Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- has been diagnosed with acetabular erosion in the clinical notes, serial radiographs or radiology reports, and
- presented with chronic hip, groin, or gluteal pain after HA surgery with an intensity of ≥4 on a 0–10 pain scoring chart (visual analog scale) which increases with weight-bearing, active, or passive hip movement that was attributed to acetabular erosion, as decided by the treating physician, and/or
- underwent or was planned for revision hip arthroplasty for chronic hip or groin pain secondary to acetabular erosion as decided by the treating physician. Conversion to THA was decided by the treating surgeon based mainly on the presence of symptomatic acetabular wear that could not be controlled conservatively.
2.2. Exclusion Criteria
- Patients with a history of postoperative periprosthetic infection.
- Patients who had a positive bacterial culture that was obtained by hip aspiration, sonication, or biopsy.
- Patients with any records of prosthetic dislocation.
- Patients who sustained ipsilateral periprosthetic or acetabular fracture.
3. Statistical Analysis
4. Results
Symptomatic Acetabular Erosion
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhandari, M.; Devereaux, P.J.; Tornetta, P., 3rd; Swiontkowski, M.F.; Berry, D.J.; Haidukewych, G.; Schemitsch, E.H.; Hanson, B.P.; Koval, K.; Dirschl, D.; et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J. Bone Jt. Surg. 2005, 87, 2122–2130. [Google Scholar] [CrossRef] [PubMed]
- Zelle, B.A.; Salazar, L.M.; Howard, S.L.; Parikh, K.; Pape, H.C. Surgical treatment options for femoral neck fractures in the elderly. Int. Orthop. 2022, 46, 1111–1122. [Google Scholar] [CrossRef] [PubMed]
- Guyen, O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop. Traumatol. Surg. Res. 2019, 105, S95–S101. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.N.; El-Husseini, T.; Elabd, M.A.; Soliman, R.A.; Maziad, A.M.; Horwitz, D.S. Metastatic Hip Disease in the Elderly: Does Uncemented Hip Hemiarthroplasty have a Role? SciBase Oncol. 2024, 2, 1015. [Google Scholar]
- Chammout, G.K.; Mukka, S.S.; Carlsson, T.; Neander, G.F.; Stark, A.W.; Skoldenberg, O.G. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: A randomized long-term follow-up study. J. Bone Jt. Surg. 2012, 94, 1921–1928. [Google Scholar] [CrossRef]
- Johansson, T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: A minimum fifteen-year follow-up study of a previously reported randomized trial. J. Bone Jt. Surg. 2014, 96, 46. [Google Scholar] [CrossRef]
