No Effect of Cigarette Smoking in the Outcome of Arthroscopic Management for Femoroacetabular Impingement: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
- P (Problem): FAI;
- I (Intervention): arthroscopy;
- C (Comparison): smokers vs. nonsmokers;
- O (Outcomes): complications and PROMs;
- T (Timings): minimum 24 months of follow-up;
- D (Design): clinical study.
2.3. Selection and Data Collection
2.4. Data Items
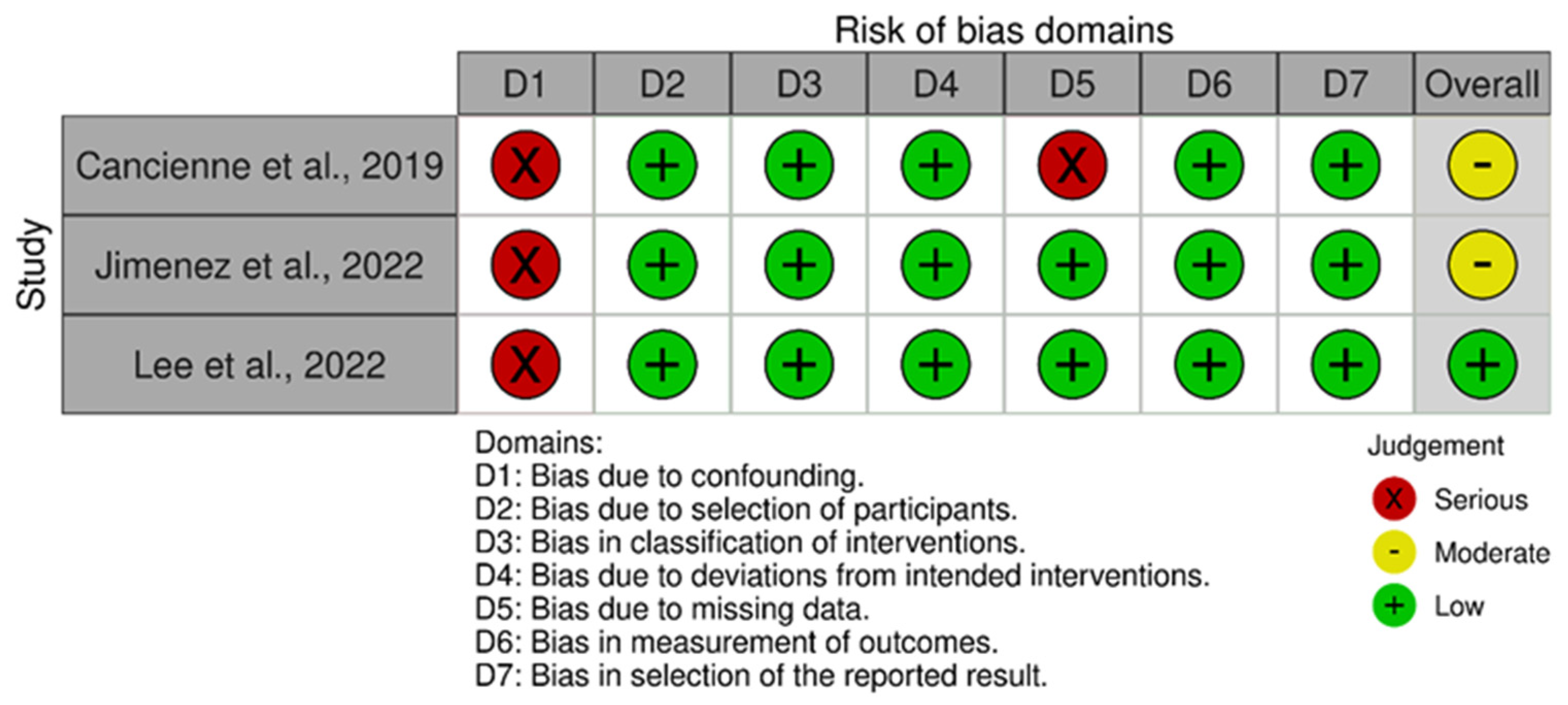
2.5. Assessment of the Risk of Bias
2.6. Synthesis Methods
3. Results
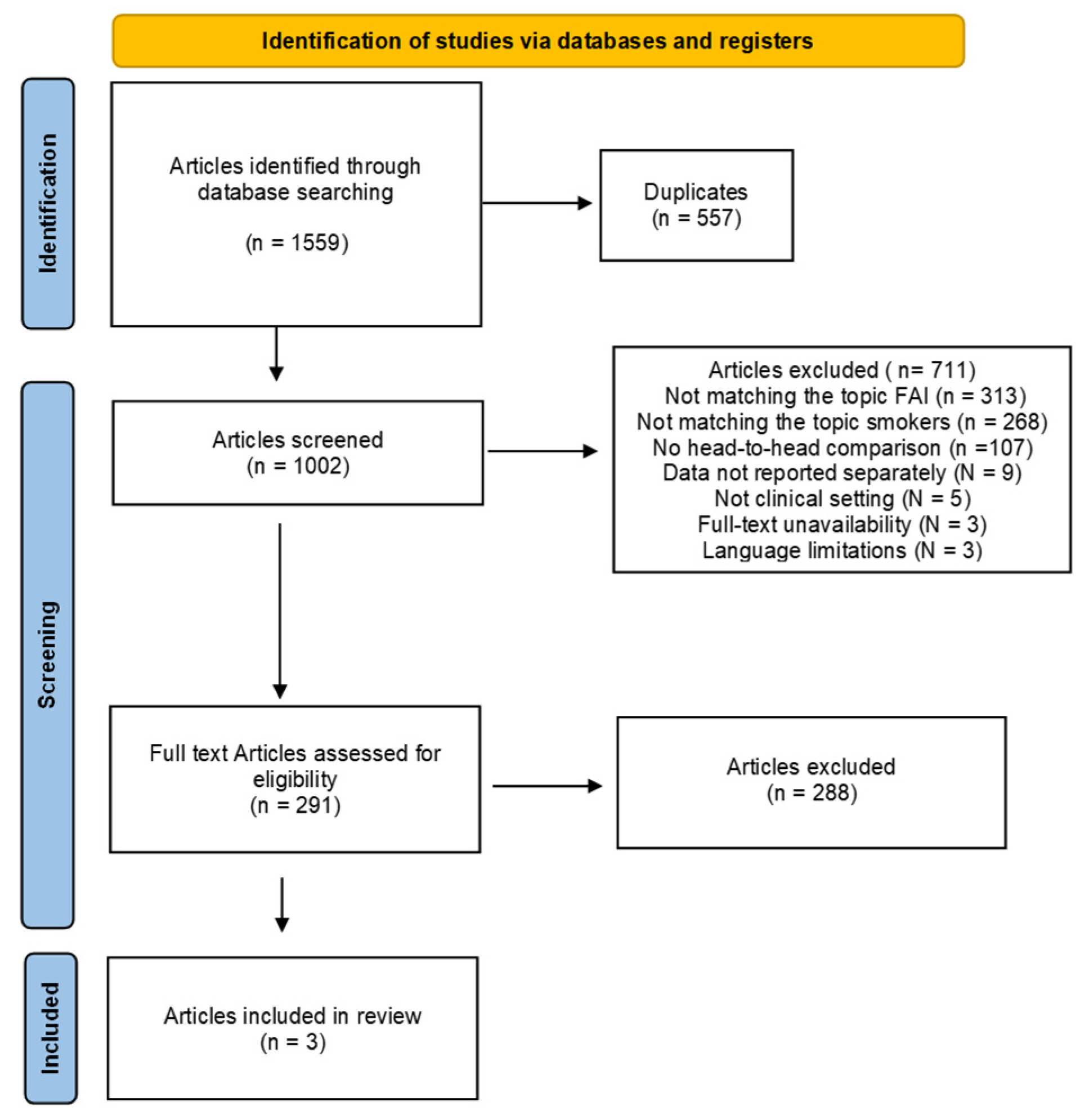
3.1. Study Selection
3.2. Risk of Bias Assessment
3.3. Study Characteristics and Results of Individual Studies
3.4. Baseline Comparability
3.5. Synthesis of Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Langhout, R.; Weir, A.; Litjes, W.; Gozeling, M.; Stubbe, J.H.; Kerkhoffs, G.; Tak, I. Hip and groin injury is the most common non-time-loss injury in female amateur football. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3133–3141. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Del Buono, A.; Franceschi, F.; Marinozzi, A.; Maffulli, N.; Denaro, V. Femoroacetabular impingement syndrome management: Arthroscopy or open surgery? Int. Orthop. 2012, 36, 903–914. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Migliorini, F.; Liu, Y.; Eschweiler, J.; Baroncini, A.; Tingart, M.; Maffulli, N. Increased range of motion but otherwise similar clinical outcome of arthroscopy over open osteoplasty for femoroacetabular impingement at midterm follow-up: A systematic review. Surgeon 2022, 20, 194–208. [Google Scholar] [CrossRef]
- Lavigne, M.; Parvizi, J.; Beck, M.; Siebenrock, K.A.; Ganz, R.; Leunig, M. Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. Clin. Orthop. Relat. Res. 2004, 418, 61–66. [Google Scholar] [CrossRef]
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin. Orthop. Relat. Res. 2003, 417, 112–120. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N.; Baroncini, A.; Eschweiler, J.; Tingart, M.; Betsch, M. Revision Surgery and Progression to Total Hip Arthroplasty After Surgical Correction of Femoroacetabular Impingement: A Systematic Review. Am. J. Sports Med. 2022, 50, 1146–1156. [Google Scholar] [CrossRef]
- Wagner, M.; Lindtner, R.A.; Schaller, L.; Schmaranzer, F.; Schmaranzer, E.; Vavron, P.; Endstrasser, F.; Brunner, A. Hip arthroscopy with initial access to the peripheral compartment for femoroacetabular impingement: Midterm results from a large-scale patient cohort. J. Orthop. Traumatol. 2024, 25, 29. [Google Scholar] [CrossRef]
- Smith-Petersen, M.N. The classic: Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. Clin. Orthop. Relat. Res. 2009, 467, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Ganz, R.; Gill, T.J.; Gautier, E.; Ganz, K.; Krügel, N.; Berlemann, U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J. Bone Jt. Surg. Br. 2001, 83, 1119–1124. [Google Scholar] [CrossRef]
- Hadeed, M.M.; Cancienne, J.M.; Gwathmey, F.W. Pincer Impingement. Clin. Sports Med. 2016, 35, 405–418. [Google Scholar] [CrossRef]
- Li, Y.; Helvie, P.; Mead, M.; Gagnier, J.; Hammer, M.R.; Jong, N. Prevalence of Femoroacetabular Impingement Morphology in Asymptomatic Adolescents. J. Pediatr. Orthop. 2017, 37, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Trigg, S.D.; Schroeder, J.D.; Hulsopple, C. Femoroacetabular Impingement Syndrome. Curr. Sports Med. Rep. 2020, 19, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Hwang, D.S.; Kim, S.B.; Kang, C.; Hwang, J.M.; Lee, G.S.; Park, E.J. The role and clinical relevance of the ligamentum teres: Long-term outcomes after hip arthroscopic surgery of cam-type femoroacetabular impingement. J. Hip Preserv. Surg. 2021, 8, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Melugin, H.P.; Hale, R.F.; Song, B.M.; Okoroha, K.R.; Levy, B.A.; Krych, A.J. Sex differences in the prevalence of radiographic findings of structural hip deformities in patients with symptomatic femoroacetabular impingement. J. Hip Preserv. Surg. 2021, 8, 233–239. [Google Scholar] [CrossRef]
- Goriainov, V.; Chapman, L.; Hindi, F.; Langdown, A.J. Preoperative Dynamic Hip Examination Under Fluoroscopic Guidance Enhances the Understanding of Femoroacetabular Impingement Pathology and Treatment Planning. Arthrosc. Sports Med. Rehabil. 2021, 3, e1599–e1606. [Google Scholar] [CrossRef]
- Metz, A.K.; Aoki, S.K. Editorial Commentary: Not Yet Convinced That the Femoroacetabular Impingement Resection (Fair) Arc Measurement Provides a “Fair” Assessment of Cam Resection Principles. Arthroscopy 2021, 37, 3466–3468. [Google Scholar] [CrossRef]
- Tassinari, E.; Mariotti, F.; Castagnini, F.; Lucchini, S.; Perdisa, F.; Bracci, G.; Cosentino, M.; Bordini, B.; Traina, F. Isolated arthroscopic treatment of intra-articular pathologies in mild hip dysplasia: A short-term case control study. J. Exp. Orthop. 2021, 8, 112. [Google Scholar] [CrossRef]
