Minimally Invasive Aortic Valve Replacement for High-Risk Populations: Transaxillary Access Enhances Survival in Patients with Obesity
Abstract
1. Introduction
2. Patients and Methods
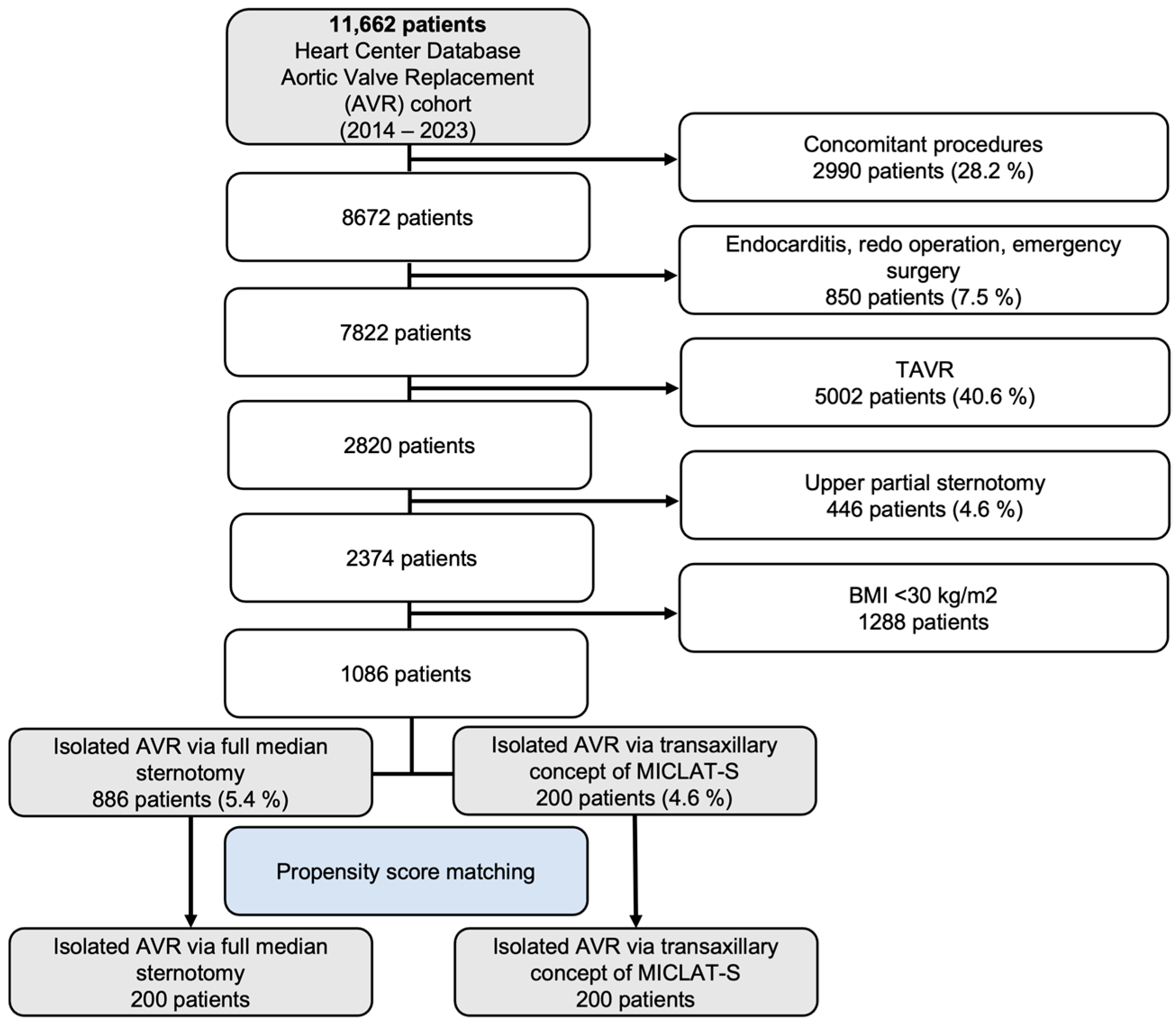
2.1. Inclusion and Exclusion Criteria
2.2. Study Design and Ethical Statement
2.3. Patient Population
2.4. Involved Surgeons
2.5. Sternum-Sparing Transaxillary Concept of MICLAT-S
2.6. Prosthesis Choice
2.7. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics
3.2. Unadjusted Outcomes
3.2.1. Procedural and Intraoperative Data
3.2.2. Postoperative Outcomes, Morbidity, and Mortality
3.3. Propensity Score-Matched Cohort
3.3.1. Adjusted Procedural and Intraoperative Data
3.3.2. Adjusted Postoperative Outcomes, Morbidity, and Mortality
4. Discussion
- -
- Combined MACCEs were less frequently observed in the MICLAT-S group;
- -
- The postoperative 30-day mortality rate was significantly lower in the MICLAT-S group;
- -
- The MICLAT-S group had a shorter median hospital stay;
- -
- The incidence of postoperative impaired wound healing was significantly lower in the MICLAT-S group;
- -
- The MICLAT-S group needed fewer transfusions of blood products.
