Medication-Related Hospital Admissions and Emergency Department Visits in Older People with Diabetes: A Systematic Review
Abstract
1. Introduction
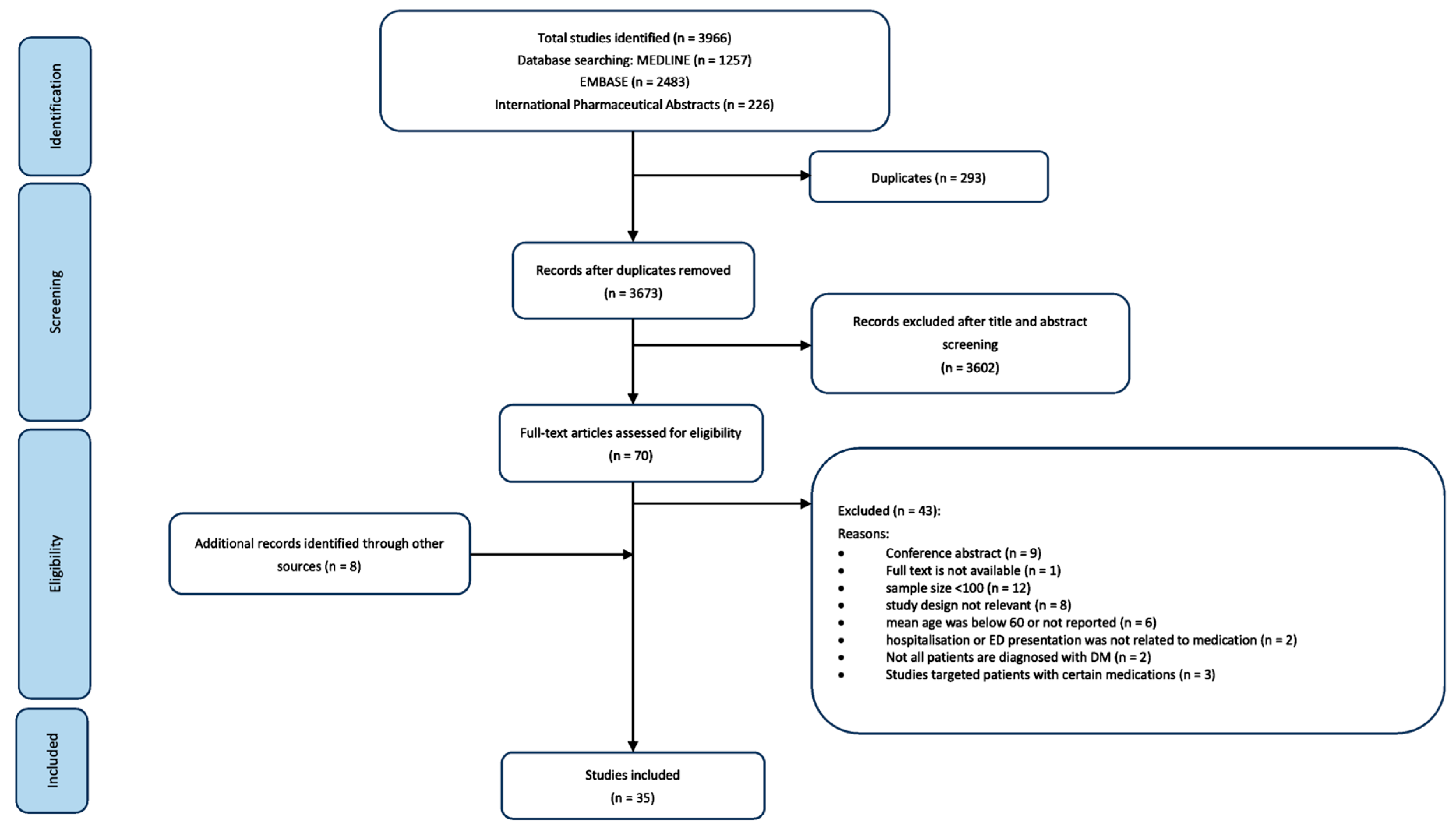
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Overview of Included Studies
3.2. Quality Assessment
3.3. Study and Patient Characteristics
3.4. Trends and Incidence of Hospital Admissions and ED Visits
3.5. Factors Associated with Hospital Admissions and ED Visits
3.5.1. Medications
3.5.2. Other Risk Factors
4. Discussion
4.1. Interpretation of Findings in Relation to Other Studies
4.2. Strength and Limitations
4.3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloom, D.E.; Canning, D.; Lubet, A. Global population aging: Facts, challenges, solutions & perspectives. Daedalus 2015, 144, 80–92. [Google Scholar]
- Silbert, R.; Salcido-Montenegro, A.; Rodriguez-Gutierrez, R.; Katabi, A.; McCoy, R.G. Hypoglycemia among patients with type 2 diabetes: Epidemiology, risk factors, and prevention strategies. Curr. Diabetes Rep. 2018, 18, 53. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ageing. Available online: https://www.who.int/health-topics/ageing (accessed on 28 July 2023).
