Effects of Supervised Rehabilitation on Psychosocial and Participation-Related Outcomes After Lumbar Spine Surgery: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Strategy
2.2. Study Selection
2.3. Data Extraction and Risk of Bias Assessment
2.4. Data Synthesis
3. Results
3.1. Study Characteristics
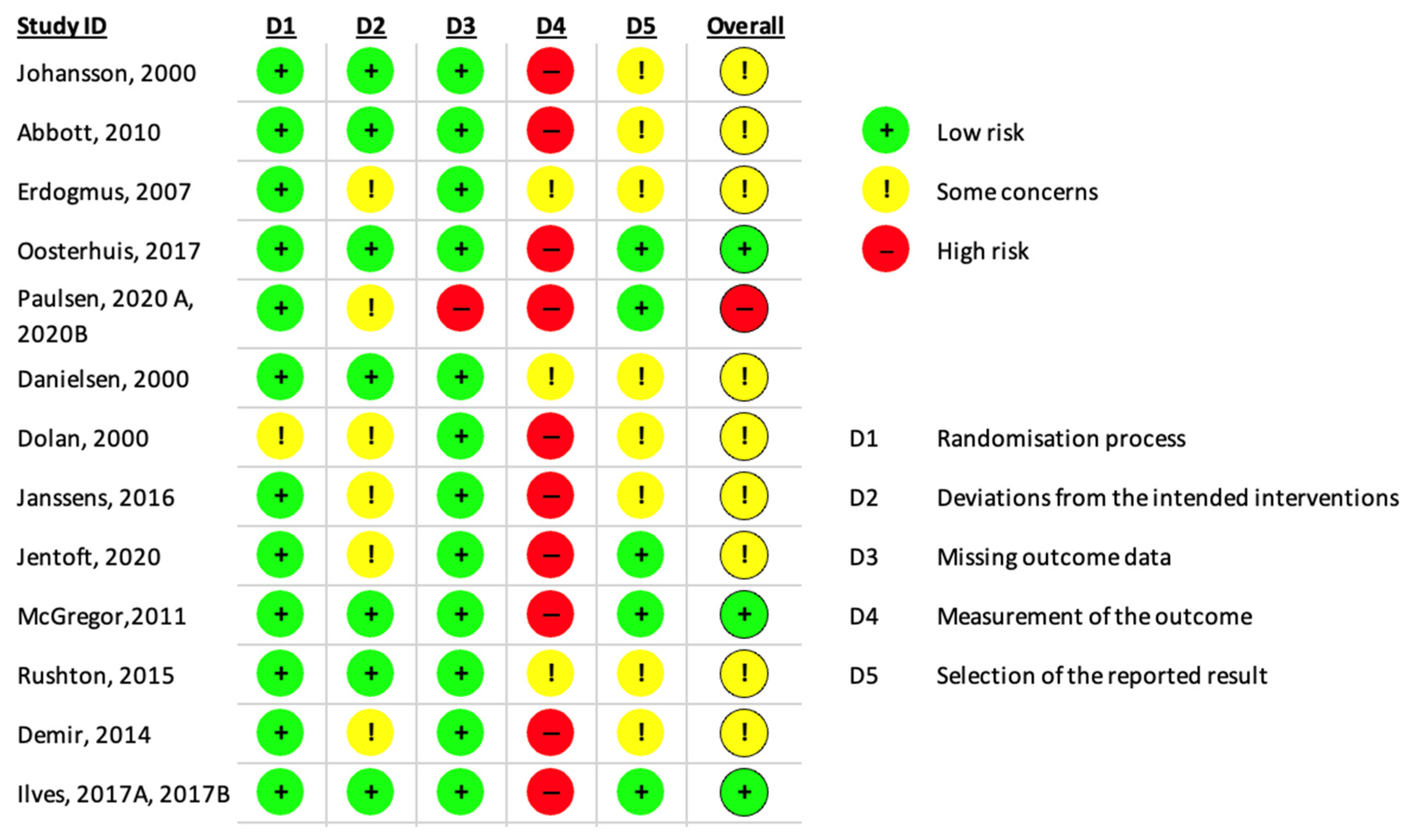
3.2. Risk of Bias
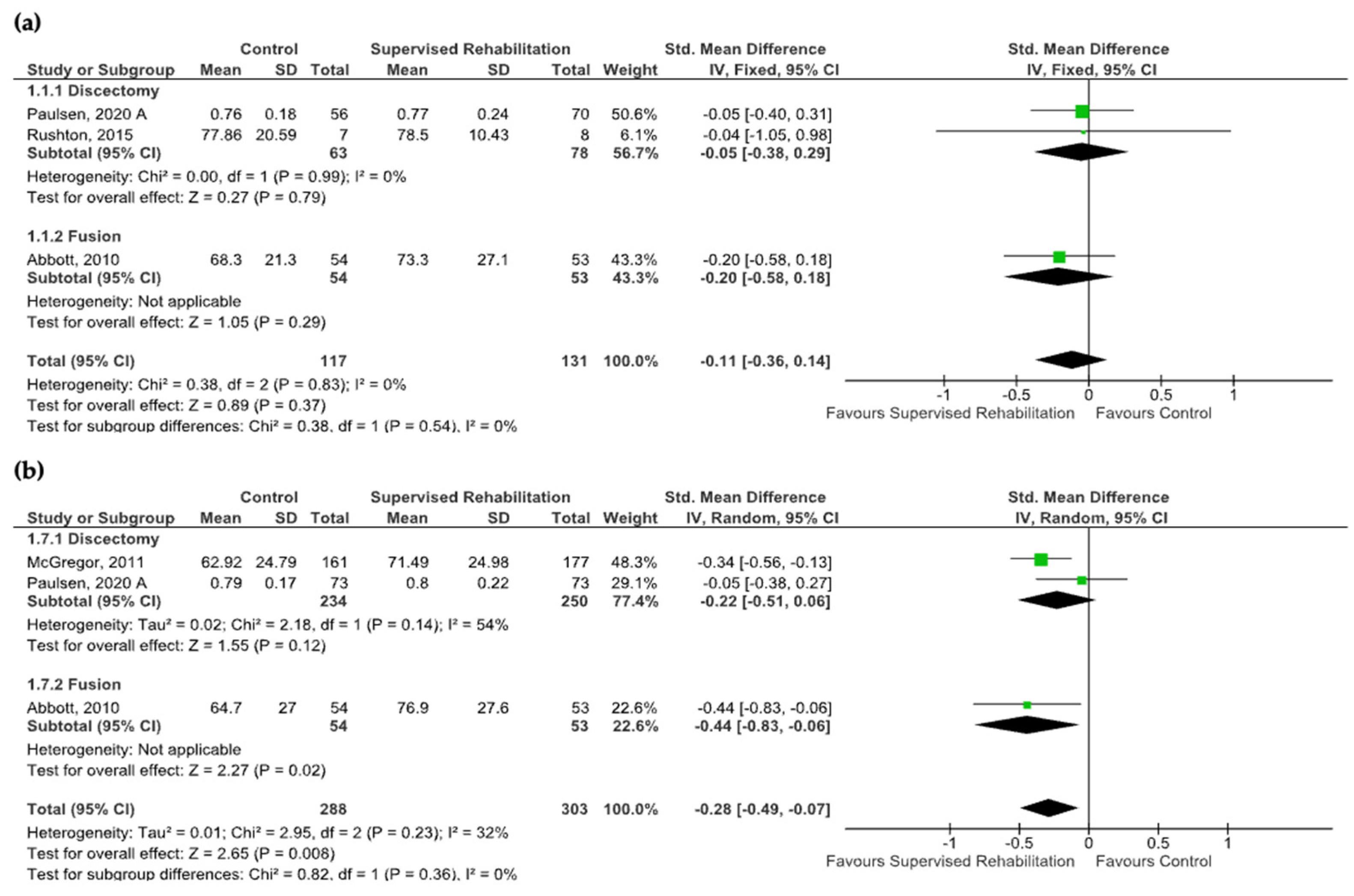
3.3. Quality of Life
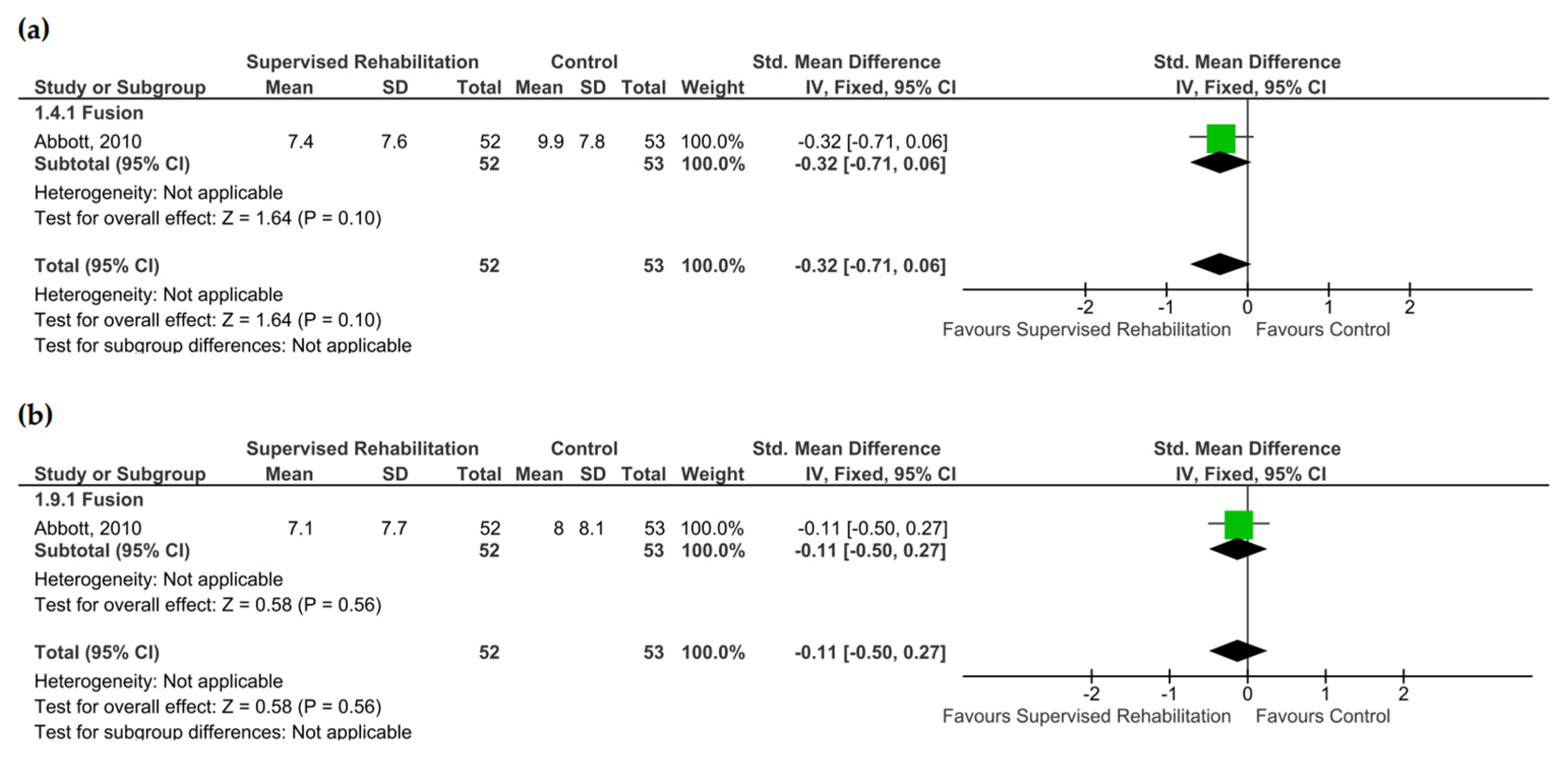
3.4. Fear-Avoidance Belief
3.5. Catastrophizing and Self-Efficacy
3.6. Anxiety and Depression
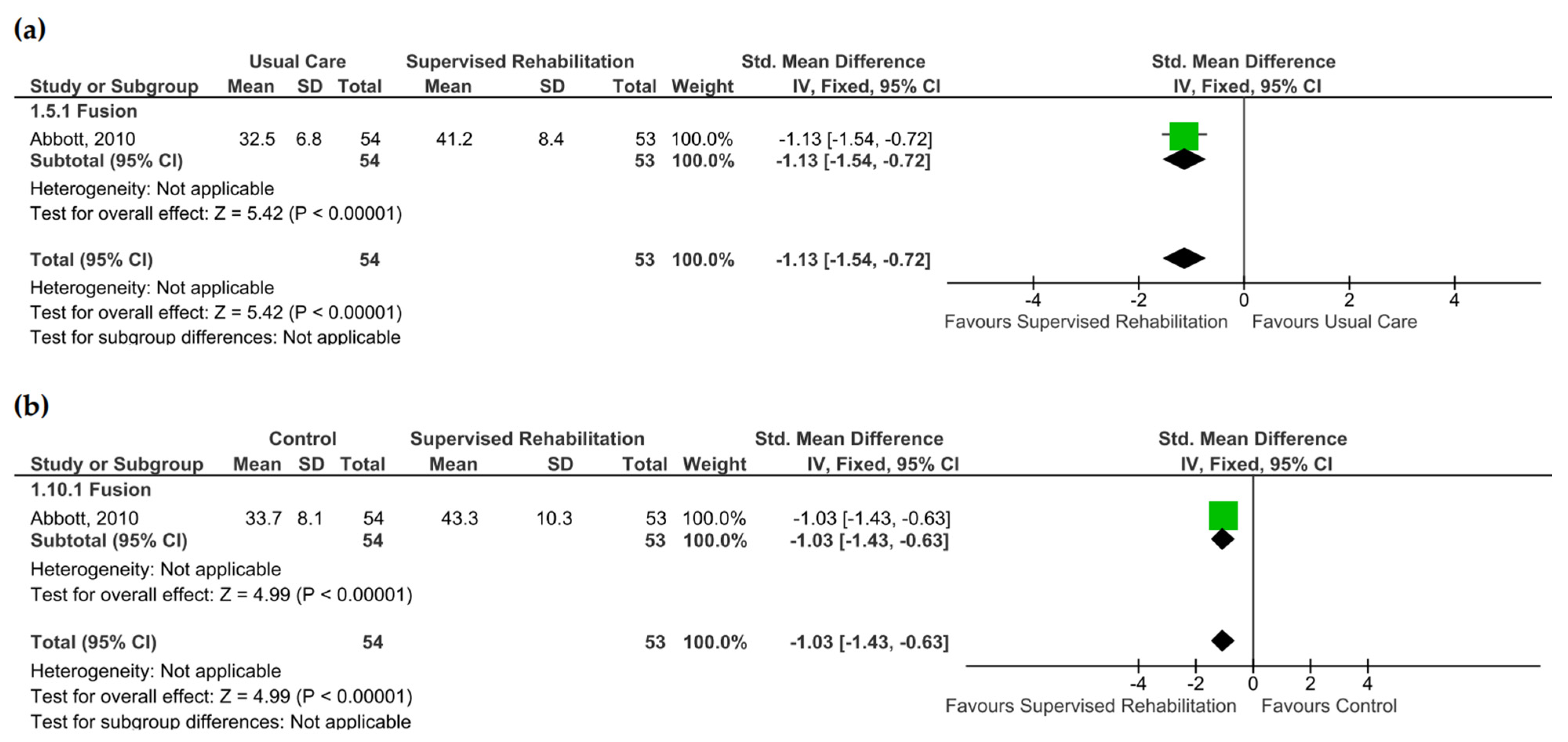
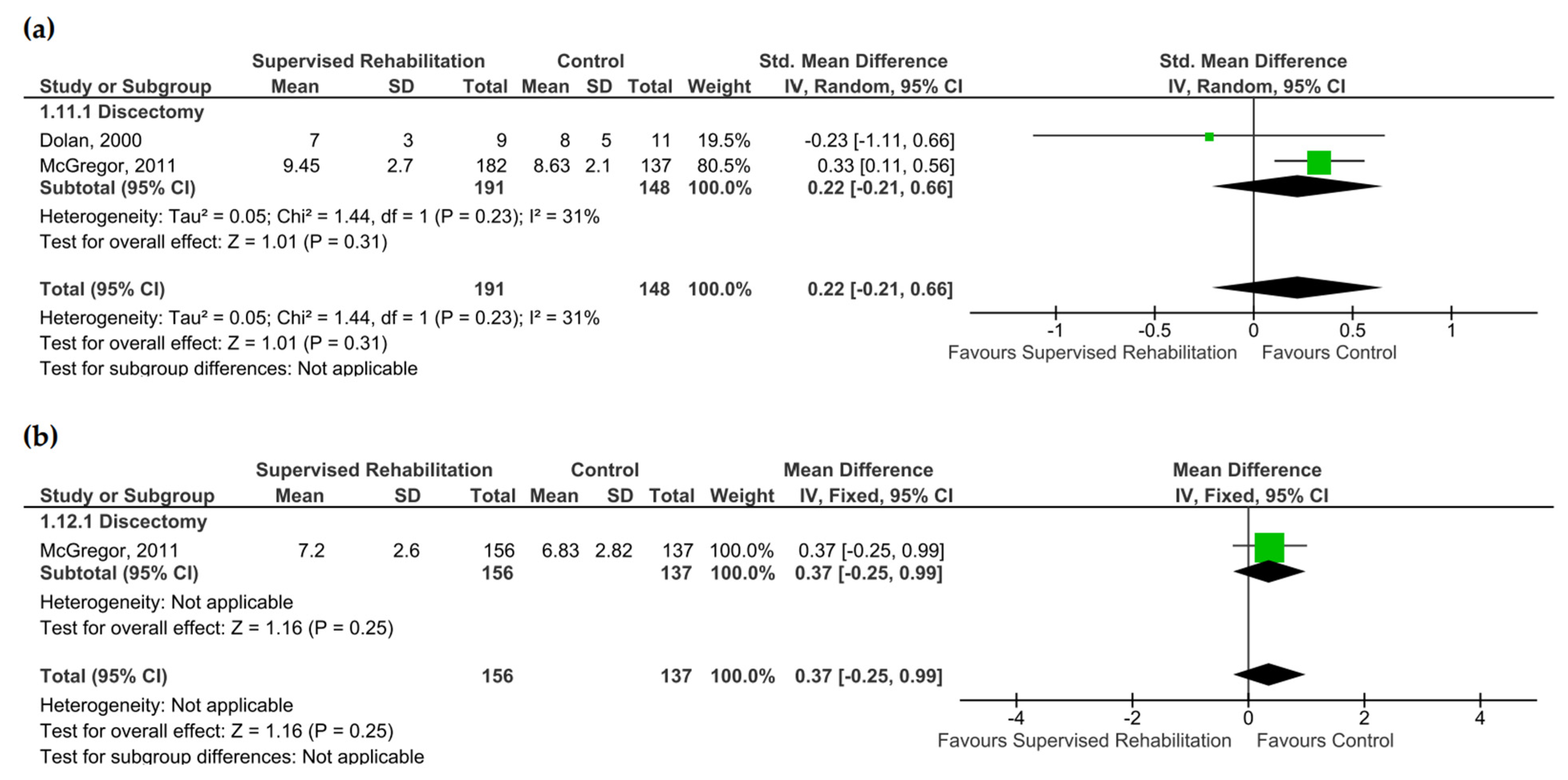
3.7. Return to Work
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2021 Low Back Pain Collaborators. Global, Regional, and National Burden of Low Back Pain, 1990–2020, Its Attributable Risk Factors, and Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e316–e329. [Google Scholar] [CrossRef] [PubMed]
- Linaker, C.; Harris, E.C.; Cooper, C.; Coggon, D.; Palmer, K.T. The burden of sickness absence from musculoskeletal causes in Great Britain. Occup. Med. 2011, 61, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Impellizzeri, F.M.; Leunig, M.; Jeszenszy, D.; Becker, H.; Haschtmann, D.; Preiss, S.; Fekete, F.T. EUROSPINE 2017 FULL PAPER AWARD: Time to remove our rose-tinted spectacles: A candid appraisal of the relative success of surgery in over 4500 patients with degenerative disorders of the lumbar spine, hip or knee. Eur. Spine J. 2018, 27, 778–788. [Google Scholar] [CrossRef]
- Oosterhuis, T.; Costa, L.O.; Maher, C.G.; de Vet, H.C.; van Tulder, M.W.; Ostelo, R.W. Rehabilitation after lumbar disc surgery. Cochrane Database Syst. Rev. 2014, 2014, CD003007. [Google Scholar] [CrossRef]
- Santagostino, A.M.; Cannizzaro, D.; Soekeland, F.; Mancin, S.; Mazzoleni, B. Pain and Quality of Life in Patients Undergoing Lumbar Arthrodesis for Degenerative Spondylolisthesis: A Systematic Review. World Neurosurg. 2023, 177, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J.; Shaw, W.S. Impact of psychological factors in the experience of pain. Phys. Ther. 2011, 91, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Wilson, H.D.; Cahana, A. Treatment of chronic non-cancer pain. Lancet 2011, 377, 2226–2235. [Google Scholar] [CrossRef]