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gammie, J.S.; Bartlett, S.T.; Griffith, B.P. Small-incision mitral valve repair: Safe, durable, and approaching perfection. Ann. Surg. 2009, 250, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.; Höfer, D.; Holfeld, J.; Hangler, H.; Bonaros, N.; Grimm, M. Indications and contra-indications for minimally invasive mitral valve surgery. J. Vis. Surg. 2018, 4, 255. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Obesity and Overweight. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 25 May 2024).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, W.T.; Hoffman, W.; Dewey, T.M.; Culica, D.; Prince, S.L.; Herbert, M.A.; Mack, M.J.; Ryan, W.H. Aortic valve replacement surgery: Comparison of outcomes in matched sternotomy and PORT ACCESS groups. Ann. Thorac. Surg. 2010, 90, 131–135. [Google Scholar] [CrossRef]
- McInerney, A.; Rodes-Cabau, J.; Veiga, G.; Lopez-Otero, D.; Munoz-Garcia, E.; Campelo-Parada, F.; Oteo, J.F.; Carnero, M.; Tafur Soto, J.D.; Amat-Santos, I.J.; et al. Transcatheter versus surgical aortic valve replacement in patients with morbid obesity: A multicentre propensity score-matched analysis. EuroIntervention 2022, 18, e417–e427. [Google Scholar] [CrossRef]
- McInerney, A.; Tirado-Conte, G.; Rodes-Cabau, J.; Campelo-Parada, F.; Tafur Soto, J.D.; Barbanti, M.; Munoz-Garcia, E.; Arif, M.; Lopez, D.; Toggweiler, S.; et al. Impact of morbid obesity and obesity phenotype on outcomes after transcatheter aortic valve replacement. J. Am. Heart Assoc. 2021, 10, e019051. [Google Scholar] [CrossRef]
- Yap, C.H.; Mohajeri, M.; Yii, M. Obesity and early complications after cardiac surgery. Med. J. Aust. 2007, 186, 350–354. [Google Scholar] [CrossRef]
- Ghanta, R.K.; LaPar, D.J.; Zhang, Q.; Devarkonda, V.; Isbell, J.M.; Yarboro, L.T.; Kern, J.A.; Kron, I.L.; Speir, A.M.; Fonner, C.E.; et al. Obesity increases risk-adjusted morbidity, mortality, and cost following cardiac surgery. J. Am. Heart Assoc. 2017, 6, e003831. [Google Scholar] [CrossRef]
- Allama, A.; Ibrahim, I.; Abdallah, A.; Ashraf, S.; Youhana, A.; Kumar, P.; Bhatti, F.; Zaidi, A. Effect of body mass index on early clinical outcomes after cardiac surgery. Asian Cardiovasc. Thorac. Ann. 2014, 22, 667–673. [Google Scholar] [CrossRef]
- Stamou, S.C.; Nussbaum, M.; Stiegel, R.M.; Reames, M.K.; Skipper, E.R.; Robicsek, F.; Lobdell, K.W. Effect of body mass index on outcomes after cardiac surgery: Is there an obesity paradox? Ann. Thorac. Surg. 2011, 91, 42–47. [Google Scholar] [CrossRef]
- Hartrumpf, M.; Kuehnel, R.U.; Albes, J.M. The obesity paradox is still there: A risk analysis of over 15 000 cardiosurgical patients based on body mass index. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 18–24. [Google Scholar] [CrossRef]
