Focal Pulsed Field Ablation for Atrial Arrhythmias: Efficacy and Safety under Deep Sedation
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Ablation Procedure
2.3. Sedation Protocol
2.4. Follow-Up
2.5. Endpoints
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
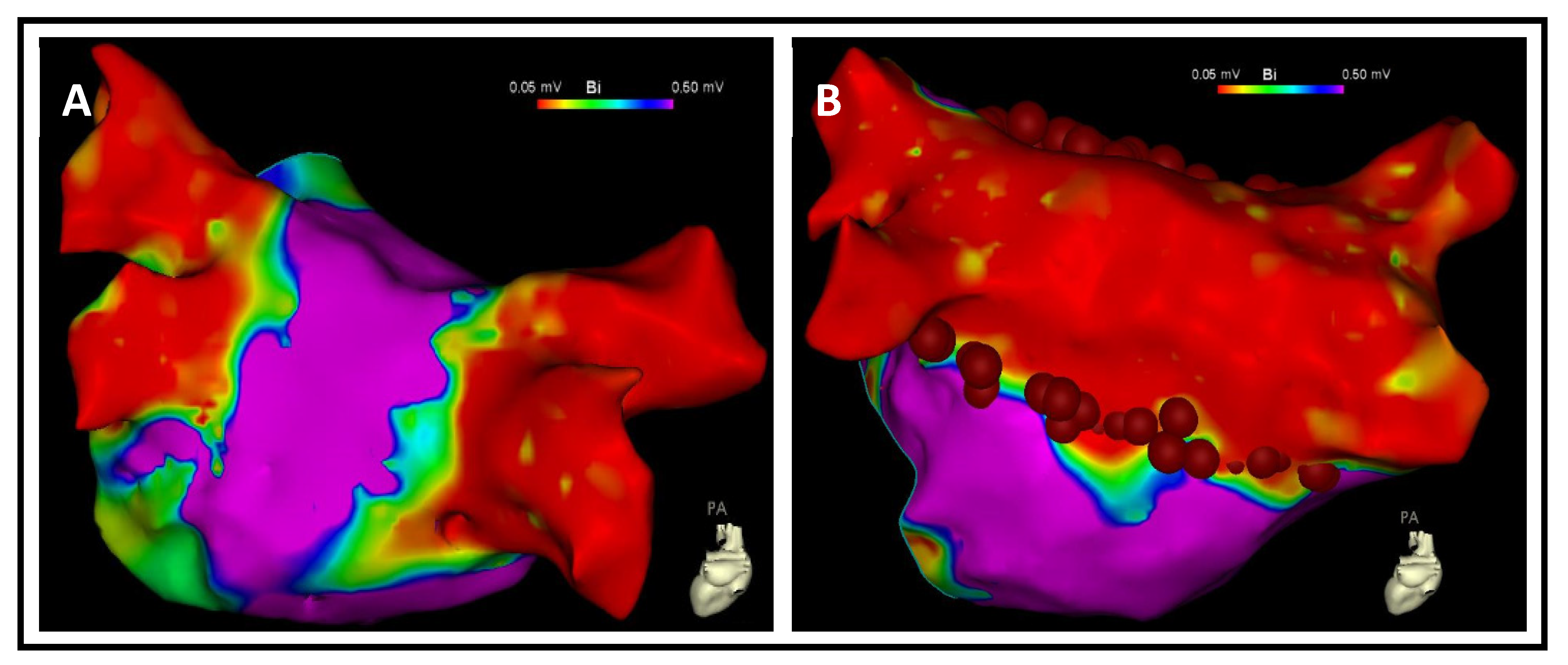
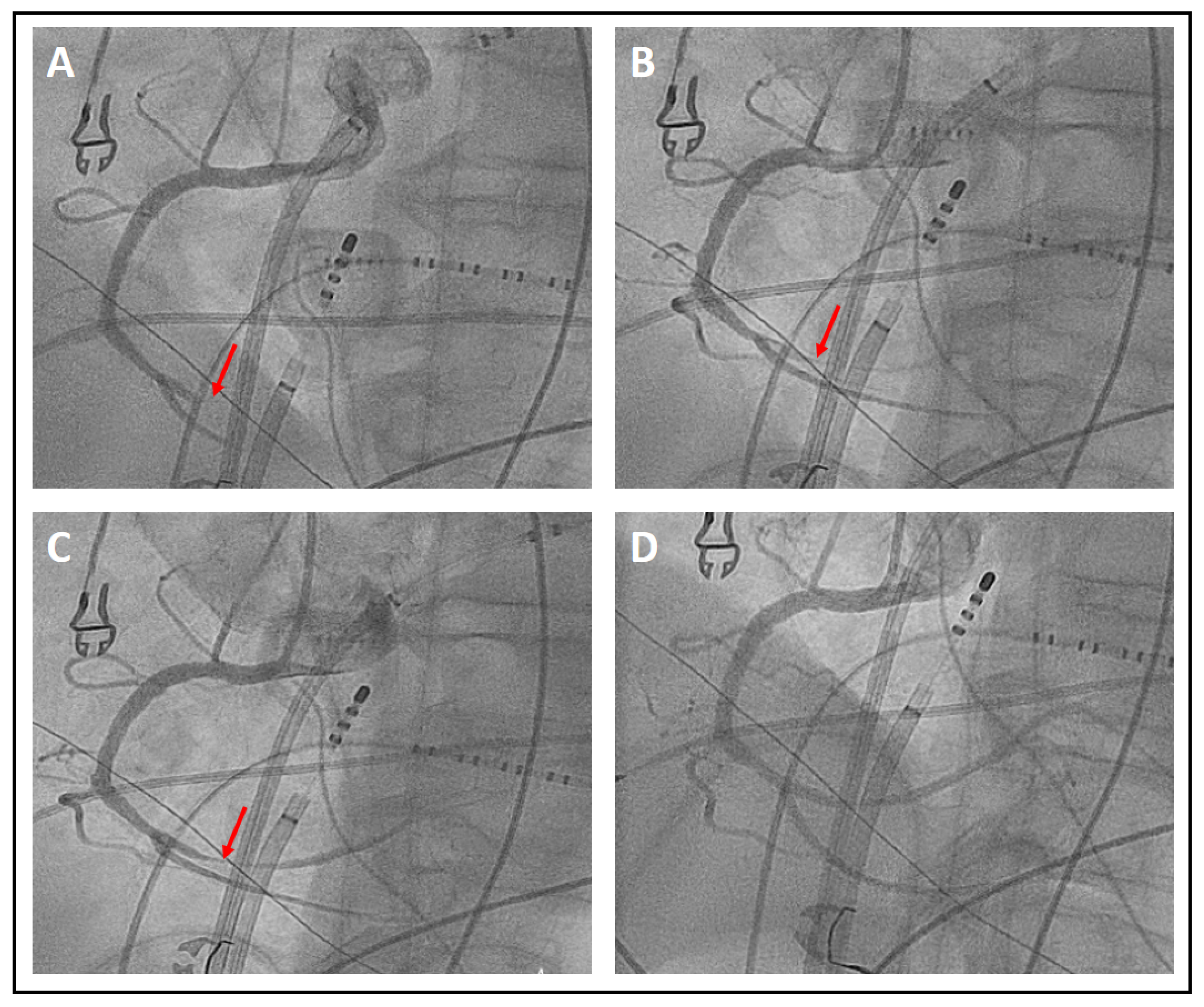
3.2. Procedural Data
3.3. Sedation Parameters
3.4. Complications
4. Discussion
4.1. Procedural Data
4.2. Sedation Concept
4.3. Complications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andrade, J.; Khairy, P.; Dobrev, D.; Nattel, S. The clinical profile and pathophysiology of atrial fibrillation: Relationships among clinical features, epidemiology, and mechanisms. Circ. Res. 2014, 114, 1453–1468. [Google Scholar] [CrossRef] [PubMed]
- Jaïs, P.; Cauchemez, B.; Macle, L.; Daoud, E.; Khairy, P.; Subbiah, R.; Hocini, M.; Extramiana, F.; Sacher, F.; Bordachar, P.; et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: The A4 study. Circulation 2008, 118, 2498–2505. [Google Scholar] [CrossRef] [PubMed]
- Mark, D.B.; Anstrom, K.J.; Sheng, S.; Piccini, J.P.; Baloch, K.N.; Monahan, K.H.; Daniels, M.R.; Bahnson, T.D.; Poole, J.E.; Rosenberg, Y.; et al. Effect of Catheter Ablation vs Medical Therapy on Quality of Life among Patients with Atrial Fibrillation: The CABANA Randomized Clinical Trial. JAMA 2019, 321, 1275–1285. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, U.; Alkukhun, L.; Kheiri, B.; Hodovan, J.; Chiang, K.; Splanger, T.; Castellvi, Q.; Zhao, Y.; Nazer, B. In vivo pulsed-field ablation in healthy vs. chronically infarcted ventricular myocardium: Biophysical and histologic characterization. Europace 2023, 25, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Neven, K.; van Es, R.; van Driel, V.; van Wessel, H.; Fidder, H.; Vink, A.; Doevendans, P.; Wittkampf, F. Acute and Long-Term Effects of Full-Power Electroporation Ablation Directly on the Porcine Esophagus. Circ. Arrhythm. Electrophysiol. 2017, 10, e004672. [Google Scholar] [CrossRef] [PubMed]
- Koruth, J.S.; Kuroki, K.; Kawamura, I.; Stoffregen, W.C.; Dukkipati, S.R.; Neuzil, P.; Reddy, V.Y. Focal Pulsed Field Ablation for Pulmonary Vein Isolation and Linear Atrial Lesions: A Preclinical Assessment of Safety and Durability. Circ. Arrhythm. Electrophysiol. 2020, 13, e008716. [Google Scholar] [CrossRef] [PubMed]
