Leading Causes of US Deaths in the 2022
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | coronavirus disease 2019 |
| CDC | Centers for Control and Prevention |
| WISQARS | Web-based Injury Statistics Query and Reporting System |
| ICD-10 | International Classification of Diseases 10th Revision |
| WHO | World Health Organization |
| NCHS | National Center for Health Statistics |
References
- Adair, T.; Mikkelsen, L.; Hooper, J.; Badr, A.; Lopez, A. Assessing the policy utility of routine mortality statistics: A global classification of countries. Bull. World Health Organ. 2023, 101, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, M.W.; Thompson, T.; McQueen, A.; Garg, R. Addressing Social Needs in Health Care Settings: Evidence, Challenges, and Opportunities for Public Health. Annu. Rev. Public. Health 2021, 42, 329–344. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.K.; Zheng, H.; Myrskylä, M. How do age and major risk factors for mortality interact over the life-course? Implications for health disparities research and public health policy. SSM Popul. Health 2019, 8, 100438. [Google Scholar]
- Janssen, F. Advances in mortality forecasting: Introduction. Genus 2018, 74, 21. [Google Scholar] [CrossRef]
- Fantini, M.P.; Lenzi, J.; Franchino, G.; Raineri, C.; Domenighetti, G.; Ricciardi, W.; Damiani, G. Mortality amenable to health care services and health inequalities among Italian Regions. Epidemiol. Prev. 2014, 38, 100–107. [Google Scholar]