- Mariscalco, G.; Wozniak, M.J.; Dawson, A.G.; Serraino, G.F.; Porter, R.; Nath, M.; Klersy, C.; Kumar, T.; Murphy, G.J. Body mass index and mortality among adults undergoing cardiac surgery: A nationwide study with a systematic review and meta-analysis. Circulation 2017, 135, 850–863. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.A.; Reinders, I.; Garcia, M.E.; Eiriksdottir, G.; Launer, L.J.; Benediktsson, R.; Gudnason, V.; Jonsson, P.V.; Harris, T.B. Adipose tissue, muscle, and function: Potential mediators of associations between body weight and mortality in older adults with type 2 diabetes. Diabetes Care 2014, 37, 3213–3219. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Xu, J.; Zhen, S.; Zhu, Y. Obesity is associated with postoperative outcomes in patients undergoing cardiac surgery: A cohort study. BMC Anesthesiol. 2023, 23, 3. [Google Scholar] [CrossRef] [PubMed]
- De Santo, L.S.; Moscariello, C.; Zebele, C. Implications of obesity in cardiac surgery: Pattern of referral, physiopathology, complications, prognosis. J. Thorac. Dis. 2018, 10, 4532–4539. [Google Scholar] [CrossRef] [PubMed]
- Karra, R.; McDermott, L.; Connelly, S.; Smith, P.; Sexton, D.J.; Kaye, K.S. Risk factors for 1-year mortality after postoperative mediastinitis. J. Thorac. Cardiovasc. Surg. 2006, 132, 537–543. [Google Scholar] [CrossRef]
- Molina, J.E.; Lew, R.S.; Hyland, K.J. Postoperative sternal dehiscence in obese patients: Incidence and prevention. Ann. Thorac. Surg. 2004, 78, 912–917; discussion 912–917. [Google Scholar] [CrossRef]
- Vargo, P.R.; Steffen, R.J.; Bakaeen, F.G.; Navale, S.; Soltesz, E.G. The impact of obesity on cardiac surgery outcomes. J. Card. Surg. 2018, 33, 588–594. [Google Scholar] [CrossRef]
- Rahmanian, P.B.; Adams, D.H.; Castillo, J.G.; Chikwe, J.; Bodian, C.A.; Filsoufi, F. Impact of body mass index on early outcome and late survival in patients undergoing coronary artery bypass grafting or valve surgery or both. Am. J. Cardiol. 2007, 100, 1702–1708. [Google Scholar] [CrossRef]
- Murtuza, B.; Pepper, J.R.; Stanbridge, R.D.; Jones, C.; Rao, C.; Darzi, A.; Athanasiou, T. Minimal access aortic valve replacement: Is it worth it? Ann. Thorac. Surg. 2008, 85, 1121–1131. [Google Scholar] [CrossRef]
- Plass, A.; Scheffel, H.; Alkadhi, H.; Kaufmann, P.; Genoni, M.; Falk, V.; Grünenfelder, J. Aortic valve replacement through a minimally invasive approach: Preoperative planning, surgical technique, and outcome. Ann. Thorac. Surg. 2009, 88, 1851–1856. [Google Scholar] [CrossRef] [PubMed]
- Wilbring, M.; Arzt, S.; Alexiou, K.; Charitos, E.; Matschke, K.; Kappert, U. Clinical Safety and Efficacy of the Transaxillary Access Route for Minimally Invasive Aortic Valve Replacement. Thorac. Cardiovasc. Surg. 2023, 71, DGTHG-V47. [Google Scholar] [CrossRef]
- Wilbring, M.; Arzt, S.; Alexiou, K.; Matschke, K.; Kappert, U. Surgery without visible scars-double valve surgery using the right lateral access. Ann. Cardiothorac. Surg. 2020, 9, 424–426. [Google Scholar] [CrossRef]
- Wilbring, M.; Matschke, K.E.; Alexiou, K.; Di Eusanio, M.; Kappert, U. Surgery without scars: Right lateral access for minimally invasive aortic valve replacement. Thorac. Cardiovasc. Surg. 2021, 69, 461–465. [Google Scholar] [CrossRef]