- Manni, T.; Ferri, N.; Vanti, C.; Ferrari, S.; Cuoghi, I.; Gaeta, C.; Sgaravatti, I.; Pillastrini, P. Rehabilitation after lumbar spine surgery in adults: A systematic review with meta-analysis. Arch. Physiother. 2023, 13, 21. [Google Scholar] [CrossRef]
- Özden, F. The Effect of Exercise Interventions After Lumbar Decompression Surgery: A Systematic Review and Meta-Analysis. World Neurosurg. 2022, 167, e904–e921. [Google Scholar] [CrossRef]
- Özden, F. The Effectiveness of Physical Exercise After Lumbar Fusion Surgery: A Systematic Review and Meta-Analysis. World Neurosurg. 2022, 163, e396–e412. [Google Scholar] [CrossRef]
- Monticone, M.; Ferrante, S.; Teli, M.; Rocca, B.; Foti, C.; Lovi, A.; Bruno, M.B. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur. Spine J. 2014, 23, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Russo, F.; Papalia, G.F.; Diaz Balzani, L.A.; Stelitano, G.; Zampogna, B.; Fontana, L.; Vadalà, G.; Iavicoli, S.; Papalia, R.; Denaro, V. Prognostic factors for return to work in patients affected by chronic low back pain: A systematic review. Musculoskelet. Surg. 2024, 108, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Murlow, C.; Gotzsche, P.; Ioannidis, J.P.; Clarke, M.; Devereaux, J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; Emberson, J.R.; Hernán, M.A.; Hopewell, S.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Li, T.; Deeks, J.J. (Eds.) Chapter 8: Assessing risk of bias in a randomized trial [last updated October 2019]. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.5; Cochrane: Hoboken, NJ, USA, 2024. [Google Scholar]
- Sullivan, G.M.; Feinn, R. Using Effect Size-or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Danielsen, J.M.; Johnsen, R.; Kibsgaard, S.K.; Hellevik, E. Early aggressive exercise for postoperative rehabilitation after discectomy. Spine 2000, 25, 1015–1020. [Google Scholar] [CrossRef]