- Duytschaever, M.; de Potter, T.; Grimaldi, M.; Anic, A.; Vijgen, J.; Neuzil, P.; van Herendael, H.; Verma, A.; Skanes, A.; Scherr, D.; et al. Paroxysmal Atrial Fibrillation Ablation Using a Novel Variable-Loop Biphasic Pulsed Field Ablation Catheter Integrated With a 3-Dimensional Mapping System: 1-Year Outcomes of the Multicenter inspIRE Study. Circ. Arrhythm. Electrophysiol. 2023, 16, e011780. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Dukkipati, S.R.; Neuzil, P.; Anic, A.; Petru, J.; Funasako, M.; Cochet, H.; Minami, K.; Breskovic, T.; Sikiric, I.; et al. Pulsed Field Ablation of Paroxysmal Atrial Fibrillation: 1-Year Outcomes of IMPULSE, PEFCAT, and PEFCAT II. JACC Clin. Electrophysiol. 2021, 7, 614–627. [Google Scholar] [CrossRef]
- Verma, A.; Haines, D.E.; Boersma, L.V.; Sood, N.; Natale, A.; Marchlinski, F.E.; Calkins, H.; Sanders, P.; Packer, D.L.; Kuck, K.-H.; et al. Pulsed Field Ablation for the Treatment of Atrial Fibrillation: PULSED AF Pivotal Trial. Circulation 2023, 147, 1422–1432. [Google Scholar] [CrossRef]
- Ruwald, M.H.; Johannessen, A.; Hansen, M.L.; Haugdal, M.; Worck, R.; Hansen, J. Focal pulsed field ablation and ultrahigh-density mapping—Versatile tools for all atrial arrhythmias? Initial procedural experiences. J. Interv. Card. Electrophysiol. 2023, 67, 99–109. [Google Scholar] [CrossRef]
- Weyand, S.; Löbig, S.; Seizer, P. First in human focal pulsed field ablation to treat an epicardial VT focus with an endocardial approach in non-ischemic cardiomyopathy. J. Interv. Card. Electrophysiol. 2023, 66, 1057–1058. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Neal, R.; Evans, J.; Castellvi, Q.; Vachani, A.; Deneke, T.; Nakagawa, H. Characteristics of pulsed electric field cardiac ablation porcine treatment zones with a focal catheter. J. Cardiovasc. Electrophysiol. 2023, 34, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Duytschaever, M.; de Pooter, J.; Demolder, A.; El Haddad, M.; Phlips, T.; Strisciuglio, T.; Debonnaire, P.; Wolf, M.; Vandekerckhove, Y.; Knecht, S.; et al. Long-term impact of catheter ablation on arrhythmia burden in low-risk patients with paroxysmal atrial fibrillation: The CLOSE to CURE study. Heart Rhythm 2020, 17, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yang, Y.; Zhang, D.; Jiang, W. Meta-analysis of high power short duration in atrial fibrillation ablation—A superior efficient ablation strategy. Acta Cardiol. 2022, 77, 14–32. [Google Scholar] [CrossRef] [PubMed]
- Anić, A.; Phlips, T.; Brešković, T.; Koopman, P.; Girouard, S.; Mediratta, V.; Jurišić, Z.; Sikirić, I.; Lisica, L.; Vijgen, J. Pulsed field ablation using focal contact force-sensing catheters for treatment of atrial fibrillation: Acute and 90-day invasive remapping results. Europace 2023, 25, euad147. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, F.D.; Reddy, V.Y.; Viswanathan, R.; Hocini, M.; Jaïs, P. Emerging Technologies for Pulmonary Vein Isolation. Circ. Res. 2020, 127, 170–183. [Google Scholar] [CrossRef]