- Coti, I.; Haberl, T.; Scherzer, S.; Werner, P.; Shabanian, S.; Kocher, A.; Laufer, G.; Andreas, M. Outcome of rapid deployment aortic valves: Long-term experience after 700 implants. Ann. Cardiothorac. Surg. 2020, 9, 314–321. [Google Scholar] [CrossRef]
- Williams, M.L.; Flynn, C.D.; Mamo, A.A.; Tian, D.H.; Kappert, U.; Wilbring, M.; Folliguet, T.; Fiore, A.; Miceli, A.; D’Onofrio, A.; et al. Long-term outcomes of sutureless and rapid-deployment aortic valve replacement: A systematic review and meta-analysis. Ann. Cardiothorac. Surg. 2020, 9, 265–279. [Google Scholar] [CrossRef]
- Pollari, F.; Mamdooh, H.; Hitzl, W.; Grossmann, I.; Vogt, F.; Fischlein, T. Ten years’ experience with the sutureless aortic valve replacement: Incidence and predictors for survival and valve durability at follow-up. Eur. J. Cardiothorac. Surg. 2023, 63, ezac572. [Google Scholar] [CrossRef]
- Rao, P.N.; Kumar, A.S. Aortic valve replacement through right thoracotomy. Tex. Heart Inst. J. 1993, 20, 307–308. [Google Scholar]
- Cosgrove, D.M., 3rd; Sabik, J.F. Minimally invasive approach for aortic valve operations. Ann. Thorac. Surg. 1996, 62, 596–597. [Google Scholar] [CrossRef]
- Svensson, L.G.; D’Agostino, R.S. “J” incision minimal-access valve operations. Ann. Thorac. Surg. 1998, 66, 1110–1112. [Google Scholar] [CrossRef]
- Lamelas, J. Minimally invasive aortic valve replacement: The “Miami Method”. Ann. Cardiothorac. Surg. 2015, 4, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Van Praet, K.M.; Van Kampen, A.; Kofler, M.; Unbehaun, A.; Hommel, M.; Jacobs, S.; Falk, V.; Kempfert, J. Minimally invasive surgical aortic valve replacement through a right anterolateral thoracotomy. Multimed. Man. Cardiothorac. Surg. 2020, 2020. [Google Scholar] [CrossRef]
- Beckmann, A.; Meyer, R.; Eberhardt, J.; Gummert, J.; Falk, V. German heart surgery report 2023: The annual updated registry of the german society for thoracic and cardiovascular surgery. Thorac. Cardiovasc. Surg. 2024, 72, 329–345. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Xie, A.; Di Eusanio, M.; Yan, T.D. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann. Thorac. Surg. 2014, 98, 1499–1511. [Google Scholar] [CrossRef]
- Doenst, T.; Lamelas, J. Do we have enough evidence for minimally-invasive cardiac surgery? A critical review of scientific and non-scientific information. J. Cardiovasc. Surg. 2017, 58, 613–623. [Google Scholar] [CrossRef]
- Brown, M.L.; McKellar, S.H.; Sundt, T.M.; Schaff, H.V. Ministernotomy versus conventional sternotomy for aortic valve replacement: A systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 2009, 137, 670–679.e5. [Google Scholar] [CrossRef]
- Scarci, M.; Young, C.; Fallouh, H. Is ministernotomy superior to conventional approach for aortic valve replacement? Interact. Cardiovasc. Thorac. Surg. 2009, 9, 314–317. [Google Scholar] [CrossRef]
- Modi, P.; Hassan, A.; Chitwood, W.R., Jr. Minimally invasive mitral valve surgery: A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2008, 34, 943–952. [Google Scholar] [CrossRef]
