Minimally Invasive Repair of Pectus Excavatum: A Lifeline to Quality of Life
Abstract
1. Introduction
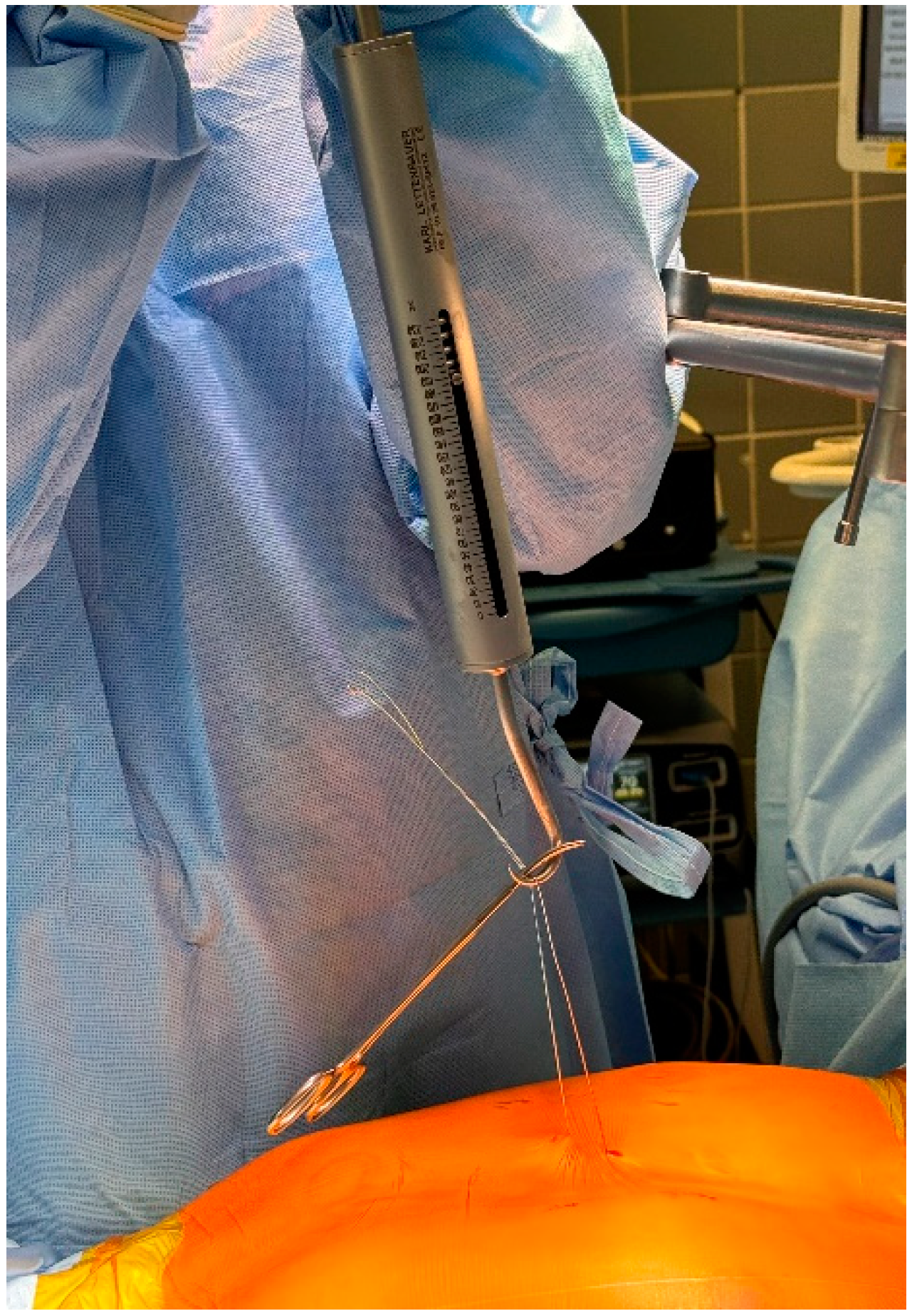
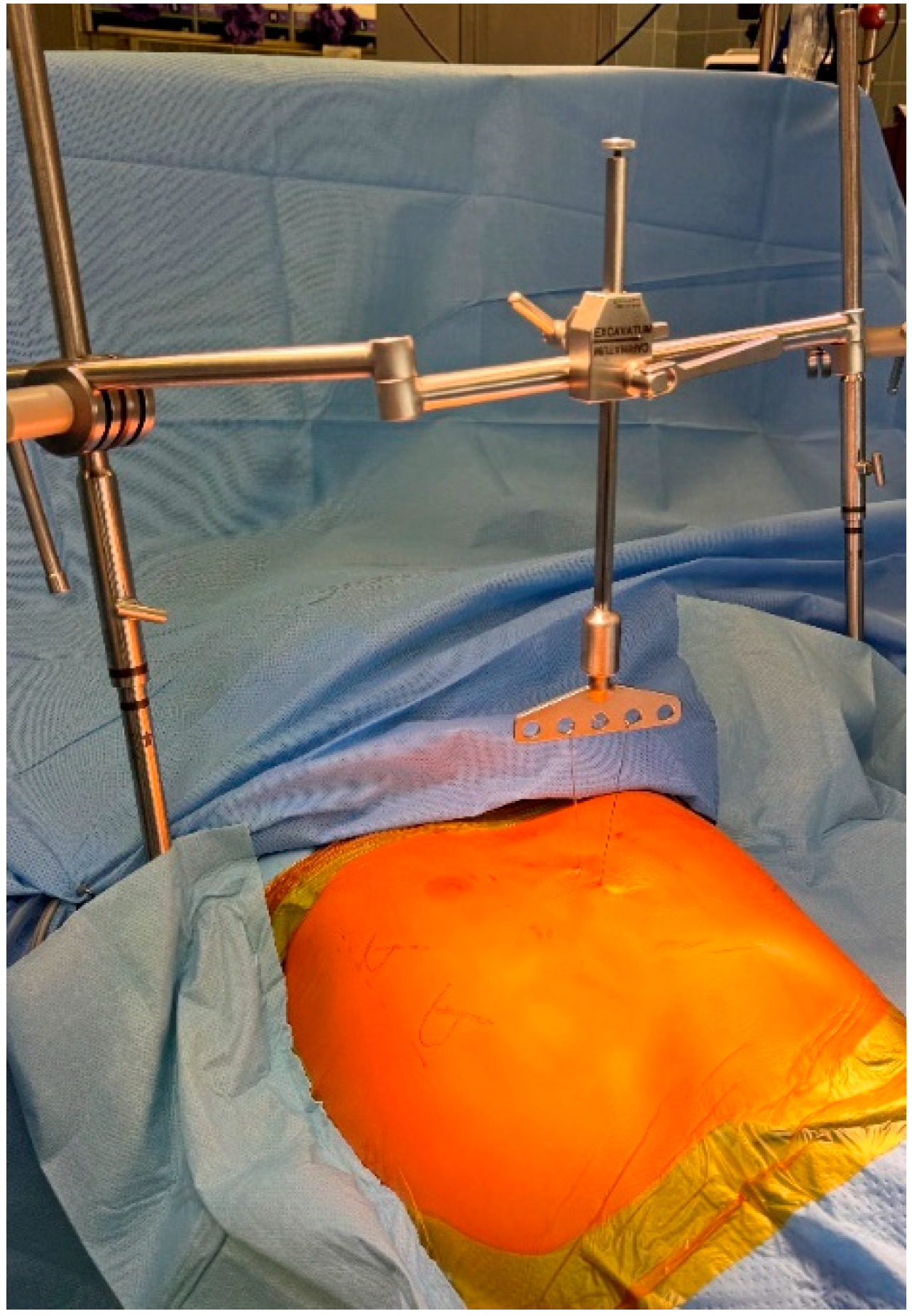
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nuss, D.; Kelly, R.E., Jr.; Croitoru, D. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J. Pediatr. Surg. 1998, 33, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Fokin, A.A.; Steuerwald, N.M.; Ahrens, W.A.; Allen, K.E. Anatomical, histologic, and genetic characteristics of congenital chest wall deformities. Semin. Thorac. Cardiovasc. Surg. 2009, 21, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Poston, P.M.; Patel, S.S.; Rajput, M.; Rossi, N.O.; Ghanamah, M.S.; Davis, J.E.; Turek, J.W. The correction index: Setting the standard for recommending operative repair of pectus excavatum. Ann. Thorac. Surg. 2014, 97, 1176–1179, discussion 1179–1180. [Google Scholar] [CrossRef] [PubMed]
- Haller, J.A., Jr.; Kramer, S.; Lietman, S. Use of CT scans in selection of patients for pectus excavatum surgery: A preliminary report. J. Pediatr. Surg. 1987, 22, 904–906. [Google Scholar] [CrossRef] [PubMed]
- Stieglitz, R.-D. Bullinger, M. & Kirchberger, I. (1998). SF-36. Fragebogen zum Gesundheitszustand. Göttingen: Hogrefe. Preis DM 298. Z. Klin. Psychol. Psychother. 1999, 28, 143–145. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Ellert, U.; Kurth, B.M. Health related quality of life in adults in Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Brazier, J.E.; Harper, R.; Jones, N.M.; O’Cathain, A.; Thomas, K.J.; Usherwood, T.; Westlake, L. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ 1992, 305, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.E., Jr.; Mellins, R.B.; Shamberger, R.C.; Mitchell, K.K.; Lawson, M.L.; Oldham, K.T.; Azizkhan, R.G.; Hebra, A.V.; Nuss, D.; Goretsky, M.J.; et al. Multicenter study of pectus excavatum, final report: Complications, static/exercise pulmonary function, and anatomic outcomes. J. Am. Coll. Surg. 2013, 217, 1080–1089. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.E.; Daniel, A. Outcomes, quality of life, and long-term results after pectus repair from around the globe. Semin. Pediatr. Surg. 2018, 27, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Hebra, A.; Kelly, R.E.; Ferro, M.M.; Yuksel, M.; Campos, J.R.M.; Nuss, D. Life-threatening complications and mortality of minimally invasive pectus surgery. J. Pediatr. Surg. 2018, 53, 728–732. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The constitution of the World Health Organization; WHO Chronicle; WHO: Geneva, Switzerland, 1947; Volume 1, p. 29. [Google Scholar]
