Comparison of Short-Term Outcomes of DSA and ALMIS Approach for Bipolar Cemented Hemiarthroplasty in Patients with Neck of Femur Fracture
Abstract
1. Introduction
2. Materials and Methods
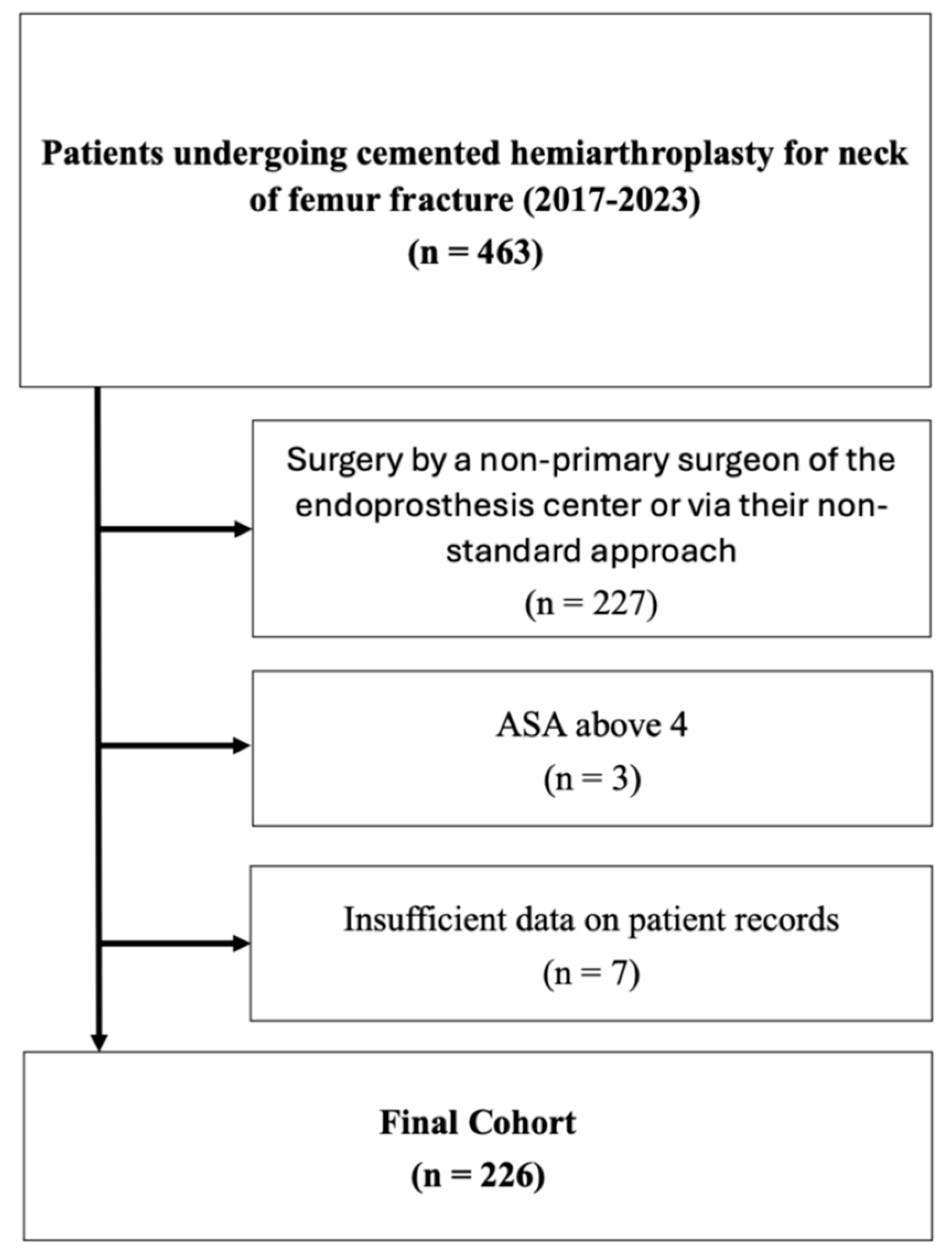
2.1. Study Population
2.2. Inclusion Criteria
- Neck of femur (NOF) fracture treated with cemented hemiarthroplasty (HA) between 2017 and 2023;
- Surgery performed by a Consultant Orthopaedic Surgeon certified as the main surgeon of the certified endoprosthesis center, using the surgeon’s standard approach (either DSA or ALMIS).
