Bianco Prevot L, Accetta R, Tronconi LP, Bolcato V, Basile G. State of the Art in Rehabilitation Strategies After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: A Systematic Review. Journal of Clinical Medicine. 2024; 13(23):7302. https://doi.org/10.3390/jcm13237302
Chicago/Turabian StyleMonselli, Claudio, Luca Bianco Prevot, Riccardo Accetta, Livio Pietro Tronconi, Vittorio Bolcato, and Giuseppe Basile. 2024. "State of the Art in Rehabilitation Strategies After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: A Systematic Review" Journal of Clinical Medicine 13, no. 23: 7302. https://doi.org/10.3390/jcm13237302
APA StyleMonselli, C., Bianco Prevot, L., Accetta, R., Tronconi, L. P., Bolcato, V., & Basile, G. (2024). State of the Art in Rehabilitation Strategies After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: A Systematic Review. Journal of Clinical Medicine, 13(23), 7302. https://doi.org/10.3390/jcm13237302