- O’Keefe, J.; Byrne, R.; Montgomery, M.; Harder, J.; Roberts, D.; Sigalet, D.L. Longer term effects of closed repair of pectus excavatum on cardiopulmonary status. J. Pediatr. Surg. 2013, 48, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.E., Jr.; Cash, T.F.; Shamberger, R.C.; Mitchell, K.K.; Mellins, R.B.; Lawson, M.L.; Oldham, K.; Azizkhan, R.G.; Hebra, A.V.; Nuss, D.; et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: Multicenter study. Pediatrics 2008, 122, 1218–1222. [Google Scholar] [CrossRef] [PubMed]
- Sigalet, D.L.; Montgomery, M.; Harder, J. Cardiopulmonary effects of closed repair of pectus excavatum. J. Pediatr. Surg. 2003, 38, 380–385, discussion 380–385. [Google Scholar] [CrossRef] [PubMed]
- Farina, J.M.; Yinadsawaphan, T.; Jaroszewski, D.E.; Aly, M.R.; Botros, M.; Cheema, K.P.; Fatunde, O.A.; Sorajja, D. The electrocardiographic manifestations of pectus excavatum before and after surgical correction. J. Electrocardiol. 2024, 82, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Jaroszewski, D.E.; Farina, J.M.; Gotway, M.B.; Stearns, J.D.; Peterson, M.A.; Pulivarthi, V.S.K.K.; Bostoros, P.; Abdelrazek, A.S.; Gotimukul, A.; Majdalany, D.S.; et al. Cardiopulmonary Outcomes After the Nuss Procedure in Pectus Excavatum. J. Am. Heart Assoc. 2022, 11, e022149. [Google Scholar] [CrossRef] [PubMed]
- Jaroszewski, D.; Notrica, D.; McMahon, L.; Steidley, D.E.; Deschamps, C. Current management of pectus excavatum: A review and update of therapy and treatment recommendations. J. Am. Board. Fam. Med. 2010, 23, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Steinmann, C.; Krille, S.; Mueller, A.; Weber, P.; Reingruber, B.; Martin, A. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: A control group comparison of psychological characteristics prior to surgical correction. Eur. J. Cardiothorac. Surg. 2011, 40, 1138–1145. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | |
|---|---|
| Age, y, median (IQR; range) | 18.7 (6.2; 14–51) |