- Santana, O.; Reyna, J.; Grana, R.; Buendia, M.; Lamas, G.A.; Lamelas, J. Outcomes of minimally invasive valve surgery versus standard sternotomy in obese patients undergoing isolated valve surgery. Ann. Thorac. Surg. 2011, 91, 406–410. [Google Scholar] [CrossRef]
- Abud, B.; Saydam, O.; Engin, A.Y.; Karaarslan, K.; Kunt, A.G.; Karacelik, M. Outcomes of aortic valve replacement via right anterior minithoracotomy and central cannulation versus conventional aortic valve replacement in obese patients. Braz. J. Cardiovasc. Surg. 2022, 37, 875–882. [Google Scholar] [CrossRef]
- Xie, X.B.; Dai, X.F.; Qiu, Z.H.; Jiang, D.B.; Wu, Q.S.; Dong, Y.; Chen, L.W. Do obese patients benefit from isolated aortic valve replacement through a partial upper sternotomy? J. Cardiothorac. Surg. 2022, 17, 179. [Google Scholar] [CrossRef] [PubMed]
- Cammertoni, F.; Bruno, P.; Pavone, N.; Nesta, M.; Chiariello, G.A.; Grandinetti, M.; D’Avino, S.; Sanesi, V.; D’Errico, D.; Massetti, M. Outcomes of minimally invasive aortic valve replacement in obese patients: A propensity-matched study. Braz. J. Cardiovasc. Surg. 2024, 39, e20230159. [Google Scholar] [CrossRef] [PubMed]
- Pisano, C.; Totaro, P.; Triolo, O.F.; Argano, V. Advantages of minimal access versus conventional aortic valve replacement in elderly or severely obese patients. Innovations 2017, 12, 102–108. [Google Scholar] [CrossRef]
- Welp, H.A.; Herlemann, I.; Martens, S.; Deschka, H. Outcomes of aortic valve replacement via partial upper sternotomy versus conventional aortic valve replacement in obese patients. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 481–486. [Google Scholar] [CrossRef]
- Girgis, S.W.G.; Leon, K.N.; Nekhila, W.S.B. Mini-sternotomy aortic valve replacement in morbid obesity: Can the little offer the greater? Egypt. J. Hosp. Med. 2022, 89, 7745–7748. [Google Scholar] [CrossRef]
- Furukawa, N.; Kuss, O.; Aboud, A.; Schonbrodt, M.; Renner, A.; Hakim Meibodi, K.; Becker, T.; Zittermann, A.; Gummert, J.F.; Borgermann, J. Ministernotomy versus conventional sternotomy for aortic valve replacement: Matched propensity score analysis of 808 patients. Eur. J. Cardiothorac. Surg. 2014, 46, 221–226; discussion 226–227. [Google Scholar] [CrossRef]
- Acharya, M.; Harling, L.; Moscarelli, M.; Ashrafian, H.; Athanasiou, T.; Casula, R. Influence of body mass index on outcomes after minimal-access aortic valve replacement through a J-shaped partial upper sternotomy. J. Cardiothorac. Surg. 2016, 11, 74. [Google Scholar] [CrossRef][Green Version]
- Lim, J.Y.; Deo, S.V.; Altarabsheh, S.E.; Jung, S.H.; Erwin, P.J.; Markowitz, A.H.; Park, S.J. Conventional versus minimally invasive aortic valve replacement: Pooled analysis of propensity-matched data. J. Card. Surg. 2015, 30, 125–134. [Google Scholar] [CrossRef]
- Abdelaal, S.A.; Abdelrahim, N.A.; Mamdouh, M.; Ahmed, N.; Ahmed, T.R.; Hefnawy, M.T.; Alaqori, L.K.; Abozaid, M. Comparative effects of minimally invasive approaches vs. conventional for obese patients undergoing aortic valve replacement: A systematic review and network meta-analysis. BMC Cardiovasc. Disord. 2023, 23, 392. [Google Scholar] [CrossRef]