- Nolte, E.; McKee, M. Measuring the health of nations: Analysis of mortality amenable to health care. BMJ 2003, 327, 1129. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Which lessons shall we learn from the 2019 novel coronavirus outbreak? Ann. Transl. Med. 2020, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Filip, R.; Puscaselu, R.G.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Foster, T.B.; Fernandez, L.; Porter, S.R.; Pharris-Ciurej, N. Racial and Ethnic Disparities in Excess All-Cause Mortality in the First Year of the COVID-19 Pandemic. Demography 2024, 61, 59–85. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). WISQARS Leading Causes of Death Visualization Tool. Available online: https://wisqars.cdc.gov/lcd/ (accessed on 19 June 2024).
- Pollack Porter, K.M.; Rutkow, L.; McGinty, E.E. The Importance of Policy Change for Addressing Public Health Problems. Public. Health Rep. 2018, 133, 9S–14S. [Google Scholar] [CrossRef]
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.A.M.; Swilam, M.M.; El-Wahed, A.A.A.; Du, M.; El-Seedi, H.H.R.; Kai, G.; Masry, S.H.D.; Abdel-Daim, M.M.; Zou, X.; Halabi, M.F.; et al. Beyond the Pandemic: COVID-19 Pandemic Changed the Face of Life. Int. J. Environ. Res. Public. Health 2021, 18, 5645. [Google Scholar] [CrossRef] [PubMed]
- Curtin, S.C.; Tejada-Vera, B.; Bastian, B.A. Deaths: Leading Causes for 2020. Natl. Vital. Stat. Rep. 2023, 72, 1–115. [Google Scholar]
- Lippi, G.; Sanchis-Gomar, F.; Lavie, C.J. Excess mortality for acute myocardial infarction in the United States during the first two years of the COVID-19 pandemic. Prog. Cardiovasc. Dis. 2024, 85, 120–121. [Google Scholar] [CrossRef] [PubMed]
