Feasibility of Home-Based Early Infant Hybrid Therapy in Children with Unilateral Cerebral Palsy
Abstract
1. Introduction
2. Materials and Methods
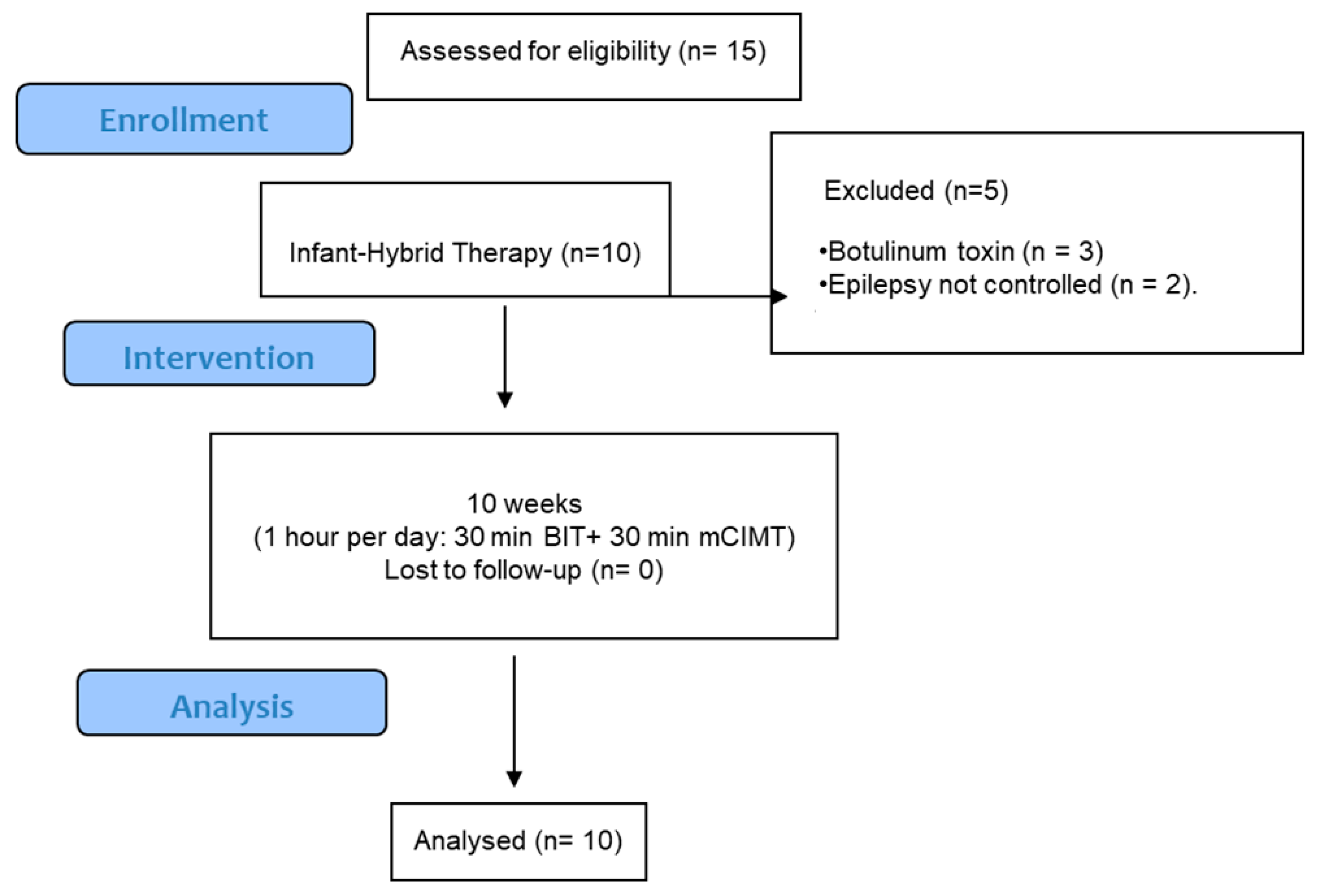
2.1. Study Design
2.2. Participants
2.3. Early Infant Hybrid Therapy (eI-Hybrid)
2.4. Family Training
2.5. Supervision of Families
2.6. Outcome Measures
2.6.1. Feasibility
- Acceptability: we evaluated the comprehensibility of the rules of the game regarding preparation and execution. This was measured using video analysis during the planning of the games, focusing on how to position the child on the table and their orientation to facilitate task execution.