- Leonardsson, O.; Sernbo, I.; Carlsson, A.; Akesson, K.; Rogmark, C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: Results at ten years in a randomised study of 450 patients. J. Bone Jt. Surg. 2010, 92, 406–412. [Google Scholar] [CrossRef]
- Keating, J.F.; Grant, A.; Masson, M.; Scott, N.W.; Forbes, J.F. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J. Bone Jt. Surg. 2006, 88, 249–260. [Google Scholar] [CrossRef]
- Health Investigators. Total hip arthroplasty or hemiarthroplasty for hip fracture. New Engl. J. Med. 2019, 381, 2199–2208. [Google Scholar] [CrossRef]
- Hedbeck, C.J.; Enocson, A.; Lapidus, G.; Blomfeldt, R.; Törnkvist, H.; Ponzer, S.; Tidermark, J. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: A concise four-year follow-up of a randomized trial. J. Bone Jt. Surg. 2011, 93, 445–450. [Google Scholar] [CrossRef]
- Macaulay, W.; Nellans, K.W.; Garvin, K.L.; Iorio, R.; Healy, W.L.; Rosenwasser, M.P.; other members of the DFACTO Consortium. Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: Winner of the Dorr Award. J. Arthroplast. 2008, 23, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Leonardsson, O.; Rolfson, O.; Hommel, A.; Garellick, G.; Åkesson, K.; Rogmark, C. Patient-reported outcome after displaced femoral neck fracture: A national survey of 4467 patients. J Bone Jt. Surg 2013, 95, 1693–1699. [Google Scholar] [CrossRef] [PubMed]
- Rogmark, C.; Leonardsson, O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Jt. J. 2016, 98, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.P.; Squires, B.; Gargan, M.F.; Bannister, G.C. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J. Bone Jt. Surg. 2006, 88, 2583–2589. [Google Scholar] [CrossRef] [PubMed]
- Macheras, G.A.; Pallis, D.; Tsivelekas, K.; Ampadiotaki, M.M.; Lepetsos, P.; Tzefronis, D.; Kateros, K.; Papadakis, S.A. Acetabular erosion after bipolar hip hemiarthroplasty for femoral neck fracture in elderly patients: A retrospective study. Hip Int. 2023, 34, 402–408. [Google Scholar] [CrossRef]
- Schiavi, P.; Pogliacomi, F.; Colombo, M.; Amarossi, A.; Ceccarelli, F.; Vaienti, E. Acetabular erosion following bipolar hemiarthroplasty: A Role for the size of femoral head? Injury 2019, 50, S21–S25. [Google Scholar] [CrossRef]
- Alazzawi, S.; Sprenger De Rover, W.B.; Brown, J.; Davis, B. The conversion rate of bipolar hemiarthroplasty after a hip fracture to a total hip arthroplasty. Clin. Orthop. Surg. 2012, 4, 117–120. [Google Scholar] [CrossRef]
- Hsu, K.H.; Tsai, S.W.; Chen, C.F.; Chang, M.C.; Chen, W.M. The risk factors of early acetabular failure after bipolar hemiarthroplasty because of fracture of the femoral neck. J. Chin. Med. Assoc. 2019, 82, 419–423. [Google Scholar] [CrossRef]
