Disparities in Heart Failure Deaths among Patients with Cirrhosis
Abstract
1. Introduction
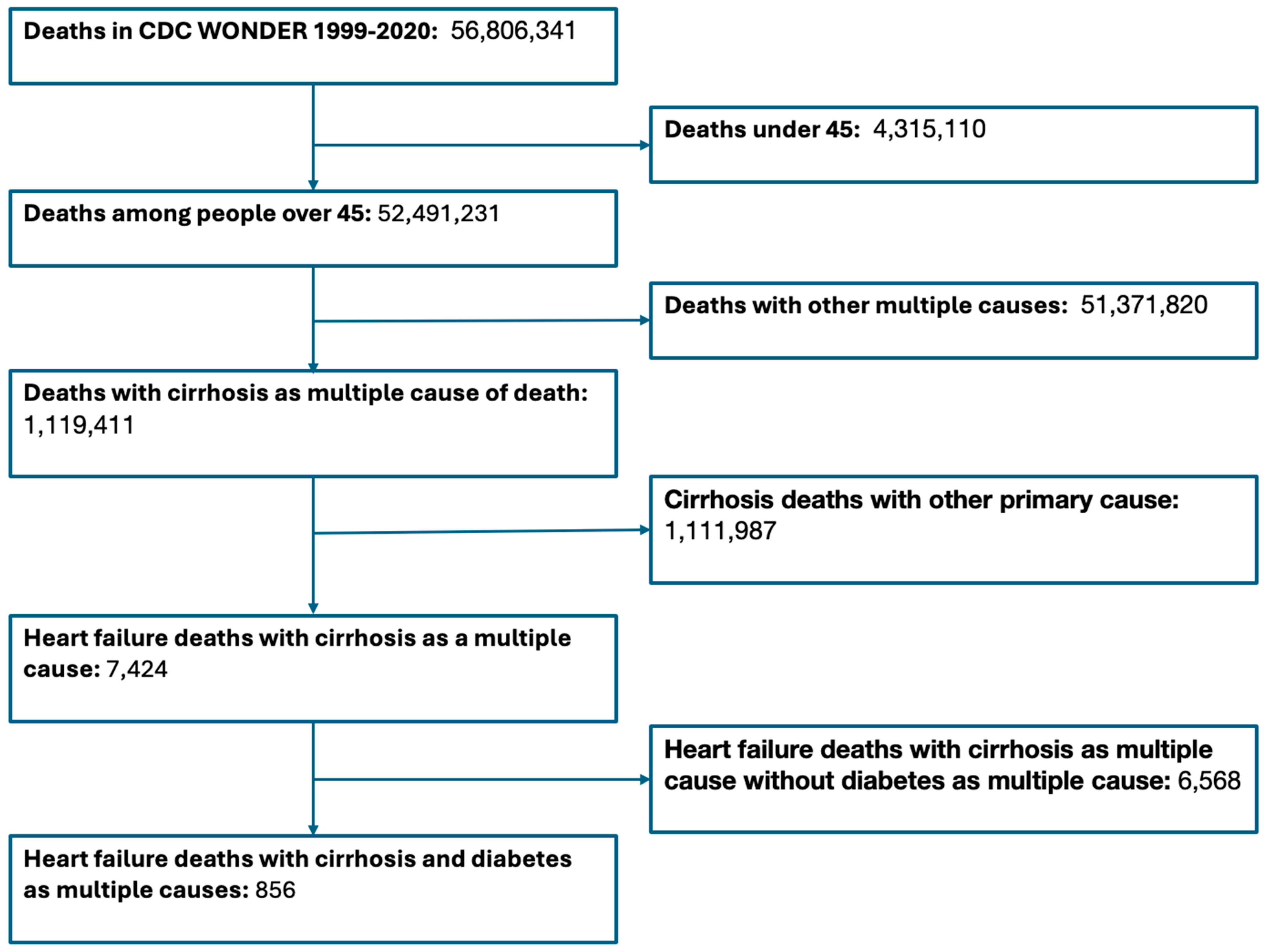
2. Materials and Methods
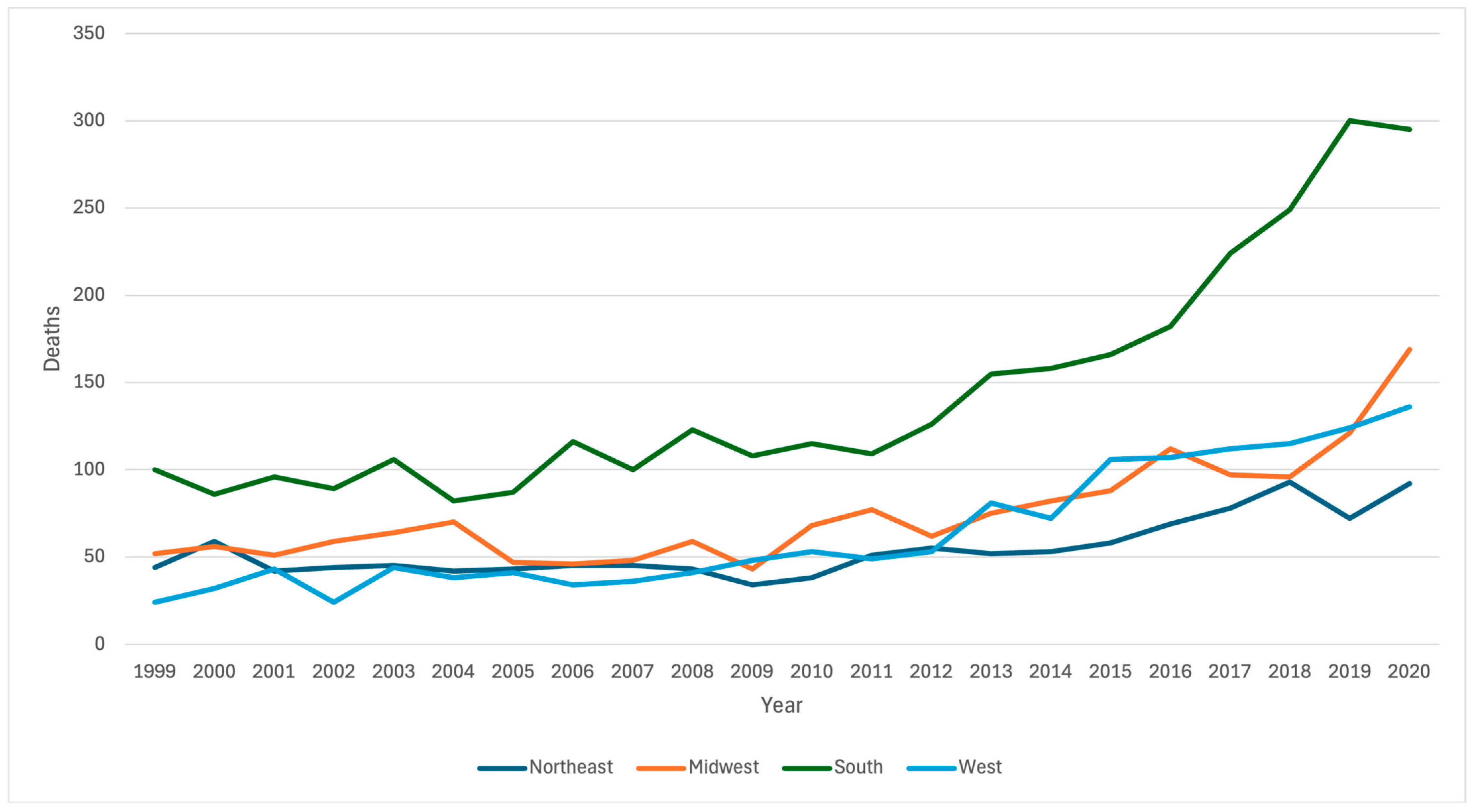
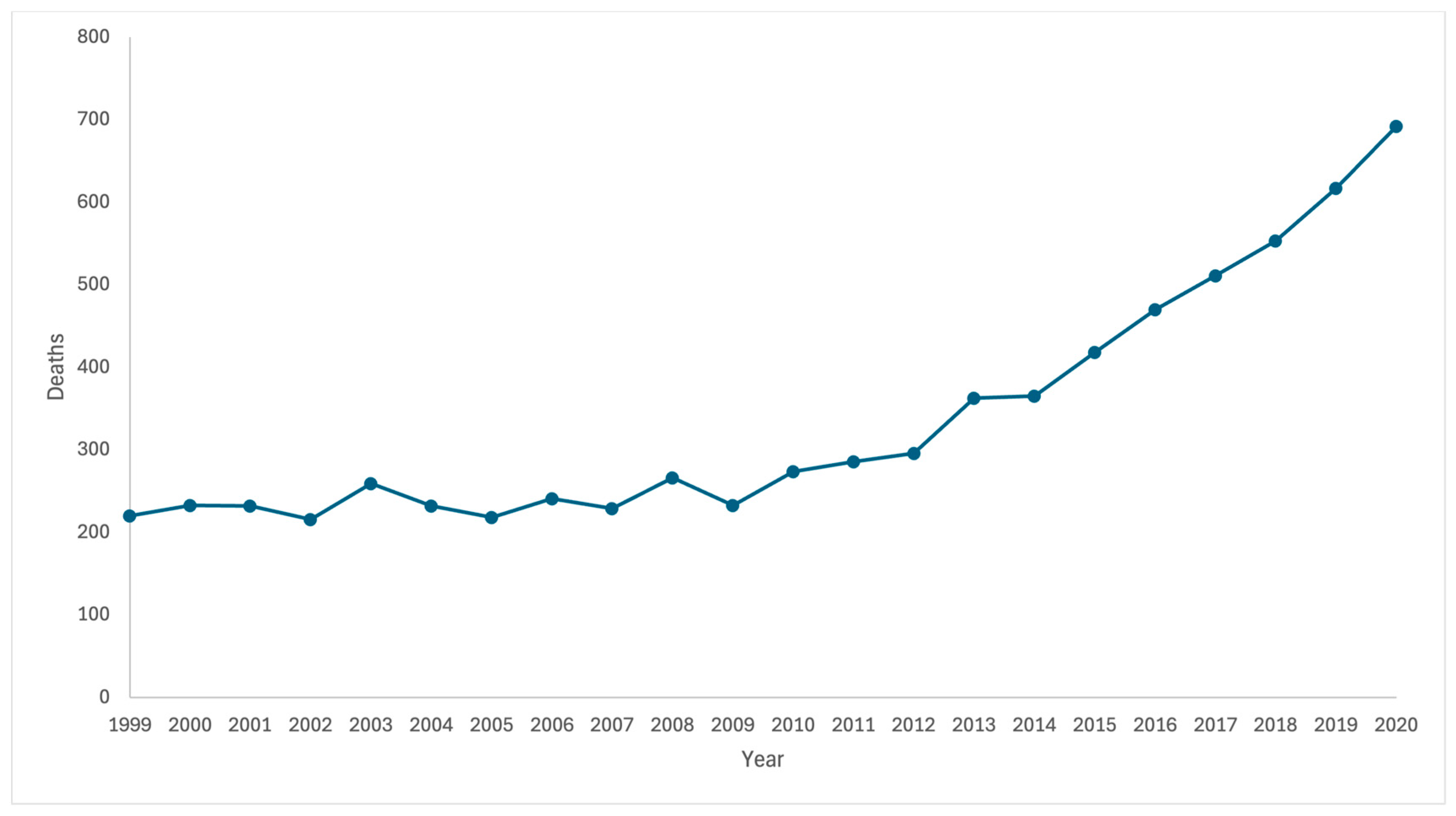
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bozkurt, B.; Ahmad, T.; Alexander, K.M.; Baker, W.L.; Bosak, K.; Breathett, K.; Fonarow, G.C.; Heidenreich, P.; Ho, J.E.; Hsich, E.; et al. Heart Failure Epidemiology and Outcomes Statistics: A Report of the Heart Failure Society of America. J. Card. Fail. 2023, 29, 1412–1451. [Google Scholar] [CrossRef] [PubMed]
- Bui, A.L.; Horwich, T.B.; Fonarow, G.C. Epidemiology and Risk Profile of Heart Failure. Nat. Rev. Cardiol. 2011, 8, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, R.; Fonarow, G.C.; Heidenreich, P.A.; Ziaeian, B. Expenditure on Heart Failure in the United States: The Medical Expenditure Panel Survey 2009–2018. JACC Heart Fail. 2022, 10, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.R.; Roalfe, A.K.; Adoki, I.; Hobbs, F.D.R.; Taylor, C.J. Survival of Patients with Chronic Heart Failure in the Community: A Systematic Review and Meta-analysis. Eur. J. Heart Fail. 2019, 21, 1306–1325. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Roger, V.L. Understanding the Epidemic of Heart Failure: Past, Present, and Future. Curr. Heart Fail. Rep. 2014, 11, 404–415. [Google Scholar] [CrossRef]
- Lewsey, S.C.; Breathett, K. Racial and Ethnic Disparities in Heart Failure: Current State and Future Directions. Curr. Opin. Cardiol. 2021, 36, 320–328. [Google Scholar] [CrossRef]
- Nassereldine, H.; Compton, K.; Li, Z.; Baumann, M.M.; Kelly, Y.O.; La Motte-Kerr, W.; Daoud, F.; Rodriquez, E.J.; Mensah, G.A.; Nápoles, A.M.; et al. The Burden of Cirrhosis Mortality by County, Race, and Ethnicity in the USA, 2000–2019: A Systematic Analysis of Health Disparities. Lancet Public Health 2024, 9, e551–e563. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Q.; Terrault, N.A.; Tacke, F.; Gluud, L.L.; Arrese, M.; Bugianesi, E.; Loomba, R. Global Epidemiology of Cirrhosis—Aetiology, Trends and Predictions. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 388–398. [Google Scholar] [CrossRef]
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global Burden of Primary Liver Cancer in 2020 and Predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef]
- Xanthopoulos, A.; Starling, R.C.; Kitai, T.; Triposkiadis, F. Heart Failure and Liver Disease. JACC Heart Fail. 2019, 7, 87–97. [Google Scholar] [CrossRef]
- Chuzi, S.; Tanaka, Y.; Bavishi, A.; Bruce, M.; Van Wagner, L.B.; Wilcox, J.E.; Ahmad, F.S.; Ladner, D.P.; Lagu, T.; Khan, S.S. Association between End-Stage Liver Disease and Incident Heart Failure in an Integrated Health System. J. Gen. Intern. Med. 2023, 38, 2445–2452. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Health and Human Services (US DHHS); Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). Multiple Cause of Death 1999–2020 on CDC WONDER. Online Database 2021. Available online: https://wonder.cdc.gov/mcd-icd10.html (accessed on 8 May 2024).
- Ha, A.Y.; Le, M.H.; Henry, L.; Yeo, Y.H.; Cheung, R.C.; Nguyen, M.H. County-Level Variation in Cirrhosis-Related Mortality in the US, 1999–2019. JAMA Netw. Open 2022, 5, e2146427. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Compean, D.; Jaquez-Quintana, J.O.; Gonzalez-Gonzalez, J.A.; Maldonado-Garza, H. Liver Cirrhosis and Diabetes: Risk Factors, Pathophysiology, Clinical Implications and Management. World J. Gastroenterol. 2009, 15, 280–288. [Google Scholar] [CrossRef]
- Kenny, H.C.; Abel, E.D. Heart Failure in Type 2 Diabetes Mellitus: Impact of Glucose-Lowering Agents, Heart Failure Therapies, and Novel Therapeutic Strategies. Circ. Res. 2019, 124, 121–141. [Google Scholar] [CrossRef]
- Klein, R.; Schoenborn, C.A. Age Adjustment Using the 2000 Projected U.S. Population; United States Department of Health and Human Services: Washington, DC, USA, 2001.
- Microsoft Excel, 2022, Microsoft: Washington, DC, USA, 2022.