- Bai, R.; Di Biase, L.; Mohanty, P.; Trivedi, C.; Dello Russo, A.; Themistoclakis, S.; Casella, M.; Santarelli, P.; Fassini, G.; Santangeli, P.; et al. Proven isolation of the pulmonary vein antrum with or without left atrial posterior wall isolation in patients with persistent atrial fibrillation. Heart Rhythm 2016, 13, 132–140. [Google Scholar] [CrossRef]
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.-H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 2018, 20, e1–e160. [Google Scholar] [CrossRef]
- Chilukuri, K.; Scherr, D.; Dalal, D.; Cheng, A.; Spragg, D.; Nazarian, S.; Barcelon, B.D.; Marine, J.E.; Calkins, H.; Henrikson, C.A. Conventional pulmonary vein isolation compared with the “box isolation” method: A randomized clinical trial. J. Interv. Card. Electrophysiol. 2011, 32, 137–146. [Google Scholar] [CrossRef]
- Worck, R.; Sørensen, S.K.; Johannessen, A.; Ruwald, M.; Haugdal, M.; Hansen, J. Posterior wall isolation in persistent atrial fibrillation feasibility, safety, durability, and efficacy. J. Cardiovasc. Electrophysiol. 2022, 33, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Zheng, J.; Fan, L. Nonthermal Irreversible Electroporation to the Esophagus: Evaluation of Acute and Long-Term Pathological Effects in a Rabbit Model. J. Am. Heart Assoc. 2021, 10, e020731. [Google Scholar] [CrossRef]
- Reddy, V.Y.; Anic, A.; Koruth, J.; Petru, J.; Funasako, M.; Minami, K.; Breskovic, T.; Sikiric, I.; Dukkipati, S.R.; Kawamura, I.; et al. Pulsed Field Ablation in Patients With Persistent Atrial Fibrillation. J. Am. Coll. Cardiol. 2020, 76, 1068–1080. [Google Scholar] [CrossRef] [PubMed]
- Kistler, P.M.; Chieng, D.; Sugumar, H.; Ling, L.-H.; Segan, L.; Azzopardi, S.; Al-Kaisey, A.; Parameswaran, R.; Anderson, R.D.; Hawson, J.; et al. Effect of Catheter Ablation Using Pulmonary Vein Isolation With vs Without Posterior Left Atrial Wall Isolation on Atrial Arrhythmia Recurrence in Patients With Persistent Atrial Fibrillation: The CAPLA Randomized Clinical Trial. JAMA 2023, 329, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Patzelt, J.; Ulrich, M.; Magunia, H.; Sauter, R.; Droppa, M.; Jorbenadze, R.; Becker, A.S.; Walker, T.; von Bardeleben, R.S.; Grasshoff, C.; et al. Comparison of Deep Sedation With General Anesthesia in Patients Undergoing Percutaneous Mitral Valve Repair. J. Am. Heart Assoc. 2017, 6, e007485. [Google Scholar] [CrossRef]