- Longo, M.; Bellastella, G.; Maiorino, M.I.; Meier, J.J.; Esposito, K.; Giugliano, D. Diabetes and aging: From treatment goals to pharmacologic therapy. Front. Endocrinol. 2019, 10, 45. [Google Scholar] [CrossRef]
- Fialová, D.; Kummer, I.; Držaić, M.; Leppee, M. Ageism in Medication Use in Older Patients; Springer International Publishing: Basel, Swizterland, 2018; pp. 213–240. [Google Scholar]
- Davies, E.A.; O’Mahony, M.S. Adverse drug reactions in special populations-the elderly. Br. J. Clin. Pharmacol. 2015, 80, 796–807. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Older Adults: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, S195–S207. [Google Scholar] [CrossRef]
- Kalyani, R.R.; Golden, S.H.; Cefalu, W.T. Diabetes and Aging: Unique Considerations and Goals of Care. Diabetes Care 2017, 40, 440–443. [Google Scholar] [CrossRef]
- Peron, E.P.; Ogbonna, K.C.; Donohoe, K.L. Antidiabetic Medications and Polypharmacy. Clin. Geriatr. Med. 2015, 31, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Hepler, C.D.; Strand, L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Hosp. Pharm. 1990, 47, 533–543. [Google Scholar] [CrossRef]
- Heaton, P.C.; Desai, V.C.A.; Kelton, C.M.L.; Rajpathak, S.N. Sulfonylurea use and the risk of hospital readmission in patients with type 2 diabetes. BMC Endocr. Disord. 2016, 16, 4. [Google Scholar] [CrossRef]
- Home, P.D.; Fritsche, A.; Schinzel, S.; Massi-Benedetti, M. Meta-analysis of individual patient data to assess the risk of hypoglycaemia in people with type 2 diabetes using NPH insulin or insulin glargine. Diabetes Obes. Metab. 2010, 12, 772–779. [Google Scholar] [CrossRef]
- Leiter, L.A.; Bhatt, D.L.; Mosenzon, O.; Scirica, B.M.; Kumar, P.; Smahelova, A.; Hirshberg, B.; Stahre, C.; Frederich, R.; Bonnici, F.; et al. Efficacy and safety of saxagliptin in older participants in the SAVOR-TIMI 53 trial. Diabetes 2014, 63, A273–A274. [Google Scholar] [CrossRef] [PubMed]
- Han, S.J.; Ha, K.H.; Lee, N.; Kim, D.J. Effectiveness and safety of sodium-glucose co-transporter-2 inhibitors compared with dipeptidyl peptidase-4 inhibitors in older adults with type 2 diabetes: A nationwide population-based study. Diabetes Obes. Metab. 2021, 23, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Zullo, A.R.; Gutman, R.; Smith, R.J.; Mor, V.; Dore, D.D. Comparative safety of dipeptidyl peptidase-4 inhibitors and sulfonylureas in older nursing home residents. J. Am. Geriatr. Soc. 2017, 65, S7. [Google Scholar] [CrossRef]
- Bang, C.; Mortensen, M.B.; Lauridsen, K.G.; Bruun, J.M. Trends in antidiabetic drug utilization and expenditure in Denmark: A 22-year nationwide study. Diabetes Obes. Metab. 2020, 22, 167–172. [Google Scholar] [CrossRef]
- Montvida, O.; Shaw, J.; Atherton, J.J.; Stringer, F.; Paul, S.K. Long-term trends in antidiabetes drug usage in the US: Real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care 2018, 41, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, S.; Douglas, I.; Stirnadel-Farrant, H.; Fogarty, D.; Pokrajac, A.; Smeeth, L.; Tomlinson, L. Changing use of antidiabetic drugs in the UK: Trends in prescribing 2000–2017. BMJ Open 2018, 8, e022768. [Google Scholar] [CrossRef]
- Yang, A.; Wu, H.; Lau, E.S.H.; Ma, R.C.W.; Kong, A.P.S.; So, W.Y.; Luk, A.O.Y.; Chan, J.C.N.; Chow, E. Trends in Glucose-Lowering Drug Use, Glycemic Control, and Severe Hypoglycemia in Adults with Diabetes in Hong Kong, 2002–2016. Diabetes Care 2020, 43, 2967–2974. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Dhaliwal, R.; Weinstock, R.S. Management of Type 1 Diabetes in Older Adults. Diabetes Spectr. 2014, 27, 9–20. [Google Scholar] [CrossRef]
