Diagnosis and Therapy of Community-Acquired Pneumonia in the Emergency Department: A Retrospective Observational Study and Medical Audit
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Study Population
2.3. Data Collection and Analysis
2.4. Guidelines
- -
- Confirming pneumonia with a chest X-ray of all patients.
- -
- Obtaining two pairs of blood cultures in hospitalized patients.
- -
- Urine antigen testing (legionella and pneumococcal antigen) in hospitalized patients.
- -
- Obtaining sputum culture if it can be processed within 4 h.
- -
- Performing influenza PCR on a respiratory specimen during influenza season (Note that this study was performed prior to the COVID-19 pandemic).
- -
- Additional aspects recommended by “med standards”: [35]
- -
- Peripheral oxygen saturation (SpO2) and respiratory rate should be measured.
- -
- Auscultation and percussion should be performed.
- -
- Hemogram and blood chemistry (including procalcitonin) should be measured.
- -
- Arterial blood gas analysis should be performed.
- -
- Therapy of CAP:
- -
- Empiric therapy according to the guidelines.
- -
- Length of antibiotic therapy is 5 days (at least 2 days after reaching clinical stability), while for severe pneumonia it is 5–7 days (at least 2 days after reaching clinical stability).
- -
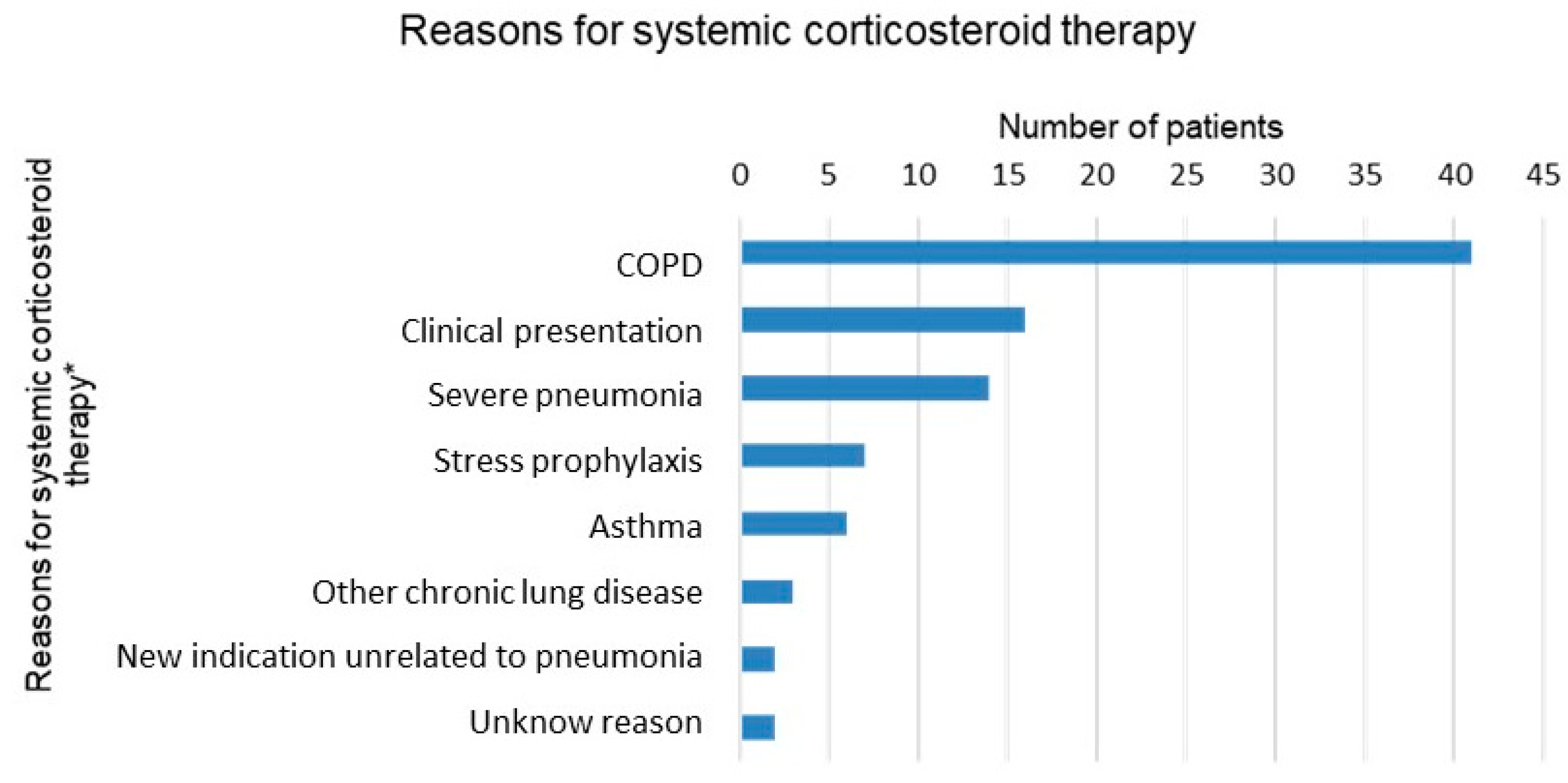
- Oral steroids for patients with chronic obstructive pulmonary disease (COPD) or asthma with evidence of obstruction on pulmonary auscultation for 5–7 days.