- Alzanbagi, A.B.; Jilani, T.L.; Qureshi, L.A.; Ibrahim, I.M.; Tashkandi, A.M.S.; Elshrief, E.E.A.; Khan, M.S.; Abdelhalim, M.A.H.; Zahrani, S.A.; Mohamed, W.M.K.; et al. Randomized trial comparing general anesthesia with anesthesiologist-administered deep sedation for ERCP in average-risk patients. Gastrointest. Endosc. 2022, 96, 983–990.e2. [Google Scholar] [CrossRef]
- Menigaux, C.; Guignard, B.; Fletcher, D.; Sessler, D.I.; Dupont, X.; Chauvin, M. Intraoperative small-dose ketamine enhances analgesia after outpatient knee arthroscopy. Anesth. Analg. 2001, 93, 606–612. [Google Scholar] [CrossRef]
- Demir, C.Y.; Yuzkat, N. Prevention of Emergence Agitation with Ketamine in Rhinoplasty. Aesthetic Plast. Surg. 2018, 42, 847–853. [Google Scholar] [CrossRef]
- Okuyama, K.; Inomata, S.; Okubo, N.; Watanabe, I. Pretreatment with small-dose ketamine reduces predicted effect-site concentration of propofol required for loss of consciousness and Laryngeal Mask Airway insertion in women. J. Clin. Anesth. 2011, 23, 113–118. [Google Scholar] [CrossRef]
- Brinck, E.C.; Tiippana, E.; Heesen, M.; Bell, R.F.; Straube, S.; Moore, R.A.; Kontinen, V. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst. Rev. 2018, 12, CD012033. [Google Scholar] [CrossRef]
- Schwenk, E.S.; Viscusi, E.R.; Buvanendran, A.; Hurley, R.W.; Wasan, A.D.; Narouze, S.; Bhatia, A.; Davis, F.N.; Hooten, W.M.; Cohen, S.P. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg. Anesth. Pain Med. 2018, 43, 456–466. [Google Scholar] [CrossRef] [PubMed]
- David, H.; Shipp, J. A randomized controlled trial of ketamine/propofol versus propofol alone for emergency department procedural sedation. Ann. Emerg. Med. 2011, 57, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Girotra, S.; Mehta, Y.; Radhakrishnan, S.; Shrivastava, S. Total intravenous anesthesia with ketamine for pediatric interventional cardiac procedures. J. Cardiothorac. Vasc. Anesth. 2000, 14, 36–39. [Google Scholar] [CrossRef]
- Wutzler, A.; Huemer, M.; Boldt, L.-H.; Parwani, A.S.; Attanasio, P.; Tscholl, V.; Haverkamp, W. Effects of deep sedation on cardiac electrophysiology in patients undergoing radiofrequency ablation of supraventricular tachycardia: Impact of propofol and ketamine. Europace 2013, 15, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Iacopino, S.; Filannino, P.; Artale, P.; Colella, J.; Cecchini, F.; Statuto, G.; Di Vilio, A.; Dini, D.; Mantovani, L.; Sorrenti, P.; et al. General anesthesia in spontaneous respiration with intravenous ketamine in patients undergoing pulsed-field ablation. Europace 2023, 25, euad122.174. [Google Scholar] [CrossRef]