- Sotiropoulos, A.; Skliros, E.; Tountas, C.; Apostolou, U.; Peppas, T.; Pappas, S. Risk factors for severe hypoglycaemia in type 2 diabetic patients admitted to hospital in Piraeus, Greece. East. Mediterr. Health J. 2005, 11, 485–489. [Google Scholar] [CrossRef]
- Greco, D.; Pisciotta, M.; Gambina, F.; Maggio, F. Severe hypoglycaemia leading to hospital admission in type 2 diabetic patients aged 80 years or older. Exp. Clin. Endocrinol. Diabetes 2010, 118, 215–219. [Google Scholar] [CrossRef]
- Feil, D.G.; Rajan, M.; Soroka, O.; Tseng, C.-L.; Miller, D.R.; Pogach, L.M. Risk of hypoglycemia in older veterans with dementia and cognitive impairment: Implications for practice and policy. J. Am. Geriatr. Soc. 2011, 59, 2263–2272. [Google Scholar] [CrossRef] [PubMed]
- Tschöpe, D.; Bramlage, P.; Binz, C.; Krekler, M.; Deeg, E.; Gitt, A.K. Incidence and predictors of hypoglycaemia in type 2 diabetes–an analysis of the prospective DiaRegis registry. BMC Endocr. Disord. 2012, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Xie, W.; Curtis, B.; Schuster, D. Identifying factors associated with hypoglycemia-related hospitalizations among elderly patients with T2DM in the US: A novel approach using influential variable analysis. Curr. Med. Res. Opin. 2014, 30, 1787–1793. [Google Scholar] [CrossRef]
- Nazish, Z.; Inayatullah, M.; Mustafa, F. Risk factors of hypoglycemia in diabetics. Med. Forum Mon. 2014, 25, 38–42. [Google Scholar]
- Liatis, S.; Mylona, M.; Kalopita, S.; Papazafiropoulou, A.; Karamagkiolis, S.; Melidonis, A.; Xilomenos, A.; Ioannidis, I.; Kaltsas, G.; Lanaras, L. Hypoglycaemia requiring medical assistance in patients with diabetes: A prospective multicentre survey in tertiary hospitals. Diabetes Metab. 2015, 41, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Salutini, E.; Bianchi, C.; Santini, M.; Dardano, A.; Daniele, G.; Penno, G.; Miccoli, R.; Del Prato, S. Access to emergency room for hypoglycaemia in people with diabetes. Diabetes Metab. Res. Rev. 2015, 31, 745–751. [Google Scholar] [CrossRef]
- Kim, H.M.; Seong, J.M.; Kim, J. Risk of hospitalization for hypoglycemia among older Korean people with diabetes mellitus: Interactions between treatment modalities and comorbidities. Medicine 2016, 95, e5016. [Google Scholar] [CrossRef]
- Mantovani, A.; Grani, G.; Chioma, L.; Vancieri, G.; Giordani, I.; Rendina, R.; Rinaldi, M.E.; Andreadi, A.; Coccaro, C.; Boccardo, C. Severe hypoglycemia in patients with known diabetes requiring emergency department care: A report from an Italian multicenter study. J. Clin. Transl. Endocrinol. 2016, 5, 46–52. [Google Scholar] [CrossRef]
- Hung, Y.; Lin, C.; Chen, H.; Chang, M.; Huang, K.; Chen, Y.; Chen, C. Severe hypoglycemia and hip fracture in patients with type 2 diabetes: A nationwide population-based cohort study. Osteoporos. Int. 2017, 28, 2053–2060. [Google Scholar] [CrossRef]
- Mazzi, S.; Ravasio, R.; Forlani, G.; Veronese, G.; Fabbri, A.; Marchesini, G. Estimating the risk of severe hypoglycemic event related to glucose-lowering treatment among Italian patients with diabetes: The HYPOTHESIS database. Clin. Outcomes Res. 2017, 9, 711–720. [Google Scholar] [CrossRef]