2.3. Exclusion Criteria
- American Society of Anesthesiologists (ASA) classification score greater than 4;
- Insufficient data in patient records.
2.4. Data Collection and Statistical Analysis
3. Results
3.1. Study Population
3.2. Results
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elliott, J.; Beringer, T.; Kee, F.; Marsh, D.; Willis, C.; Stevenson, M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J. Clin. Epidemiol. 2003, 56, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Aprato, A.; Bechis, M.; Buzzone, M.; Bistolfi, A.; Daghino, W.; Massè, A. No rest for elderly femur fracture patients: Early surgery and early ambulation decrease mortality. J. Orthop. Traumatol. 2020, 21, 12. [Google Scholar] [CrossRef] [PubMed]
- Ramadanov, N.; Bueschges, S.; Liu, K.; Lazaru, P.; Marintschev, I. Direct anterior approach vs. SuperPATH vs. conventional approaches in total hip replacement: A network meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2021, 107, 103058. [Google Scholar] [CrossRef] [PubMed]
- Angerame, M.R.; Dennis, D.A. Surgical approaches for total hip arthroplasty. Ann. Jt. 2018, 3, 368–376. [Google Scholar] [CrossRef]
- Shigemura, T.; Murata, Y.; Yamamoto, Y.; Shiratani, Y.; Hamano, H.; Wada, Y. Minimally invasive anterolateral approach versus lateral transmuscular approach for total hip arthroplasty: A systematic review and meta-analysis. Surgeon 2022, 20, e254–e261. [Google Scholar] [CrossRef]
- de Jong, L.; Klem, T.M.A.L.; Kuijper, T.M.; Roukema, G.R. The minimally invasive anterolateral approach versus the traditional anterolateral approach (Watson-Jones) for hip hemiarthroplasty after a femoral neck fracture: An analysis of clinical outcomes. Int. Orthop. 2018, 42, 1943–1948. [Google Scholar] [CrossRef]