- Wirries, N.; Heinrich, G.; Derksen, A.; Budde, S.; Floerkemeier, T.; Windhagen, H. Is a Femoro-Acetabular Impingement Type Cam Predictable after Slipped Capital Femoral Epiphysis? Children 2021, 8, 992. [Google Scholar] [CrossRef]
- Maldonado, D.R.; Owens, J.S.; Jimenez, A.E.; Saks, B.R.; Lall, A.C.; Domb, B.G. Endoscopic Shelf Procedure and Ischiofemoral Decompression with Arthroscopic Acetabular Labral Reconstruction: A Case Report. JBJS Case Connect. 2021, 11, e21. [Google Scholar] [CrossRef]
- Arner, J.W. Editorial Commentary: Femoroplasty May Not Be Necessary in All Patients with Hip Femoroacetabular Impingement, But Cam Lesions Should Not Be Ignored in Patients with Significant Femoral Head-Neck Offset. Arthroscopy 2021, 37, 3295–3296. [Google Scholar] [CrossRef]
- Lerch, T.D.; Boschung, A.; Schmaranzer, F.; Todorski, I.A.S.; Vanlommel, J.; Siebenrock, K.A.; Steppacher, S.D.; Tannast, M. Lower pelvic tilt, lower pelvic incidence, and increased external rotation of the iliac wing in patients with femoroacetabular impingement due to acetabular retroversion compared to hip dysplasia. Bone Jt. Open 2021, 2, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Catelli, D.S.; Kowalski, E.; Beaule, P.E.; Lamontagne, M. Muscle and Hip Contact Forces in Asymptomatic Men with Cam Morphology During Deep Squat. Front. Sports Act. Living 2021, 3, 716626. [Google Scholar] [CrossRef] [PubMed]
- Shimamura, M.; Iwata, K.; Fujiki, T.; Mashiba, T.; Yamamoto, T. Eccentric Rotational Acetabular Osteotomy Using Computed Navigation Guidance for Developmental Dysplasia of the Hip, Sacroiliac Fusion, and Femoroacetabular Impingement Owing to Acetabular Retroversion: A Case Report. Orthop. Surg. 2021, 13, 2177–2181. [Google Scholar] [CrossRef] [PubMed]
- Addai, D.; Zarkos, J.; Pettit, M.; Sunil Kumar, K.H.; Khanduja, V. Outcomes following surgical management of femoroacetabular impingement: A systematic review and meta-analysis of different surgical techniques. Bone Jt. Res. 2021, 10, 574–590. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Maffulli, N.; Bell, A.; Cuozzo, F.; Hildebrand, F.; Weber, C.D. Midterm results after arthroscopic femoral neck osteoplasty combined with labral debridement for cam type femoroacetabular impingement in active adults. J. Orthop. Surg. Res. 2023, 18, 67. [Google Scholar] [CrossRef]
- Lerch, T.D.; Ambuhl, D.; Schmaranzer, F.; Todorski, I.A.S.; Steppacher, S.D.; Hanke, M.S.; Haefeli, P.C.; Liechti, E.F.; Siebenrock, K.A.; Tannast, M. Biochemical MRI with dGEMRIC Corresponds to 3D-CT Based Impingement Location for Detection of Acetabular Cartilage Damage in FAI Patients. Orthop. J. Sports Med. 2021, 9, 2325967120988175. [Google Scholar] [CrossRef]
- Yamamoto, T.; Zurmuhle, C.A.; Stetzelberger, V.M.; Schwab, J.M.; Steppacher, S.D.; Tannast, M. The New Bern Chondrolabral Classification Is Reliable and Reproducible. Clin. Orthop. Relat. Res. 2021, 479, 1002–1013. [Google Scholar] [CrossRef]
- Narvaez, M.V.; Cady, A.; Serrano, B.; Youssefzadeh, K.; Banffy, M. Outside-In Capsulotomy of the Hip for Arthroscopic Pincer Resection. Arthrosc. Tech. 2021, 10, e615–e620. [Google Scholar] [CrossRef]
- Nehme, A.; El-Hajj, G.; Maalouly, J.; Ayoubi, R.; Abdel-Nour, H.; Moucharafieh, R.; Ashou, R. Hip joint space width in an asymptomatic population: Computed tomography analysis according to femoroacetabular impingement morphologies. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2021, 24, 14–22. [Google Scholar] [CrossRef]
- Bento, A.O.; Falotico, G.; Enseki, K.; Cunha, R.A.; Ejnisman, B.; Arliani, G.; Cohen, M. Morphological Changes of the Hip Commonly Associated with Femoroacetabular Impingement Are Not Correlated with Rotational Range of Hip Motion in Elite Soccer Athletes. Sports Health 2021, 13, 341–346. [Google Scholar] [CrossRef]
- Larson, C.M.; LaPrade, R.F.; Floyd, E.R.; McGaver, R.S.; Bedi, A. Acetabular Rim Disorders/Pincer-type Femoroacetabular Impingement and Hip Arthroscopy. Sports Med. Arthrosc. Rev. 2021, 29, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.R.; Dickenson, E.J.; O’Donnell, J.; Agricola, R.; Awan, T.; Beck, M.; Clohisy, J.C.; Dijkstra, H.P.; Falvey, E.; Gimpel, M.; et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): An international consensus statement. Br. J. Sports Med. 2016, 50, 1169–1176. [Google Scholar] [CrossRef]
- Ito, K.; Minka, M.A., 2nd; Leunig, M.; Werlen, S.; Ganz, R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J. Bone Jt. Surg. Br. 2001, 83, 171–176. [Google Scholar] [CrossRef]
- Beck, M.; Leunig, M.; Parvizi, J.; Boutier, V.; Wyss, D.; Ganz, R. Anterior femoroacetabular impingement: Part II. Midterm results of surgical treatment. Clin. Orthop. Relat. Res. 2004, 418, 67–73. [Google Scholar] [CrossRef]