- Theil, C.; Möllenbeck, B.; Gosheger, G.; Schmidt-Bräkling, T.; Andreou, D.; Henrichs, M.P.; Dieckmann, R. Acetabular Erosion After Bipolar Hemiarthroplasty in Proximal Femoral Replacement for Malignant Bone Tumors. J. Arthroplast. 2019, 34, 2692–2697. [Google Scholar] [CrossRef]
- Emre, F.; Ertaş, E.S.; Bozkurt, M. Factors associated with acetabular degeneration and protrusion in bipolar hip hemiarthroplasty. Genel Tıp Dergisi. 2022, 32, 564–570. [Google Scholar] [CrossRef]
- Vajapey, S.P.; Morris, J.; Spitzer, A.I.; Glassman, A.H.; Greco, N.J.; Li, M. Outcome reporting patterns in total knee arthroplasty: A systematic review. J. Clin. Orthop. Trauma 2020, 11, S464–S471. [Google Scholar] [CrossRef] [PubMed]
- Panula, J.; Pihlajamäki, H.; Mattila, V.M.; Jaatinen, P.; Vahlberg, T.; Aarnio, P.; Kivelä, S.L. Mortality and cause of death in hip fracture patients aged 65 or older: A population-based study. BMC Musculoskelet. Disord. 2011, 12, 105. [Google Scholar] [CrossRef] [PubMed]
- Guzon-Illescas, O.; Perez Fernandez, E.; Crespí Villarias, N.; Quirós Donate, F.J.; Peña, M.; Alonso-Blas, C.; García-Vadillo, A.; Mazzucchelli, R. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. Res. 2019, 14, 203. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Bi, N.; Zheng, J.; Xi, N. Does total hip arthroplasty provide better outcomes than hemiarthroplasty for the femoral neck fracture? A systematic review and meta-analysis. Chin. J. Traumatol. 2020, 23, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, N.M.; Fruth, K.M.; Larson, D.R.; Kremers, H.M.; Sierra, R.J. Conversion of Hemiarthroplasty to THA Carries an Increased Risk of Reoperation Compared With Primary and Revision THA. Clin. Orthop. Relat. Res. 2019, 477, 1392–1399. [Google Scholar] [CrossRef]
- Hoskins, W.; Corfield, S.; Lorimer, M.; Peng, Y.; Bingham, R.; Graves, S.E.; Vince, K.G. Is the Revision Rate for Femoral Neck Fracture Lower for Total Hip Arthroplasty Than for Hemiarthroplasty?: A Comparison of Registry Data for Contemporary Surgical Options. J. Bone Jt. Surg. Am. 2022, 104, 1530–1541. [Google Scholar] [CrossRef]
- Moon, N.H.; Shin, W.C.; Do, M.U.; Kang, S.W.; Lee, S.M.; Suh, K.T. High conversion rate to total hip arthroplasty after hemiarthroplasty in young patients with a minimum 10 years follow-up. BMC Musculoskelet. Disord. 2021, 22, 273. [Google Scholar] [CrossRef]
- Grosso, M.J.; Danoff, J.R.; Murtaugh, T.S.; Trofa, D.P.; Sawires, A.N.; Macaulay, W.B. Hemiarthroplasty for Displaced Femoral Neck Fractures in the Elderly Has a Low Conversion Rate. J. Arthroplast. 2017, 32, 150–154. [Google Scholar] [CrossRef]