- Tsailas, P.G.; Argyrou, C.; Valavanis, A. Management of femoral neck fractures with the ALMIS approach in elderly patients: Outcomes compared to posterior approach. Injury 2021, 52, 3666–3672. [Google Scholar] [CrossRef]
- Ulivi, M.; Orlandini, L.; Vitale, J.A.; Meroni, V.; Prandoni, L.; Mangiavini, L.; Rossi, N.; Peretti, G.M. Direct superior approach versus posterolateral approach in total hip arthroplasty: A randomized controlled trial on early outcomes on gait, risk of fall, clinical and self-reported measurements. Acta Orthop. 2021, 92, 274–279. [Google Scholar] [CrossRef]
- Duijnisveld, B.J.; van den Hout, J.; Wagenmakers, R.; Koenraadt, K.L.M.; Bolder, S.B.T. No Learning Curve of the Direct Superior Approach in Total Hip Arthroplasty. Orthop. Surg. 2020, 12, 852–860. [Google Scholar] [CrossRef]
- Leonard, H.J.; Ohly, N.E. Direct superior approach for total hip arthroplasty. Bone Jt. J. 2021, 103-B, 500–506. [Google Scholar] [CrossRef]
- Nam, D.; Meyer, Z.; Rames, R.D.; Nunley, R.M.; Barrack, R.L.; Roger, D.J. Is the Direct Superior, Iliotibial Band-Sparing Approach Associated With Decreased Pain After Total Hip Arthroplasty? J Arthroplast. 2017, 32, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Faggiani, M.; Risitano, S.; Rissolio, L.; Baroni, C.; Alberghina, F.; Conforti, L. Comparison of Anterior and Lateral Approach in Hip Hemiarthroplasty for Femur Neck Fractures in the Elderly: Clinical and Radiographic Outcomes. Malays. Orthop. J. 2022, 16, 113–119. [Google Scholar] [CrossRef] [PubMed]