- Ganz, R.; Leunig, M.; Leunig-Ganz, K.; Harris, W.H. The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin. Orthop. Relat. Res. 2008, 466, 264–272. [Google Scholar] [CrossRef]
- Pierannunzii, L. Femoroacetabular impingement: Question-driven review of hip joint pathophysiology from asymptomatic skeletal deformity to end-stage osteoarthritis. J. Orthop. Traumatol. 2019, 20, 32. [Google Scholar] [CrossRef] [PubMed]
- Hankins, D.A.; Korcek, L.; Richter, D.L. Femoroacetabular Impingement and Management of Labral Tears in the Athlete. Clin. Sports Med. 2021, 40, 259–270. [Google Scholar] [CrossRef]
- Migliorini, F.; Baroncini, A.; Eschweiler, J.; Knobe, M.; Tingart, M.; Maffulli, N. Return to sport after arthroscopic surgery for femoroacetabular impingement. Surgeon 2023, 21, 21–30. [Google Scholar] [CrossRef]
- Di Benedetto, P.; Barbattini, P.; Povegliano, L.; Beltrame, A.; Gisonni, R.; Cainero, V.; Causero, A. Extracapsular vs standard approach in hip arthroscopy. Acta Biomed. 2016, 87 (Suppl. S1), 41–45. [Google Scholar]
- Goldsmith, C.; Cheng, J.; Mintz, D.; Moley, P. Correlation of femoral version measurements between computed tomography and magnetic resonance imaging studies in patients presenting with a femoroacetabular impingement-related complaint. J. Hip Preserv. Surg. 2022, 9, 219–224. [Google Scholar] [CrossRef]
- Tuncay, I.; Ucan, V.; Agir, M.; Anwar, W.; Elmali, N. Is Only Peripheral Hip Arthroscopy Enough for Selected Patients with Femoroacetabular Impingement Syndrome? Arch. Bone Jt. Surg. 2022, 10, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Mohd-Hanaffi, A.F.; Puji, A. An Overlooked Entity in Diagnosing Hip Pain with Neuropathy in an Athletic Young Adult: A Case Report. Malays. Orthop. J. 2022, 16, 136–138. [Google Scholar] [CrossRef] [PubMed]
- Aprato, A.; Masse, A.; Faletti, C.; Valente, A.; Atzori, F.; Stratta, M.; Jayasekera, N. Magnetic resonance arthrography for femoroacetabular impingement surgery: Is it reliable? J. Orthop. Traumatol. 2013, 14, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Schmaranzer, F.; Kheterpal, A.B.; Bredella, M.A. Best Practices: Hip Femoroacetabular Impingement. AJR Am. J. Roentgenol. 2021, 216, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Sutter, R.; Pfirrmann, C.W.A. Update on Femoroacetabular Impingement: What Is New, and How Should We Assess It? Semin. Musculoskelet. Radiol. 2017, 21, 518–528. [Google Scholar] [CrossRef]
- DeFroda, S.F.; Alter, T.D.; Lambers, F.; Malloy, P.; Clapp, I.M.; Chahla, J.; Nho, S.J. Quantification of Acetabular Coverage on 3-Dimensional Reconstructed Computed Tomography Scan Bone Models in Patients with Femoroacetabular Impingement Syndrome: A Descriptive Study. Orthop. J. Sports Med. 2021, 9, 23259671211049457. [Google Scholar] [CrossRef]
- Samim, M. 3D MRI Models of the Musculoskeletal System. Semin. Musculoskelet. Radiol. 2021, 25, 388–396. [Google Scholar] [CrossRef]
- Kuhaimi, T.A.; Alenezi, G.; Alawaji, A.; Alshaikh, M.; Bauones, S. Intra-articular hip joint osteoid osteoma: Challenging diagnosis and percutaneous radiofrequency ablation treatment. Radiol. Case Rep. 2021, 16, 3315–3320. [Google Scholar] [CrossRef]
- Dijkstra, H.P.; Ardern, C.L.; Serner, A.; Mosler, A.B.; Weir, A.; Roberts, N.W.; Mc Auliffe, S.; Oke, J.L.; Khan, K.M.; Clarke, M.; et al. Primary cam morphology; bump, burden or bog-standard? A concept analysis. Br. J. Sports Med. 2021, 55, 1212–1221. [Google Scholar] [CrossRef]
- Hanke, M.S.; Lerch, T.D.; Schmaranzer, F.; Meier, M.K.; Steppacher, S.D.; Siebenrock, K.A. Complications of hip preserving surgery. EFORT Open Rev. 2021, 6, 472–486. [Google Scholar] [CrossRef]
- Kaymakoglu, M.; Dut, R.; Imre, D.; Bilge Ergen, F.; Ali Talmac, M.; Aksoy, C. Characteristics of femoroacetabular impingement morphology and relation with skeletal maturity among asymptomatic adolescents. Acta Orthop. Belg. 2021, 87, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T.; Watanabe, H.; Taki, N.; Onuma, S.; Kikkawa, I. Unilateral premature osteoarthritis of the hip with excessive anteversion of the femoral neck developing in the early second decade: Two surgical cases. BMC Musculoskelet. Disord. 2021, 22, 517. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.; Wu, R.; Liu, R.; Ao, Y.; Wang, J.; Xu, Y. Hip arthroscopy has good clinical outcomes in the treatment of osteoid osteoma of the acetabulum. BMC Musculoskelet. Disord. 2021, 22, 491. [Google Scholar] [CrossRef]
- Haviv, B.; Singh, P.J.; Takla, A.; O’Donnell, J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J. Bone Jt. Surg. Br. 2010, 92, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.R.; Dickenson, E.J.; Achana, F.; Griffin, J.; Smith, J.; Wall, P.D.; Realpe, A.; Parsons, N.; Hobson, R.; Fry, J.; et al. Arthroscopic hip surgery compared with personalised hip therapy in people over 16 years old with femoroacetabular impingement syndrome: UK FASHIoN RCT. Health Technol. Assess. 2022, 26, 1–236. [Google Scholar] [CrossRef]