- Zhong, V.W.; Juhaeri, J.; Cole, S.R.; Kontopantelis, E.; Shay, C.M.; Gordon-Larsen, P.; Mayer-Davis, E.J. Incidence and trends in hypoglycemia hospitalization in adults with type 1 and type 2 diabetes in England, 1998–2013: A retrospective cohort study. Diabetes Care 2017, 40, 1651–1660. [Google Scholar] [CrossRef] [PubMed]
- Conceição, J.; Dores, J.; Araújo, F.; Laires, P.A.; Carr, R.D.; Brodovicz, K.; Radican, L.; Nogueira, A.M. Severe hypoglycaemia among patients with type 2 diabetes requiring emergency hospital admission: The Hypoglycaemia in Portugal Observational Study–Emergency Room (HIPOS–ER). Diabetes Obes. Metab. 2018, 20, 50–59. [Google Scholar] [CrossRef]
- Misra-Hebert, A.D.; Pantalone, K.M.; Ji, X.; Milinovich, A.; Dey, T.; Chagin, K.M.; Bauman, J.M.; Kattan, M.W.; Zimmerman, R.S. Patient characteristics associated with severe hypoglycemia in a type 2 diabetes cohort in a large, integrated health care system from 2006 to 2015. Diabetes Care 2018, 41, 1164–1171. [Google Scholar] [CrossRef]
- Namba, M.; Iwakura, T.; Nishimura, R.; Akazawa, K.; Matsuhisa, M.; Atsumi, Y.; Satoh, J.; Yamauchi, T. The current status of treatment-related severe hypoglycemia in Japanese patients with diabetes mellitus: A report from the committee on a survey of severe hypoglycemia in the Japan Diabetes Society. J. Diabetes Investig. 2018, 9, 642–656. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-Y.; Jang, E.J.; Shin, J.-Y.; Lee, M.-Y.; Kim, D.; Lee, E.-K. Prevalence and predictors of hypoglycemia in South Korea. Am. J. Manag. Care 2018, 24, 278–286. [Google Scholar]
- Caballero-Corchuelo, J.; Guerrero-Perez, F.; Garcia-Sancho de la Jordana, P.; Perez-Maraver, M. Analysis of the characteristics of patients with diabetes mellitus who attend a tertiary hospital emergency department for a hypoglycemic event. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2019, 66, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Kaewput, W.; Thongprayoon, C.; Varothai, N.; Sirirungreung, A.; Rangsin, R.; Bathini, T.; Mao, M.A.; Cheungpasitporn, W. Prevalence and associated factors of hospitalization for dysglycemia among elderly type 2 diabetes patients: A nationwide study. World J. Diabetes 2019, 10, 212. [Google Scholar] [CrossRef] [PubMed]
- Andreano, A.; Bosio, M.; Russo, A.G. Emergency attendance for acute hyper-and hypoglycaemia in the adult diabetic population of the metropolitan area of Milan: Quantifying the phenomenon and studying its predictors. BMC Endocr. Disord. 2020, 20, 72. [Google Scholar] [CrossRef] [PubMed]
- McCoy, R.G.; Lipska, K.J.; Van Houten, H.K.; Shah, N.D. Association of cumulative multimorbidity, glycemic control, and medication use with hypoglycemia-related emergency department visits and hospitalizations among adults with diabetes. JAMA Netw. Open 2020, 3, e1919099. [Google Scholar] [CrossRef]
- Müller, N.; Lehmann, T.; Klöss, A.; Günster, C.; Kloos, C.; Müller, U.A. Changes in incidence of severe hypoglycaemia in people with type 2 diabetes from 2006 to 2016: Analysis based on health insurance data in Germany considering the anti-hyperglycaemic medication. Diabet. Med. 2020, 37, 1326–1332. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.A.; Almeida, R.; Dores, J. Characteristics of hypoglycaemic episodes in diabetic patients treated at the emergency room of a Portuguese tertiary centre, 2012–2016. Endocrinol. Diabetes Metab. 2020, 3, e00150. [Google Scholar] [CrossRef] [PubMed]