| Gender, n (%) | |
| Male | 195 (83) |
| Female | 39 (17) |
| Haller index, median (IQR) | 4.0 (1.3) |
| Preoperative symptoms, n (%) | |
| Exercise intolerance | 199 (85.0) |
| Psychosocial complaints | 156 (66.7) |
| Dyspnea at rest | 168 (71.8) |
| Cardiovascular Symptoms | 134 (57.3) |
| Chest pain other than angina pectoris | 80 (34.2) |
| Back pain | 83 (35.5) |
| Muscle stiffness | 38 (16.2) |
| Gastrointestinal Symptoms | 8 (3.4) |
| Dimension (abbr.) | No° of Questions | |
|---|---|---|
| Functional status | Physical functioning (PF) | 10 |
| Social functioning (SF) | 2 | |
| Physical role limitations (PRL) | 4 | |
| Emotional role limitations (ERL) | 3 | |
| Well-being | Mental health (MH) | 5 |
| Vitality (VI) | 4 | |
| Bodily Pain (PA) | 2 | |
| General health perception (GH) | 5 | |
| Health change | 1 | |
| Total | 36 |
| Physical Functioning (PF) | This domain assesses the patient’s ability to perform basic and advanced physical activities of daily living. |
| Social Functioning (SF) | This domain evaluates the patient’s ability to participate in social activities and maintain social relationships. |
| Physical role limitations (PRL) | This domain evaluates the impact of physical health on the patient’s ability to carry out work or other significant role-related activities. |
| Emotional role limitations (ERL) | This domain assesses the impact of emotional problems on the patient’s ability to perform work or other role-related activities. |
| Mental health (MH) | This domain reflects the patient’s overall emotional and psychological well-being |
| Vitality (VI) | This domain assesses the patient’s energy levels and overall sense of well-being. |
| Bodily pain (PA) | This domain measures the intensity and interference of pain on daily life. |
| General health (GH) | This domain captures the patient’s subjective assessment of their overall health status. |
| Characteristics | |
|---|---|
| Bars inserted, n (%) | |
| 1 bar | 86 (37) |
| 2 bars | 140 (60) |
| 3 bars | 8 (3) |
| Bar length, inches, median (IQR) | |
| Cranial bar | 12 (2) |
| Caudal bar | 12 (1) |
| Tensiometrie, Nm, median (IQR) | 160 (50) |
| Operation time, min, median (IQR) | 89 (38) |
| Length of hospital stay, d, median (IQR) | 7 (2) |
| Postoperative morbidity, n (%) | |
