Maternal Morbidity Associated with Early Preterm Birth in Low-Risk Singleton Pregnancies
Abstract
1. Introduction
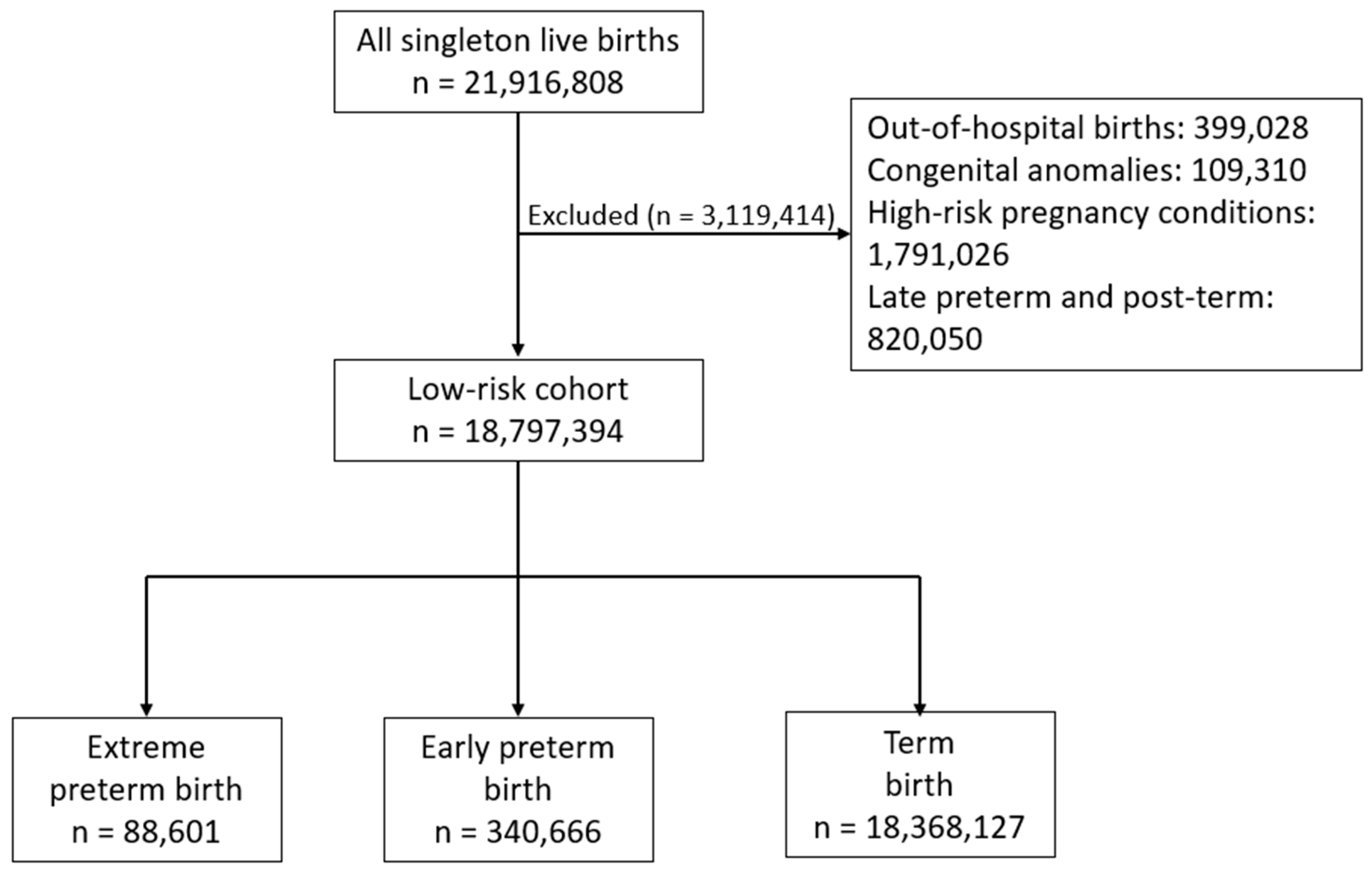
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Osterman, M.J.; Hamilton, B.E.; Martin, J.A.; Driscoll, A.K.; Valenzuela, C.P. Births: Final Data for 2022. Natl. Vital Stat. Rep. 2024, 73, 1–56. [Google Scholar] [PubMed]
- Ohuma, E.O.; Moller, A.B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Perin, J.; Mulick, A.; Yeung, D.; Villavicencio, F.; Lopez, G.; Strong, K.L.; Prieto-Merino, D.; Cousens, S.; Black, R.E.; Liu, L. Global, regional, and national causes of under-5 mortality in 2000—19: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc. Health 2022, 6, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Sarda, S.P.; Sarri, G.; Siffel, C. Global prevalence of long-term neurodevelopmental impairment following extremely preterm birth: A systematic literature review. J. Int. Med. Res. 2021, 49, 3000605211028026. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 171: Management of Preterm Labor. Obstet. Gynecol. 2016, 128, e155–e164. [Google Scholar] [CrossRef]
- Manuck, T.A.; Rice, M.M.; Bailit, J.L.; Grobman, W.A.; Reddy, U.M.; Wapner, R.J.; Thorp, J.M.; Caritis, S.N.; Prasad, M.; Tita, A.T.; et al. Preterm neonatal morbidity and mortality by gestational age: A contemporary cohort. Am. J. Obstet. Gynecol. 2016, 215, 103.e1–103.e14. [Google Scholar] [CrossRef] [PubMed]
- Raju, T.N.; Mercer, B.M.; Burchfield, D.J.; Joseph, G.F., Jr. Periviable birth: Executive summary of a joint workshop by the Eunice Kennedy Shriver Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Am. J. Obstet. Gynecol. 2014, 210, 406–417. [Google Scholar] [PubMed]
- Cerra, C.; Morelli, R.; Di Mascio, D.; Buca, D.; Di Sebastiano, F.; Liberati, M.; D’Antonio, F. Maternal outcomes of cesarean delivery performed at early gestational ages: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2021, 3, 100360. [Google Scholar] [CrossRef]
- Cahill, A.; Beigi, R.; Heine, P. Placenta accreta spectrum. Obstetric Care Consensus No. 7. American College of Obstetricians and Gynecologists. Obstet. Gynecol. 2018, 132, e259–e275. [Google Scholar]
- Centers for Disease Control and Prevention. CDC Wonder Natality Information: Natality for 2016–2021 (Expanded). Available online: https://wonder.cdc.gov/natality-expanded-current.html (accessed on 29 October 2023).
- Rossi, R.M.; De Franco, E.A. Maternal Complications Associated With Periviable Birth. Obstet. Gynecol. 2018, 132, 107–114. [Google Scholar] [CrossRef]