- Aalbers, T.T.J.; Vroon, L.C.; Westra, S.W.; Scheffer, G.J.; van Eijk, L.T.; Vaneker, M. Respiratory Acidosis during Procedural Sedation and Analgesia for Pulmonary Vein Isolation: A Prospective Observational Study. Interv. Cardiol. J. 2021, 7, 164. [Google Scholar]
- Eastwood, G.M.; Young, P.J.; Bellomo, R. The impact of oxygen and carbon dioxide management on outcome after cardiac arrest. Curr. Opin. Crit. Care 2014, 20, 266–272. [Google Scholar] [CrossRef]
- Helmerhorst, H.J.F.; Roos-Blom, M.-J.; van Westerloo, D.J.; Abu-Hanna, A.; de Keizer, N.F.; de Jonge, E. Associations of arterial carbon dioxide and arterial oxygen concentrations with hospital mortality after resuscitation from cardiac arrest. Crit. Care 2015, 19, 348. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Petru, J.; Funasako, M.; Kopriva, K.; Hala, P.; Chovanec, M.; Janotka, M.; Kralovec, S.; Neuzil, P. Coronary Arterial Spasm During Pulsed Field Ablation to Treat Atrial Fibrillation. Circulation 2022, 146, 1808–1819. [Google Scholar] [CrossRef]
- de Greef, Y.; Ströker, E.; Schwagten, B.; Kupics, K.; de Cocker, J.; Chierchia, G.-B.; de Asmundis, C.; Stockman, D.; Buysschaert, I. Complications of pulmonary vein isolation in atrial fibrillation: Predictors and comparison between four different ablation techniques: Results from the MIddelheim PVI-registry. Europace 2018, 20, 1279–1286. [Google Scholar] [CrossRef]
| Baseline Characteristics | n = 30 |
|---|---|
| Age (years) | 71.07 ± 7.11 |
| Male | 14 (46.47) |
| BMI (kg/m2) | 27.95 ± 5.03 |
Type of arrhythmia
| 3 (10) 22 (73.33) 17 (56.67) |
| CHA2DS2-VASc score | 2.62 ± 1.21 |
| LV ejection fraction (%) | 56.64 ± 6.92 |
| Moderate or severely dilated LA | 18 (60) |
| Low voltage areas (<0.5 mV) in the LA (%) | 34.09 ± 36.47 |
| Chronic kidney disease | 5 (16.67) |
| Coronary artery disease | 6 (20) |
| Hypertension | 24 (80) |
| Diabetes mellitus | 1 (3.33) |
| Prior Stroke/TIA | 0 (0) |
Current Medication
| 22 (73.33) 2 (6.67) 30 (100) |
| n = 30 | |
|---|---|
| Isolation/linear anatomical block | 30 (100) |
| Patients discharged in sinus rhythm | 30 (100) |
| Procedural duration (min) | 122.5 ± 42.85 |
3D mapping system
| 21 (70) 9 (30) |
| Fluoroscopy time (min) | 9.14 ± 6.65 |
| Dose area product (cGy*cm2) | 654.3 ± 502.6 |
Rhythm at start of procedure
| 15 (50) 12 (40) 3 (10) |
First-time left atrial ablation
| 6 (20) 2 (33.33) 4 (66.67) |
Repeat ablation
| 24 (80) 16 (66.67) 21 (87.5) |
| Posterior box | 20 (66.67) |
| Anterior mitral line | 15 (50) |
| Lateral mitral isthmus | 2 (6.67) |
| Post-adenosine conduction recovery | 2 (6.67) |
| CTI ablation | 4 (13.33) |
| Major complication | 0 (0%) |