- Anzillotti, G.; Iacomella, A.; Grancagnolo, M.; Bertolino, E.M.; Marcacci, M.; Sconza, C.; Kon, E.; Di Matteo, B. Conservative vs. Surgical Management for Femoro-Acetabular Impingement: A Systematic Review of Clinical Evidence. J. Clin. Med. 2022, 11, 5852. [Google Scholar] [CrossRef]
- Mansell, N.S.; Rhon, D.I.; Meyer, J.; Slevin, J.M.; Marchant, B.G. Arthroscopic Surgery or Physical Therapy for Patients with Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial with 2-Year Follow-up. Am. J. Sports Med. 2018, 46, 1306–1314. [Google Scholar] [CrossRef]
- Mansell, N.S.; Rhon, D.I.; Marchant, B.G.; Slevin, J.M.; Meyer, J.L. Two-year outcomes after arthroscopic surgery compared to physical therapy for femoracetabular impingement: A protocol for a randomized clinical trial. BMC Musculoskelet. Disord. 2016, 17, 60. [Google Scholar] [CrossRef]
- Kaldau, N.C.; Brorson, S.; Hölmich, P.; Lund, B. Good midterm results of hip arthroscopy for femoroacetabular impingement. Dan. Med. J. 2018, 65, A5483. [Google Scholar]
- Migliorini, F.; Maffulli, N.; Knobe, M.; Eschweiler, J.; Tingart, M.; Baroncini, A. Arthroscopic labral repair for femoroacetabular impingement: A systematic review. Surgeon 2022, 20, e225–e230. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N. Arthroscopic Management of Femoroacetabular Impingement in Adolescents: A Systematic Review. Am. J. Sports Med. 2021, 49, 3708–3715. [Google Scholar] [CrossRef] [PubMed]
- Gatz, M.; Driessen, A.; Eschweiler, J.; Tingart, M.; Migliorini, F. Arthroscopic surgery versus physiotherapy for femoroacetabular impingement: A meta-analysis study. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 1151–1162. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Liu, Y.; Catalano, G.; Trivellas, A.; Eschweiler, J.; Tingart, M.; Maffulli, N. Medium-term results of arthroscopic treatment for femoroacetabular impingement. Br. Med. Bull. 2021, 138, 68–84. [Google Scholar] [CrossRef]
- Zhu, Y.; Su, P.; Xu, T.; Zhang, L.; Fu, W. Conservative therapy versus arthroscopic surgery of femoroacetabular impingement syndrome (FAI): A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 296. [Google Scholar] [CrossRef]
- Basques, B.A.; Waterman, B.R.; Ukwuani, G.; Beck, E.C.; Neal, W.H.; Friel, N.A.; Stone, A.V.; Nho, S.J. Preoperative Symptom Duration Is Associated with Outcomes After Hip Arthroscopy. Am. J. Sports Med. 2019, 47, 131–137. [Google Scholar] [CrossRef]
- Chahla, J.; Beck, E.C.; Okoroha, K.; Cancienne, J.M.; Kunze, K.N.; Nho, S.J. Prevalence and Clinical Implications of Chondral Injuries After Hip Arthroscopic Surgery for Femoroacetabular Impingement Syndrome. Am. J. Sports Med. 2019, 47, 2626–2635. [Google Scholar] [CrossRef]
- Cvetanovich, G.L.; Weber, A.E.; Kuhns, B.D.; Alter, J.; Harris, J.D.; Mather, R.C., 3rd; Nho, S.J. Hip Arthroscopic Surgery for Femoroacetabular Impingement with Capsular Management: Factors Associated with Achieving Clinically Significant Outcomes. Am. J. Sports Med. 2018, 46, 288–296. [Google Scholar] [CrossRef]
- Kunze, K.N.; Beck, E.C.; Nwachukwu, B.U.; Ahn, J.; Nho, S.J. Early Hip Arthroscopy for Femoroacetabular Impingement Syndrome Provides Superior Outcomes When Compared with Delaying Surgical Treatment Beyond 6 Months. Am. J. Sports Med. 2019, 47, 2038–2044. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Szymski, D.; Kurtz, S.; Alt, V.; Lowenberg, D.W.; Lau, E.; Rupp, M. Factors associated with mortality after proximal femoral fracture. J. Orthop. Traumatol. 2023, 24, 31. [Google Scholar] [CrossRef]
- Guevara-Ramirez, W.; Miranda-Salinas, S.; Diaz-Salamanca, P.; Gribbell-Pizarro, J.; Saldias-Carrasset, V. Determining factors of the accident rate and occupational diseases of the shellfish divers of the Coquimbo Region, Chile. Rev. Salud Publica 2020, 22, 77–81. [Google Scholar] [CrossRef]
- Reddy, C.N.; Belaldavar, B.P.; Havaldar, R.R. Study of Efficacy of Intraoral Submucosal Injections of Corticosteroids and Placentrex in the Management of Oral Submucous Fibrosis. Indian. J. Otolaryngol. Head. Neck Surg. 2022, 74, 1996–2001. [Google Scholar] [CrossRef] [PubMed]
- Chethana, R.; Mishra, P.; Kaushik, M.; Jadhav, R.; Dehadaray, A. Effect of Smoking on Nasal Mucociliary Clearance. Indian. J. Otolaryngol. Head. Neck Surg. 2022, 74, 956–959. [Google Scholar] [CrossRef] [PubMed]
- Cong, S.; Pan, J.; Huang, G.; Xie, D.; Zeng, C. The Modified Longitudinal Capsulotomy by Outside-In Approach in Hip Arthroscopy for Femoroplasty and Acetabular Labrum Repair-A Cohort Study. J. Clin. Med. 2022, 11, 4548. [Google Scholar] [CrossRef] [PubMed]
- Roksmall o, C.a.C.E.A.; Panova, I.A.; Malyshkina, A.I.; Fetisova, I.N.; Fetisov, N.S.; Kharlamova, N.V.; Kuligina, M.V. Technologies for Prediction of Preeclampsia. Sovrem. Tekhnologii Med. 2021, 12, 78–84. [Google Scholar] [CrossRef]