- Training compliance: The compliance with the intervention duration (10 weeks) was documented through weekly reviews. These included oral reports from parents regarding their adherence to the therapy schedule and confirmation of completed sessions.
- Training smoothness: We examined the smoothness of activities by recording the number of problems and difficulties encountered. These data were be gathered through weekly documents that assessed task execution times and noted instances of rejection or interest in activities.
- Training motivation: The motivation and perceived effort of the child was evaluated through direct observation during therapy sessions. Observers recorded behavioral indicators of engagement, and parents completed a questionnaire about their expectations prior to therapy and after the 50 h of intervention. This questionnaire contains five questions, each with five possible answers (see Supplementary Materials).
2.6.2. Procedure Outcomes
Mini Assisting Hand Assessment (mini-AHA) Outcome
Goal Attainment Scale (GAS)
- Initial assessment: The therapeutic team conducted an initial assessment to understand the child’s current abilities and difficulties. This included gathering information from standardized assessments, clinical observations, and input from family members.
- Family engagement: Families would actively participate in discussions about their child’s needs, preferences and aspirations. Through structured interviews or focus groups, family members expressed their priorities for therapy, focusing on functional activities that would enhance their child’s daily life.
- Goal identification: Based on the information gathered, the therapy team and families would collaboratively identify specific, measurable, attainable, relevant, and time-bound (SMART) goals. Each goal was be tailored to the child’s individual circumstances and focused on improving functional independence in areas such as self-care, communication, and mobility.
- Review and refinement: The identified goals were reviewed to ensure that they were realistic and fitted the child’s developmental stage. The therapy team provided feedback and guidance to help families refine their goals as needed.
- Documentation: Each goal was documented, clearly stating the desired outcomes and how they would be measured. This documentation serves as a reference throughout the intervention to track progress and make adjustments as needed, as well as to propose new goals once achieved.
Satisfaction and Expectations from Parents
2.7. Statistical Analysis
3. Results
3.1. Feasibility Outcomes
- Acceptability: families reported adequate preparation and execution of activities, with no complications encountered.
- Training compliance: all children successfully completed the therapy within the designated 10-week period.
- Training smoothness: families demonstrated a clear understanding of how to implement activities with their infants. Initial suggestions were provided to enhance both children’s and parents’ positioning at the beginning of treatment, leading to smooth execution without complications.
- Training expectations and functional goals: Parents’ expectations (Table 3), captured through questionnaires, evolved over time. Initially, many felt unprepared to carry out the therapy; however, as they gained self-confidence through initial training and ongoing weekly reviews with physiotherapists, their involvement in the intervention improved significantly.
3.2. Mini Assisting Hand Assessment (Mini-AHA) Outcomes
3.3. Goal Attainment Scale (GAS)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A. Prevalence and characteristics of children with cerebral palsy in Europe. Dev. Med. Child Neurol. 2002, 44, 633–640. [Google Scholar] [CrossRef]