3. Results
3.1. Patient Characteristics
3.2. Diagnostics and Assessment
3.3. Therapy
4. Discussion
4.1. Comparison of Findings to the Guidelines: Narrative Discussion
4.1.1. Diagnosis of CAP
- -
- Confirming pneumonia with a chest X-ray on all patients
- -
- Obtaining two pairs of blood cultures in hospitalized patients
- -
- Urine legionella and pneumococcal antigen testing
- -
- Obtaining sputum culture if it can be processed within 4 h
- -
- Performing influenza PCR during influenza season
- -
- Respiratory multiplex PCR panel only in selected cases
- -
- Peripheral oxygen saturation (SpO2) and respiratory should be measured
- -
- Complete blood count and blood chemistry (including CRP and PCT) should be measured
- -
- Auscultation and percussion should be performed
- -
- Arterial blood gas analysis should be performed
- -
- Additional comments on the diagnosis of CAP
4.1.2. Therapy of Community-Acquired Pneumonia
- -
- Empiric therapy according to the guidelines
- -
- Duration of antibiotic therapy: 5 days (at least 2 days after reaching clinical stability), for severe pneumonia, 5–7 days (at least 2 days after reaching clinical stability)
- -
- Systemic corticosteroids for patients with COPD or asthma with evidence of bronchial obstruction, for 5–7 days
4.2. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Type of Complication Documented | n, (%) |
|---|---|
| Pleural effusion a | 55 (21.7) |
| Sepsis | 5 (2.0) |
| ARDS | 0 (0) |
| Empyema | 1 (0.4) |
| Cardiac complications | 45 (17.7) |
| Thromboembolic complications | 2 (0.8) |
| Acute kidney injury (at least AKIN I) | 52 (20.5) |
| Electrolyte disorders | 48 (18.9) |
| Elevated liver enzymes | 18 (7.1) |
| Neurological complications | 14 (5.5) |
| Fall | 17 (6.7) |
| Syncope | 3 (1.2) |
References
- Ott, S.R. Ambulant erworbene und nosokomiale Pneumonie. Swiss Med. Forum 2018, 18, 569–574. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016; WHO: Geneva, Switzerland, 2018; Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates (accessed on 1 January 2020).
- Troeger, C.; Blacker, B.; Khalil, I.A.; Rao, P.C.; Cao, J.; Zimsen, S.R.; Albertson, S.B.; Deshpande, A.; Farag, T.; Abebe, Z.; et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1191–1210. [Google Scholar] [CrossRef] [PubMed]
- Peyrani, P.; Mandell, L.; Torres, A.; Tillotson, G.S. The burden of community-acquired bacterial pneumonia in the era of antibiotic resistance. Expert Rev. Respir. Med. 2019, 13, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Bjarnason, A.; Westin, J.; Lindh, M.; Andersson, L.-M.; Kristinsson, K.G.; Löve, A.; Baldursson, O.; Gottfredsson, M. Incidence, Etiology, and Outcomes of Community-Acquired Pneumonia: A Population-Based Study. Open Forum Infect. Dis. 2018, 5, ofy010. [Google Scholar] [CrossRef] [PubMed]
- Said, M.A.; Johnson, H.L.; Nonyane, B.A.S.; Deloria-Knoll, M.; O’Brien, K.L.; Andreo, F.; Beovic, B.; Blanco, S.; Boersma, W.G.; Boulware, D.R.; et al. Estimating the burden of pneumococcal pneumonia among adults: A systematic review and meta-analysis of diagnostic techniques. PLoS ONE 2013, 8, e60273. [Google Scholar] [CrossRef]
- Brown, J.S. Community-acquired pneumonia. Clin. Med. 2012, 12, 538–543. [Google Scholar] [CrossRef]
- Lim, W.S.; Macfarlane, J.T.; Boswell, T.C.; Harrison, T.G.; Rose, D.; Leinonen, M.; Saikku, P. Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: Implications for management guidelines. Thorax 2001, 56, 296–301. [Google Scholar] [CrossRef]
- Musher, D.M.; Roig, I.L.; Cazares, G.; Stager, C.E.; Logan, N.; Safar, H. Can an etiologic agent be identified in adults who are hospitalized for community-acquired pneumonia: Results of a one-year study. J. Infect. 2013, 67, 11–18. [Google Scholar] [CrossRef]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, D.M.; et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef]
- Viasus, D.; Vecino-Moreno, M.; de La Hoz, J.M.; Carratalà, J. Antibiotic stewardship in community-acquired pneumonia. Expert Rev. Anti Infect. Ther. 2017, 15, 351–359. [Google Scholar] [CrossRef]
- Ewig, S.; Birkner, N.; Strauss, R.; Schaefer, E.; Pauletzki, J.; Bischoff, H.; Schraeder, P.; Welte, T.; Hoeffken, G. New perspectives on community-acquired pneumonia in 388406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax 2009, 64, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Ewig, S.; Höffken, G.; Kern, W.V.; Rohde, G.; Flick, H.; Krause, R.; Ott, S.; Bauer, T.; Dalhoff, K.; Gatermann, S.; et al. Behandlung von erwachsenen Patienten mit ambulant erworbener Pneumonie und Prävention—Update 2016. Pneumologie 2016, 70, 151–200. [Google Scholar] [CrossRef] [PubMed]
