Injury Pattern and Current Early Clinical Care of Pediatric Polytrauma Comparing Different Age Groups in a Level I Trauma Center
Abstract
:1. Introduction
- Are there significant differences in injury patterns, early clinical care, and treatment outcomes among different age groups within the pediatric population of severely injured patients?
- Which injured body regions are associated with higher mortality rates in severely injured pediatric patients (ISS > 16)?
2. Materials and Methods
2.1. Study Design and Inclusion Criteria
2.2. Ethics Statement and Anonymity
2.3. Statistical Analysis
3. Results
3.1. Demographic Data
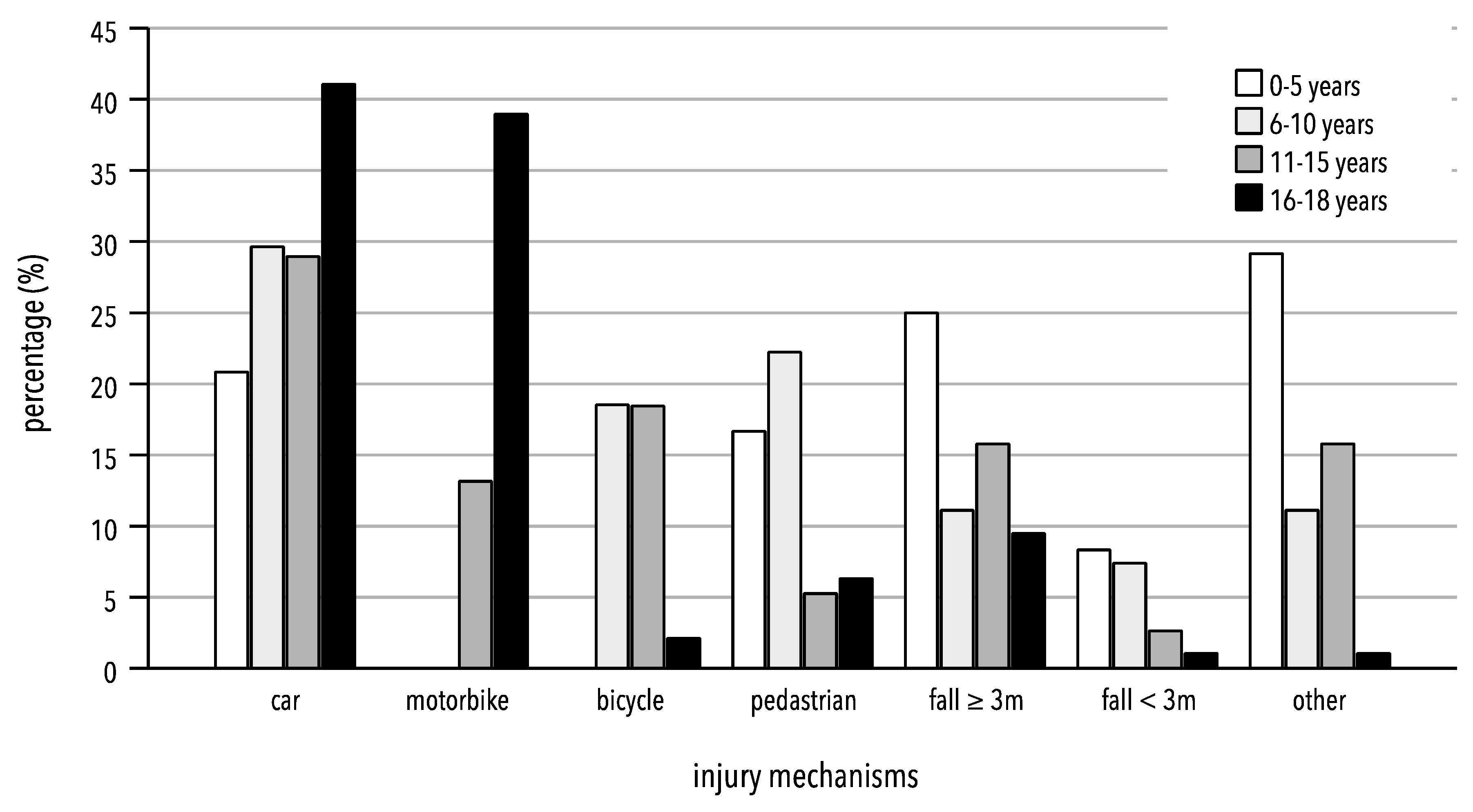
3.2. Mechanisms of Injury
3.3. Injury Pattern
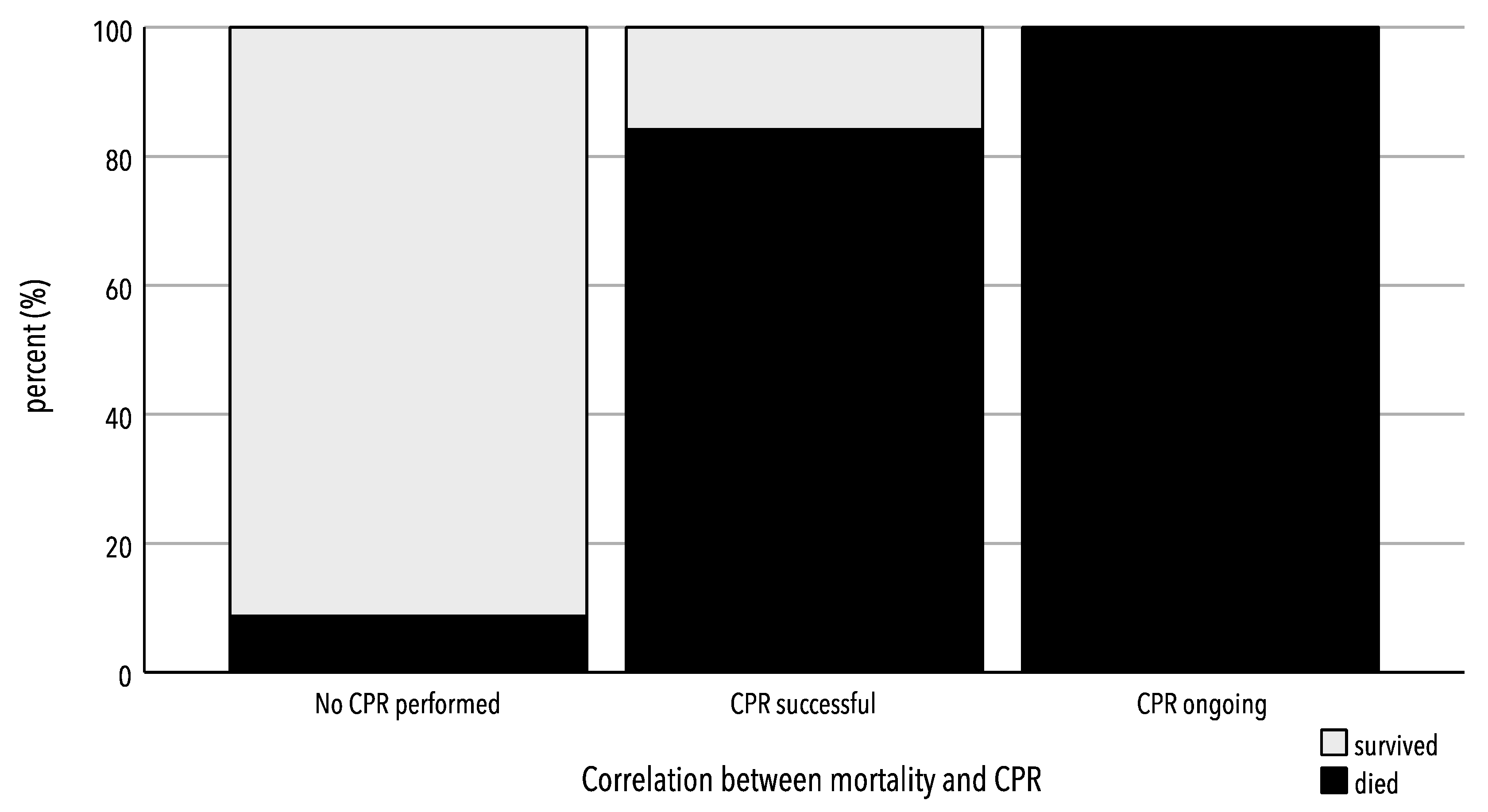
3.4. General Influence of Resuscitation on Mortality
3.5. Thirty-Day Survival/Mortality Rate
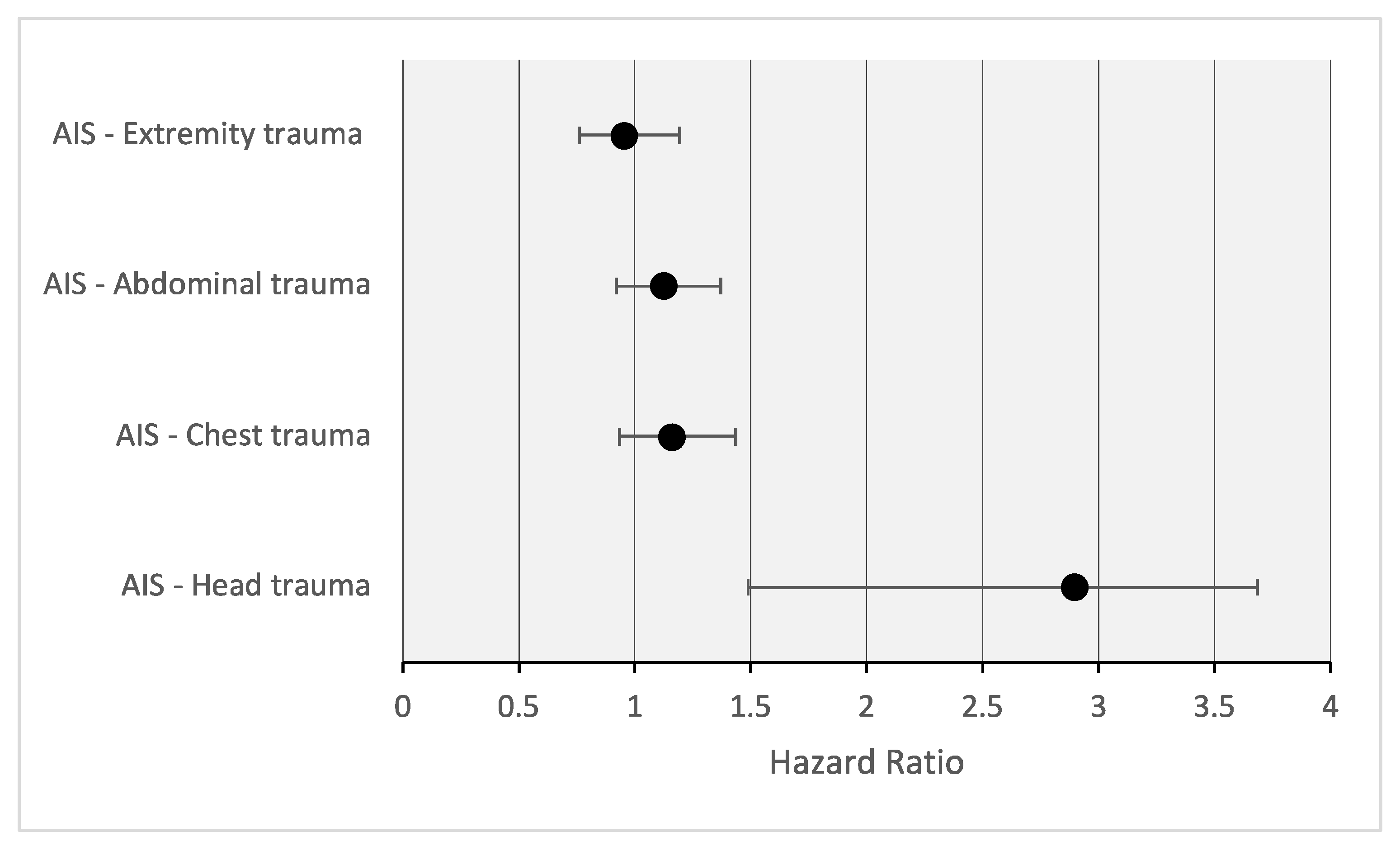
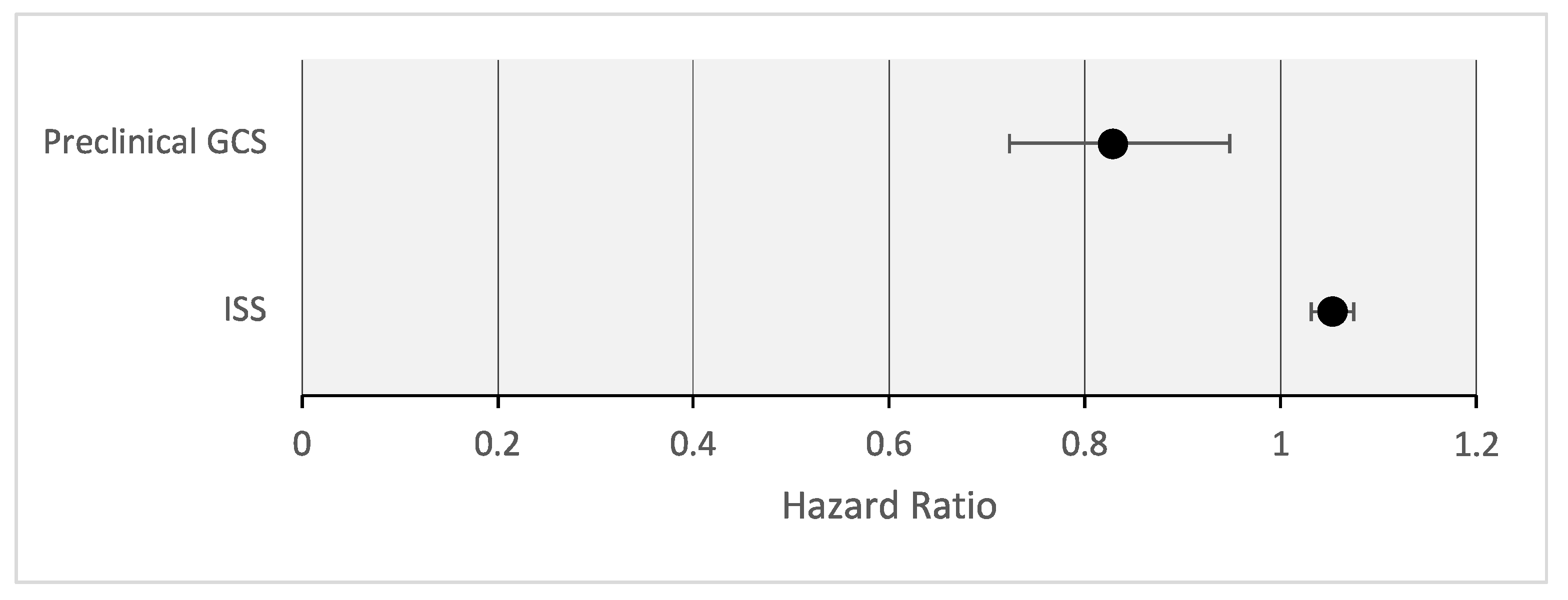
3.6. Influence of Injury Patterns on Mortality
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIS | Abbreviated Injury Scale |
| CPR | Cardiopulmonary Resuscitation |
| ED | Emergency Department |
| GCS | Glasgow Coma Scale |
| ISS | Injury Severity Score |
References
- Debus, F.; Lefering, R.; Frink, M.; Kühne, C.; Mand, C.; Ruchholtz, S. Polytrauma in children and adolescents. Choice of the primary care clinic and importance of pediatric traumatology competence centers. Unfallchirurg 2015, 118, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Statistisches Bundesamt. Fallpauschalenbezogene Krankenhausstatistik (DRG-Statistik) Diagnosen, Prozeduren, Fallpauschalen und Case Mix der Vollstationären Patientinnen und Patienten in Krankenhäusern. 2016. Available online: http://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Publikationen/Downloads-Krankenhaeuser/fallpauschalen-krankenhaus-2120640167004.pdf?__blob=publicationFile (accessed on 8 October 2023).