- Dolan, P.; Greenfield, K.; Nelson, R.J.; Nelson, I.W. Can exercise therapy improve the outcome of microdiscectomy? Spine 2000, 25, 1523–1532. [Google Scholar] [CrossRef]
- Erdogmus, C.B.; Resch, K.L.; Sabitzer, R.; Müller, H.; Nuhr, M.; Schöggl, A.; Posch, M.; Osterode, W.; Ungersböck, K.; Ebenbichler, G.R. Physiotherapy-based rehabilitation following disc herniation operation: Results of a randomized clinical trial. Spine 2007, 32, 2041–2049. [Google Scholar] [CrossRef]
- Johansson, A.C.; Linton, S.J.; Bergkvist, L.; Nilsson, O.; Cornefjord, M. Clinic-based training in comparison to home-based training after first-time lumbar disc surgery: A randomised controlled trial. Eur. Spine J. 2009, 18, 398–409. [Google Scholar] [CrossRef]
- Abbott, A.D.; Tyni-Lenné, R.; Hedlund, R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: A randomized controlled trial. Spine 2010, 35, 848–857. [Google Scholar] [CrossRef]
- McGregor, A.H.; Doré, C.J.; Morris, T.P.; Morris, S.; Jamrozik, K. ISSLS prize winner: Function After Spinal Treatment, Exercise, and Rehabilitation (FASTER): A factorial randomized trial to determine whether the functional outcome of spinal surgery can be improved. Spine 2011, 36, 1711–1720. [Google Scholar] [CrossRef] [PubMed]
- Demir, S.; Dulgeroglu, D.; Cakci, A. Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. Randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2014, 50, 627–640. [Google Scholar]
- Rushton, A.; Heneghan, N.R.; Calvert, M.; Heap, A.; White, L.; Goodwin, P.C. Physiotherapy Post Lumbar Discectomy: Prospective Feasibility and Pilot Randomised Controlled Trial. PLoS ONE 2015, 10, e0142013. [Google Scholar] [CrossRef] [PubMed]
- Janssens, L.; Brumagne, S.; Claeys, K.; Pijnenburg, M.; Goossens, N.; Rummens, S.; Depreitere, B. Proprioceptive use and sit-to-stand-to-sit after lumbar microdiscectomy: The effect of surgical approach and early physiotherapy. Clin. Biomech. 2016, 32, 40–48. [Google Scholar] [CrossRef]