- Bodí, M.; Rodríguez, A.; Solé-Violán, J.; Gilavert, M.C.; Garnacho, J.; Blanquer, J.; Jimenez, J.; de La Torre, M.V.; Sirvent, J.M.; Almirall, J.; et al. Antibiotic prescription for community-acquired pneumonia in the intensive care unit: Impact of adherence to Infectious Diseases Society of America guidelines on survival. Clin. Infect. Dis. 2005, 41, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Bateman, R.M.; Sharpe, M.D.; Jagger, J.E.; Ellis, C.G.; Solé-Violán, J.; López-Rodríguez, M.; Herrera-Ramos, E.; Ruíz-Hernández, J.; Borderías, L.; Horcajada, J.; et al. 36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium, 15–18 March 2016. Crit. Care 2016, 20, 94. [Google Scholar] [CrossRef]
- McCabe, C.; Kirchner, C.; Zhang, H.; Daley, J.; Fisman, D.N. Guideline-concordant therapy and reduced mortality and length of stay in adults with community-acquired pneumonia: Playing by the rules. Arch. Intern. Med. 2009, 169, 1525–1531. [Google Scholar] [CrossRef] [PubMed]
- Liapikou, A.; Torres, A. Current treatment of community-acquired pneumonia. Expert Opin. Pharmacother. 2013, 14, 1319–1332. [Google Scholar] [CrossRef]
- Albrich, W.; Kahlert, C.; Blanco, N.B.; Hauser, C.; Pedrazini, B.; Ott, S.; Swiss Society for Infectious Diseases. Pneumonie/Ambulant-Erworbene Pneumonie CAP. SSI Guidelines. Available online: https://ssi.guidelines.ch/guideline/3007 (accessed on 15 February 2023).
- Ewig, S.; Kolditz, M.; Pletz, M.; Altiner, A.; Albrich, W.; Drömann, D.; Flick, H.; Gatermann, S.; Krüger, S.; Nehls, W.; et al. Behandlung von erwachsenen Patienten mit ambulant erworbener Pneumonie—Update 2021. Pneumologie 2021, 75, 665–729. [Google Scholar] [CrossRef]
- Lim, W.S.; Baudouin, S.V.; George, R.C.; Hill, A.T.; Jamieson, C.; Le Jeune, I.; Macfarlane, J.T.; Read, R.C.; Roberts, H.J.; Levy, M.L.; et al. BTS guidelines for the management of community acquired pneumonia in adults: Update 2009. Thorax 2009, 64 (Suppl. S3), iii1–iii55. [Google Scholar] [CrossRef]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). Pneumonia in Adults: Diagnosis and Management; NICE: London, UK, 2022; ISBN 9781473108646. [Google Scholar]
- Dean, N.C.; Silver, M.P.; Bateman, K.A.; James, B.; Hadlock, C.J.; Hale, D. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am. J. Med. 2001, 110, 451–457. [Google Scholar] [CrossRef]
- Capelastegui, A.; España, P.P.; Quintana, J.M.; Gorordo, I.; Ortega, M.; Idoiaga, I.; Bilbao, A. Improvement of process-of-care and outcomes after implementing a guideline for the management of community-acquired pneumonia: A controlled before-and-after design study. Clin. Infect. Dis. 2004, 39, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D. Adherence to guidelines for community-acquired pneumonia: Does it decrease cost of care? Pharmacoeconomics 2004, 22, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Nyamande, K.; Lalloo, U.G. Poor adherence to South African guidelines for the management of community-acquired pneumonia. S. Afr. Med. J. 2007, 97, 601–603. [Google Scholar] [PubMed]
- Silveira, C.D.; Ferreira, C.S.; Corrêa, R.d.A. Adherence to guidelines and its impact on outcomes in patients hospitalized with community-acquired pneumonia at a university hospital. J. Bras. Pneumol. 2012, 38, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllidis, C.; Kapordelis, V.; Papaetis, G.S.; Orphanidou, D.; Apostolidou, M.; Nikolopoulos, I.; Pefanis, A. Guidelines adherence for patients with community acquired pneumonia in a Greek hospital. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1–9. [Google Scholar] [PubMed]
- Costantini, E.; Allara, E.; Patrucco, F.; Faggiano, F.; Hamid, F.; Balbo, P.E. Adherence to guidelines for hospitalized community-acquired pneumonia over time and its impact on health outcomes and mortality. Intern. Emerg. Med. 2016, 11, 929–940. [Google Scholar] [CrossRef]
- Dixon, N. Getting Clinical Audit Right to Benefit Patients; Healthcare Quality Quest: Romsey, UK, 2008; ISBN 1873543069. [Google Scholar]
- Dixon, N. What is clinical audit’s purpose: Quality assurance or quality improvement? FDJ 2011, 2, 79–83. [Google Scholar] [CrossRef]