- Hoare, B.; Imms, C.; Randall, M.; Carey, L. Linking cerebral palsy upper limb measures to the International Classification of Functioning, Disability and Health. J. Rehabil. Med. 2011, 43, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.A.; Sullivan, E.; Engelstad, A. Annual Research Review: Early intervention viewed through the lens of developmental neuroscience. J. Child Psychol. Psychiatry 2024, 65, 435–455. [Google Scholar] [CrossRef]
- Houwink, A.; Aarts, P.B.; Geurts, A.C.; Steenbergen, B. A neurocognitive perspective on developmental disregard in children with hemiplegic cerebral palsy. Res. Dev. Disabil. 2011, 32, 2157–2163. [Google Scholar] [CrossRef]
- Akhbari Ziegler, S.; Hadders-Algra, M. Coaching approaches in early intervention and paediatric rehabilitation. Dev. Med. Child Neurol. 2020, 62, 569–574. [Google Scholar] [CrossRef]
- Palomo-Carrión, R.; Romay-Barrero, H.; Pinero-Pinto, E.; Romero-Galisteo, R.P.; López-Muñoz, P.; Martínez-Galán, I. Early Inter-vention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study. Children 2021, 8, 750. [Google Scholar] [CrossRef]
- Festante, F.; Antonelli, C.; Mazzotti, S.; Guzzetta, A. Early Intervention in Cerebral Palsy: From Theory to Current Practice. In Family-Centered Care in Childhood Disability: Theory, Research, Practice; Springer International Publishing: Berlin/Heidelberg, Germany; Cham, Switzerland, 2023; pp. 149–192. [Google Scholar]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Baker, A.; Niles, N.; Kysh, L.M.; Sargent, B. Effect of Motor Intervention for Infants and Toddlers with Cerebral Palsy: A Systematic Review and Meta-analysis. Pediatr. Phys. Ther. 2022, 34, 297–307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Walker, C.; Shierk, A.; Roberts, H. Constraint induced movement therapy in infants and toddlers with hemiplegic cerebral palsy: A scoping review. Occup. Ther. Health Care 2021, 36, 29–45. [Google Scholar] [CrossRef]
- Jackman, M.; Sakzewski, L.; Morgan, C.; Boyd, R.N.; Brennan, S.E.; Langdon, K.; Toovey, R.A.M.; Greaves, S.; Thorley, M.; Novak, I. Interventions to improve physical function for children and young people with cerebral palsy: International clinical practice guideline. Dev. Med. Child Neurol. 2022, 64, 536–549. [Google Scholar] [CrossRef] [PubMed]
- Charles, J.; Gordon, A.M. Development of hand–arm bimanual intensive training (HABIT) for improving bimanual coordination in children with hemiplegic cerebral palsy. Dev. Med. Child Neurol. 2006, 48, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Araneda, R.; Ebner-Karestinos, D.; Paradis, J.; Klöcker, A.; Saussez, G.; Demas, J.; Bailly, R.; Bouvier, S.; de Tournai, A.C.; Herman, E.; et al. Changes Induced by Early Hand-Arm Bimanual Intensive Therapy Including Lower Extremities in Young Children with Unilateral Cerebral Palsy: A Randomized Clinical Trial. JAMA Pediatr. 2024, 178, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Aarts, P.B.; Jongerius, P.H.; Geerdink, Y.A.; van Limbeek, J.; Geurts, A.C. Modified Constraint-Induced Movement Therapy combined with Bimanual Training (mCIMT–BiT) in children with unilateral spastic cerebral palsy: How are improvements in arm-hand use established? Res. Dev. Disabil. 2011, 32, 271–279. [Google Scholar] [CrossRef]
- Palomo-Carrión, R.; Lirio-Romero, C.; Ferri-Morales, A.; Jovellar-Isiegas, P.; Cortés-Vega, M.-D.; Romay-Barrero, H. Combined intensive therapies at home in spastic unilateral cerebral palsy with high bimanual functional performance. What do they offer? A comparative randomised clinical trial. Ther. Adv. Chronic Dis. 2021, 12, 20406223211034996. [Google Scholar] [CrossRef]
- Bansal, A.; Diwan, S. Effect of Modified Constraint Induced Movement Therapy and Hand Arm Bimanual Intensive Training on Upper Extremity Skills and Functional Performance in Children with Spastic Hemiplegic Cerebral Palsy. Int. J. Health Sci. Res. 2021, 11, 32–43. [Google Scholar]
- Cohen-Holzer, M.; Katz-Leurer, M.; Meyer, S.; Green, D.; Parush, S. The Effect of Bimanual Training with or Without Constraint on Hand Functions in Children with Unilateral Cerebral Palsy: A Non-Randomized Clinical Trial. Phys. Occup. Ther. Pediatr. 2017, 37, 516–527. [Google Scholar] [CrossRef]