| Minor complication | 2 (6.67%) |
| n = 30 | |
|---|---|
| General anesthesia/intubation | 0 (0) |
| Mean propofol infusion rate (mg/h) | 286.3 ± 66.72 |
| Mean remifentanil infusion rate (µg/h) RASS of −5 achieved before mapping | 134.66 ± 45.76 30 (100) |
| Application of 12.5 mg ketamine | 14 (46.67) |
| Nasal oxygen administered (L/min) | 3.83 ± 1.56 |
| Mapshift requiring remapping | 1 (3.33) |
| Oxygen drop requiring mask ventilation | 0 (0) |
| pH (before start of ablation) | 7.28 ± 0.05 |
| pCO2 (before start of ablation) (mmHg) | 56.59 ± 8.29 |
| Major Complications | |
|---|---|
| Procedure-related deaths | 0 (0) |
| Atrio-esophageal fistulae | 0 (0) |
| Procedure-related strokes or TIAs | 0 (0) |
| Pericardial tamponades requiring intervention | 0 (0) |
| Hemothorax | 0 (0) |
| Severe air embolism with ST elevation | 0 (0) |
| Nitrosensitive ST elevation (vasospasm) | 1 (3.33) |
| New-onset renal failure requiring dialysis | 0 (0) |
| Vascular access complications requiring intervention | 0 (0) |
| Minor Complications | |
| Vascular access complications without intervention | 1 (3.33) |
| Pneumonia | 0 (0) |
| Hemoptysis | 0 (0) |
| Acute hypersensitivity reactions to the contrast agent | 0 (0) |
| Postinterventional pericarditis or small pericardial effusion | 0 (0) |
| Total Complications | 2 (6.67) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weyand, S.; Adam, V.; Biehler, P.; Hägele, P.; Hanger, S.; Heinzmann, D.; Löbig, S.; Pinchuk, A.; Waechter, C.; Seizer, P. Focal Pulsed Field Ablation for Atrial Arrhythmias: Efficacy and Safety under Deep Sedation. J. Clin. Med. 2024, 13, 576. https://doi.org/10.3390/jcm13020576
Weyand S, Adam V, Biehler P, Hägele P, Hanger S, Heinzmann D, Löbig S, Pinchuk A, Waechter C, Seizer P. Focal Pulsed Field Ablation for Atrial Arrhythmias: Efficacy and Safety under Deep Sedation. Journal of Clinical Medicine. 2024; 13(2):576. https://doi.org/10.3390/jcm13020576
Chicago/Turabian StyleWeyand, Sebastian, Viola Adam, Paloma Biehler, Patricia Hägele, Simon Hanger, David Heinzmann, Stephanie Löbig, Andrei Pinchuk, Christian Waechter, and Peter Seizer. 2024. "Focal Pulsed Field Ablation for Atrial Arrhythmias: Efficacy and Safety under Deep Sedation" Journal of Clinical Medicine 13, no. 2: 576. https://doi.org/10.3390/jcm13020576
APA StyleWeyand, S., Adam, V., Biehler, P., Hägele, P., Hanger, S., Heinzmann, D., Löbig, S., Pinchuk, A., Waechter, C., & Seizer, P. (2024). Focal Pulsed Field Ablation for Atrial Arrhythmias: Efficacy and Safety under Deep Sedation. Journal of Clinical Medicine, 13(2), 576. https://doi.org/10.3390/jcm13020576