- Nigam, K.; Samadi, F.M.; Srivastava, S.; Mohammad, S.; Sanyal, S. Smoking and XPC Gene Polymorphism Interact to Modulate the Risk of Oral Cancer. J. Maxillofac. Oral. Surg. 2021, 20, 607–611. [Google Scholar] [CrossRef]
- Goyal, R.; Goyal, M.K. Influence of Life Style Factors on Oral Potentially Malignant and Malignant Disorders: A Cross Sectional Study. Indian. J. Otolaryngol. Head. Neck Surg. 2021, 73, 443–446. [Google Scholar] [CrossRef]
- Tourangeau, R.; Sun, H.; Yan, T. Comparing Methods for Assessing Reliability. J. Surv. Stat. Methodol. 2021, 9, 651–673. [Google Scholar] [CrossRef]
- Jimenez-Ruiz, C.A.; Lopez-Padilla, D.; Alonso-Arroyo, A.; Aleixandre-Benavent, R.; Solano-Reina, S.; de Granda-Orive, J.I. COVID-19 and Smoking: A Systematic Review and Meta-Analysis of the Evidence. Arch. Bronconeumol. 2021, 57, 21–34. [Google Scholar] [CrossRef]
- Urrutia-Pereira, M.; Oliano, V.J.; Aranda, C.S.; Mallol, J.; Solé, D. Prevalence and factors associated with smoking among adolescents. J. Pediatr 2017, 93, 230–237. [Google Scholar] [CrossRef]
- Urrutia-Pereira, M.; Solé, D.; Chong Neto, H.J.; Badellino, H.; Acosta, V.; Castro-Almarales, R.L.; León, M.G.; Avalos, M.M.; Fernández, C.C.; Sisul-Alvariza, J.C.; et al. Youth tobacco use in Latin America: What is the real extent of the problem? Allergol. Immunopathol. 2019, 47, 328–335. [Google Scholar] [CrossRef]
- Fernandez, A.C.; Bohnert, K.M.; Bicket, M.C.; Weng, W.; Singh, K.; Englesbe, M. Adverse Surgical Outcomes Linked to Co-occurring Smoking and Risky Alcohol Use Among General Surgery Patients. Ann. Surg. 2023, 278, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Howard, R.; Albright, J.; Osborne, N.; Englesbe, M.; Goodney, P.; Henke, P. Impact of a regional smoking cessation intervention for vascular surgery patients. J. Vasc. Surg. 2022, 75, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Cancienne, J.; Kunze, K.N.; Beck, E.C.; Chahla, J.; Suppauksorn, S.; Nho, S.J. Influence of Cigarette Smoking at the Time of Surgery on Postoperative Outcomes in Patients with Femoroacetabular Impingement: A Matched-Pair Cohort Analysis. Am. J. Sports Med. 2019, 47, 1138–1144. [Google Scholar] [CrossRef]
- Jimenez, A.E.; Lee, M.S.; Owens, J.S.; Maldonado, D.R.; Saks, B.R.; Lall, A.C.; Domb, B.G. Effect of Cigarette Smoking on Midterm Outcomes After Arthroscopic Surgery for Femoroacetabular Impingement Syndrome: A Propensity-Matched Controlled Study with Minimum 5-Year Follow-up. Orthop. J. Sports Med. 2022, 10, 23259671221090905. [Google Scholar] [CrossRef]
- Lee, M.S.; Jimenez, A.E.; Owens, J.S.; Curley, A.J.; Paraschos, O.A.; Maldonado, D.R.; Lall, A.C.; Domb, B.G. Comparison of Outcomes Between Nonsmokers and Patients Who Discontinued Smoking 1 Month Before Primary Hip Arthroscopy: A Propensity-Matched Study with Minimum 2-Year Follow-up. Orthop. J. Sports Med. 2022, 10, 23259671221097372. [Google Scholar] [CrossRef]
- Deng, W.; Shao, H.; Tang, H.; Tang, Q.; Wang, Z.; Yang, D.; Zhou, Y. Better PROMs and higher return-to-sport rate after modular bicompartmental knee arthroplasty than after total knee arthroplasty for medial and patellofemoral compartment osteoarthritis. Front. Surg. 2022, 9, 1078866. [Google Scholar] [CrossRef]
- Mou, D.; Sisodia, R.C.; Castillo-Angeles, M.; Ladin, K.; Bergmark, R.W.; Pusic, A.L.; Del Carmen, M.G.; Heng, M. The Surgeon’s Perceived Value of Patient-reported Outcome Measures (PROMs): An Exploratory Qualitative Study of 5 Different Surgical Subspecialties. Ann. Surg. 2022, 275, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Wittich, L.; Tsatsaronis, C.; Kuklinski, D.; Schoner, L.; Steinbeck, V.; Busse, R.; Rombey, T. Patient-Reported Outcome Measures (PROMs) as an intervention: A comprehensive overview of systematic reviews on the effects of PROM feedback. Value Health 2024, 27, 1436–1453. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N.; Memminger, M.K.; Simeone, F.; Rath, B.; Huber, T. Clinical relevance of patient-reported outcome measures in patients who have undergone total hip arthroplasty: A systematic review. Arch. Orthop. Trauma. Surg. 2024, 144, 4907–4916. [Google Scholar] [CrossRef]
- Migliorini, F.; Coppola, F.; D’Addona, A.; Rosolani, M.; Della Rocca, F. Revision of Failed Short Stems in Total Hip Arthroplasty. J. Clin. Med. 2024, 13, 2459. [Google Scholar] [CrossRef]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H.; Goddard, O.M.; et al. The 2011 Oxford CEBM Levels of Evidence; Oxford Centre for Evidence-Based Medicine: Oxford, UK, 2011; Available online: https://www.cebm.net/index.aspx?o=5653 (accessed on 1 September 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Cochrane. 2022. Available online: www.training.cochrane.org/handbook (accessed on 1 September 2024).