- Zucchini, R.; Sambri, A.; Fiore, M.; Giannini, C.; Donati, D.M.; De Paolis, M. Megaprosthesis Reconstruction of the Proximal Femur following Bone Tumour Resection: When Do We Need the Cup? Hip Pelvis 2021, 33, 147–153. [Google Scholar] [CrossRef]
- Jeffcote, B.; Li, M.G.; Barnet-Moorcroft, A.; Wood, D.; Nivbrant, B. Roentgen stereophotogrammetric analysis and clinical assessment of unipolar versus bipolar hemiarthroplasty for subcapital femur fracture: A randomized prospective study. ANZ J. Surg. 2010, 80, 242–246. [Google Scholar] [CrossRef]
- Figved, W.; Svenøy, S.; Röhrl, S.M.; Dahl, J.; Nordsletten, L.; Frihagen, F. Higher cartilage wear in unipolar than bipolar hemiarthroplasties of the hip at 2 years: A randomized controlled radiostereometric study in 19 fit elderly patients with femoral neck fractures. Acta Orthop. 2018, 89, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Hedbeck, C.J.; Blomfeldt, R.; Lapidus, G.; Törnkvist, H.; Ponzer, S.; Tidermark, J. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: A randomised, controlled trial. Int. Orthop. 2011, 35, 1703–1711. [Google Scholar] [CrossRef] [PubMed]
- Inngul, C.; Hedbeck, C.J.; Blomfeldt, R.; Lapidus, G.; Ponzer, S.; Enocson, A. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures: A four-year follow-up of a randomised controlled trial. Int. Orthop. 2013, 37, 2457–2464. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.Q.; Mohammad, J.; Qamar, R.; Siddiqui, Y.S.; Sabir, A.B.; Abbas, M. Cemented unipolar or modular bipolar hemiarthroplasty for femoral neck fractures in elderly patients—Which is better? Int. J. Burn. Trauma 2021, 11, 447–455. [Google Scholar]
- Rosen, L.L.; Miller, B.J.; Dupuis, P.R.; Jarzem, P.; Hadjipavlou, A. A prospective randomized study comparing bipolar hip arthroplasty and hemiarthroplasty in elderly patients with subcapital fractures. J. Bone Jt. Surg. Br. 1992, 74, 282. [Google Scholar]
- Comeau-Gauthier, M.; Bzovsky, S.; Axelrod, D.; Poolman, R.W.; Frihagen, F.; Bhandari, M.; Schemitsch, E.; Sprague, S.; HEALTH investigators. Is the use of bipolar hemiarthroplasty over monopolar hemiarthroplasty justified? A propensity score-weighted analysis of a multicentre randomized controlled trial. Bone Jt. Open 2023, 4, 370–377. [Google Scholar] [CrossRef]


| Age at the Time of Surgery | Less than 65 | Patients 65–80 | Patients Older than 80 |
|---|---|---|---|
| Number (cases) | 172 | 752 | 1553 |
| Percentage | 6.9% | 30.3% | 62.7% |
| Mean age | 57.6 | 74.2 | 87.7 |
| Mean follow-up | 4.9 years | 3.85 years | 3.5 years |
| Incidence of symptomatic acetabular erosion | 3/172 (1.7%) | 5/752 (0.66%) | 4/1553 (0.26%) |
| Chi-square test: p = 0.0199 (statistically insignificant) | |||