- Grobman, B.; Mansur, A.; Lu, C.Y. Disparities in the Risk of Heart Disease Death among People with Chronic Lower Respiratory Disease. Int. J. Cardiol. 2024, 412, 132323. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Grobman, B.; Kothapalli, N.; Mansur, A.; Lu, C.Y. Suicide Risk Among Patients With Heart Disease and Heart Failure. Am. J. Cardiol. 2023, 203, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Grobman, B.; Kothapalli, N.; Mansur, A.; Lu, C.Y. Risk of Suicide among Stroke Survivors in the United States. J. Stroke Cerebrovasc. Dis. 2023, 32, 107272. [Google Scholar] [CrossRef]
- Mansur, A.; Grobman, B.; Lu, C.Y. Suicide Among Patients with Chronic Kidney Disease in the United States: 1999–2020. J. Nephrol. 2024, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the Tidyverse. JOSS 2019, 4, 1686. [Google Scholar] [CrossRef]
- Mazumder, N.R.; Simpson, D.; Atiemo, K.; Jackson, K.; Zhao, L.; Daud, A.; Kho, A.; Gabra, L.G.; Caicedo, J.C.; Levitsky, J.; et al. Black Patients With Cirrhosis Have Higher Mortality and Lower Transplant Rates: Results from a Metropolitan Cohort Study. Hepatology 2021, 74, 926–936. [Google Scholar] [CrossRef]
- Nguyen, V.H.; Le, I.; Ha, A.; Le, R.H.; Rouillard, N.A.; Fong, A.; Gudapati, S.; Park, J.E.; Maeda, M.; Barnett, S.; et al. Differences in Liver and Mortality Outcomes of Non-Alcoholic Fatty Liver Disease by Race and Ethnicity: A Longitudinal Real-World Study. Clin. Mol. Hepatol. 2023, 29, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.H.; Mueller, S.H.; Chung, S.-C.; Foster, G.R.; Lai, A.G. Increased Burden of Cardiovascular Disease in People with Liver Disease: Unequal Geographical Variations, Risk Factors and Excess Years of Life Lost. J. Transl. Med. 2022, 20, 2. [Google Scholar] [CrossRef]
- Fudim, M.; Zhong, L.; Patel, K.V.; Khera, R.; Abdelmalek, M.F.; Diehl, A.M.; McGarrah, R.W.; Molinger, J.; Moylan, C.A.; Rao, V.N.; et al. Nonalcoholic Fatty Liver Disease and Risk of Heart Failure Among Medicare Beneficiaries. JAHA 2021, 10, e021654. [Google Scholar] [CrossRef] [PubMed]
- Szanto, K.; Li, J.; Cordero, P.; Oben, J. Ethnic Differences and Heterogeneity in Genetic and Metabolic Makeup Contributing to Nonalcoholic Fatty Liver Disease. DMSO 2019, 12, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Chandramouli, C.; Tay, W.T.; Bamadhaj, N.S.; Tromp, J.; Teng, T.-H.K.; Yap, J.J.L.; MacDonald, M.R.; Hung, C.-L.; Streng, K.; Naik, A.; et al. Association of Obesity with Heart Failure Outcomes in 11 Asian Regions: A Cohort Study. PLoS Med. 2019, 16, e1002916. [Google Scholar] [CrossRef]
- Grobman, B.; Ortega, G.; Molina, G. The Hispanic Paradox and the Rising Incidence and Mortality from Hepatobiliary and Gastric Cancers Among Hispanic Individuals in the US: A Call for Surgeon Advocates. Ann. Surg. 2024. [Google Scholar] [CrossRef]
- Atiemo, K.; Mazumder, N.R.; Caicedo, J.C.; Ganger, D.; Gordon, E.; Montag, S.; Maddur, H.; VanWagner, L.B.; Goel, S.; Kho, A.; et al. The Hispanic Paradox in Patients With Liver Cirrhosis: Current Evidence From a Large Regional Retrospective Cohort Study. Transplantation 2019, 103, 2531–2538. [Google Scholar] [CrossRef]