- Migliorini, F.; Maffulli, N.; Eschweiler, J.; Schenker, H.; Tingart, M.; Betsch, M. Arthroscopic versus mini-open rotator cuff repair: A meta-analysis. Surgeon 2023, 21, e1–e12. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.; Hon, S.D.; Cheng, C.; Franklin, J.D.; Aoki, S.K.; Anderson, M.B.; Kapron, A.L.; Peters, C.L.; Pelt, C.E. Psychometric Evaluation of the Lower Extremity Computerized Adaptive Test, the Modified Harris Hip Score, and the Hip Outcome Score. Orthop. J. Sports Med. 2014, 2, 2325967114562191. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.L.; Kelly, B.T.; Philippon, M.J. Evidence of validity for the hip outcome score. Arthroscopy 2006, 22, 1304–1311. [Google Scholar] [CrossRef]
- Christensen, C.P.; Althausen, P.L.; Mittleman, M.A.; Lee, J.A.; McCarthy, J.C. The nonarthritic hip score: Reliable and validated. Clin. Orthop. Relat. Res. 2003, 406, 75–83. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020, 12, 55–61. [Google Scholar] [CrossRef]
- Lucenti, L.; Maffulli, N.; Bardazzi, T.; Saggini, R.; Memminger, M.; Simeone, F.; Migliorini, F. Return to Sport Following Arthroscopic Management of Femoroacetabular Impingement: A Systematic Review. J. Clin. Med. 2024, 13, 5219. [Google Scholar] [CrossRef] [PubMed]
- Parvaresh, K.; Rasio, J.P.; Wichman, D.; Chahla, J.; Nho, S.J. The Influence of Body Mass Index on Outcomes After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: Five-Year Results in 140 Patients. Am. J. Sports Med. 2021, 49, 90–96. [Google Scholar] [CrossRef]
- Yang, F.; Shao, J.; Zheng, X.; Bi, G.; Zhang, X.; Huang, H.; Wang, J. Does Preoperative Activity Level Affect Postoperative Clinical Outcomes Following Hip Arthroscopy in Femoroacetabular Impingement Syndrome (FAIS) Patients? Orthop. Surg. 2023, 15, 1756–1762. [Google Scholar] [CrossRef]
- Bizzini, M.; Schaub, G.; Ferrari, E.; Monn, S.; Leunig, M.; Casartelli, N.C.; Maffiuletti, N.A. Hip muscle strength in male and female patients with femoroacetabular impingement syndrome: Comparison to healthy controls and athletes. Phys. Ther. Sport. 2023, 61, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Alrashdi, N.Z.; Brown-Taylor, L.; Bell, M.M.; Ithurburn, M.P. Movement Patterns and Their Associations with Pain, Function, and Hip Morphology in Individuals with Femoroacetabular Impingement Syndrome: A Scoping Review. Phys. Ther. 2021, 101, pzab185. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Ahedo, C.; Camacho-Galindo, J.; López-Reyes, A.; Martinez-Gómez, L.E.; Pineda, C.; Domb, B.G. A comprehensive review of hip arthroscopy techniques and outcomes. SAGE Open Med. 2024, 12, 20503121231222212. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, G.E.; O’Keeffe, M.; Maher, C.G.; Harris, I.A.; Kwok, W.S.; Peek, A.L.; Zadro, J.R. The effectiveness of hip arthroscopic surgery for the treatment of femoroacetabular impingement syndrome: A systematic review and meta-analysis. J. Sci. Med. Sport. 2021, 24, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Annin, S.; Lall, A.C.; Yelton, M.J.; Shapira, J.; Rosinsky, P.J.; Meghpara, M.B.; Maldonado, D.R.; Ankem, H.; Domb, B.G. Patient-Reported Outcomes in Athletes Following Hip Arthroscopy for Femoroacetabular Impingement with Subanalysis on Return to Sport and Performance Level: A Systematic Review. Arthroscopy 2021, 37, 2657–2676. [Google Scholar] [CrossRef]
- Hack, K.; Di Primio, G.; Rakhra, K.; Beaulé, P.E. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J. Bone Jt. Surg. Am. 2010, 92, 2436–2444. [Google Scholar] [CrossRef]
- Gerhardt, M.B.; Romero, A.A.; Silvers, H.J.; Harris, D.J.; Watanabe, D.; Mandelbaum, B.R. The prevalence of radiographic hip abnormalities in elite soccer players. Am. J. Sports Med. 2012, 40, 584–588. [Google Scholar] [CrossRef]
- Tanzer, M.; Noiseux, N. Osseous abnormalities and early osteoarthritis: The role of hip impingement. Clin. Orthop. Relat. Res. 2004, 429, 170–177. [Google Scholar] [CrossRef]
- Debbi, E.M.; Rajaee, S.S.; Spitzer, A.I.; Paiement, G.D. Smoking and Total Hip Arthroplasty: Increased Inpatient Complications, Costs, and Length of Stay. J. Arthroplasty 2019, 34, 1736–1739. [Google Scholar] [CrossRef]
- Duchman, K.R.; Gao, Y.; Pugely, A.J.; Martin, C.T.; Noiseux, N.O.; Callaghan, J.J. The Effect of Smoking on Short-Term Complications Following Total Hip and Knee Arthroplasty. J. Bone Jt. Surg. Am. 2015, 97, 1049–1058. [Google Scholar] [CrossRef]
- Sloan, A.; Hussain, I.; Maqsood, M.; Eremin, O.; El-Sheemy, M. The effects of smoking on fracture healing. Surgeon 2010, 8, 111–116. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.C.; Browning, K.K. Smoking, chronic wound healing, and implications for evidence-based practice. J. Wound Ostomy Cont. Nurs. 2014, 41, 415–423; quiz E411–412. [Google Scholar] [CrossRef]
- Kainiemi, K.; Malmivaara, A.; Sillman-Tetri, S.; Lasander, M.; Heinonen, M.; Korhonen, T.; Sand, J.; Laatikainen, T.; Kyrö, A. Smoking cessation intervention prior to orthopedic surgery: A study protocol to determine patient outcomes and feasibility. Tob. Prev. Cessat. 2022, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, H.; Park, H.J.; Chakir, J.; Semlali, A.; Rouabhia, M. Comparative study of the effects of cigarette smoke and electronic cigarettes on human gingival fibroblast proliferation, migration and apoptosis. Food Chem. Toxicol. 2018, 118, 390–398. [Google Scholar] [CrossRef]