- Keim-Malpass, J.; Vavolizza, R.D.; Cohn, W.F.; Kennedy, E.M.; Showalter, S.L. Cancer Screening and Treatment Delays During the COVID-19 Pandemic and the Role of Health Literacy in Care Re-engagement: Findings from an NCI-Designated Comprehensive Cancer Center sample. J. Cancer Educ. 2023, 38, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Karmali, S.; Saxena, S.; Richards, O.; Thompson, W.; McFaull, S.R.; Pike, I. What was the impact of COVID-19 restrictions on unintentional injuries, in Canada and globally? A scoping review investigating how lockdown measures impacted the global burden of unintentional injury. Front. Public. Health 2024, 12, 1385452. [Google Scholar] [CrossRef]
- Quercioli, C.; Bosco, R.; Bova, G.; Mando, M.; De Marco, M.F.; Dei, S.; Gusinu, R.; Messina, G. Evaluating the effect of COVID-19 incidence on Emergency Departments admissions. Results from a retrospective study in Central Italy during the first year of pandemic. Ann. Ig. 2023, 35, 572–585. [Google Scholar]
- Luo, W.; Liu, X.; Bao, K.; Huang, C. Ischemic stroke associated with COVID-19: A systematic review and meta-analysis. J. Neurol. 2022, 269, 1731–1740. [Google Scholar] [CrossRef]
- Sorrell, J.M. Losing a Generation: The Impact of COVID-19 on Older Americans. J. Psychosoc. Nurs. Ment. Health Serv. 2021, 59, 9–12. [Google Scholar] [CrossRef]
- Li, R.; Shen, M.; Yang, Q.; Fairley, C.K.; Chai, Z.; McIntyre, R.; Ong, J.J.; Liu, H.; Lu, P.; Hu, W.; et al. Global Diabetes Prevalence in COVID-19 Patients and Contribution to COVID-19—Related Severity and Mortality: A Systematic Review and Meta-analysis. Diabetes Care 2023, 46, 890–897. [Google Scholar] [CrossRef]