- Wilbring, M.; Alexiou, K.; Schmidt, T.; Petrov, A.; Taghizadeh-Waghefi, A.; Charitos, E.; Matschke, K.; Arzt, S.; Kappert, U. Safety and Efficacy of the Transaxillary Access for Minimally Invasive Aortic Valve Surgery. Medicina 2023, 59, 160. [Google Scholar] [CrossRef]
- Murphy, G.J.; Reeves, B.C.; Rogers, C.A.; Rizvi, S.I.; Culliford, L.; Angelini, G.D. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007, 116, 2544–2552. [Google Scholar] [CrossRef]
- Rahmanian, P.B.; Kaya, S.; Eghbalzadeh, K.; Menghesha, H.; Madershahian, N.; Wahlers, T. Rapid deployment aortic valve replacement: Excellent results and increased effective orifice areas. Ann. Thorac. Surg. 2018, 105, 24–30. [Google Scholar] [CrossRef]






| Pre-Matched Cohort | Propensity Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Sternotomy (n = 886) | MICLAT-S (n = 200) | p | Sternotomy (n = 200) | MICLAT-S (n = 200) | p | |
| Age (year), mean ± SD | 69.0 ± 8.65 | 67.6 ± 8.27 | 0.034 * | 68.4 ± 8.25 | 67.6 ± 8.27 | 0.327 |
| BMI (kg/m2), mean ± SD | 33.8 ± 3.43 | 34.1 ± 3.76 | 0.205 | 34.6 ± 4.21 | 34.1 ± 3.76 | 0.227 |
| Diabetes mellitus, n (%) | 379 (42.8) | 69 (35.5) | 0.038 * | 75 (37.5) | 69 (34.5) | 0.603 |
| Previous MI, n (%) | 24 (2.7) | 6 (3.0) | 1 | 8 (4.0) | 6 (3.0) | 0.787 |
| LVEF > 50%, n (%) | 671 (75.7) | 155 (77.5) | 0.156 | 159 (79.5) | 155 (77.5) | 0.948 |
| Atrial fibrillation, n (%) | 107 (12.1) | 37 (18.5) | 0.021 * | 48 (24.0) | 37 (18.5) | 0.221 |
| COPD, n (%) | 75 (8.5) | 24 (12.0) | 0.152 | 31 (15.5) | 24 (12.0) | 0.384 |
| Renal insufficiency, n (%) | 243 (27.4) | 48 (24.0) | 0.368 | 53 (26.5) | 48 (24.0) | 0.645 |
| Hemodialysis, n (%) | 7 (0.8) | 4 (2.0) | 0.249 | 4 (2.0) | 4 (2.0) | 1 |
| PAOD, n (%) | 126 (14.2) | 13 (6.5) | 0.004 ** | 17 (8.5) | 13 (6.5) | 0.570 |
| TIA, n (%) | 0 (0) | 4 (2.0) | <0.001 ** | 0 (0) | 4 (2.0) | 0.123 |
| EuroSCORE II (%), mean ± SD | 1.68 ± 1.24 | 1.83 ± 1.21 | 0.286 | 1.83 ± 1.81 | 1.83 ± 1.21 | 0.989 |
| Pre-Matched Cohort | Propensity Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Sternotomy (n = 886) | MICLAT-S (n = 200) | p | Sternotomy (n = 200) | MICLAT-S (n = 200) | p | |
| Prosthesis size (mm), mean ± SD | 23.2 ± 1.8 | 24.2 ± 2.1 | ≤0.001 ** | 23.7 ± 1.9 | 24.1 ± 2.0 | 0.041 * |
| STST (min), mean ± SD | 120.1 ± 33.6 | 135.0 ± 37.7 | ≤0.001 ** | 119.0 ± 33.8 | 135.0 ± 37.7 | ≤0.001 ** |
| CPBT (min), mean ± SD | 59.2 ± 23.5 | 69.1 ± 19.1 | ≤0.001 ** | 56.1 ± 21.4 | 69.1 ± 19.1 | ≤0.001 ** |
| ACCT (min), mean ± SD | 41.9 ± 15.2 | 44.0 ± 13.4 | 0.044 * | 41.9 ± 13.3 | 44.0 ± 13.4 | 0.044 * |
| Prosthesis type | ||||||
| 136 (15.3) | 10 (5.0) | 29 (14.5) | 10 (5.0) | ||
| 750 (84.7) | 21 (10.5) | ≤0.001 ** | 171 (85.5) | 21 (10.5) | ≤0.001 ** |
| 0 (0.0) | 169 (84.5) | 0 (0.0) | 169 (84.5) | ||
| Pre-Matched Cohort | Propensity Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Sternotomy (n = 886) | MICLAT-S (n = 200) | p | Sternotomy (n = 200) | MICLAT-S (n = 200) | p | |