- Jakob, H.; Wyen, H.; Marzi, I. Polytrauma im Kindesalter. Trauma Berufskrankh. 2013, 15, 67–74. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Tödliche Verletzungen von Kindern und Jugendlichen. 2021. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Todesursachen/_inhalt.html (accessed on 7 October 2023).
- Deutsche Gesellschaft für Kinderchirurgie, e.V. (DGKCH). S2k-Leitlinie Polytraumaversorgung im Kindesalter Registernummer 006-120. Available online: https://register.awmf.org/de/leitlinien/detail/006-120 (accessed on 7 October 2023).
- Gruen, R.L.; Jurkovich, G.J.; McIntyre, L.K.; Foy, H.M.; Maier, R.V. Patterns of errors contributing to trauma mortality: Lessons learned from 2594 deaths. Ann. Surg. 2006, 244, 371–380. [Google Scholar] [CrossRef]
- Settervall, C.H.; de Alencar Domingues, C.; Sousa, R.M.; de Souza Nogueira, L. Preventable trauma deaths. Rev. Saude Publica 2012, 46, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Unfallchirurgie: Weißbuch Schwerverletztenversorgung. 3., Erweiterte Auflage. 2019. Available online: https://www.dgu-online.de/fileadmin/dgu-online/Dokumente/6._Versorgung_und_Wissenschaft/Qualität_und_Sicherheit/2019_DGU-Weissbuch_Schwerverletztenversorgung_3._Auflage_FINAL.PDF (accessed on 5 December 2023).
- Hall, J.R.; Reyes, H.M.; Meller, J.L.; Loeff, D.S.; Dembek, R. The outcome for children with blunt trauma is best at a pediatric trauma center. J. Pediatr. Surg. 1996, 31, 72–76; discussion 76–77. [Google Scholar] [CrossRef] [PubMed]
- Osler, T.M.; Vane, D.W.; Tepas, J.J.; Rogers, F.B.; Shackford, S.R.; Badger, G.J. Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J. Trauma 2001, 50, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Potoka, D.A.; Schall, L.C.; Gardner, M.J.; Stafford, P.W.; Peitzman, A.B.; Ford, H.R. Impact of pediatric trauma centers on mortality in a statewide system. J. Trauma 2000, 49, 237–245. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Hegde, S.; Bawa, M.; Kanojia, R.P.; Mahajan, J.K.; Menon, P.; Samujh, R.; Rao, K.L.N. Pediatric Trauma: Management and Lessons Learned. J. Indian Assoc. Pediatr. Surg. 2020, 25, 142–146. [Google Scholar] [CrossRef]
- Naqvi, G.; Johansson, G.; Yip, G.; Rehm, A.; Carrothers, A.; Stöhr, K. Mechanisms, patterns and outcomes of paediatric polytrauma in a UK major trauma centre. Ann. R. Coll. Surg. Engl. 2017, 99, 39–45. [Google Scholar] [CrossRef]
- Zwingmann, J.; Schmal, H.; Südkamp, N.P.; Strohm, P.C. Injury severity and localisations seen in polytraumatised children compared to adults and the relevance for emergency room management. Zentralbl. Chir. 2008, 133, 68–75. [Google Scholar] [CrossRef]