| Mortality at | Number of Cases | Percent |
|---|---|---|
| 3 months | 327 | 13.9% |
| 1 year | 558 | 22.5% |
| 3 years | 884 | 35.7% |
| 5 years | 1054 | 42.5% |
| Follow-Up Term [21] | Short Term: Less than 2 Years | Midterm 2–10 Years | Long Term: Longer than 10 Years |
|---|---|---|---|
| Number of cases | 973 | 1350 | 154 |
| Average follow-up (Y) | 0.8 Y | 4.7 Y | 12.9 Y |
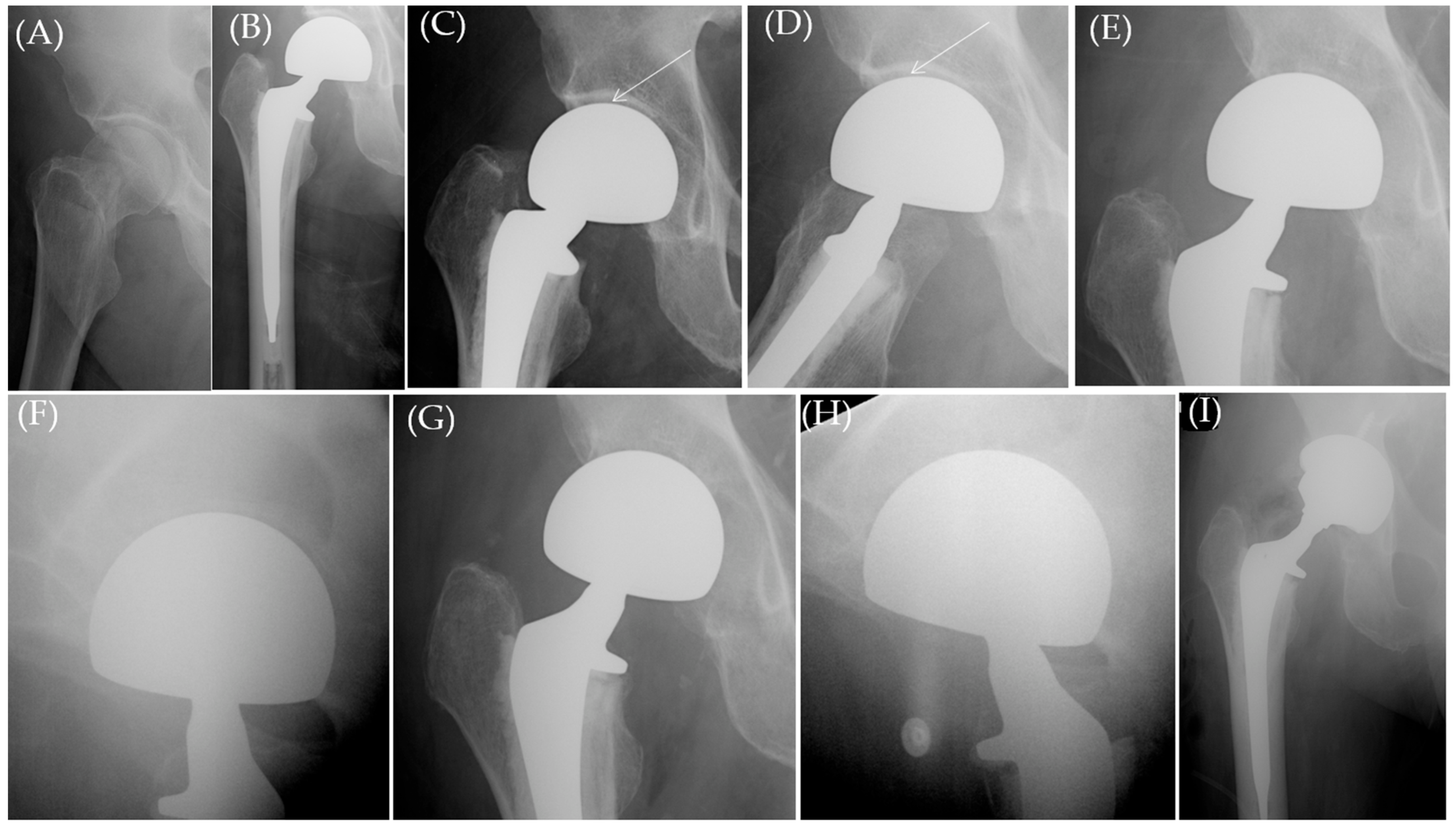
| Pt | Sex | Age (Y) | BMI | Implant Type | Symptomatic Acetabular Erosion per Implant Type & Statistical Comparison | Femoral Head Size | Stem Collared(C) /Uncollared (U) | Time Until Presentation (Pain) (M) | Medical Comorbidities | Management | Follow-Up (M) from the Index HA Surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 83.7 | 25 | UNI | 5/1109 (0.45%) | 46 | C | 11.54 | Conservative | 25.4 M | |
| 2 | F | 80.2 | 26 | UNI | 50 | C | 4.17 | Hypothyroid, Dementia, MS | THA | Died after 79.3 M | |
| 3 | F | 83.3 | 18.08 | UNI | 44 | C | 1.48 | Hypothyroid | Conservative | 69 | |
| 4 | F | 79.78 | 26 | UNI | 48 | U | 35.4 | Conservative | 47.5 | ||
| 5 | F | 66.89 | 26.54 | UNI | 48 | U | 2.76 | Conservative | 43.6 | ||
| 6 | F | 64.7 | 19.54 | BIP | 7/1368 (0.5%) Chi-square test: p = 0.8 (not statistically significant) | 48 | C | 4.3 | Osteoporosis | THA | 146.25 |
| 7 | F | 61.78 | 24.11 | BIP | 53 | C | 146.48 | Osteoporosis, Hypothyroid | Conservative | Died after 150 M | |
| 8 | F | 66.19 | 23.81 | BIP | 44 | C | 18.19 | Heavy Smoking, COPD | THA | Died after 31.9 M | |
| 9 | M | 47.1 | 22.46 | BIP | 40 | C | 61.6 | Spastic CP | Conservative | 177 M | |
| 10 | M | 76.58 | 27 | BIP | 54 | C | 2.5 | COPD, Epilepsy | THA | Died after 143.88 M | |
| 11 | M | 66.4 | 28 | BIP | 50 | C | 15.36 | THA | 215 M | ||
| 12 | M | 91.99 | 26.71 | BIP | 54 | C | 3.22 | Conservative | Died after 6 M |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahmoud, A.N.; Suk, M.; Horwitz, D.S. Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases. J. Clin. Med. 2024, 13, 6756. https://doi.org/10.3390/jcm13226756
Mahmoud AN, Suk M, Horwitz DS. Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases. Journal of Clinical Medicine. 2024; 13(22):6756. https://doi.org/10.3390/jcm13226756
Chicago/Turabian StyleMahmoud, Ahmed Nageeb, Michael Suk, and Daniel S. Horwitz. 2024. "Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases" Journal of Clinical Medicine 13, no. 22: 6756. https://doi.org/10.3390/jcm13226756
APA StyleMahmoud, A. N., Suk, M., & Horwitz, D. S. (2024). Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases. Journal of Clinical Medicine, 13(22), 6756. https://doi.org/10.3390/jcm13226756