| Bar displacement requiring reoperation | 9 (3.8) |
| Empyema | 2 (0.85) |
| Deep wound infection requiring reoperation | 3 (1.28) |
| Pleural effusion requiring intervention | 2 (0.85) |
| Pneumothorax requiring intervention | 10 (4.27) |
| Hemothorax requiring intervention | 2 (0.85) |
| Recurrence after bar removal | 2 (0.85) |
| Wound infection | 4 (1.7) |
| Chronic pain | 5 (2.13) |
| Characteristics | German Population | Before Surgery | After Surgery | p-Value |
|---|---|---|---|---|
| Physical functioning (PF) | 94.9 (94.0–95.7) | 80.02 ± 20.7 | 94.68 ± 14.0 | 0.087 |
| Social Functioning (SF) | 87.1 (85.6–88.7) | 68.05 ± 28.8 | 91.27 ± 16.2 | <0.001 |
| Physical role limitations (PRL) | 91.5 (90.4–92.6) | 68.78 ± 38.7 | 89.69 ± 27.3 | 0.016 |
| Emotional role limitations (ERL) | 88.8 (87.4–90.1) | 67.72 ± 40.3 | 94.53 ± 19.7 | 0.003 |
| Mental health (MH) | 72.4 (71.2–73.5) | 65.19 ± 19.8 | 83.75 ± 13.6 | <0.001 |
| Vitality (VI) | 60.4 (59.4–61.4) | 49.23 ± 19.6 | 71.43 ± 19.0 | <0.001 |
| Bodily pain (PA) | 85.0 (83.5–86.5) | 68.34 ± 27.7 | 84.50 ± 21.7 | 0.002 |
| General health (GH) | 74.5 (73.3–75.6) | 61.03 ± 23.2 | 86.54 ± 16.8 | <0.001 |
| Summary | ||||
| Physical Component Summary Score (PCS) | 55.8 (55.4–56.2) | 47.36 ± 10.2 | 53.99 ± 7.6 | 0.007 |
| Mental Component Summary Score (MCS) | 48.0 (47.3–48.7) | 43.70 ± 11.5 | 54.42 ± 7.3 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Higaze, M.; Haj Khalaf, M.A.; Parjiea, C.; Sirbu, H. Minimally Invasive Repair of Pectus Excavatum: A Lifeline to Quality of Life. J. Clin. Med. 2024, 13, 6888. https://doi.org/10.3390/jcm13226888
Higaze M, Haj Khalaf MA, Parjiea C, Sirbu H. Minimally Invasive Repair of Pectus Excavatum: A Lifeline to Quality of Life. Journal of Clinical Medicine. 2024; 13(22):6888. https://doi.org/10.3390/jcm13226888
Chicago/Turabian StyleHigaze, Mostafa, Mohamed Anwar Haj Khalaf, Chirag Parjiea, and Horia Sirbu. 2024. "Minimally Invasive Repair of Pectus Excavatum: A Lifeline to Quality of Life" Journal of Clinical Medicine 13, no. 22: 6888. https://doi.org/10.3390/jcm13226888
APA StyleHigaze, M., Haj Khalaf, M. A., Parjiea, C., & Sirbu, H. (2024). Minimally Invasive Repair of Pectus Excavatum: A Lifeline to Quality of Life. Journal of Clinical Medicine, 13(22), 6888. https://doi.org/10.3390/jcm13226888