- Søreide, K.; Krüger, A.J.; Ellingsen, C.L.; Tjosevik, K.E. Pediatric trauma deaths are predominated by severe head injuries during spring and summer. Scand. J. Trauma Resusc. Emerg. Med. 2009, 17, 3. [Google Scholar] [CrossRef]
- Wyen, H.; Jakob, H.; Wutzler, S.; Lefering, R.; Laurer, H.L.; Marzi, I.; Lehnert, M. Prehospital and Early Clinical Care of Infants, Children, and Teenagers Compared to an Adult Cohort: Analysis of 2961 Children in Comparison to 21,435 Adult Patients from the Trauma Registry of DGU in a 15-Year Period. Eur. J. Trauma Emerg. Surg. 2010, 36, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Capizzani, A.R.; Drongowski, R.; Ehrlich, P.F. Assessment of termination of trauma resuscitation guidelines: Are children small adults? J. Pediatr. Surg. 2010, 45, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.; Barlow, B.; DiScala, C.; String, D. Mortality and truncal injury: The pediatric perspective. J. Pediatr. Surg. 1994, 29, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.F.; Sokolove, P.E.; Brant, W.E.; Kuppermann, N. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann. Emerg. Med. 2002, 39, 492–499. [Google Scholar] [CrossRef]
- Dykes, E.H. Paediatric trauma. Br. J. Anaesth. 1999, 83, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Charyk Stewart, T.; McClafferty, K.; Shkrum, M.; Comeau, J.L.; Gilliland, J.; Fraser, D.D. A comparison of injuries, crashes, and outcomes for pediatric rear occupants in traffic motor vehicle collisions. J. Trauma Acute Care Surg. 2013, 74, 628–633. [Google Scholar] [CrossRef]
- Schoeneberg, C.; Schilling, M.; Keitel, J.; Burggraf, M.; Hussmann, B.; Lendemans, S. Mortality in severely injured children: Experiences of a German level 1 trauma center (2002–2011). BMC Pediatr. 2014, 14, 194. [Google Scholar] [CrossRef]
- Narotam, P.K.; Burjonrappa, S.C.; Raynor, S.C.; Rao, M.; Taylon, C. Cerebral oxygenation in major pediatric trauma: Its relevance to trauma severity and outcome. J. Pediatr. Surg. 2006, 41, 505–513. [Google Scholar] [CrossRef]
- Kipfmueller, F.; Wyen, H.; Borgman, M.A.; Spinella, P.C.; Wirth, S.; Maegele, M. Epidemiology, risk stratification and outcome of severe pediatric trauma. Klin. Padiatr. 2013, 225, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.B.; Gestring, M.L.; Leeper, C.M.; Sperry, J.L.; Peitzman, A.B.; Billiar, T.R.; Gaines, B.A. The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury? J. Trauma Acute Care Surg. 2017, 82, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- Störmann, P.; Weber, J.N.; Jakob, H.; Marzi, I.; Schneidmueller, D. Thorakale Verletzungen beim schwer verletzten Kind. Unfallchirurg 2018, 121, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Ruchholtz, S.; Wirtz, D.C. (Eds.) Schwerstverletztenversorgung. Orthopädie und Unfallchirurgie Essentials; Georg Thieme Verlag KG: Stuttgart, Germany, 2019. [Google Scholar] [CrossRef]