- de Vries, E.N.; Gardenbroek, T.J.; Ammerlaan, H.; Steenstra, F.; Vervest, A.M.J.S.; Hogervorst, M.; van Velde, R. The optimal approach in hip hemiarthroplasty: A cohort of 1009 patients. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Bűcs, G.; Dandé, Á.; Patczai, B.; Sebestyén, A.; Almási, R.; Nöt, L.G.; Wiegand, N. Bipolar hemiarthroplasty for the treatment of femoral neck fractures with minimally invasive anterior approach in elderly. Injury 2021, 52 (Suppl. 1), S37–S43. [Google Scholar] [CrossRef]
- Krassnig, R.; Prager, W.; Wildburger, R.; Hohenberger, G.M. Direct anterior versus antero-lateral approach in hip joint hemiarthroplasty. Arch. Orthop. Trauma. Surg. 2023, 143, 4141–4148. [Google Scholar] [CrossRef]
- Khan, I.A.; Magnuson, J.A.; Arshi, A.; Krueger, C.A.; Freedman, K.B.; Fillingham, Y.A. Direct Anterior Approach in Hip Hemiarthroplasty for Femoral Neck Fractures: Do Short-Term Outcomes Differ with Approach?: A Systematic Review and Meta-Analysis. JBJS Rev. 2022, 10, e21. [Google Scholar] [CrossRef]
- Spina, M.; Luppi, V.; Chiappi, J.; Bagnis, F.; Balsano, M. Direct anterior approach versus direct lateral approach in total hip arthroplasty and bipolar hemiarthroplasty for femoral neck fractures: A retrospective comparative study. Aging Clin. Exp. Res. 2021, 33, 1635–1644. [Google Scholar] [CrossRef]
- Barrack, R.L.; Mulroy, R.D.; Harris, W.H. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J. Bone Joint Surg. Br. 1992, 74, 385–389. [Google Scholar] [CrossRef]
- Garcia, F.L.; Sugo, A.T.; Picado, C.H. Radiographic grading of femoral stem cementation in hip arthroplasty. Acta Ortop. Bras. 2013, 21, 30–33. [Google Scholar] [CrossRef]
- Nadler, S.B.; Hidalgo, J.H.; Bloch, T. Prediction of blood volume in normal human adults. Surgery 1962, 51, 224–232. [Google Scholar]