- Palomo-Carrión, R.; Romay-Barrero, H.; Lirio-Romero, C.; Arroyo-Fernádez, R.; M-Guijarro-Herraiz, M.; Ferri-Morales, A. Feasibility of family-directed home-based bimanual intensive therapy combined with modified constraint induced movement therapy (h-BITmCI) in very low and low bimanual functional level: A brief report. Dev. Neurorehabilit. 2022, 26, 63–70. [Google Scholar] [CrossRef]
- Afzal, M.T.; Amjad, I.; Ghous, M. Comparison of classic constraint-induced movement therapy and its modified form on upper extremity motor functions and psychosocial impact in hemiplegic cerebral pals. J. Pak. Med Assoc. 2022, 72, 1418–1421. [Google Scholar] [CrossRef]
- Nawge, S.; Karthikbabu, S. Does bimanual task training benefit manual ability and hand function of children with bilateral spastic cerebral palsy? J. Pediatr. Rehabil. Med. 2023, 16, 49–57. [Google Scholar] [CrossRef]
- Steinbusch, C.V.M.; Defesche, A.; van der Leij, B.; Rameckers, E.A.A.; Knijnenburg, A.C.S.; Vermeulen, J.R.J.; Janssen-Potten, Y.J.M. The Effect of Bimanual Intensive Functional Training on Somatosensory Hand Function in Children with Unilateral Spastic Cerebral Palsy: An Observational Study. J. Clin. Med. 2023, 12, 1595. [Google Scholar] [CrossRef] [PubMed]
- Dong, V.A.-Q.; Tung, I.H.-H.; Siu, H.W.-Y.; Fong, K.N.-K. Studies comparing the efficacy of constraint-induced movement therapy and bimanual training in children with unilateral cerebral palsy: A systematic review. Dev. Neurorehabilit. 2012, 16, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Brauers, L.; Geijen, M.M.; Speth, L.A.; Rameckers, E.A. Does intensive upper limb treatment modality Hybrid Constrained Induced Movement Therapy (H-CIMT) improve grip and pinch strength or fatigability of the affected hand? J. Pediatr. Rehabil. Med. 2017, 10, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Sudati, I.P.; Sakzewski, L.; da Silva, C.F.R.; Jackman, M.; Haddon, M.; Pool, D.; Patel, M.; Boyd, R.N.; de Campos, A.C. Efficacy and threshold dose of intensive training targeting mobility for children with cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2024, 66, 1542–1557. [Google Scholar] [CrossRef] [PubMed]
- Kiresuk, T.J.; Smith, A.; Cardillo, J.E. Goal Attainment Scaling: Applications, Theory, and Measurement. Lawrence Erlbaum Associ-Ates. 1994. Available online: https://www.routledge.com/Goal-Attainment-Scaling-Applications-Theory-and-Measurement/Kiresuk-Smith-Cardillo/p/book/9780898598896 (accessed on 28 April 2022).
- King, G.A.; McDougall, J.; Tucker, M.A.; Gritzan, J.; Malloy-Miller, T.; Alambets, P.; Cunning, D.; Thomas, K.; Gregory, K. An evaluation of functional, school-based therapy services for children with special needs. Phys. Occup. Therap. Pediatr. 2009, 19, 5–29. [Google Scholar] [CrossRef]
- Greaves, S.; Imms, C.; Dodd, K.; Krumlinde-Sundholm, L. Development of the Mini-Assisting Hand Assessment: Evidence for content and internal scale validity. Dev. Med. Child Neurol. 2013, 55, 1030–1037. Available online: https://pubmed.ncbi.nlm.nih.gov/23899017/ (accessed on 28 April 2022). [CrossRef]
- Holmefur, M.M.; Krumlinde-Sundholm, L. Psychometric properties of a revised version of the Assisting Hand Assessment (Kids-AHA 5.0). Dev. Med. Child Neurol. 2015, 58, 618–624. Available online: https://pubmed.ncbi.nlm.nih.gov/26507383/ (accessed on 28 April 2022). [CrossRef]
- Krumlinde-Sundholm, L.; Eliasson, A.-C. Development of the assisting hand assessment: A rasch-built measure intended for children with unilateral upper limb impairments. Scand. J. Occup. Ther. 2003, 10, 16–26. [Google Scholar] [CrossRef]