- Narcı, A.; Solak, O.; Turhan-Haktanır, N.; Ayçiçek, A.; Demir, Y.; Ela, Y.; Özkaraca, E.; Terzi, Y. The prognostic importance of trauma scoring systems in pediatric patients. Pediatr. Surg. Int. 2009, 25, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.W.; Barry, T.M.; Ciesla, D.J.; Thatch, K.; Poulos, N.; Danielson, P.D.; Chandler, N.M.; Pracht, E.E. The International Classification of Disease Critical Care Severity Score demonstrates that pediatric burden of injury is similar to that of adults: Validation using the National Trauma Databank (☆). J. Pediatr. Surg. 2022, 57, 1354–1357. [Google Scholar] [CrossRef] [PubMed]
- Hatchimonji, J.S.; Luks, V.L.; Swendiman, R.A.; Allukian, M., 3rd; Nance, M.L.; Nace, G.W., Jr. Settling the Score: Injury Severity Score Fails to Capture Nuances in Pediatric Trauma. Pediatr. Emerg. Care 2022, 38, e828–e832. [Google Scholar] [CrossRef]
- Snyder, C.W.; Kristiansen, K.O.; Jensen, A.R.; Sribnick, E.A.; Anders, J.F.; Chen, C.X.; Lerner, E.B.; Conti, M.E. Defining Pediatric Trauma Center Resource Utilization: Multidisciplinary Consensus-Based Criteria from the Pediatric Trauma Society. J. Trauma Acute Care Surg. 2023. [Google Scholar] [CrossRef]
- Gatto, A.; Rivetti, S.; Capossela, L.; Pata, D.; Covino, M.; Chiaretti, A. Utility of a pediatric observation unit for the management of children admitted to the emergency department. Ital. J. Pediatr. 2021, 47, 11. [Google Scholar] [CrossRef]

| Total | 0–5 Years | 6–10 Years | 11–15 Years | 16–18 Years | |
|---|---|---|---|---|---|
| Number (n) | 184 | 24 | 27 | 38 | 95 |
| Age * | 16 (9.25; 17) | 3 (1; 4) | 9 (6; 9) | 14 (13; 15) | 17 (16; 18) |
| Male (n/%) | 119/64.7 | 12/50.0 | 14/51.9 | 23/60.5 | 70/73.7 |
| ISS * | 29 (22; 38) | 29 (21.25; 40.25) | 24 (21; 25) | 29 (21; 38.75) | 30 (22; 41) |
| Preclinical GCS * | 9 (3; 14) | 8 (4; 10) | 9 (3; 14) | 9 (4; 15) | 10 (3; 14) |
| Intubated (n/%) | 141/76.6 | 22/91.7 | 23/85.2 | 28/73.7 | 68/71.6 |
| Thereof preclinical (n/%) | 132/93.6 | 20/90.9 | 22/95.7 | 26/92.9 | 64/94.1 |
| Thoracic drainage (n/%) | 35/19.0 | 4/16.7 | 3/11.1 | 8/21.1 | 20/21.1 |
| Thereof bilateral (n/%) | 13/37.1 | 3/75.0 | 1/33.3 | 1/12.5 | 8/40.0 |
| Preclinical CPR (n/%) | 24/13.0 | 5/20.8 | 3/11.1 | 5/13.2 | 11/11.6 |
| Thereof successful until emergency room (n/%) | 19/79.2 | 3/60.0 | 2/66.7 | 5/100.0 | 9/82.8 |
| 30-days mortality (n/%) | 35/19.0 | 7/29.2 | 4/14.8 | 9/23.7 | 15/15.8 |
| Time of hospitalization * | 14 (6; 21) | 13 (3; 23) | 13 (7; 18) | 11 (2; 19) | 14 (9; 21) |