- Good, L.; Peterson, E.; Lisander, B. Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br. J. Anaesth. 2003, 90, 596–599. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Song, J.W.; Soh, S.; Kwak, Y.L.; Shim, J.K. Perioperative management of patients receiving non-vitamin K antagonist oral anticoagulants: Up-to-date recommendations. Anesth. Pain. Med. 2020, 15, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Jobory, A.; Kärrholm, J.; Hansson, S.; Åkesson, K.; Rogmark, C. Dislocation of hemiarthroplasty after hip fracture is common and the risk is increased with posterior approach: Result from a national cohort of 25,678 individuals in the Swedish Hip Arthroplasty Register. Acta Orthop. 2021, 92, 413–418. [Google Scholar] [CrossRef]
- Charles, T.; Bloemers, N.; Kapanci, B.; Jayankura, M. Complication rates after direct anterior. World J. Orthop. 2024, 15, 22–29. [Google Scholar] [CrossRef]
| DSA | ALMIS | p | ||
|---|---|---|---|---|
| Age in Years | 84 (SD 8.0) | 83.3 (SD 7.2) | 0.438 | |
| Gender | male | 28 (45%) | 60 (37%) | 0.238 |
| female | 34 (55%) | 104 (63%) | ||
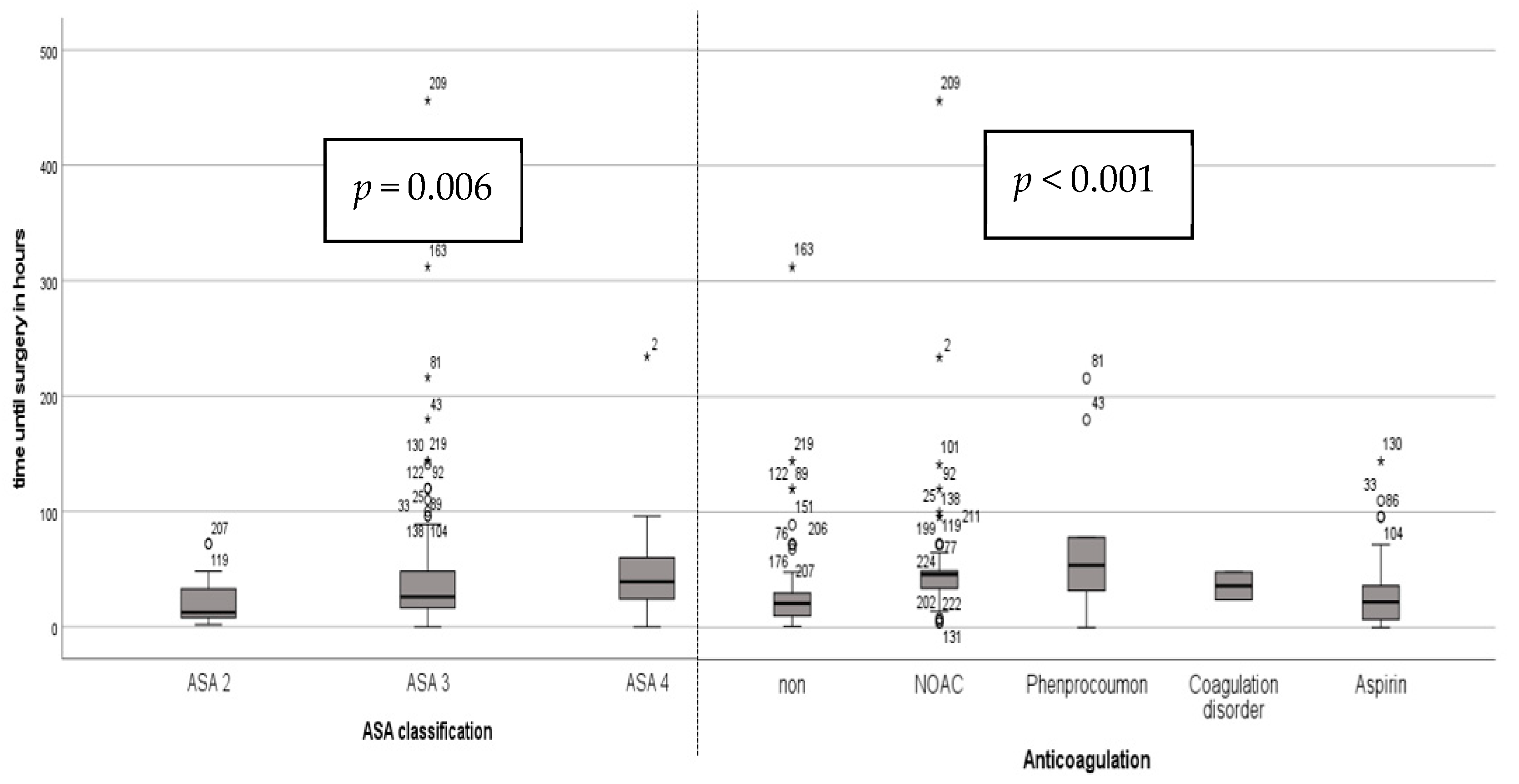
| ASA | 2 | 3 (5%) | 25 (15%) | 0.101 |
| 3 | 54 (87%) | 129 (79%) | ||
| 4 | 5 (8%) | 10 (6%) | ||
| BMI | mean in kg/m2 | 24.2 (SD 3.9) | 25.2 (SD 4.6) | 0.103 |
| Side | right | 25 (40%) | 82 (50%) | 0.194 |
| left | 37 (60%) | 82 (50%) | ||
| Implant | Mathys | 46 (74%) | 127 (77%) | 0.607 |
| Stryker | 16 (26%) | 37 (23%) | ||
| Anticoagulation | non | 31 (50%) | 74 (45%) | 0.767 |
| NOAC | 16 (26%) | 53 (32%) | ||
| Phenprocoumon | 3 (5%) | 8 (5%) | ||
| Disorder | 0 (0%) | 2 (1%) | ||
| Aspirin | 12 (19%) | 27 (17%) | ||
| Musculoskeletal disorders | No | 61 (98%) | 153 (93%) | 0.128 |
| Yes | 1 (2%) | 11 (7%) | ||
| Osteoporosis | No | 55 (89%) | 128 (78%) | 0.068 |