- Lincoln, A.E.; Smith, G.S.; Amoroso, P.J.; Bell, N.S. The effect of cigarette smoking on musculoskeletal-related disability. Am. J. Ind. Med. 2003, 43, 337–349. [Google Scholar] [CrossRef]
- Du, J.Y.; Weinberg, D.S.; Moore, T.A.; Vallier, H.A. Smoking Is Associated with Longer Intensive Care Unit Stays in Spine Trauma Patients. J. Orthop. Trauma. 2020, 34, e250–e255. [Google Scholar] [CrossRef]
- Gao, H.; Huang, Z.; Jia, Z.; Ye, H.; Fu, F.; Song, M.; Zhao, Y.; Chen, W. Influence of passive smoking on the onset of Legg-Calve-Perthes disease: A systematic review and meta-analysis. J. Pediatr. Orthop. 2020, 29, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Herrero, C.; Tang, A.; Wasterlain, A.; Sherman, S.; Bosco, J.; Lajam, C.; Schwarzkopf, R.; Slover, J. Smoking cessation correlates with a decrease in infection rates following total joint arthroplasty. J. Orthop. 2020, 21, 390–394. [Google Scholar] [CrossRef]
- Heyer, J.H.; Perim, D.A.; Amdur, R.L.; Pandarinath, R. Impact of smoking on outcomes following knee and shoulder arthroscopy. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 329–336. [Google Scholar] [CrossRef]
- Kwon, J.W.; Ha, J.W.; Lee, T.S.; Moon, S.H.; Lee, H.M.; Park, Y. Comparison of the Prevalence of Low Back Pain and Related Spinal Diseases among Smokers and Nonsmokers: Using Korean National Health Insurance Database. Clin. Orthop. Surg. 2020, 12, 200–208. [Google Scholar] [CrossRef]
- Hart, A.; Rainer, W.G.; Taunton, M.J.; Mabry, T.M.; Berry, D.J.; Abdel, M.P. Smoking Cessation Before and After Total Joint Arthroplasty-An Uphill Battle. J. Arthroplast. 2019, 34, S140–S143. [Google Scholar] [CrossRef] [PubMed]
- Sahota, S.; Lovecchio, F.; Harold, R.E.; Beal, M.D.; Manning, D.W. The Effect of Smoking on Thirty-Day Postoperative Complications After Total Joint Arthroplasty: A Propensity Score-Matched Analysis. J. Arthroplast. 2018, 33, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Berman, D.; Oren, J.H.; Bendo, J.; Spivak, J. The Effect of Smoking on Spinal Fusion. Int. J. Spine Surg. 2017, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Gurel, R.; Vidra, M.; Elbaz, E.; Factor, S.; Kazum, E.; Bivas, A.; Maman, E.; Chechik, O.; Rotman, D. Arthroscopic rotator cuff repair in fibromyalgia patients had comparable outcomes to a matched control group. J. Orthop. Traumatol. 2023, 24, 21. [Google Scholar] [CrossRef]
- Migliorini, F.; Asparago, G.; Cuozzo, F.; Oliva, F.; Hildebrand, F.; Maffulli, N. Patient outcomes and return to play after arthroscopic rotator cuff repair in overhead athletes: A systematic review. J. Orthop. Traumatol. 2023, 24, 3. [Google Scholar] [CrossRef]
- Deng, Z.; Zheng, Y.; Deng, Z.; Lu, C.; Wu, Y.; Chen, K.; Fu, Z.; Zhang, H.; Lu, W.; Zhu, W. Arthroscopic reconstruction of anterior cruciate ligaments with allograft: Single-tunnel single-bundle versus single-tunnel double-bundle techniques. J. Orthop. Traumatol. 2022, 23, 26. [Google Scholar] [CrossRef]
- Emara, A.K.; Grits, D.; Samuel, L.T.; Acuña, A.J.; Rosneck, J.T.; Kamath, A.F. Hip Arthroscopy in Smokers: A Systematic Review of Patient-Reported Outcomes and Complications in 18,585 Cases. Am. J. Sports Med. 2021, 49, 1101–1108. [Google Scholar] [CrossRef]
- De Vita, M.J.; Maisto, S.A.; Ansell, E.B.; Zale, E.L.; Ditre, J.W. Pack-years of tobacco cigarette smoking as a predictor of spontaneous pain reporting and experimental pain reactivity. Exp. Clin. Psychopharmacol. 2019, 27, 552–560. [Google Scholar] [CrossRef]
- Karlsdottir, B.R.; Zhou, P.P.; Wahba, J.; Mott, S.L.; Goffredo, P.; Hrabe, J.; Hassan, I.; Kapadia, M.R.; Gribovskaja-Rupp, I. Male gender, smoking, younger age, and preoperative pain found to increase postoperative opioid requirements in 592 elective colorectal resections. Int. J. Color. Dis. 2022, 37, 1799–1806. [Google Scholar] [CrossRef]
- Shiri, R.; Karppinen, J.; Leino-Arjas, P.; Solovieva, S.; Viikari-Juntura, E. The association between smoking and low back pain: A meta-analysis. Am. J. Med. 2010, 123, 87.E7–87.E35. [Google Scholar] [CrossRef]
- Audet, M.A.; Benedick, A.; Vallier, H.A. Tobacco smoking is associated with more pain and worse functional outcomes after torsional ankle fracture. OTA Int. 2022, 5, e175. [Google Scholar] [CrossRef] [PubMed]
- Schneider, B.J.; Ehsanian, R. Effects of smoking on pain intensity in patients with chronic pain: Are there clinical implications? Ann. Palliat. Med. 2020, 9, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.O.; Eom, J.S.; Jung, H.G. The effect of smoking on the outcomes of lateral ankle ligament reconstruction. J. Orthop. Sci. 2018, 23, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Green, K.T.; Wilson, S.M.; Dennis, P.A.; Runnals, J.J.; Williams, R.A.; Bastian, L.A.; Beckham, J.C.; Dedert, E.A.; Kudler, H.S.; Straits-Troster, K.; et al. Cigarette Smoking and Musculoskeletal Pain Severity Among Male and Female Afghanistan/Iraq Era Veterans. Pain. Med. 2017, 18, 1795–1804. [Google Scholar] [CrossRef]
- Ditre, J.W.; Heckman, B.W.; LaRowe, L.R.; Powers, J.M. Pain Status as a Predictor of Smoking Cessation Initiation, Lapse, and Relapse. Nicotine Tob. Res. 2021, 23, 186–194. [Google Scholar] [CrossRef]