- Shetty, P.A.; Ayari, L.; Madry, J.; Betts, C.; Robinson, D.M.; Kirmani, B.F. The Relationship between COVID-19 and the Development of Depression: Implications on Mental Health. Neurosci. Insights 2023, 18, 26331055231191513. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.B.; Cisewski, J.A.; Anderson, R.N. Leading Causes of Death in the US, 2019–2023. JAMA 2024, 332, 957–958. [Google Scholar] [CrossRef] [PubMed]
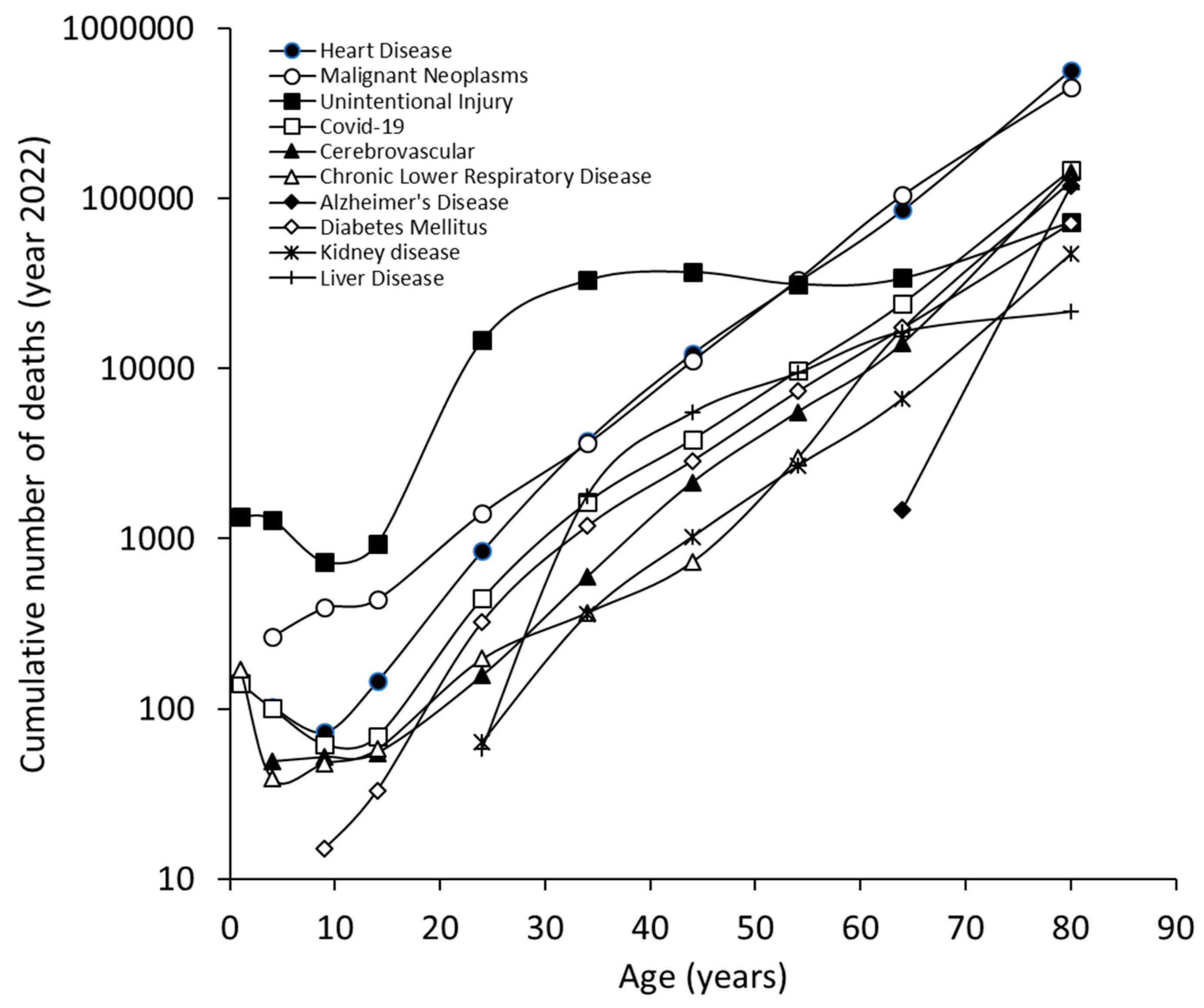
| n. | Cause | Number of Deaths | Crude Rate | Age-Adjusted Rate | Percentage of All Deaths |
|---|---|---|---|---|---|
| Cumulative | |||||
| 1 | Heart Disease | 702,880 | 210.9 | 167.2 | 26.2% |
| 2 | Malignant Neoplasms | 608,371 | 182.5 | 142.3 | 22.7% |
| 3 | Unintentional Injury | 227,039 | 68.1 | 64.0 | 8.5% |
| 4 | COVID-19 | 186,552 | 56.0 | 44.5 | 6.9% |
| 5 | Stroke | 165,393 | 49.6 | 39.5 | 6.2% |
| 6 | Chronic Lower Respiratory Disease | 147,382 | 44.2 | 34.3 | 5.5% |
| 7 | Alzheimer’s Disease | 120,122 | 36.0 | 28.9 | 4.5% |
| 8 | Diabetes Mellitus | 101,209 | 30.4 | 24.1 | 3.8% |
| 9 | Kidney disease | 57,937 | 17.4 | 13.8 | 2.2% |
| 10 | Liver Disease | 54,803 | 16.4 | 13.8 | 2.0% |
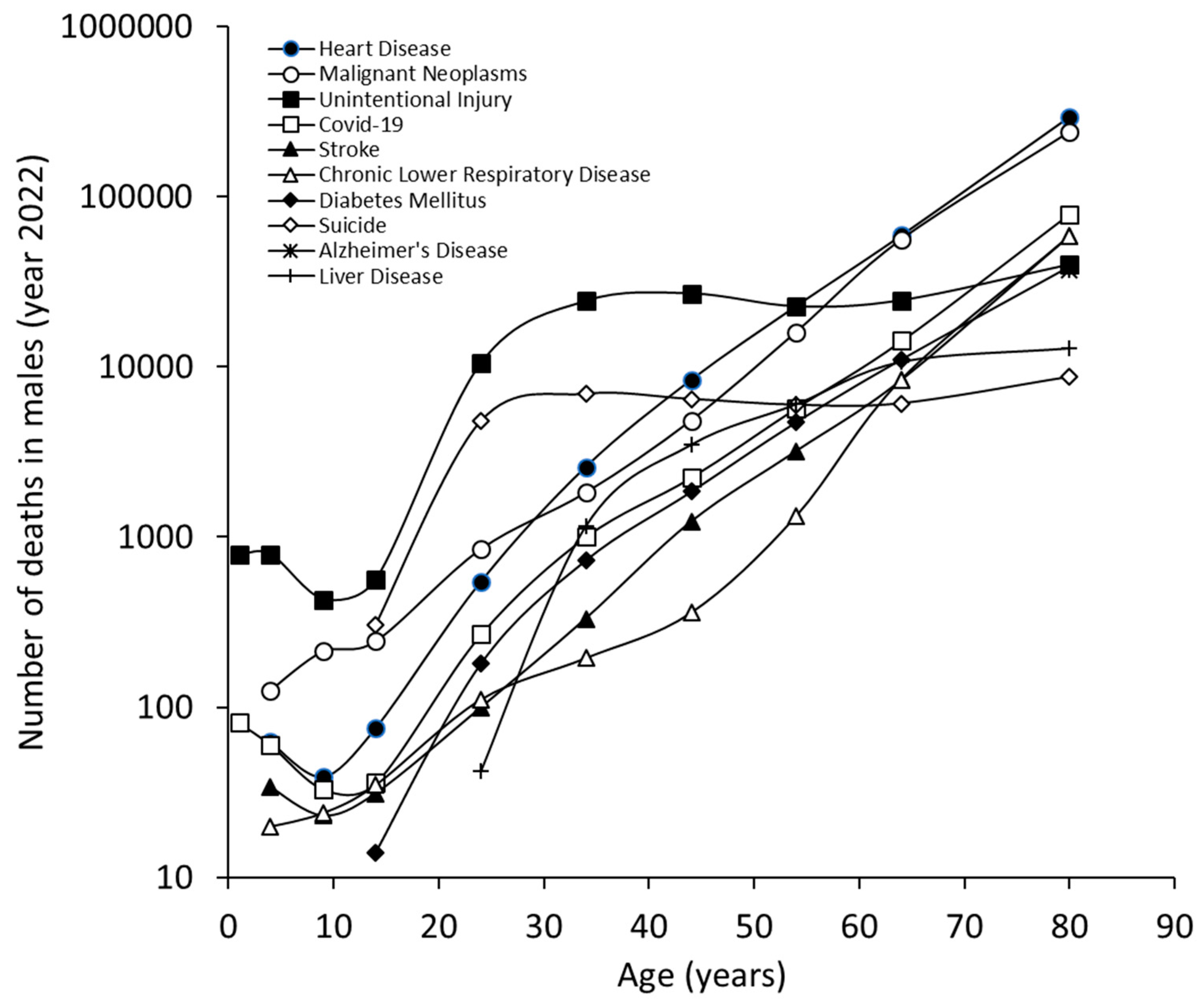
| Males | |||||
| 1 | Heart Disease | 386,766 | 234.0 | 213.5 | 26.8% |
| 2 | Malignant Neoplasms | 319,336 | 193.2 | 167.2 | 22.1% |
| 3 | Unintentional Injury | 151,629 | 91.7 | 89.5 | 10.5% |
| 4 | COVID-19 | 102,660 | 62.1 | 56.7 | 7.1% |
| 5 | Stroke | 71,819 | 43.5 | 40.5 | 5.0% |