| Yes | 7 (11%) | 36 (22%) | ||
| Diabetes mellitus II | No | 49 (79%) | 114 (70%) | 0.325 |
| Yes | 13 (21%) | 49 (30%) | ||
| DSA | ALMIS | p | ||
|---|---|---|---|---|
| GT avulsion | No | 61 (100%) | 158 (97%) | 0.167 |
| Yes | 0 (0%) | 5 (3%) | ||
| Other periprosth. fracture | No | 61 (100%) | 163 (100%) | n/a |
| Yes | 0 (0%) | 0 (0%) | ||
| Shaft alignment | Varus | 9 (15%) | 17 (11%) | 0.636 |
| Parallel | 33 (54%) | 96 (59%) | ||
| Valgus | 19 (31%) | 49 (30%) | ||
| Quality of cementation | A | 27 (45%) | 94 (58%) | 0.250 |
| B | 17 (29%) | 43 (26%) | ||
| C | 8 (13%) | 12 (7%) | ||
| D | 8 (13%) | 14 (9%) | ||
| Revision due to wound healing or infection | No | 61 (100%) | 157 (96%) | 0.129 |
| Yes | 0 (0%) | 6 (4%) | ||
| Dislocation of bipolar head | No | 61 (100%) | 161 (99%) | 0.385 |
| Yes | 0 (0%) | 2 (1%) | ||
| Degree of mobilization | Only bed | 6 (11%) | 21 (14%) | 0.839 |
| Few steps | 23 (40%) | 54 (37%) | ||
| At ward level | 28 (49%) | 71 (49%) | ||
| Death during hospital stay | No | 57 (92%) | 154 (94%) | 0.596 |
| Yes | 5 (8%) | 10 (6%) | ||
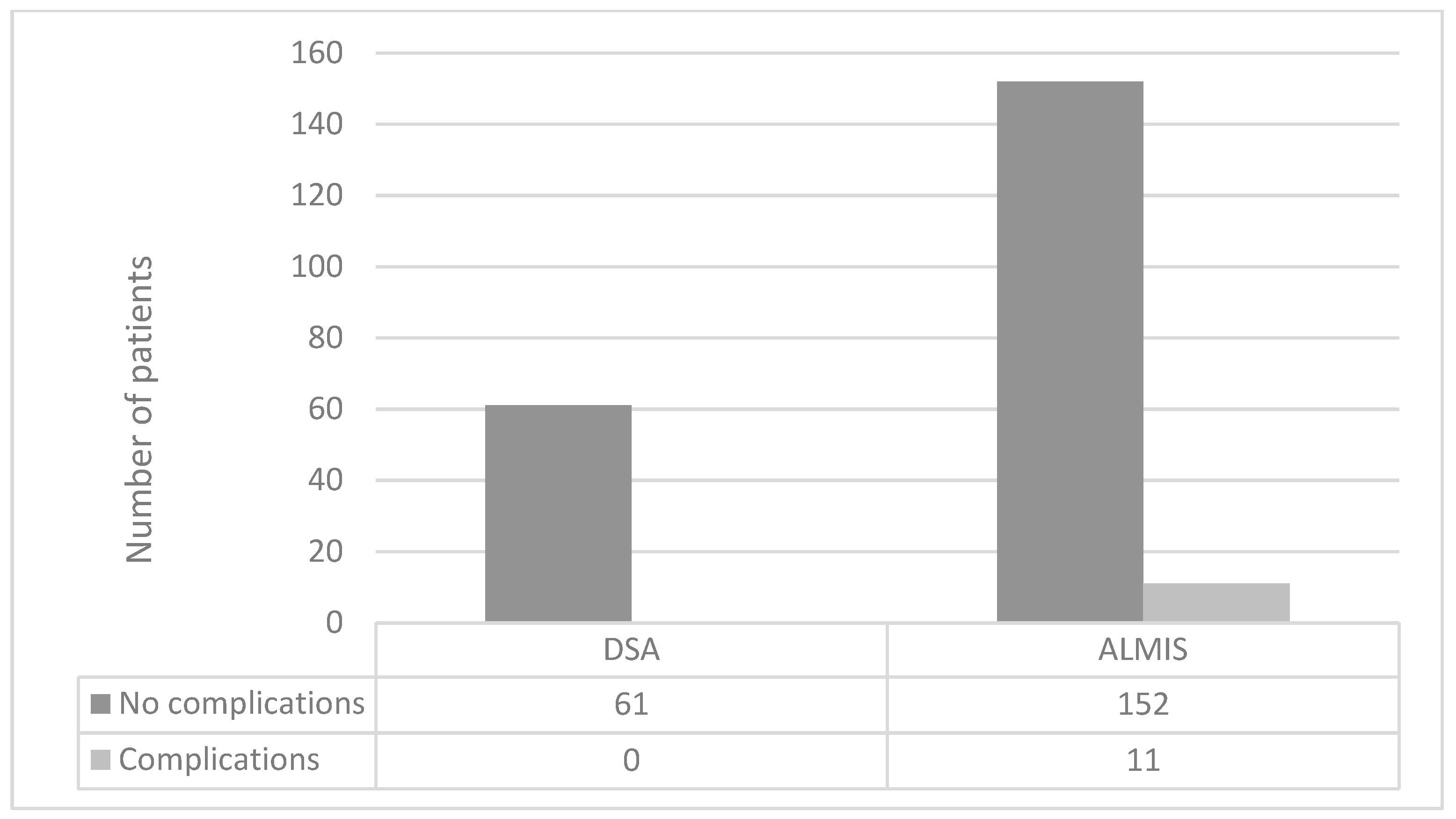
| Combined complications excl. death | No | 61 (100%) | 152 (93%) | * 0.037 |
| Yes | 0 (0%) | 11 (7%) | ||
| DSA | ALMIS | p | |
|---|---|---|---|
| Length of hospital stay in days | 11.3 (SD 6.3) | 11.2 (SD 5.3) | 0.411 |
| Length of stay in ICU in days | 0.5 (SD 1.3) | 0.5 (SD 2) | 0.190 |
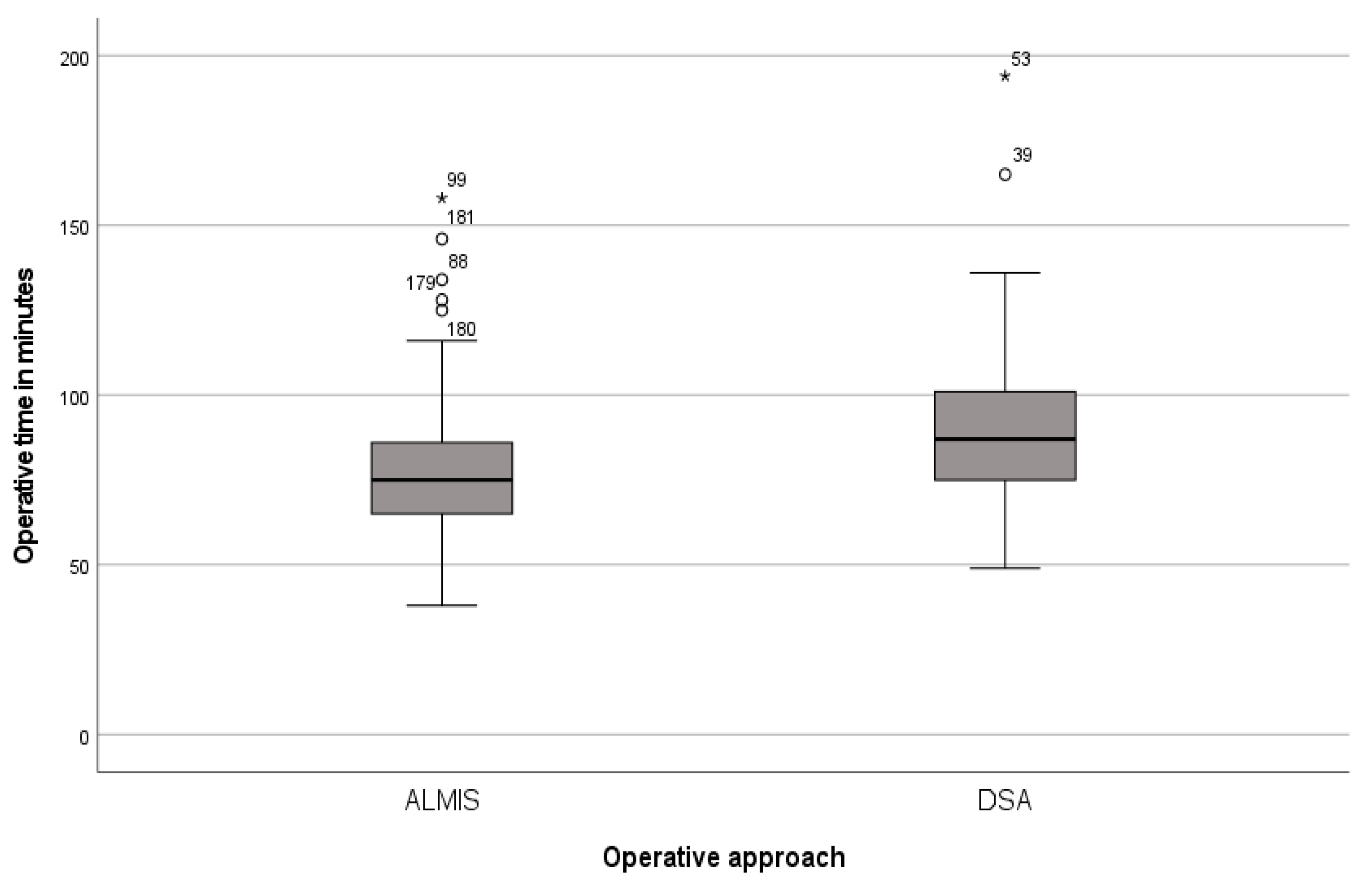
| Operative time in minutes | 89.7 (SD 25.6) | 77.2 (SD 19.1) | * <0.001 |
| Setup time in minutes | 36.7 (SD 14.1) | 32.6 (SD 10) | 0.063 |
| Preoperative hemoglobin in mmol/L | 7.4 (SD 1.3) | 7.6 (SD 1.0) | 0.169 |
| Postoperative hemoglobin in mmol/L | 6.0 (SD 1.0) | 6.0 (SD 0.9) | 0.528 |