- Zabrzyński, J.; Paczesny, Ł.; Zabrzyńska, A.; Huri, G.; Graboń, K.; Pielak, T.; Kruczyński, J.; Łapaj, Ł. Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones-A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 16127. [Google Scholar] [CrossRef]
- Schmid, M.; Sood, A.; Campbell, L.; Kapoor, V.; Dalela, D.; Klett, D.E.; Chun, F.K.; Kibel, A.S.; Sammon, J.D.; Menon, M.; et al. Impact of smoking on perioperative outcomes after major surgery. Am. J. Surg. 2015, 210, 221–229.e226. [Google Scholar] [CrossRef]
- Yue, C.; Cui, G.; Ma, M.; Tang, Y.; Li, H.; Liu, Y.; Zhang, X. Associations between smoking and clinical outcomes after total hip and knee arthroplasty: A systematic review and meta-analysis. Front. Surg. 2022, 9, 970537. [Google Scholar] [CrossRef]
- Ehnert, S.; Aspera-Werz, R.H.; Ihle, C.; Trost, M.; Zirn, B.; Flesch, I.; Schröter, S.; Relja, B.; Nussler, A.K. Smoking Dependent Alterations in Bone Formation and Inflammation Represent Major Risk Factors for Complications Following Total Joint Arthroplasty. J. Clin. Med. 2019, 8, 406. [Google Scholar] [CrossRef]
- Kamma, S.A.; Pathapati, R.K.; Somerson, J.S. Smoking cessation prior to total shoulder arthroplasty: A systematic review of outcomes and complications. Shoulder Elb. 2023, 15, 484–496. [Google Scholar] [CrossRef]
- Lieberman, J.R. Hip Arthroscopy for Femoroacetabular Impingement Patients Older Than 50 Years-Proceed with Caution. Arthroscopy 2019, 35, 2759–2760. [Google Scholar] [CrossRef]
- Khan, M.; Habib, A.; de Sa, D.; Larson, C.M.; Kelly, B.T.; Bhandari, M.; Ayeni, O.R.; Bedi, A. Arthroscopy Up to Date: Hip Femoroacetabular Impingement. Arthroscopy 2016, 32, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Matar, H.E.; Rajpura, A.; Board, T.N. Femoroacetabular impingement in young adults: Assessment and management. Br. J. Hosp. Med. 2019, 80, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Gollwitzer, H.; Möckel, G.; Sobau, C. Surgical treatment of femoroacetabular impingement syndrome: Arthroscopy-mini-open-surgical hip dislocation. Orthopade 2022, 51, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Chen, L.; Wang, G. Hip arthroscopy versus open surgical dislocation for femoroacetabular impingement: A systematic review and meta-analysis. Medicine 2016, 95, e5122. [Google Scholar] [CrossRef]
- Lovett-Carter, D.; Jawanda, A.S.; Hannigan, A. Meta-Analysis of the Surgical and Rehabilitative Outcomes of Hip Arthroscopy in Athletes with Femoroacetabular Impingement. Clin. J. Sport. Med. 2020, 30, 404–411. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Journal | Design | Follow-Up (Months) | Smokers | Patients (n) | Women (n) | Mean Age (y) | Mean BMI |
|---|---|---|---|---|---|---|---|---|
| Cancienne et al., 2019 [83] | Am J Sports Med | Retrospective | 24.0 | Yes | 40 | 24 | 35.5 | 27.0 |
| No | 80 | 49 | 36.1 | 24.6 | ||||
| Jimenez et al., 2022 [84] | Orthop J Sports Med | Retrospective | 39.9 | Yes | 20 | 41.4 | 30.2 | |
| No | 60 | 42.5 | 28.7 | |||||
| Lee et al., 2022 [85] | Orthop J Sports Med | Retrospective | 38.6 | Yes | 84 | 62 | 45.0 | 26.6 |
| No | 84 | 58 | 28.0 |
| Endpoint | Smokers (N = 144) | Nonsmokers (N = 224) | p |
|---|---|---|---|
| Women | 69.4% (86 of 124) | 65.2% (107 of 164) | 0.8 |
| Mean follow-up (months) | 34.7 ± 6.7 | 33.7 ± 7.3 | 0.5 |
| Age (mean) | 41.9 ± 4.1 | 38.8 ± 3.2 | 0.4 |
| BMI (mean) | 27.2 ± 1.2 | 27.0 ± 1.8 | 0.7 |
| VAS (mean) | 6.2 ± 2.2 | 6.0 ± 2.2 | 0.7 |
| mHHS (mean) | 58.2 ± 13.4 | 61.3 ± 15.3 | 0.2 |
| NAHS (mean) | 57.7 ± 16.6 | 60.2 ± 15.6 | 0.5 |
| HOS-SSS (mean) | 42.2 ± 21.9 | 47.8 ± 22.7 | 0.9 |
| Endpoint | Smokers (N = 144) | Nonsmokers (N = 224) | Effect Size | p |
|---|---|---|---|---|
| VAS (mean) | 2.3 ± 2.7 | 1.9 ± 2.4 | 0.4 | 0.4 |
| mHHS (mean) | 82.6 ± 20.6 | 84.1 ± 15.5 | −1.5 | 0.6 |
| NAHS (mean) | 85.7 ± 13.5 | 85.4 ± 17.8 | 0.3 | 0.8 |
| HOS-SSS (mean) | 65.7 ± 17.1 | 69.8 ± 14.1 | −4.1 | 0.6 |
| Endpoint | Smokers (N = 144) | Nonsmokers (N = 224) | p |
|---|---|---|---|
| Reoperation | 5.8% (6 of 104) | 4.9% (7 of 144) | 0.6 |
| Progression to THA | 7.7% (8 of 104) | 2.8% (4 of 144) | 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucenti, L.; Maffulli, N.; Bardazzi, T.; Pipino, G.; Pappalardo, G.; Migliorini, F. No Effect of Cigarette Smoking in the Outcome of Arthroscopic Management for Femoroacetabular Impingement: A Systematic Review. J. Clin. Med. 2024, 13, 7214. https://doi.org/10.3390/jcm13237214
Lucenti L, Maffulli N, Bardazzi T, Pipino G, Pappalardo G, Migliorini F. No Effect of Cigarette Smoking in the Outcome of Arthroscopic Management for Femoroacetabular Impingement: A Systematic Review. Journal of Clinical Medicine. 2024; 13(23):7214. https://doi.org/10.3390/jcm13237214
Chicago/Turabian StyleLucenti, Ludovico, Nicola Maffulli, Tommaso Bardazzi, Gennaro Pipino, Gaetano Pappalardo, and Filippo Migliorini. 2024. "No Effect of Cigarette Smoking in the Outcome of Arthroscopic Management for Femoroacetabular Impingement: A Systematic Review" Journal of Clinical Medicine 13, no. 23: 7214. https://doi.org/10.3390/jcm13237214
APA StyleLucenti, L., Maffulli, N., Bardazzi, T., Pipino, G., Pappalardo, G., & Migliorini, F. (2024). No Effect of Cigarette Smoking in the Outcome of Arthroscopic Management for Femoroacetabular Impingement: A Systematic Review. Journal of Clinical Medicine, 13(23), 7214. https://doi.org/10.3390/jcm13237214