- Ilves, O.; Häkkinen, A.; Dekker, J.; Wahlman, M.; Tarnanen, S.; Pekkanen, L.; Ylinen, J.; Kautiainen, H.; Neva, M. Effectiveness of postoperative home-exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: A randomized controlled trial. J. Rehabil. Med. 2017, 49, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Ilves, O.; Häkkinen, A.; Dekker, J.; Pekkanen, L.; Piitulainen, K.; Järvenpää, S.; Marttinen, I.; Vihtonen, K.; Neva, M.H. Quality of life and disability: Can they be improved by active postoperative rehabilitation after spinal fusion surgery in patients with spondylolisthesis? A randomised controlled trial with 12-month follow-up. Eur. Spine J. 2017, 26, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Oosterhuis, T.; Ostelo, R.W.; van Dongen, J.M.; Peul, W.C.; de Boer, M.R.; Bosmans, J.E.; Vleggeert-Lankamp, C.L.; Art, M.P.; van Tulder, M.W. Early rehabilitation after lumbar disc surgery is not effective or cost-effective compared to no referral: A randomised trial and economic evaluation. J. Physiother. 2017, 63, 144–153. [Google Scholar] [CrossRef]
- Jentoft, E.S.; Kvåle, A.; Assmus, J.; Moen, V.P. Effect of information and exercise programmes after lumbar disc surgery: A randomized controlled trial. Physiother. Res. Int. 2020, 25, e1864. [Google Scholar] [CrossRef]
- Paulsen, R.T.; Carreon, L.Y.; Andersen, M.Ø. Patient-reported Outcomes After Surgery for Lumbar Disc Herniation, a Randomized Controlled Trial Comparing the Effects of Referral to Municipal Physical Rehabilitation Versus No Referral. Spine 2020, 45, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, R.T.; Rasmussen, J.; Carreon, L.Y.; Andersen, M.Ø. Return to work after surgery for lumbar disc herniation, secondary analyses from a randomized controlled trial comparing supervised rehabilitation versus home exercises. Spine J. 2020, 20, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Staszkiewicz, R.; Ulasavets, U.; Dobosz, P.; Drewniak, S.; Niewiadomska, E.; Grabarek, B.O. Assessment of quality of life, pain level and disability outcomes after lumbar discectomy. Sci. Rep. 2023, 13, 6009. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy. In Encyclopedia of Human Behavior; Ramachaudran, V.S., Ed.; Academic Press: New York, NY, USA, 1994; Volume 4, pp. 71–81. [Google Scholar]