| Total | 0–5 Years | 6–10 Years | 11–15 Years | 16–18 Years | |
|---|---|---|---|---|---|
| Car (n/%) | 63/34.2 | 5/20.8 | 8/29.6 | 11/28.9 | 39/41.1 |
| Motorcycle (n/%) | 42/22.8 | 0 | 0 | 5/13.2 | 37/38.9 |
| Bicycle (n/%) | 14/7.6 | 0 | 5/18.5 | 7/18.4 | 2/2.1 |
| Pedestrians (n/%) | 18/9.8 | 4/16.7 | 6/22.2 | 2/5.3 | 6/6.3 |
| Fall ≥ 3 m (n/%) | 24/13.0 | 6/25.0 | 3/11.1 | 6/15.8 | 9/9.5 |
| Fall ≤ 3 m (n/%) | 6/3.3 | 2/8.3 | 2/7.4 | 1/2.6 | 1/1.1 |
| Others (n/%) | 17/9.2 | 7/29.2 | 3/11.1 | 6/15.8 | 1/1.1 |
| Total | 0–5 Years | 6–10 Years | 11–15 Years | 16–18 Years | |
|---|---|---|---|---|---|
| AIS–Head trauma * | 4 (2; 5) | 4 (3.25; 5) | 4 (3; 4) | 3 (1; 4) | 4 (1; 5) |
| AIS–Chest trauma * | 3 (0; 3) | 3 (0; 3.75) | 2 (0; 3) | 3 (0; 4) | 3 (0; 3) |
| AIS–Abdominal trauma * | 0 (0; 2) | 0 | 0 | 0 (0; 3.25) | 2 (0; 2) |
| AIS–Extremity trauma * | 2 (0; 3) | 0 (0; 2) | 2 (0; 2) | 2 (0; 3) | 3 (0; 3) |
| Total | 0–5 Years | 6–10 Years | 11–15 Years | 16–18 Years | |
|---|---|---|---|---|---|
| AIS–Head trauma (n/%) | 140/76.1 | 23/95.8 | 25/92.6 | 23/60.5 | 69/72.6 |
| AIS–Chest trauma (n/%) | 129/70.1 | 16/66.7 | 17/63.0 | 26/68.4 | 70/73.7 |
| AIS–Abdominal trauma (n/%) | 78/42.4 | 4/16.7 | 6/22.2 | 18/47.4 | 50/52.6 |
| AIS–Extremity trauma (n/%) | 116/63.0 | 8/33.3 | 15/55.6 | 24/63.2 | 69/72.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schuster, A.; Klute, L.; Kerschbaum, M.; Kunkel, J.; Schaible, J.; Straub, J.; Weber, J.; Alt, V.; Popp, D. Injury Pattern and Current Early Clinical Care of Pediatric Polytrauma Comparing Different Age Groups in a Level I Trauma Center. J. Clin. Med. 2024, 13, 639. https://doi.org/10.3390/jcm13020639
Schuster A, Klute L, Kerschbaum M, Kunkel J, Schaible J, Straub J, Weber J, Alt V, Popp D. Injury Pattern and Current Early Clinical Care of Pediatric Polytrauma Comparing Different Age Groups in a Level I Trauma Center. Journal of Clinical Medicine. 2024; 13(2):639. https://doi.org/10.3390/jcm13020639
Chicago/Turabian StyleSchuster, Anna, Lisa Klute, Maximilian Kerschbaum, Jürgen Kunkel, Jan Schaible, Josina Straub, Johannes Weber, Volker Alt, and Daniel Popp. 2024. "Injury Pattern and Current Early Clinical Care of Pediatric Polytrauma Comparing Different Age Groups in a Level I Trauma Center" Journal of Clinical Medicine 13, no. 2: 639. https://doi.org/10.3390/jcm13020639
APA StyleSchuster, A., Klute, L., Kerschbaum, M., Kunkel, J., Schaible, J., Straub, J., Weber, J., Alt, V., & Popp, D. (2024). Injury Pattern and Current Early Clinical Care of Pediatric Polytrauma Comparing Different Age Groups in a Level I Trauma Center. Journal of Clinical Medicine, 13(2), 639. https://doi.org/10.3390/jcm13020639