- Reddy, U.M.; Rice, M.M.; Grobman, W.A.; Bailit, J.L.; Wapner, R.J.; Varner, M.W.; Thorp, J.M., Jr.; Leveno, K.J.; Caritis, S.N.; Prasad, M.; et al. Serious maternal complications after early preterm delivery (24–33 weeks’ gestation). Am. J. Obstet. Gynecol. 2015, 213, 538.e1–538.e9. [Google Scholar] [CrossRef] [PubMed]
- Favilli, A.; Tosto, V.; Ceccobelli, M.; Parazzini, F.; Franchi, M.; Bini, V.; Gerli, S. Risk factors for non-adherent retained placenta after vaginal delivery: A systematic review. BMC Pregnancy Childbirth 2021, 21, 268. [Google Scholar] [CrossRef]
- Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: Postpartum Hemorrhage. Obstet. Gynecol. 2017, 130, e168–e186. [Google Scholar] [CrossRef]
- Jung, E.J.; Romero, R.; Gomez-Lopez, N.; Paredes, C.; Diaz-Primera, R.; Hernandez-Andrade, E.; Hsu, C.D.; Yeo, L. Cervical insufficiency, amniotic fluid sludge, intra-amniotic infection, and maternal bacteremia: The need for a point-of-care test to assess inflammation and bacteria in amniotic fluid. J. Matern. Fetal Neonatal Med. 2022, 35, 4775–4781. [Google Scholar] [CrossRef]
- Christiaens, I.; Zaragoza, D.B.; Guilbert, L.; Roberston, S.A.; Mitchell, B.F.; Olson, D.M. Inflammatory process in preterm and term parturition. J. Reprod. Immunol. 2008, 79, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Romero, R.; Espinoza, J.; Kusanovic, J.P.; Gotsch, F.; Hassan, S.; Erez, O.; Chaiworapongsa, T.; Mazor, M. The preterm parturition syndrome. BJOG Int. J. Obstet. Gynaecol. 2006, 113 (Suppl. S3), 17–42. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Hauth, J.C.; Andrews, W.W. Intrauterine infection and preterm delivery. N. Engl. J. Med. 2000, 342, 1500–1507. [Google Scholar] [CrossRef]
- Gobioff, S.; Lenchner, E.; Gulersen, M.; Bar-El, L.; Grünebaum, A.; Chervenak, F.A.; Bornstein, E. Risk factors associated with third- and fourth-degree perineal lacerations in singleton vaginal deliveries: A comprehensive United States population analysis 2016–2020. J. Perinat. Med. 2023, 51, 1006–1012. [Google Scholar] [CrossRef]
- Perry, A.K.; Rossi, R.M.; De Franco, E.A. Severe adverse maternal outcomes associate with chorioamnionitis. Am. J. Obstet. Gynecol. MFM 2019, 1, 100027. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No. 6: Periviable Birth. Obstet. Gynecol. 2017, 130, e187–e199. [Google Scholar] [CrossRef] [PubMed]