- El Fahimi, N.; Calleja, M.A.; Ratnayake, L.; Ali, I. Audit of a multidisciplinary approach to improve management of community-acquired pneumonia. Eur. J. Hosp. Pharm. 2019, 26, 223–225. [Google Scholar] [CrossRef]
- O’Kelly, B.; Rueda-Benito, A.; O’Regan, M.; Finan, K. An audit of community-acquired pneumonia antimicrobial compliance using an intervention bundle in an Irish hospital. J. Glob. Antimicrob. Resist. 2020, 23, 38–45. [Google Scholar] [CrossRef]
- Alyacoubi, S.; Abuowda, Y.; Albarqouni, L.; Böttcher, B.; Elessi, K. Inpatient management of community-acquired pneumonia at the European Gaza Hospital: A clinical audit. Lancet 2018, 391 (Suppl. S2), S40. [Google Scholar] [CrossRef]
- University Hospital Basel. MedStandards. Available online: https://www.medstandards.ch/ (accessed on 15 February 2023).
- Viasus, D.; Calatayud, L.; McBrown, M.V.; Ardanuy, C.; Carratalà, J. Urinary antigen testing in community-acquired pneumonia in adults: An update. Expert Rev. Anti Infect. Ther. 2019, 17, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Molinos, L.; Zalacain, R.; Menéndez, R.; Reyes, S.; Capelastegui, A.; Cillóniz, C.; Rajas, O.; Borderías, L.; Martín-Villasclaras, J.J.; Bello, S.; et al. Sensitivity, Specificity, and Positivity Predictors of the Pneumococcal Urinary Antigen Test in Community-Acquired Pneumonia. Ann. Am. Thorac. Soc. 2015, 12, 1482–1489. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, A.; Xie, X.; Teltscher, M.; Dendukuri, N. Systematic review and meta-analysis of a urine-based pneumococcal antigen test for diagnosis of community-acquired pneumonia caused by Streptococcus pneumoniae. J. Clin. Microbiol. 2013, 51, 2303–2310. [Google Scholar] [CrossRef] [PubMed]
- Erdede, M.; Denizbasi, A.; Onur, O.; Guneysel, O. Do we really need blood cultures in treating patients with community-acquired pneumonia? Bratisl. Lek. Listy 2010, 111, 286–289. [Google Scholar] [PubMed]
- Waterer, G.W.; Jennings, S.G.; Wunderink, R.G. The impact of blood cultures on antibiotic therapy in pneumococcal pneumonia. Chest 1999, 116, 1278–1281. [Google Scholar] [CrossRef] [PubMed]
- van der Eerden, M.M.; Vlaspolder, F.; de Graaff, C.S.; Groot, T.; Bronsveld, W.; Jansen, H.M.; Boersma, W.G. Comparison between pathogen directed antibiotic treatment and empirical broad spectrum antibiotic treatment in patients with community acquired pneumonia: A prospective randomised study. Thorax 2005, 60, 672–678. [Google Scholar] [CrossRef]
- Couturier, M.R.; Graf, E.H.; Griffin, A.T. Urine antigen tests for the diagnosis of respiratory infections: Legionellosis, histoplasmosis, pneumococcal pneumonia. Clin. Lab. Med. 2014, 34, 219–236. [Google Scholar] [CrossRef]
- Kim, P.; Deshpande, A.; Rothberg, M.B. Urinary Antigen Testing for Respiratory Infections: Current Perspectives on Utility and Limitations. Infect. Drug Resist. 2022, 15, 2219–2228. [Google Scholar] [CrossRef]
- Asti, L.; Bartsch, S.M.; Umscheid, C.A.; Hamilton, K.; Nachamkin, I.; Lee, B.Y. The potential economic value of sputum culture use in patients with community-acquired pneumonia and healthcare-associated pneumonia. Clin. Microbiol. Infect. 2019, 25, e1–e1038. [Google Scholar] [CrossRef]
- Hyams, C.; Williams, O.M.; Williams, P. Urinary antigen testing for pneumococcal pneumonia: Is there evidence to make its use uncommon in clinical practice? ERJ Open Res. 2020, 6, 00223-2019. [Google Scholar] [CrossRef]
- Rosón, B.; Carratalà, J.; Verdaguer, R.; Dorca, J.; Manresa, F.; Gudiol, F. Prospective study of the usefulness of sputum Gram stain in the initial approach to community-acquired pneumonia requiring hospitalization. Clin. Infect. Dis. 2000, 31, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Kitsios, G.D.; Iwata, M.; Terasawa, T. Sputum Gram Stain for Bacterial Pathogen Diagnosis in Community-acquired Pneumonia: A Systematic Review and Bayesian Meta-analysis of Diagnostic Accuracy and Yield. Clin. Infect. Dis. 2020, 71, 499–513. [Google Scholar] [CrossRef] [PubMed]
- Bundesamt für Gesundheit. Bericht zur Grippesaison 2018/19. BAG-Bulletin 2019, 29, 9–21. Available online: https://www.bag.admin.ch/dam/bag/de/dokumente/mt/infektionskrankheiten/grippe/saisonbericht-grippe-2018-19.pdf.download.pdf/saisonbericht-grippe-2018-19-de.pdf (accessed on 15 February 2023).