- Glynn, P.A.; Molsberry, R.; Harrington, K.; Shah, N.S.; Petito, L.C.; Yancy, C.W.; Carnethon, M.R.; Lloyd-Jones, D.M.; Khan, S.S. Geographic Variation in Trends and Disparities in Heart Failure Mortality in the United States, 1999 to 2017. JAHA 2021, 10, e020541. [Google Scholar] [CrossRef]
- Siddiqi, T.J.; Khan Minhas, A.M.; Greene, S.J.; Van Spall, H.G.C.; Khan, S.S.; Pandey, A.; Mentz, R.J.; Fonarow, G.C.; Butler, J.; Khan, M.S. Trends in Heart Failure–Related Mortality Among Older Adults in the United States from 1999–2019. JACC Heart Fail. 2022, 10, 851–859. [Google Scholar] [CrossRef]
- Singh, G.K.; Daus, G.P.; Allender, M.; Ramey, C.T.; Martin, E.K.; Perry, C.; Reyes, A.A.D.L.; Vedamuthu, I.P. Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935–2016. Int. J. MCH AIDS 2017, 6, 139–164. [Google Scholar] [CrossRef]
- Mathews, L.; Ding, N.; Mok, Y.; Shin, J.; Crews, D.C.; Rosamond, W.D.; Newton, A.; Chang, P.P.; Ndumele, C.E.; Coresh, J.; et al. Impact of Socioeconomic Status on Mortality and Readmission in Patients With Heart Failure With Reduced Ejection Fraction: The ARIC Study. JAHA 2022, 11, e024057. [Google Scholar] [CrossRef] [PubMed]
- Couch, C.A.; Gray, M.S.; Shikany, J.M.; Howard, V.J.; Howard, G.; Long, D.L.; McClure, L.A.; Manly, J.J.; Cushman, M.; Zakai, N.A.; et al. Correlates of a Southern Diet Pattern in a National Cohort Study of Blacks and Whites: The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Br. J. Nutr. 2021, 126, 1904–1910. [Google Scholar] [CrossRef] [PubMed]
- Sterling, S.; Judd, S.; Bertrand, B.; Carson, T.L.; Chandler-Laney, P.; Baskin, M.L. Dietary Patterns Among Overweight and Obese African-American Women Living in the Rural South. J. Racial Ethn. Health Disparities 2018, 5, 141–150. [Google Scholar] [CrossRef]
- Kant, A.K.; Graubard, B.I. Secular Trends in Regional Differences in Nutritional Biomarkers and Self-Reported Dietary Intakes among American Adults: National Health and Nutrition Examination Survey (NHANES) 1988–1994 to 2009–2010. Public Health Nutr. 2018, 21, 927–939. [Google Scholar] [CrossRef]
- Ufere, N.N.; Patzer, R.E.; Kavalieratos, D.; Louissaint, J.; Kaplan, A.; Cross, S.H. Rural-Urban Disparities in Mortality From Cirrhosis in the United States From 1999 to 2019. Am. Coll. Gastroenterol. 2022, 117, 1162–1165. [Google Scholar] [CrossRef]
- Gaffney, A.W.; Hawks, L.; White, A.C.; Woolhandler, S.; Himmelstein, D.; Christiani, D.C.; McCormick, D. Health Care Disparities Across the Urban—Rural Divide: A National Study of Individuals with COPD. J. Rural. Health 2022, 38, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Loccoh, E.C.; Joynt Maddox, K.E.; Wang, Y.; Kazi, D.S.; Yeh, R.W.; Wadhera, R.K. Rural-Urban Disparities in Outcomes of Myocardial Infarction, Heart Failure, and Stroke in the United States. J. Am. Coll. Cardiol. 2022, 79, 267–279. [Google Scholar] [CrossRef]
- Turecamo, S.E.; Xu, M.; Dixon, D.; Powell-Wiley, T.M.; Mumma, M.T.; Joo, J.; Gupta, D.K.; Lipworth, L.; Roger, V.L. Association of Rurality With Risk of Heart Failure. JAMA Cardiol. 2023, 8, 231. [Google Scholar] [CrossRef]