| Extreme Preterm Births 23 0/7–27 6/7 Weeks (n = 88,601) | Early Preterm Births 28 0/7–33 6/7 Weeks (n = 340,666) | Term Births 37 0/7–41 6/7 Weeks (n = 18,368,127) | p Value | |
|---|---|---|---|---|
| Maternal age (years) | <0.001 | |||
| <20 | 6179 (7.0) | 19,405 (5.7) | 880,428 (4.8) | |
| 20–24 | 18,106 (20.5) | 64,808 (19.1) | 3,549,418 (19.4) | |
| 25–29 | 23,447 (26.6) | 88,662 (26.1) | 5,310,755 (29.0) | |
| 30–34 | 22,621 (25.6) | 92,045 (27.1) | 5,307,570 (29.0) | |
| 35–39 | 14,159 (16.0) | 58,089 (17.1) | 2,715,975 (14.8) | |
| ≥40 | 3752 (4.3) | 16,098 (4.7) | 564,337 (3.1) | |
| Body mass index (kg/m2) | <0.001 | |||
| <18.5 | 2842 (3.4) | 12,811 (3.9) | 556,879 (3.1) | |
| 18.5–24.9 | 27,035 (32.4) | 116,820 (35.9) | 7,506,115 (41.7) | |
| 25–29.9 | 21,021 (25.2) | 82,078 (25.2) | 4,830,199 (26.9) | |
| 30–34.9 | 15,627 (18.7) | 56,152 (17.3) | 2,759,017 (15.3) | |
| 35–39.9 | 9290 (11.1) | 31,386 (9.6) | 1,360,927 (7.6) | |
| ≥40 | 7619 (9.1) | 26,050 (8.0) | 970,686 (5.4) | |
| Education | <0.001 | |||
| Less than high school | 13,530 (15.7) | 52,621 (15.7) | 2,231,357 (12.3) | |
| High school graduate | 28,002 (32.4) | 100,989 (30.2) | 4,723,452 (26.0) | |
| Some college credit | 26,645 (30.8) | 99,780 (29.9) | 5,118,070 (28.2) | |
| College graduate | 11,968 (13.8) | 51,325 (15.4) | 3,789,271 (20.9) | |
| Master’s or higher | 6287 (7.3) | 29,550 (8.8) | 2,270,181 (12.5) | |
| Insurance type | <0.001 | |||
| Medicaid | 46,288 (52.2) | 172,316 (50.6) | 7,739,174 (42.1) | |
| Private | 34,652 (39.1) | 140,657 (41.3) | 9,239,734 (50.3) | |
| Self pay/other | 7661 (8.6) | 27,693 (8.1) | 1,389,219 (7.6) | |
| Race or ethnic group | <0.001 | |||
| Non-Hispanic white | 30,094 (34.0) | 143,087 (42.0) | 9,368,005 (51.0) | |
| Non-Hispanic black | 29,407 (33.2) | 83,476 (24.5) | 2,574,516 (14.0) | |
| Other/multiracial | 3929 (3.7) | 14,952 (4.4) | 697,087 (3.8) | |
| Asian and Pacific Islander | 4271 (5.6) | 19,081 (5.6) | 1,250,744 (6.8) | |
| Hispanic | 20,830 (23.5) | 80,070 (23.5) | 4,477,775 (24.4) | |
| Prenatal Care | <0.001 | |||
| Initiated in first-trimester | 60,823 (74.4) | 238,784 (74.3) | 14,070,178 (78.3) | |
| Initiated in second-trimester | 13,061 (16.0) | 51,775 (16.1) | 2,844,413 (15.8) | |
| Initiated in third-trimester | 55 (0.1) | 8592 (2.7) | 792,373 (4.4) | |
| No prenatal care | 7822 (9.6) | 22,281 (6.9) | 263,657 (1.5) | |
| Tobacco use during pregnancy | 7841 (8.9) | 33,009 (9.8) | 1,097,338 (6.0) | <0.001 |
| Chorioamnionitis | 4544 (5.4) | 7746 (2.4) | 280,394 (1.6) | <0.001 |