- University Hospital Basel, M. Immunosuppression, Sepsis, Suspected MRSA, Suspected Pseudomonas Aeruginosa, Suspected Atypical Pneumonia. Available online: https://medstandards.com/view/standard/4054 (accessed on 15 February 2023).
- Strauß, R.; Ewig, S.; Richter, K.; König, T.; Heller, G.; Bauer, T.T. The prognostic significance of respiratory rate in patients with pneumonia: A retrospective analysis of data from 705,928 hospitalized patients in Germany from 2010–2012. Dtsch. Arztebl. Int. 2014, 111, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Kamat, I.S.; Ramachandran, V.; Eswaran, H.; Guffey, D.; Musher, D.M. Procalcitonin to Distinguish Viral From Bacterial Pneumonia: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2020, 70, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, P.; Wirz, Y.; Sager, R.; Christ-Crain, M.; Stolz, D.; Tamm, M.; Bouadma, L.; Luyt, C.E.; Wolff, M.; Chastre, J.; et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: A patient level meta-analysis. Lancet Infect. Dis. 2018, 18, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Pepper, D.J.; Sun, J.; Rhee, C.; Welsh, J.; Powers, J.H.; Danner, R.L.; Kadri, S.S. Procalcitonin-Guided Antibiotic Discontinuation and Mortality in Critically Ill Adults: A Systematic Review and Meta-analysis. Chest 2019, 155, 1109–1118. [Google Scholar] [CrossRef]
- Huang, D.T.; Yealy, D.M.; Filbin, M.R.; Brown, A.M.; Chang, C.-C.H.; Doi, Y.; Donnino, M.W.; Fine, J.; Fine, M.J.; Fischer, M.A.; et al. Procalcitonin-Guided Use of Antibiotics for Lower Respiratory Tract Infection. N. Engl. J. Med. 2018, 379, 236–249. [Google Scholar] [CrossRef]
- Levin, K.P.; Hanusa, B.H.; Rotondi, A.; Singer, D.E.; Coley, C.M.; Marrie, T.J.; Kapoor, W.N.; Fine, M.J. Arterial blood gas and pulse oximetry in initial management of patients with community-acquired pneumonia. J. Gen. Intern. Med. 2001, 16, 590–598. [Google Scholar] [CrossRef]
- Majumdar, S.R.; Eurich, D.T.; Gamble, J.-M.; Senthilselvan, A.; Marrie, T.J. Oxygen saturations less than 92% are associated with major adverse events in outpatients with pneumonia: A population-based cohort study. Clin. Infect. Dis. 2011, 52, 325–331. [Google Scholar] [CrossRef]
- Mortensen, E.M.; Coley, C.M.; Singer, D.E.; Marrie, T.J.; Obrosky, D.S.; Kapoor, W.N.; Fine, M.J. Causes of death for patients with community-acquired pneumonia: Results from the Pneumonia Patient Outcomes Research Team cohort study. Arch. Intern. Med. 2002, 162, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Lüthi-Corridori, G.; Boesing, M.; Roth, A.; Giezendanner, S.; Leuppi-Taegtmeyer, A.B.; Schuetz, P.; Leuppi, J.D. Predictors of Length of Stay, Rehospitalization and Mortality in Community-Acquired Pneumonia Patients: A Retrospective Cohort Study. J. Clin. Med. 2023, 12, 5601. [Google Scholar] [CrossRef] [PubMed]
- Breuer, O.; Picard, E.; Benabu, N.; Erlichman, I.; Reiter, J.; Tsabari, R.; Shoseyov, D.; Kerem, E.; Cohen-Cymberknoh, M. Predictors of Prolonged Hospitalizations in Pediatric Complicated Pneumonia. Chest 2018, 153, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Freund, Y.; Lemachatti, N.; Krastinova, E.; van Laer, M.; Claessens, Y.-E.; Avondo, A.; Occelli, C.; Feral-Pierssens, A.-L.; Truchot, J.; Ortega, M.; et al. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017, 317, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.; Edinger, F.; Fischer, T.; Brenck, F.; Hecker, A.; Katzer, C.; Markmann, M.; Sander, M.; Schneck, E. Comparison of qSOFA score, SOFA score, and SIRS criteria for the prediction of infection and mortality among surgical intermediate and intensive care patients. World J. Emerg. Surg. 2020, 15, 63. [Google Scholar] [CrossRef]
- Grudzinska, F.S.; Aldridge, K.; Hughes, S.; Nightingale, P.; Parekh, D.; Bangash, M.; Dancer, R.; Patel, J.; Sapey, E.; Thickett, D.R.; et al. Early identification of severe community-acquired pneumonia: A retrospective observational study. BMJ Open Respir. Res. 2019, 6, e000438. [Google Scholar] [CrossRef]
- Lim, W.S.; Lawrence, H. National Audit Report: Adult Community Acquired Pneumonia Audit 2018–2019. Br. Thorac. Soc. Rep. 2019, 10. Available online: https://www.brit-thoracic.org.uk/document-library/quality-improvement/audit-reports/adult-community-acquired-pneumonia-2018-19/ (accessed on 15 February 2023).