| 6 | Chronic Lower Respiratory Disease | 69,004 | 41.7 | 37.0 | 4.8% |
| 7 | Diabetes Mellitus | 57,557 | 34.8 | 30.5 | 4.0% |
| 8 | Suicide | 39,273 | 23.8 | 23.0 | 2.7% |
| 9 | Alzheimer’s Disease | 37,475 | 22.7 | 23.0 | 2.6% |
| 10 | Liver Disease | 34,340 | 20.8 | 18.0 | 2.4% |
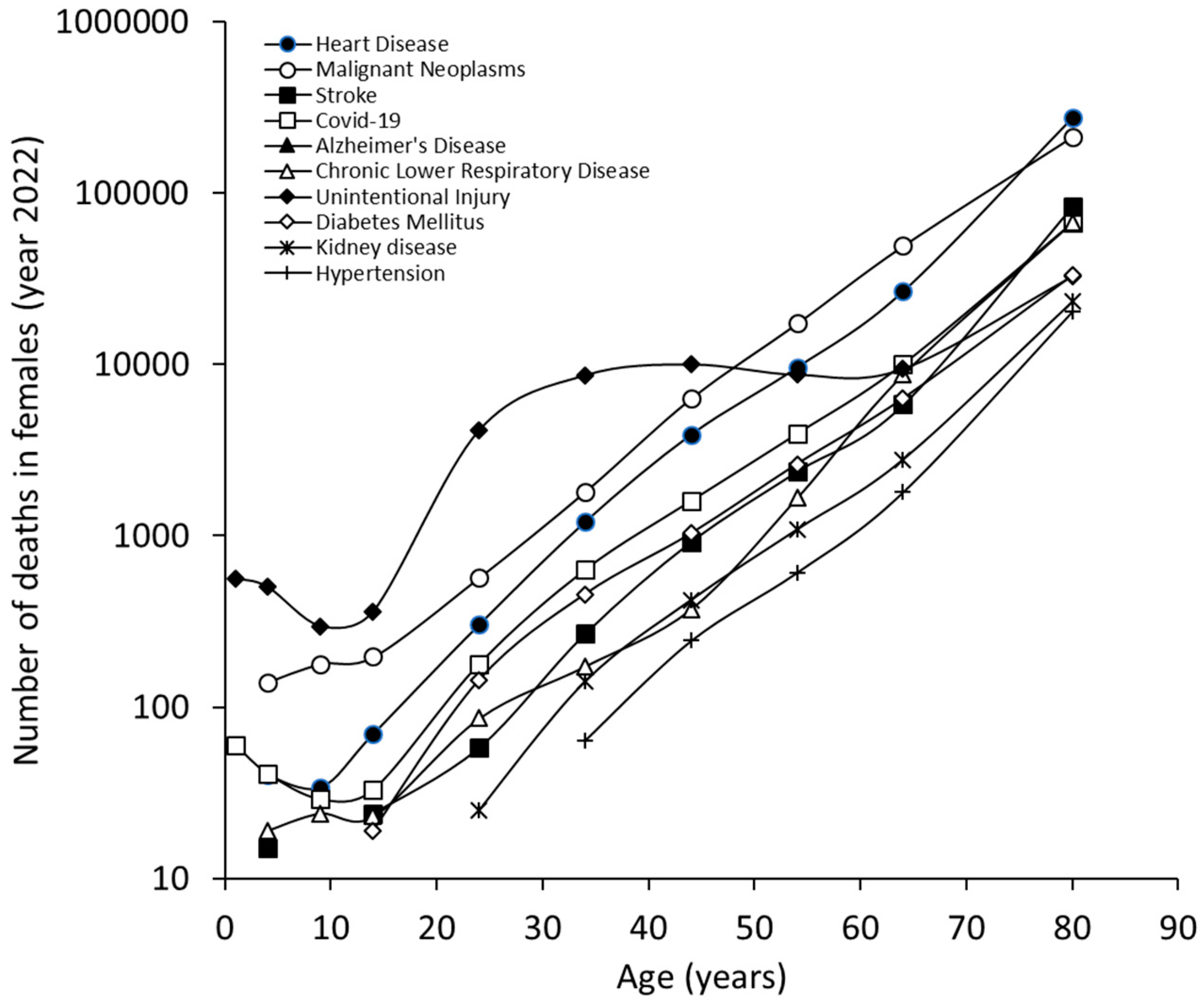
| Females | |||||
| 1 | Heart Disease | 316,114 | 188.2 | 129.5 | 25.4% |
| 2 | Malignant Neoplasms | 289,035 | 172.0 | 124.2 | 23.3% |
| 3 | Stroke | 93,574 | 55.7 | 38.2 | 7.5% |
| 4 | COVID-19 | 83,892 | 49.9 | 35.4 | 6.8% |
| 5 | Alzheimer’s Disease | 82,647 | 49.2 | 32.6 | 6.7% |
| 6 | Chronic Lower Respiratory Disease | 78,378 | 46.7 | 32.3 | 6.3% |
| 7 | Unintentional Injury | 75,410 | 44.9 | 39.4 | 6.1% |
| 8 | Diabetes Mellitus | 43,652 | 26.0 | 18.8 | 3.5% |
| 9 | Kidney disease | 27,759 | 16.5 | 11.6 | 2.2% |
| 10 | Hypertension | 23,056 | 13.7 | 9.4 | 1.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mattiuzzi, C.; Lippi, G. Leading Causes of US Deaths in the 2022. J. Clin. Med. 2024, 13, 7088. https://doi.org/10.3390/jcm13237088
Mattiuzzi C, Lippi G. Leading Causes of US Deaths in the 2022. Journal of Clinical Medicine. 2024; 13(23):7088. https://doi.org/10.3390/jcm13237088
Chicago/Turabian StyleMattiuzzi, Camilla, and Giuseppe Lippi. 2024. "Leading Causes of US Deaths in the 2022" Journal of Clinical Medicine 13, no. 23: 7088. https://doi.org/10.3390/jcm13237088
APA StyleMattiuzzi, C., & Lippi, G. (2024). Leading Causes of US Deaths in the 2022. Journal of Clinical Medicine, 13(23), 7088. https://doi.org/10.3390/jcm13237088