- Zampolini, M.; Selb, M.; Boldrini, P.; Branco, C.A.; Golyk, V.; Hu, X.; Kiekens, C.; Negrini, S.; Nulle, A.; Oral, A.; et al. The Individual Rehabilitation Project as the core of person-centered rehabilitation: The Physical and Rehabilitation Medicine Section and Board of the European Union of Medical Specialists Framework for Rehabilitation in Europe. Eur. J. Phys. Rehabil. Med. 2022, 58, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Potcovaru, C.G.; Salmen, T.; Bîgu, D.; Săndulescu, M.I.; Filip, P.V.; Diaconu, L.S.; Pop, C.; Ciobanu, I.; Cinteză, D.; Berteanu, M. Assessing the Effectiveness of Rehabilitation Interventions through the World Health Organization Disability Assessment Schedule 2.0 on Disability—A Systematic Review. J. Clin. Med. 2024, 13, 1252. [Google Scholar] [CrossRef] [PubMed]
- Fenn, K.; Byrne, M. The key principles of cognitive behavioural therapy. InnovAiT 2013, 6, 579–585. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Bushnell, M.C.; Treede, R.D.; Zubieta, J.K. Human brain mechanisms of pain perception and regulation inhealth and disease. Eur. J. Pain 2005, 9, 463–484. [Google Scholar] [CrossRef]
- Wiech, K.; Ploner, M.; Tracey, I. Neurocognitive aspects of pain perception. Trends Cogn. Sci 2008, 12, 306–313. [Google Scholar] [CrossRef]
- Baliki, M.N.; Mansour, A.R.; Baria, A.T.; Apkarian, A.V. Functional reorganization of the default mode network across chronic pain conditions. PLoS ONE 2014, 9, e106133. [Google Scholar] [CrossRef]
- Bekeris, J.; Wilson, L.A.; Fiasconaro, M.; Poeran, J.; Liu, J.; Girardi, F.; Memtsoudis, S.G. New Onset Depression and Anxiety After Spinal Fusion Surgery: Incidence and Risk Factors. Spine 2020, 45, 1161–1169. [Google Scholar] [CrossRef]
- Atarod, M.; Mirzamohammadi, E.; Ghandehari, H.; Mehrdad, R.; Izadi, N. Predictive factors for return to work after lumbar discectomy. Int. J. Occup. Saf. Ergon. 2019, 27, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Hebert, J.J.; Abraham, E.; Vandewint, A.; Bigney, E.; Richardson, E.; El-Mughayyar, D.; Attabib, N.; Wedderkopp, N.; Kingwell, S.; et al. Postoperative recovery patterns following discectomy surgery in patients with lumbar radiculopathy. Sci. Rep. 2022, 12, 11146. [Google Scholar] [CrossRef] [PubMed]