| All (n = 254) | Missing n (%) | |
|---|---|---|
| Demographics | ||
| Age, median (IQR) | 78 (66–85) | |
| Male, n (%) | 131 (51.6) | |
| Housing situation prior to admission | ||
| Private home, n (%) | 219 (86.2) | |
| Care facility, n (%) | 35 (13.8) | |
| BMI, median (IQR) | 25.7 (22.3–30.1) | 92 (36.2) |
| Obesity (BMI ≧ 30), n (%) | 60 (23.6) | 19 (7.5) |
| Smoking status | 122 (48) | |
| Lifelong non-smoker, n (%) | 42 (31.8) | |
| Current smoker, n (%) | 33 (25) | |
| Former smoker, n (%) | 57 (43.2) | |
| Comorbidities | ||
| Hypertension, n (%) | 149 (58.7) | |
| Other cardiovascular disease, n (%) | 144 (56.7) | |
| COPD, n (%) | 56 (22) | |
| Asthma, n (%) | 20 (7.9) | |
| Other chronic lung diseases, n (%) | 35 (13.8) | |
| Oxygen therapy at home, n (%) | 15 (5.9) | |
| Diabetes mellitus type 1 and 2, n (%) | 45 (17.7) | |
| Active cancer, n (%) | 21 (8.3) | |
| Severe chronic kidney disease (KDIGO G3b or higher), n (%) | 34 (13.4) | |
| Hospital outcomes | ||
| Length of stay in day LOS, median (IQR) | 6.5 (5–9) | |
| Admission to ICU/IMC, n (%) | 24 (9.4) | |
| Death within 30 days, n (%) | 3 (1.2) | |
| Death within 1 year, n (%) | 23 (9.1) | |
| Readmission to KSBL within 30 days, n (%) | 24 (9.4) |
| Images Performed, n = 253, (99.6%) | n (%) |
|---|---|
| Imaging | 253 (99.6) |
| Chest X-ray at admission | 239 (94.1) |
| Chest CT all | 49 (19.3) |
| CT at admission | 28 (11.0) |
| CT during hospitalization | 24 (9.4) |
| Infiltrate detected | 219 (86.6) |
| Type of Test | Result | n (%) | ||
|---|---|---|---|---|
| Blood cultures | performed, n (%) | 206 (81.1) | ||
| positive, n (%) | 19 (9.2) | |||
| no growth, n (%) | 187 (90.8) | |||
| Urinary antigen testing | ||||
| Legionella antigen | performed, n (%) | 230 (90.6) | ||
| positive, n (%) | 7 (3.0) | |||
| negative, n (%) | 223 (97.0) | |||
| Pneumococcal antigen | performed, n (%) | 227 (89.4) | ||
| positive, n (%) | 51 (22.5) | |||
| negative, n (%) | 176 (77.5) | |||
| Influenza | ||||
| All patients | performed, n (%) | 127 (50.0) | ||
| Influenza A | positive, n (%) | 20 (15.7) | ||
| Influenza B | positive, n (%) | 0 (0) | ||
| During influenza season (n = 168) a | performed, n (%) | 122 (72.6) | ||
| Sputum microbiology | performed, n (%) | 42 (16.5) | ||
| growth of a respiratory pathogen, n (%) | 11 (26.2) | |||
| no growth, n (%) | 31 (73.8) | |||