- Bengtsen, M.B.; Knudsen, J.S.; Bengtsen, M.B.; Møller, N.; Thomsen, R.W. Hospitalization for hypoglycaemia in people with diabetes in Denmark, 1997–2017: Time trends in incidence and HbA1c and glucose-lowering drug use before and after hypoglycaemia. Endocrinol. Diabetes Metab. 2021, 4, e00227. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.H.; Hejlesen, O.; Vestergaard, P. Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998–2018. Diabetologia 2021, 64, 2193–2203. [Google Scholar] [CrossRef] [PubMed]
- Lacy, M.E.; Whitmer, R.A.; Lee, S.J.; Rushakoff, R.J.; Pletcher, M.J. Identifying Potential Intervention Points for Acute Hypoglycemic Events in Patients with Type 2 Diabetes Using Retrospective Clinical Data. Clin. Diabetes 2021, 39, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Kim, K.-A.; Son, K.J.; Song, S.O.; Park, K.H.; Park, S.H.; Nam, J.Y. Trends and risk factors in severe hypoglycemia among individuals with type 2 diabetes in Korea. Diabetes Res. Clin. Pract. 2021, 178, 108946. [Google Scholar] [CrossRef]
- Pilla, S.J.; Kraschnewski, J.L.; Lehman, E.B.; Kong, L.; Francis, E.; Poger, J.M.; Bryce, C.L.; Maruthur, N.M.; Yeh, H.-C. Hospital utilization for hypoglycemia among patients with type 2 diabetes using pooled data from six health systems. BMJ Open Diabetes Res. Care 2021, 9, e002153. [Google Scholar] [CrossRef]
- Chen, N.-C.; Chen, C.-L.; Shen, F.-C. The Risk Factors of Severe Hypoglycemia in Older Patients with Dementia and Type 2 Diabetes Mellitus. J. Pers. Med. 2022, 12, 67. [Google Scholar] [CrossRef]
- Galea, A.; Farrugia, S.; Calleja, N.; Coppini, D.V. Risk factors and outcomes of severe hypoglycaemia requiring hospital admission: A retrospective study. Pract. Diabetes 2022, 39, 19. [Google Scholar] [CrossRef]
- Galindo, R.J.; Ali, M.K.; Funni, S.A.; Dodge, A.B.; Kurani, S.S.; Shah, N.D.; Umpierrez, G.E.; McCoy, R.G. Hypoglycemic and hyperglycemic crises among US adults with diabetes and end-stage kidney disease: Population-based study, 2013–2017. Diabetes Care 2022, 45, 100–107. [Google Scholar] [CrossRef]
- Nuzzo, A.; Brignoli, A.; Ponziani, M.C.; Zavattaro, M.; Prodam, F.; Castello, L.M.; Avanzi, G.C.; Marzullo, P.; Aimaretti, G. Aging and comorbidities influence the risk of hospitalization and mortality in diabetic patients experiencing severe hypoglycemia. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Poret, F.; Nacher, M.; Pujo, J.; Cauvin, J.M.; Demar, M.; Massicard, M.; Sabbah, N. Risk factors for hypoglycaemia in people with diabetes admitted to the Emergency Department of a Hospital in French Guiana. Diabet. Med. 2022, 39, e14736. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.S.; Han, K.; Ko, S.H. Trends of severe hypoglycemia in patients with type 2 diabetes in Korea: A longitudinal nationwide cohort study. J. Diabetes Investig. 2022, 13, 1438–1443. [Google Scholar] [CrossRef] [PubMed]
- Horii, T.; Otsuka, M.; Yasu, T. Risk of non-hypoglycemic agents for hypoglycemia-related hospitalization in patients with type 2 diabetes: A large-scale medical receipt database analysis. BMJ Open Diabetes Res. Care 2023, 11, e003177. [Google Scholar] [CrossRef]
- Davis, T.M.; Brown, S.G.; Jacobs, I.G.; Bulsara, M.; Bruce, D.G.; Davis, W.A. Determinants of severe hypoglycemia complicating type 2 diabetes: The Fremantle diabetes study. J. Clin. Endocrinol. Metab. 2010, 95, 2240–2247. [Google Scholar] [CrossRef]