- Schnackers, M.; COAD Focus Group; Beckers, L.; Janssen-Potten, Y.; Aarts, P.; Rameckers, E.; van der Burg, J.; de Groot, I.; Smeets, R.; Geurts, S.; et al. Home-based bimanual training based on motor learning principles in children with unilateral cerebral palsy and their parents (the COAD-study): Rationale and protocols. BMC Pediatr. 2018, 18, 139. [Google Scholar] [CrossRef]
- Holmefur, M.; Aarts, P.; Hoare, B.; Krumlinde-Sundholm, L. Test-retest and alternate forms reliability of the assisting hand as-sessment. J. Rehabil. Med. 2009, 41, 886–891. Available online: https://pubmed.ncbi.nlm.nih.gov/19841839/ (accessed on 28 April 2022). [CrossRef]
- Krumlinde-Sundholm, L.; Holmefur, M.; Kottorp, A.; Eliasson, A. The Assisting Hand Assessment: Current evidence of validity, reliability, and responsiveness to change. Dev. Med. Child Neurol. 2007, 49, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Churilov, I.; Brock, K.; Churilov, J.M.; Sutton, E.; Murphy, D.; MacIsaac, R.J.; Ekinci, E.I. Goal attainment scaling outcomes in general inpatient rehabilitation: Association with functional independence and perceived goal importance and difficulty. J. Rehabil. Med. 2020, 52, jrm00054. [Google Scholar] [CrossRef] [PubMed]
- Harpster, K.; Sheehan, A.; Foster, E.A.; Leffler, E.; Schwab, S.M.; Angeli, J.M. The methodological application of goal attainment scaling in pediatric rehabilitation research: A systematic review. Disabil. Rehabil. 2019, 41, 2855–2864. [Google Scholar] [CrossRef] [PubMed]
- Ferre, C.L.; Brandão, M.; Surana, B.; Dew, A.P.; Moreau, N.G.; Gordon, A.M. Caregiver-directed home-based intensive bimanual training in young children with unilateral spastic cerebral palsy: A randomized trial. Dev. Med. Child Neurol. 2017, 59, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Ferre, C.L.; Brandão, M.B.; Hung, Y.-C.; Carmel, J.B.; Gordon, A.M. Feasibility of caregiver-directed home-based hand-arm bimanual intensive training: A brief report. Dev. Neurorehabilit. 2015, 18, 69–74. [Google Scholar] [CrossRef]
- Reiss, A.P.; Wolf, S.L.; Hammel, E.A.; McLeod, E.L.; Williams, E.A. Constraint-Induced Movement Therapy (CIMT): Current Perspectives and Future Directions. Stroke Res. Treat. 2012, 2012, 159391. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Svensson, K.; Eliasson, A.-C.; Sundelin, H.; Holmqvist, K.L. Parents in the Driver’s Seat—Experiences of Parent-Delivered Baby-mCIMT Coached Remotely. J. Clin. Med. 2024, 13, 4864. [Google Scholar] [CrossRef]
- Darrah, J.; Law, M.C.; Pollock, N.; Wilson, B.; Russell, D.J.; Walter, S.D.; Rosenbaum, P.; Galuppi, B. Context therapy: A new intervention approach for children with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 615–620. [Google Scholar] [CrossRef]
- Löwing, K.; Hamer, E.G.; Bexelius, A.; Carlberg, E.B. Exploring the relationship of family goals and scores on standardized measures in children with cerebral palsy, using the ICF-CY. Dev. Neurorehabilit. 2011, 14, 79–86. [Google Scholar] [CrossRef]
- Eliasson, A.-C.; Nordstrand, L.; Ek, L.; Lennartsson, F.; Sjöstrand, L.; Tedroff, K.; Krumlinde-Sundholm, L. The effectiveness of Baby-CIMT in infants younger than 12 months with clinical signs of unilateral-cerebral palsy; an explorative study with randomized design. Res. Dev. Disabil. 2018, 72, 191–201. [Google Scholar] [CrossRef]
- Nordstrand, L.; Holmefur, M.; Kits, A.; Eliasson, A.-C. Improvements in bimanual hand function after baby-CIMT in two-year old children with unilateral cerebral palsy: A retrospective study. Res. Dev. Disabil. 2015, 41–42, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, E.; Varzeshnejad, M.; Masoumpour, A.; Ahmadimehr, F. The impact of the family-centered empowerment model on the children’s quality of life with chemical burns and their parent’s perceived stress. Burns 2023, 49, 838–847. [Google Scholar] [CrossRef] [PubMed]
- Ghazavi, Z.; Minooei, M.S.; Abdeyazdan, Z.; Gheissari, A. Effect of family empowerment model on quality of life in children with chronic kidney diseases. Iran J. Nurs. Midwifery Res. 2014, 19, 371–375. [Google Scholar] [PubMed] [PubMed Central]