- Halvorson, R.T.; Torres-Espin, A.; Callahan, M.; Tay, B.; O’Neill, C.; Berven, S.; Lotz, J.C.; Bailey, J.F. Multi-domain biopsychosocial postoperative recovery trajectories associate with patient outcomes following lumbar fusion. Eur. Spine J. 2023, 32, 1429–1436. [Google Scholar] [CrossRef] [PubMed]



| Author, Year [Reference] | No. Patients and Gender | Experimental Group | Control Group | Timing of Treatment Start | Outcome Measures and Timepoint |
|---|---|---|---|---|---|
| Danielsen et al., 2000 [19] | 63 patients after discectomy M/F: 41/66 | Supervised strength exercises for lumbar muscles, core muscles, and lower limb muscles for 8 weeks. | Information on the self-management of the first 2 months postoperative pathway and home-based exercise training program. | 4 weeks after surgery. | Return to work (sick leave period). |
| Dolan et al., 2000 [20] | 20 patients after discectomy M/F: 17/3 | Supervised aerobic exercises, stretching, and lumbar extension exercises for 8 weeks. | Usual postoperative care and information about exercises and return to work management. | 6 weeks after surgery. | 1 year: - Zung Depression Scale. |
| Erdogmus et al., 2007 [21] | 99 patients after discectomy M/F: 67/32 | Supervised strength training and mobilization, stretching and stabilization exercises, ergonomic activities, and work-return advice for 12 weeks. | No treatment. | 1 week after surgery. | 6 months: - Return to work (Yes/No). |
| Johansson et al., 2009 [22] | 59 patients after discectomy M/F: 35/24 | Supervised exercises with positive reinforcement of healthy behaviors for 8 weeks. | Home-based unsupervised exercises with recommendations on gradual increases in exercise intensity. | 2 weeks after surgery. | 1 year: - EQ-5D VAS - TSK - CSQ-CAT. |
| Abbott et al., 2010 [23] | 107 patients after spinal fusion M/F: 41/66 | Supervised sessions with education for modifying maladaptive pain cognition, behavior, and performance of motor control exercise, plus home-based exercises for 12 weeks. | Home-based exercise program. | Hospital discharge (not specified). | 6 months: - EQ-5D - TSK - SES - CSQ-CAT. 1 year: - EQ-5D - TSK - SES - CSQ-CAT. |