- Borders, T.F.; Booth, B.M.; Suburban, R. Urban Variations in Alcohol Consumption in the United States: Findings From the National Epidemiologic Survey on Alcohol and Related Conditions. J. Rural. Health 2007, 23, 314–321. [Google Scholar] [CrossRef]
- Peters, S.A.E.; Muntner, P.; Woodward, M. Sex Differences in the Prevalence of, and Trends in, Cardiovascular Risk Factors, Treatment, and Control in the United States, 2001 to 2016. Circulation 2019, 139, 1025–1035. [Google Scholar] [CrossRef]
- Rubin, J.B.; Sundaram, V.; Lai, J.C. Gender Differences among Patients Hospitalized With Cirrhosis in the United States. J. Clin. Gastroenterol. 2020, 54, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Giard, J.-M.; Terrault, N.A. Women with Cirrhosis. Gastroenterol. Clin. North Am. 2016, 45, 345–358. [Google Scholar] [CrossRef] [PubMed]
- Abboud, Y.; Mathew, A.G.; Meybodi, M.A.; Medina-Morales, E.; Alsakarneh, S.; Choi, C.; Jiang, Y.; Pyrsopoulos, N.T. Chronic Liver Disease and Cirrhosis Mortality Rates Are Disproportionately Increasing in Younger Women in the United States Between 2000–2020. Clin. Gastroenterol. Hepatol. 2024, 22, 798–809.e28. [Google Scholar] [CrossRef] [PubMed]

| Category | Heart Failure as Primary Cause of Death | Cirrhosis as Multiple Cause of Death (Regardless of Primary Cause of Death) | Heart Failure Death Rate | Rate of Cirrhosis as a Multiple Cause of Death | |
|---|---|---|---|---|---|
| Overall | 1,415,533 | 1,119,411 | 54.7 | 42.2 | |
| Race | |||||
| Black | 139,073 | 108,240 | 61.7 | 37.3 | |
| White | 1,252,933 | 968,619 | 55.2 | 43.5 | |
| Asian | 18,373 | 22,304 | 20.9 | 20.4 | |
| Ethnicity | |||||
| Hispanic | 52,041 | 151,432 | 37.7 | 65.0 | |
| Non-Hispanic | 1,361,099 | 963,785 | 23.8 | 40.0 | |
| Region | |||||
| Northeast | 262,327 | 170,249 | 49.2 | 33.8 | |
| Midwest | 371,686 | 217,435 | 62.1 | 37.0 | |
| South | 554,864 | 439,767 | 60.6 | 44.8 | |
| West | 226,656 | 291,960 | 41.6 | 50.1 | |
| Urbanization | |||||
| Urban | 1,097,013 | 810,721 | 51.6 | 41.5 | |
| Rural | 318,520 | 308,690 | 69.2 | 44.1 | |
| Sex | |||||
| Female | 817,396 | 393,513 | 50.5 | 27.6 | |
| Male | 598,137 | 725,898 | 60.4 | 58.6 | |
| Year | |||||
| 1999–2004 | 335,850 | 220,543 | 57.0 | 36.6 | |
| 2005–2010 | 343,911 | 265,792 | 51.8 | 38.2 | |
| 2011–2015 | 325,075 | 286,259 | 51.4 | 43.8 | |
| 2016–2020 | 410,697 | 346,817 | 58.4 | 48.5 |
| Category | Cirrhosis-Associated Heart Failure Deaths | AAMR Ratio | p-Value | ||
|---|---|---|---|---|---|
| Overall | 7424 | 211.1 (210.7–211.5) | |||
| With Comorbid Diabetes | 856 | 233.9 (232.5–235.3) | |||
| Race | |||||
| White | 6449 | 206.6 (206.2–207.0) | ref | ref | |
| Black | 768 | 266.2 (264.6–267.8) | 1.288 (1.282–1.295) | <0.0001 | |
| Asian | 129 | 683.8 (674.9–692.9) | 3.310 (3.297–3.323) | <0.0001 | |
| Ethnicity | |||||
| Non-Hispanic | 6668 | 218.1 (217.7–218.6) | ref | ref | |
| Hispanic | 739 | 183.4 (182.4–184.4) | 0.841 (0.835–0.847) | <0.0001 | |
| Region | |||||
| Northeast | 1197 | 203.3 (202.4–204.3) | ref | ref | |
| Midwest | 1642 | 232.7 (231.8–233.7) | 1.145 (1.138–1.151) | <0.0001 | |
| South | 3172 | 234.2 (233.6–234.9) | 1.152 (1.146–1.158) | <0.0001 | |