| Respiratory multiplex PCR | performed, n (%) | 11 (4.3) | ||
| pathologic, n (%) | 6 (54.5) | |||
| Vital Signs | |
|---|---|
| Respiratory rate measured, n (%) | 195 (76.8) |
| Respiratory rate, mean (SD) | 22.15 (±5.91) |
| Tachypnoea (respiratory rate >20), n (%) | 100 (51.3) |
| Oxygen saturation measured n (%) | 254 (100) |
| Without supplemental oxygen therapy, n = 221 (87%), mean % (SD) | 92.59 (±4.79) |
| Hypoxaemia (SpO2 < 90%), n (%) | 38 (17.2) |
| With supplemental oxygen therapy n = 33 (13%), mean % (SD) | 93.64 (±3.26) |
| Hypoxaemia (SpO2 < 90%), n (%) | 3 (9.1) |
| Supplemental oxygen administered during hospitalization, n (%) | 122 (48) |
| Blood pressure measured, n (%) | 246 (96.9) |
| Systolic blood pressure (mmHg), mean (SD) | 131.65 (±24.34) |
| Diastolic blood pressure (mmHg), mean (SD) | 75.57 (±15.65) |
| Hypertension (systolic blood pressure > 140 mmHg) | 85 (33.6%) |
| Hypotension (systolic blood pressure < 100 mmHg) | 18 (7.1%) |
| Heart rate measured, n (%) | 254 (100) |
| Heart rate, mean (SD) | 92.61 (±18.95) |
| Tachycardia (heart rate ≥ 100 bpm), n (%) | 88 (34.6) |
| Bradycardia (heart rate < 60 bpm), n (%) | 7 (2.76) |
| Body temperature measured, n (%) | 243 (95.7) |
| Body temperature °C, mean (SD) c | 37.70 (±0.98) |
| Fever (≥38.5° C), n (%) | 59 (23.80) |
| Hypothermia (<36.0 °C), n (%) | 6 (2.36) |
| CRP measured, n (%) | 254 (100) |
| Value at admission, median (IQR) | 129 (54.5, 222.0) |
| Elevated at admission (value ≥ 5 mg/L), n (%) | 248 (97.6) |
| Highest value during hospitalization, median (IQR) | 161.5 (91.5, 248,8) |
| Leucocytes measured at admission, n (%) | 254 (100) |
| Value at admission, median (IQR) | 12.0 (8.9, 15.5) |
| Elevated at admission (value > 10.5 109/L), n (%) | 161 (63.39) |
| PCT measured, n (%) | 58 (22.8) |
| Value at admission, median (IQR) | 0.29 (0.10, 0.91) |
| Elevated value at admission (value ≥ 0.25 μg/L), n (%) | 31 (53.5) |
| Value measured during hospitalization, median | 0.23 (0.16, 0.58) |
| Type of Antibiotic Therapy | n (%) |
|---|---|
| Amoxicillin/clavulanate only | 144 (56.7) |
| Amoxicillin/clavulanate + Clarithromycin | 29 (11.4) |
| Amoxicillin/clavulanate + Clarithromycin + Clindamycin | 1 (0.4) |
| Amoxicillin/clavulanate + Clindamycin | 1 (0.4) |
| Piperacillin + Tazobactam | 6 (2.4) |
| Ceftriaxone only | 50 (19.7) |