- Linkens, A.; Milosevic, V.; van der Kuy, P.H.M.; Damen-Hendriks, V.H.; Mestres Gonzalvo, C.; Hurkens, K. Medication-related hospital admissions and readmissions in older patients: An overview of literature. Int. J. Clin. Pharm. 2020, 42, 1243–1251. [Google Scholar] [CrossRef] [PubMed]
- Abigail, S.; Joanne, M.; Mark, A.; Stuart, M.; Tara, Q.; Alastair, L.; Martin, S.; Theodore, I.; Pamela, M. Medication-related problems in critical care survivors: A systematic review. Eur. J. Hosp. Pharm. 2023, 30, 1–7. [Google Scholar]
- El Morabet, N.; Uitvlugt, E.B.; Van Den Bemt, B.J.F.; Van Den Bemt, P.M.L.A.; Janssen, M.J.A.; Karapinar-Çarkit, F. Prevalence and Preventability of Drug-Related Hospital Readmissions: A Systematic Review. J. Am. Geriatr. Soc. 2018, 66, 602–608. [Google Scholar] [CrossRef]
- Topaz, M.; Shafran-Topaz, L.; Bowles, K.H. ICD-9 to ICD-10: Evolution, revolution, and current debates in the United States. Perspect. Health Inf. Manag. 2013, 10, 1d. [Google Scholar]
- Cartwright, D.J. ICD-9-CM to ICD-10-CM codes: What? why? how? Adv. Wound Care 2013, 2, 588–592. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Older Adults: Standards of Medical Care in Diabetes—2024. Diabetes Care 2024, 47, S244–S257. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2022, 65, 1925–1966. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Feng, L.; Yao, H.; Yang, L.; Qin, Y. Efficacy and safety of diazoxide for treating hyperinsulinemic hypoglycemia: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246463. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.N.; Shavers, C.; Costa, F. Gender-Related Differences in Counterregulatory Responses to Antecedent Hypoglycemia in Normal Humans1. J. Clin. Endocrinol. Metab. 2000, 85, 2148–2157. [Google Scholar] [CrossRef]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef]
- Östgren, C.J.; Lindblad, U.; Ranstam, J.; Melander, A.; Råstam, L. Glycaemic control, disease duration and β-cell function in patients with Type 2 diabetes in a Swedish community. Skaraborg Hypertension and Diabetes Project. Diabet. Med. 2002, 19, 125–129. [Google Scholar] [CrossRef]
- Bruce, D.; Davis, W.; Casey, G.; Clarnette, R.; Brown, S.; Jacobs, I.; Almeida, O.; Davis, T. Severe hypoglycaemia and cognitive impairment in older patients with diabetes: The Fremantle Diabetes Study. Diabetologia 2009, 52, 1808–1815. [Google Scholar] [CrossRef]
| Author, Year, Country | Study Design | Data Sources | Years Reported (Duration) (Years) | Type of Diabetes | Patients’ Age (Mean [SD]/Median [IQR]) (Years) | Outcome Observed (Diagnosis Code) | Trend or Events of Outcome Observed |
|---|---|---|---|---|---|---|---|
| Studies that reported medication-related hospital admissions and/or emergency department (ED) visits as the trend over time | |||||||
| Zhong et al. (2017), UK [34] | retrospective, cohort | patients’ registry | 1998–2013 (16) | T2DM | 100% ≥65 years | hospitalisations due to hypoglycaemia (ICD-10) | (Annual percent change [95% CI]) Decreased: 1998–2009: 8.59 [5.76–11.50]; 2009–2013: −8.05 [−14.48 to −1.13] of older adult patients with T2DM. |
| Misra-Hebert et al. (2018), US [36] | retrospective, cohort | hospital medical record | 2006–2015 (10) | T2DM | 61.0 (51.9, 69.9) | ED visits or hospitalisations due to hypoglycaemia (ICD-9/-10) | (Percentage [%]) Increased: 2006–2015: 0.12 to 0.31 (p = 0.01) of patients with T2DM who had either a primary care or endocrinology visit within 2 years. |