| McGregor et al., 2011 [24] | 338 patients after discectomy M/F: 159/179 | Group 1: supervised stretching, strength training, aerobic training, endurance, and ergonomic exercises for 6 weeks. Group 2: performance of the same exercises as Group 1 for 6 weeks plus informational booklet. | Group 1: information booklet. Group 2: Usual care according to advice delivered by the surgeon. | 6–8 weeks after surgery. | 1 year: - EQ-5D VAS - FAB-Q - HADS. |
| Demir et al., 2014 [25] | 44 patients after discectomy M/F: 24/20 | Supervised dynamic lumbar stabilization exercises for 4 weeks. | Home-based exercise program, including stretching, pelvic tilt mobilization, flexion, and extension exercises for 4 weeks. | 4 weeks after surgery. | 6 months: - Nottingham Health Profile - FAB-Q - Return to work (sick leave period). |
| Rushton et al., 2015 [26] | 59 patients after discectomy M/F: 28/31 | Supervised treatment including education, advice, mobility, and core stability exercises for 8 weeks. | Leaflet regarding anatomical and surgical information, advice on progressive exercises execution, and answers to frequently asked questions. | 4 weeks after surgery. | 6 months: - EQ-5D - TSK - Return to work (Yes/No). |
| Janssens et al., 2016 [27] | 25 patients after discectomy M/F: 11/14 | Supervised sessions focused on correction of sitting posture, deep abdominal muscles exercises, neurodynamic exercises, and segmental thoracolumbar mobilization for 2 weeks. | Ergonomic advice and the “stay active” advice. | 2 weeks after surgery. | 6 months: - TSK 1 year: - TSK - Return to work (sick leave period). |
| Ilves et al., 2017 (A) [28] and Ilves et al., 2017 (B) [29] | 98 patients after spinal fusion M/F: 72/26 | Supervised sessions with a physiotherapist and home-based program focused on back-specific exercises and aerobic exercises for 52 weeks. | Instructions for standard home-based exercises. | 12 weeks after surgery. | 1 year: - RAND-36 (A) - TSK (B). |