Ventilation time (h)
| 232 (26.2) 525 (59.3) 57 (6.4) | 181 (90.5) 13 (6.5) 6 (3.0) | ≤0.001 ** | 47 (23.5) 139 (69.5) 14 (7.0) | 181 (90.5) 13 (6.5) 6 (3.0) | ≤0.001 ** |
| Respiratory failure †, n (%) | 40 (4.5) | 6 (3.0) | 0.442 | 11 (5.5) | 6 (3.0) | 0.322 |
ICU stay (days), mean ± SD
| 511 (57.7) 133 (15.0) 89 (10.0) 152 (17.2) | 141 (70.5) 17 (8.5) 21 (10.5) 21 (10.5) | 0.006 ** | 120 (60.0) 27 (13.5) 19 (9.5) 34 (17.0) | 141 (70.5) 17 (8.5) 21 (10.5) 21 (10.5) | 0.068 |
| Hospital stay (days), mean ± SD | 12.6 ± 8.60 | 9.71 ± 6.19 | ≤0.001 ** | 12.4 ± 7.13 | 9.71 ± 6.19 | ≤0.001 ** |
| Transfusion of PRBCs, mean ± SD | 4.02 ± 7.37 | 0.540 ± 1.67 | ≤0.001 ** | 5.17 ± 9.38 | 0.540 ± 1.67 | ≤0.001 ** |
| AKI stage III or CVVH, n (%) | 44 (5.0) | 4 (2.0) | 0.097 | 18 (9.0) | 4 (2.0) | 0.022 * |
| Conversion to sternotomy, n (%) | N/A | 7 (1.6) | N/A | N/A | 7 (1.6) | N/A |
| Re-exploration, n (%) | 28 (3.2) | 13 (6.5) | 0.043 * | 5 (2.5) | 13 (6.5) | 0.0888 |
| Impaired wound healing, n (%) | 53 (6.0) | 10 (5.0) | 0.707 | 24 (12.0) | 10 (5.0) | 0.012 ** |
| Postoperative delirium, n (%) | 157 (17.7) | 40 (20.0) | 0.517 | 26 (13.0) | 40 (20.0) | 0.0794 |
| Ischemic stroke (Rankin ≥ 2), n (%) | 12 (1.4) | 1 (0.5) | 0.490 | 2 (1.0) | 1 (0.5) | 0.745 |
| TIA, n (%) | 9 (1.0) | 1 (0.5) | 0.745 | 2 (1.0) | 1 (0.5) | 0.618 |
| PPM implantation, n (%) | 4 (0.5) | 11 (5.5) | 0.446 | 1 (0.5) | 11 (5.5) | 1 |
| Myocardial infarction, n (%) | 4 (0.5) | 0 (0.0) | 0.758 | 1 (0.5) | 0 (0) | 1 |
| 30-day mortality, n (%) | 30 (3.4) | 3 (1.5) | 0.240 | 12 (6.0) | 3 (1.5) | 0.031 * |
| MACCE, n (%) | 45 (5.1) | 4 (2.0) | 0.028 * | 15 (7.5) | 4 (2.0) | 0.003 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taghizadeh-Waghefi, A.; Petrov, A.; Arzt, S.; Alexiou, K.; Matschke, K.; Kappert, U.; Wilbring, M. Minimally Invasive Aortic Valve Replacement for High-Risk Populations: Transaxillary Access Enhances Survival in Patients with Obesity. J. Clin. Med. 2024, 13, 6529. https://doi.org/10.3390/jcm13216529
Taghizadeh-Waghefi A, Petrov A, Arzt S, Alexiou K, Matschke K, Kappert U, Wilbring M. Minimally Invasive Aortic Valve Replacement for High-Risk Populations: Transaxillary Access Enhances Survival in Patients with Obesity. Journal of Clinical Medicine. 2024; 13(21):6529. https://doi.org/10.3390/jcm13216529
Chicago/Turabian StyleTaghizadeh-Waghefi, Ali, Asen Petrov, Sebastian Arzt, Konstantin Alexiou, Klaus Matschke, Utz Kappert, and Manuel Wilbring. 2024. "Minimally Invasive Aortic Valve Replacement for High-Risk Populations: Transaxillary Access Enhances Survival in Patients with Obesity" Journal of Clinical Medicine 13, no. 21: 6529. https://doi.org/10.3390/jcm13216529
APA StyleTaghizadeh-Waghefi, A., Petrov, A., Arzt, S., Alexiou, K., Matschke, K., Kappert, U., & Wilbring, M. (2024). Minimally Invasive Aortic Valve Replacement for High-Risk Populations: Transaxillary Access Enhances Survival in Patients with Obesity. Journal of Clinical Medicine, 13(21), 6529. https://doi.org/10.3390/jcm13216529