- Miller, V.; Sampson, M.A.; Howell, D.; Kitzman, P. Coaching to Support Children with Disabilities in Occupational Therapy: A Literature Review. Occup. Ther. Health Care 2024, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Chamudot, R.; Parush, S.; Rigbi, A.; Horovitz, R.; Gross-Tsur, V. Effectiveness of Modified Constraint-Induced Movement Therapy Compared with Bimanual Therapy Home Programs for Infants with Hemiplegia: A Randomized Controlled Trial. Am. J. Occup. Ther. 2018, 72, 7206205010p1–7206205010p9. [Google Scholar] [CrossRef]
- Hoare, B.; Imms, C.; Carey, L.; Wasiak, J. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: A Cochrane systematic review. Clin. Rehabil. 2007, 21, 675–685. [Google Scholar] [CrossRef]

| Movements | Unimanual Examples (Infant CIMT Part) Using More-Affected Upper Limb/Hand | Bimanual Examples (Infant BIT Part) Using Both Upper Limbs/Hands | Action Type |
|---|---|---|---|
| Shoulder flexion | Throw a ball, touch different objects located at different heights, touch balloons, reach different rattles, use toys that are offered at different distances. | Throw a big ball, touch different objects located at different heights, touch big balloons, put on necklaces, hats, reach different rattles, use toys that are offered at different distances. | Reaching actions |
| Elbow extension | Push a box with different weights, throw towers, put paint on paper at a distance so that it can stretch, throw a ball, reach different rattles, with toys that are offered at different distances. | Push a box with different weights, throw towers, throw a ball, reach different rattles, use toys that are offered at different distances. | Reaching actions |
| Forearm supination | Turn around a toy, put food in the mouth, give them objects in the palm of the hand, play the toy trumpet. | Move maracas or other toys between hands, manipulate an object, give them objects in the palm of both hands, put marbles in a bottle (held with the more-affected hand). | Manipulating actions and grasping actions |
| Wrist extension, finger extension, opening hand | Squeeze playdough, move sand, pick up sand and drop it, pick up a round rattle or ball, play the toy piano. | Squeeze playdough, move sand, pick up sand and drop it, pick up a round rattle or ball, play the toy piano, stretching plasticine, colliding two round toys, clapping while singing a song. | Reaching actions, manipuling actions, and grasping actions |
| Fine grasp | Move balls of different sizes, uncover objects by pulling the handle, pick up cereals, bits of biscuit. | Breaking pieces of paper, putting the marbles in the bottle with the more-affected hand, moving a small object from one hand to another hand. | Grasping actions |
| Early Infant Hybrid Therapy (N = 10) | ||
|---|---|---|
| Mean (SD) | IR | |
| Age | 12.8 (3.4) | 9.8–16.3 |
| Mini-AHA Basal situation | 41–9 (7.7) | 34.8–50.3 |
| N | % | |
| Sex | ||
| Female | 6 | 60 |
| Male | 4 | 40 |
| Affected upper limb | ||
| Left | 6 | 60 |
| Right | 4 | 40 |
| Unilateral Cerebral Palsy cause | ||
| Perinatal stroke | 10 | 100 |
| Postnatal stroke | 0 | 0 |
| Other | 0 | 0 |
| Birth (gestational age) | ||
| Extremely premature | 0 | 0 |
| Moderately premature | 3 | 30 |
| Not premature | 7 | 70 |
| Associated disorders | ||
| Epilepsy | 0 | 0 |
| Other disorders | 0 | 0 |
| No disorders | 10 | 100 |
| Outcomes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Qo1 | Qo2 | Qo3 | Qo4 | Qo5 | ||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Mean (SD) | 3.4 (0.5) | 1.6 (0.5) | 4 (0) | 2.0 (0) | 4.4 (0.5) | 1.4 (0.5) | 3.5 (0.5) | 1.1 (0.3) | 3.0 (0) | 1.0 (0) |
| p Value | 0.004 * | 0.002 * | 0.002 * | 0.004 * | 0.002 * | |||||
| Outcomes | |||
|---|---|---|---|
| Mini-AHA/AHA | |||
| Pre | Post | 6 mo | |
| Mean (SD) | 41.9 (7.7) | 50.9 (6.0) | 50.3 (5.6) |
| p Value | <0.001 * | ||
| Pre–Post | <0.001 * | ||