| Oosterhuis et al., 2017 [30] | 169 patients after discectomy M/F: 71/98 | Supervised usual postoperative exercises for 6–8 weeks. | No postoperative rehabilitation. | 3 days after surgery. | 6 months - SF-12. |
| Jentoft et al., 2020 [31] | 70 patients after discectomy M/F: 44/26 | Supervised stretching and muscle coordination exercises, strength training for 18–20 weeks, and education at discharge. | Educational session at discharge on spine anatomy, pain physiology, surgery intervention, and suggested postoperative activities. | At discharge. | 1 year: - TKS. |
| Paulsen et al., 2020 (A) [32] and Paulsen et al., 2020 (B) [33] | 146 patients after discectomy M/F: 92/54 | Supervised spinal stability exercises for 6–12 weeks. | No postoperative rehabilitation. | 4–6 weeks after surgery. | 6 months: - EQ-5D (A) - Return to work (Yes/No) (B). 1 year: - EQ-5D (A) - Return to work (Yes/No) (B). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scandelli, F.; De Leo, D.; Marino, G.; De Martino, E.; Cannizzaro, D.; Adamo, P.; Temporiti, F. Effects of Supervised Rehabilitation on Psychosocial and Participation-Related Outcomes After Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 7246. https://doi.org/10.3390/jcm13237246
Scandelli F, De Leo D, Marino G, De Martino E, Cannizzaro D, Adamo P, Temporiti F. Effects of Supervised Rehabilitation on Psychosocial and Participation-Related Outcomes After Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(23):7246. https://doi.org/10.3390/jcm13237246
Chicago/Turabian StyleScandelli, Francesco, Davide De Leo, Giorgia Marino, Emanuela De Martino, Delia Cannizzaro, Paola Adamo, and Federico Temporiti. 2024. "Effects of Supervised Rehabilitation on Psychosocial and Participation-Related Outcomes After Lumbar Spine Surgery: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 23: 7246. https://doi.org/10.3390/jcm13237246
APA StyleScandelli, F., De Leo, D., Marino, G., De Martino, E., Cannizzaro, D., Adamo, P., & Temporiti, F. (2024). Effects of Supervised Rehabilitation on Psychosocial and Participation-Related Outcomes After Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(23), 7246. https://doi.org/10.3390/jcm13237246