| West | 1413 | 160.4 (159.9–161.0) | 0.789 (0.783–0.795) | <0.0001 | |
| Urbanization | |||||
| Urban | 5848 | 201.5 (201.0–201.9) | ref | ref | |
| Rural | 1576 | 255.0 (253.9–256.2) | 1.266 (1.261–1.271) | <0.0001 | |
| Sex | |||||
| Female | 2910 | 205.4 (204.8–206.0) | ref | ref | |
| Male | 4514 | 216.4 (215.9–216.9) | 1.053 (1.050–1.057) | 0.0004 | |
| Year | |||||
| 1999–2004 | 1392 | 194.4 (193.6–195.2) | ref | ref | |
| 2005–2010 | 1461 | 181.8 (181.1–182.5) | 0.935 (0.930–0.941) | <0.0001 | |
| 2011–2015 | 1728 | 199.9 (199.1–200.6) | 1.028 (1.023–1.034) | <0.0001 | |
| 2016–2020 | 2853 | 255.9 (255.0–256.7) | 1.317 (1.311–1.322) | <0.0001 | |
| Category | 1999–2004 | 2016–2020 | AAMR Ratio * | p Value | |
|---|---|---|---|---|---|
| Race | Death rate per 100,000 (95% CI) | Death rate per 100,000 (95% CI) | |||
| White | 191.5 (190.7–192.4) | 249.2 (248.3–250.1) | 1.301 (1.295–1.307) | <0.0001 | |
| Black | 231.8 (228.8–234.7) | 353.3 (349.4–357.3) | 1.525 (1.508–1.542) | <0.0001 | |
| Region | |||||
| Northeast | 198.4 (196.5–200.4) | 243.0 (240.7–245.2) | 1.225 (1.211–1.238) | <0.0001 | |
| Midwest | 237.2 (235.0–239.4) | 272.1 (270.0–274.1) | 1.147 (1.315–1.159) | <0.0001 | |
| South | 215.2 (213.8–216.7) | 278.0 (276.6–279.5) | 1.292 (1.283–1.300) | <0.0001 | |
| West | 122.5 (121.4–123.5) | 211.4 (210.0–212.8) | 1.726 (1.715–1.737) | <0.0001 | |
| Urbanization | |||||
| Urban | 181.2 (180.3–182.0) | 246.6 (245.7–247.5) | 1.361 (1.356–1.367) | <0.0001 | |
| Rural | 259.3 (256.6–261.9) | 298.0 (295.7–300.3) | 1.149 (1.136–1.162) | <0.0001 | |
| Sex | |||||
| Female | 199.3 (197.9–200.7) | 238.5 (237.2–239.9) | 1.197 (1.188–1.206) | <0.0001 | |
| Male | 190.4 (189.4–191.4) | 268.0 (266.9–269.1) | 1.408 (1.401–1.414) | <0.0001 |
| Category | 1994–2004 | p Value | 2016–2020 | p Value | |
|---|---|---|---|---|---|
| Race | Difference in Death Rate (Deaths per 100,000) 1 | Difference in Death Rate (Deaths per 100,000) | |||
| Black vs. White | 40.3 | <0.0001 | 104.1 | <0.0001 | |
| Region | |||||
| Midwest vs. Northeast | 38.8 | <0.0001 | 29.1 | <0.0001 | |
| South vs. Northeast | 16.8 | <0.0001 | 35.0 | <0.0001 | |
| West vs. Northeast | −75.9 | <0.0001 | −31.6 | <0.0001 | |
| Urbanization | |||||
| Rural vs. Urban | 78.1 | <0.0001 | 51.4 | <0.0001 | |
| Sex | |||||
| Male vs. Female | −8.9 | <0.0001 | 29.5 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grobman, B.; Mansur, A.; Lu, C.Y. Disparities in Heart Failure Deaths among Patients with Cirrhosis. J. Clin. Med. 2024, 13, 6153. https://doi.org/10.3390/jcm13206153
Grobman B, Mansur A, Lu CY. Disparities in Heart Failure Deaths among Patients with Cirrhosis. Journal of Clinical Medicine. 2024; 13(20):6153. https://doi.org/10.3390/jcm13206153
Chicago/Turabian StyleGrobman, Benjamin, Arian Mansur, and Christine Y. Lu. 2024. "Disparities in Heart Failure Deaths among Patients with Cirrhosis" Journal of Clinical Medicine 13, no. 20: 6153. https://doi.org/10.3390/jcm13206153
APA StyleGrobman, B., Mansur, A., & Lu, C. Y. (2024). Disparities in Heart Failure Deaths among Patients with Cirrhosis. Journal of Clinical Medicine, 13(20), 6153. https://doi.org/10.3390/jcm13206153