| Pre-6 mo | <0.001 * | ||
| Post-6 mo | 0.072 | ||
| Goal | +2 | +1 | 0 | −1 | −2 |
|---|---|---|---|---|---|
| Throwing a ball with both hands | Throws the ball with both hands | Shakes the ball with both hands | Raises the ball with both hands over the head | Touches the ball with both hands | Touches the ball with one hand |
| Playing with sand in the park using both hands | Picks up sand with both hands and moves it in the park | Drags sand with both hands in the park | Transfers sand from one hand to the other in the park | Touches the sand with both hands in the park | Touches the sand with one hand in the park |
| Building towers | Fits two Lego pieces together with both hands at home | Contacts the two Lego pieces with both hands at home | Puts the two Lego pieces together with both hands at home | Picks up a Lego piece with each hand at home | Picks up a Lego piece with one hand at home |
| Holding a glass with both hands | Brings the glass to the mouth with both hands | Lifts the glass with two hands | Drags the glass from the center of the table to the trunk with both hands | Touches the glass with both hands | Touches the glass with one hand |
| Goal | Importance | Difficulty | Baseline | Achieved | |
|---|---|---|---|---|---|
| Throwing a ball with both hands | 0 1 2 3 | 0 1 2 3 | −1: somewhat less than expected −2: much less than expected | Yes | Much better A little better As expected |
| No | Partially achieved Same as baseline | ||||
| Worse | |||||
| Playing with sand in the park using both hands | 0 1 2 3 | 0 1 2 3 | −1: somewhat less than expected −2: much less than expected | Yes | Much better A little better As expected |
| No | Partially achieved Same as baseline | ||||
| Worse | |||||
| Building towers | 0 1 2 3 | 0 1 2 3 | −1: somewhat less than expected −2: much less than expected | Yes | Much better A little better As expected |
| No | Partially achieved Same as baseline | ||||
| Worse | |||||
| Holding a glass with both hands | 0 1 2 3 | 0 1 2 3 | −1: somewhat less than expected −2: much less than expected | Yes | Much better A little better As expected |
| No | Partially achieved Same as baseline | ||||
| Worse | |||||
| Goal | Baseline GAS T-Score | Achieved GAS T-Score | Change in GAS T Score |
|---|---|---|---|
| Throwing a ball with both hands | 30 | 70 | 40 |
| Playing with sand in the park using both hands | 30 | 60 | 30 |
| Building towers | 30 | 60 | 30 |
| Holding a glass with both hands | 30 | 60 | 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palomo-Carrión, R.; Romay-Barrero, H.; Pinero-Pinto, E.; Romero-Galisteo, R.-P.; Coello-Villalón, M.; Ferri-Morales, A.; López-Muñoz, P.; Lirio-Romero, C. Feasibility of Home-Based Early Infant Hybrid Therapy in Children with Unilateral Cerebral Palsy. J. Clin. Med. 2024, 13, 6725. https://doi.org/10.3390/jcm13226725
Palomo-Carrión R, Romay-Barrero H, Pinero-Pinto E, Romero-Galisteo R-P, Coello-Villalón M, Ferri-Morales A, López-Muñoz P, Lirio-Romero C. Feasibility of Home-Based Early Infant Hybrid Therapy in Children with Unilateral Cerebral Palsy. Journal of Clinical Medicine. 2024; 13(22):6725. https://doi.org/10.3390/jcm13226725
Chicago/Turabian StylePalomo-Carrión, Rocío, Helena Romay-Barrero, Elena Pinero-Pinto, Rita-Pilar Romero-Galisteo, María Coello-Villalón, Asunción Ferri-Morales, Purificación López-Muñoz, and Cristina Lirio-Romero. 2024. "Feasibility of Home-Based Early Infant Hybrid Therapy in Children with Unilateral Cerebral Palsy" Journal of Clinical Medicine 13, no. 22: 6725. https://doi.org/10.3390/jcm13226725
APA StylePalomo-Carrión, R., Romay-Barrero, H., Pinero-Pinto, E., Romero-Galisteo, R.-P., Coello-Villalón, M., Ferri-Morales, A., López-Muñoz, P., & Lirio-Romero, C. (2024). Feasibility of Home-Based Early Infant Hybrid Therapy in Children with Unilateral Cerebral Palsy. Journal of Clinical Medicine, 13(22), 6725. https://doi.org/10.3390/jcm13226725