| Cesarean delivery | 57,367 (64.7) | 204,687 (60.1) | 5,490,890 (29.9) | <0.001 |
| Extreme Preterm Births 23 0/7–27 6/7 Weeks (n = 88,601) | Term Births 37 0/7–41 6/7 Weeks (n = 18,368,127) | Unadjusted OR (95% CI) | * Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Maternal transfusion | 1457 (1.6) | 59,316 (0.3) | 5.16 (4.90–5.44) | 3.32 (3.13–3.53) |
| Uterine rupture | 181 (0.2) | 4783 (0.03) | 7.86 (6.78–9.12) | 3.75 (3.14–4.48) |
| Unplanned hysterectomy | 245 (0.3) | 5451 (0.03) | 9.34 (8.22–10.62) | 5.60 (4.85–6.48) |
| ICU admission | 1731 (2.0) | 17,507 (0.1) | 20.89 (19.88–21.96) | 10.58 (9.97–11.54) |
| Third- or fourth-degree perineal laceration | 25 (0.03) | 146,849 (0.8) | 0.04 (0.02–0.05) | 0.07 (0.04–0.11) |
| Early Preterm Births 28 0/7–33 6/7 Weeks (n = 340,666) | Term Births 37 0/7–41 6/7 Weeks (n = 18,368,127) | Unadjusted OR (95% CI) | * Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Maternal transfusion | 4483 (1.3) | 59,316 (0.3) | 4.12 (3.99–4.24) | 2.96 (2.86–3.07) |
| Uterine rupture | 601 (0.2) | 4783 (0.03) | 6.79 (6.23–7.39) | 4.13 (3.76–4.54) |
| Unplanned hysterectomy | 970 (0.3) | 5451 (0.03) | 9.62 (8.99–10.30) | 5.92 (5.47–6.40) |
| ICU admission | 5620 (1.7) | 17,507 (0.1) | 17.59 (17.06–18.13) | 10.13 (9.77–10.50) |
| Third- or fourth-degree perineal laceration | 336 (0.1) | 146,849 (0.8) | 0.12 (0.11–0.14) | 0.23 (0.20–0.26) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gulersen, M.; Lenchner, E.; Goyal, A.; Grunebaum, A.; Chervenak, F.A.; Bornstein, E. Maternal Morbidity Associated with Early Preterm Birth in Low-Risk Singleton Pregnancies. J. Clin. Med. 2024, 13, 7061. https://doi.org/10.3390/jcm13237061
Gulersen M, Lenchner E, Goyal A, Grunebaum A, Chervenak FA, Bornstein E. Maternal Morbidity Associated with Early Preterm Birth in Low-Risk Singleton Pregnancies. Journal of Clinical Medicine. 2024; 13(23):7061. https://doi.org/10.3390/jcm13237061
Chicago/Turabian StyleGulersen, Moti, Erez Lenchner, Alisha Goyal, Amos Grunebaum, Frank A. Chervenak, and Eran Bornstein. 2024. "Maternal Morbidity Associated with Early Preterm Birth in Low-Risk Singleton Pregnancies" Journal of Clinical Medicine 13, no. 23: 7061. https://doi.org/10.3390/jcm13237061
APA StyleGulersen, M., Lenchner, E., Goyal, A., Grunebaum, A., Chervenak, F. A., & Bornstein, E. (2024). Maternal Morbidity Associated with Early Preterm Birth in Low-Risk Singleton Pregnancies. Journal of Clinical Medicine, 13(23), 7061. https://doi.org/10.3390/jcm13237061