| Pre- to postoperative difference in hemoglobin in mmol/L | 1.4 (SD 1.0) | 1.6 (SD 0.8) | * 0.034 |
| Number of transfusions in units | 0.3 (SD 0.9) | 0.1 (SD 0.4) | 0.181 |
| Blood loss according to Nagler in dL | 42.67 (SD 8.31) | 42.74 (SD 7.21) | 0.716 |
| Blood loss according to Good in L | 1.04 (SD 0.74) | 1.08 (SD 0.58) | 0.313 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moussaoui, J.; Hallbauer, J.; Wilharm, A.; Marintschev, I.; Hofmann, G.O.; Weschenfelder, W. Comparison of Short-Term Outcomes of DSA and ALMIS Approach for Bipolar Cemented Hemiarthroplasty in Patients with Neck of Femur Fracture. J. Clin. Med. 2024, 13, 6465. https://doi.org/10.3390/jcm13216465
Moussaoui J, Hallbauer J, Wilharm A, Marintschev I, Hofmann GO, Weschenfelder W. Comparison of Short-Term Outcomes of DSA and ALMIS Approach for Bipolar Cemented Hemiarthroplasty in Patients with Neck of Femur Fracture. Journal of Clinical Medicine. 2024; 13(21):6465. https://doi.org/10.3390/jcm13216465
Chicago/Turabian StyleMoussaoui, Juliane, Jakob Hallbauer, Arne Wilharm, Ivan Marintschev, Gunther Olaf Hofmann, and Wolfram Weschenfelder. 2024. "Comparison of Short-Term Outcomes of DSA and ALMIS Approach for Bipolar Cemented Hemiarthroplasty in Patients with Neck of Femur Fracture" Journal of Clinical Medicine 13, no. 21: 6465. https://doi.org/10.3390/jcm13216465
APA StyleMoussaoui, J., Hallbauer, J., Wilharm, A., Marintschev, I., Hofmann, G. O., & Weschenfelder, W. (2024). Comparison of Short-Term Outcomes of DSA and ALMIS Approach for Bipolar Cemented Hemiarthroplasty in Patients with Neck of Femur Fracture. Journal of Clinical Medicine, 13(21), 6465. https://doi.org/10.3390/jcm13216465