| Ceftriaxone + Clarithromycin | 12 (4.7) |
| Ceftriaxone + Azithromycin | 1 (0.4) |
| Cefuroxime | 4 (1.6) |
| Cefepime | 1 (0.4) |
| Levofloxacin | 4 (1.6) |
| Clarithromycin only | 1 (0.4) |
| Choice of empiric antibiotic therapy according to Swiss guidelines | 191 (75.2) |
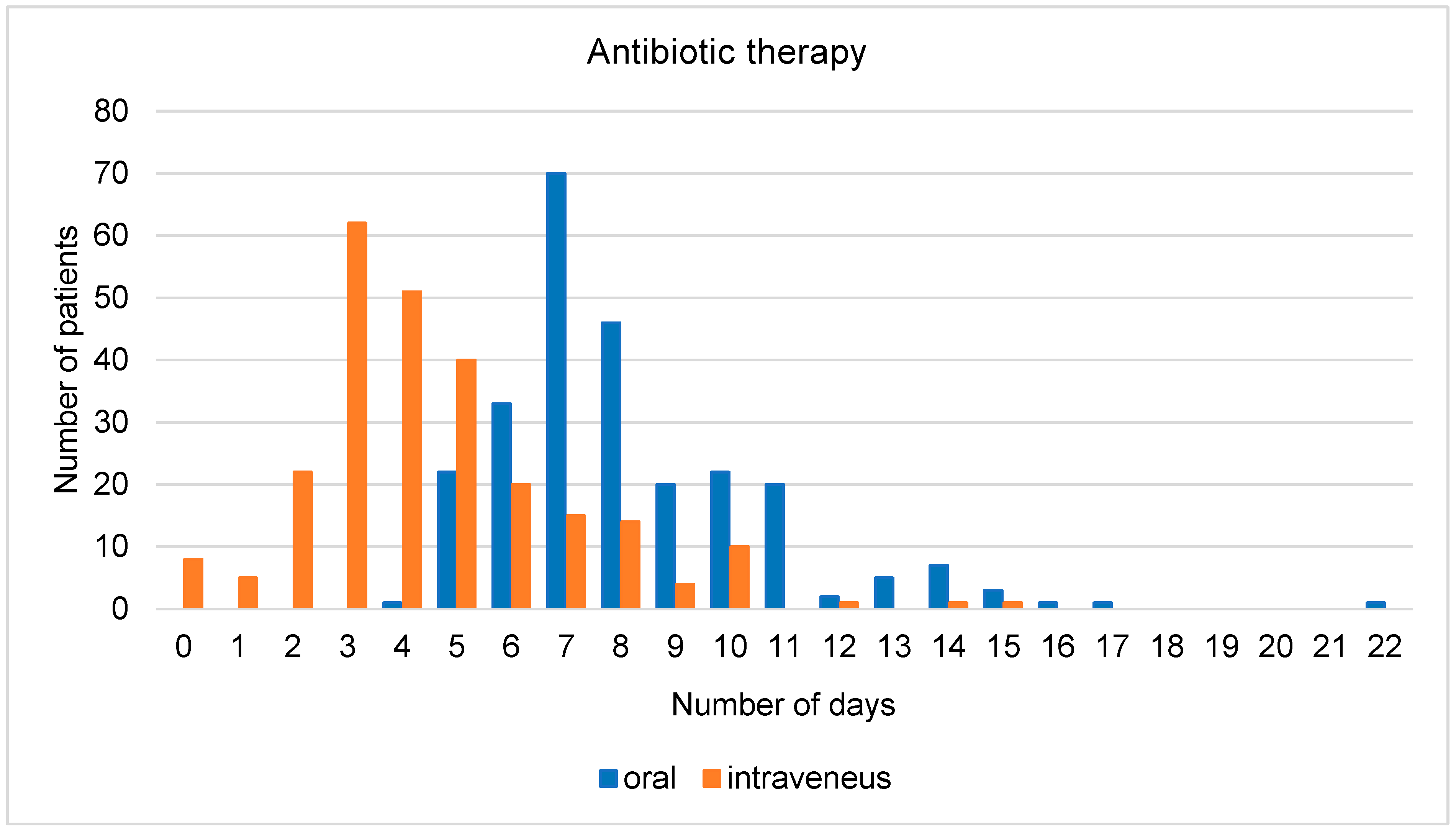
| Length of antibiotic therapy (days) | |
| Total number of days of antibiotic therapy, mean (SD) | 8.2 (±2.5) |
| Number of days of intravenous antibiotic therapy, mean (SD) | 4.3 (±2.4) |
| Number of days of macrolide therapy a (n = 57), mean (SD) | 4.1 (±3.4) |
| Time to antibiotics | |
| All patients b, mean (SD) hours from admission to emergency department to first antibiotic dose administered | 5.0 (±9.3) |
| When received within 24 h (n = 245), mean (SD) | 3.7 (±4.2) |
| Allergy to antibiotics | |
| Penicillin allergy, n (%) | 27 (10.6) |
| Cephalosporin allergy, n (%) | 2 (0.8) |
| Fluoroquinolone allergy, n (%) | 3 (1.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lüthi-Corridori, G.; Roth, A.I.; Boesing, M.; Jaun, F.; Tarr, P.E.; Leuppi-Taegtmeyer, A.B.; Leuppi, J.D. Diagnosis and Therapy of Community-Acquired Pneumonia in the Emergency Department: A Retrospective Observational Study and Medical Audit. J. Clin. Med. 2024, 13, 574. https://doi.org/10.3390/jcm13020574
Lüthi-Corridori G, Roth AI, Boesing M, Jaun F, Tarr PE, Leuppi-Taegtmeyer AB, Leuppi JD. Diagnosis and Therapy of Community-Acquired Pneumonia in the Emergency Department: A Retrospective Observational Study and Medical Audit. Journal of Clinical Medicine. 2024; 13(2):574. https://doi.org/10.3390/jcm13020574
Chicago/Turabian StyleLüthi-Corridori, Giorgia, Andrea I. Roth, Maria Boesing, Fabienne Jaun, Philip E. Tarr, Anne B. Leuppi-Taegtmeyer, and Jörg D. Leuppi. 2024. "Diagnosis and Therapy of Community-Acquired Pneumonia in the Emergency Department: A Retrospective Observational Study and Medical Audit" Journal of Clinical Medicine 13, no. 2: 574. https://doi.org/10.3390/jcm13020574
APA StyleLüthi-Corridori, G., Roth, A. I., Boesing, M., Jaun, F., Tarr, P. E., Leuppi-Taegtmeyer, A. B., & Leuppi, J. D. (2024). Diagnosis and Therapy of Community-Acquired Pneumonia in the Emergency Department: A Retrospective Observational Study and Medical Audit. Journal of Clinical Medicine, 13(2), 574. https://doi.org/10.3390/jcm13020574