| Müller et al. (2020), Germany [43] | retrospective, cohort | administrative database | 2006, 2011, 2016 (1) | T2DM | 2006: 72.8 (12.4); 2011: 73.4 (12.3); 2016: 73.0 (13.2) | ED visits or hospitalisations due to hypoglycaemia (ICD-10) | (Events per 100,000 people) Decreased: 2006 = 460; 2011: 490; 2016: 360 of patients with T2DM. |
| Pereira et al. (2020), Portugal [44] | retrospective, prevalence | hospital medical record | 2012–2016 (5) | T1DM and T2DM | 71 (57–81) | ED visits due to hypoglycaemia (ICD-9) | (Percentage [%]) Decreased: 0.15% in 2012 to 0.10% in 2016 (p < 0.001) of all ED visits. |
| Bengtsen et al. (2021), Denmark [45] | retrospective, case-control | administrative database | 1997–2017 (21) | T1DM and T2DM | 73.70 (63.60, 81.50) | hospitalisations due to hypoglycaemia (ICD-10) | (Events per 100,000 people) Decreased: 1997–2003: 17.7–30.3; 2010: 30.4; 2017: 22.0 of patients with diabetes. |
| Jensen et al. (2021), Denmark [46] | retrospective, cohort | administrative database | 1998–2018 (21) | T2DM | 61 (17) | hospitalisations due to hypoglycaemia (ICD-10) | (Events per 100,000 people) Decreased: 1998: 700; 2003: 1100; 2018: 400 of patients with T2DM. |
| Lee et al. (2021), Korea [48] | retrospective, analytical cross-sectional | administrative database | 2006–2015 (10) | T2DM | 100% ≥65 years | ED visits or hospitalisations due to hypoglycaemia (ICD-10) | (Events per 100,000 people) Decreased: 2006–2010: 859 to 1327, 2011–2015: 1262 to 1060 of T2DM people aged 65 years or older. |
| Pilla et al. (2021), US [49] | retrospective, cohort | hospital medical record | 2009–2019 (11) | T2DM | 61.0 (14.3); 47% ≥65 years in 2014 | ED visits or hospitalisations due to hypoglycaemia (ICD-9 and ICD-10) | (Events per 100,000 people) Decreased: 2009: 270; 2014: 160 (ICD-9). Increased: 2016: 560, 2019: 660 (limited ICD-10); 2016: 630, 2019: 730 (expanded ICD-10) of patients with T2DM who had either a primary care or endocrinology visit within 3 years. |
| Galindo et al. (2022), US [52] * | retrospective, cohort | patients’ registry | 2013–2017 (5) | not specified | 65.0 (57.0–73.0) | ED visits or hospitalisations due to hypoglycaemia (ICD-9 and ICD-10) | (Events per 100,000 people) Decreased: 2013: 6400; 2017:4750 |
| Yun et al. (2022), Korea [55] | retrospective, cohort | administrative database | 2002–2019 (18) | T2DM | more than 50% are people ≥ 65 years | ED visits due to hypoglycaemia (ICD-10) | (Events per 100,000 people) Decreased from 2013 to 2019 2003–2012: 356 to 684, 2013–2019: 650 to 443 of patients with T2DM. |
| Studies that reported medication-related hospital admissions and/or emergency department (ED) visits as events during time period | |||||||
| Sotiropoulos et al. (2005), Greece [22] | prospective, analytical, cross-sectional | hospital medical record | 1996–1999 (3) | T2DM | 62.1 (8.7) | hospitalisations due to hypoglycaemia (NA) | 207 out of 2858 T2DM patients admitted to hospital (7.2%). |
| Greco et al. (2010), Italy [23] | prospective, prevalence | hospital medical record | 2001–2008 (8) | T2DM | 84.7 (4.3) (100% ≥80 years) | hospitalisations due to hypoglycaemia (NA) | 99 patients out of 591 medical admissions due to diabetes in patients ≥80 years. |
| Feil et al. (2011), US [24] | Prospective, analytical, cross-sectional | administrative database | 2002–2003 (1) | not specified | 100% ≥65 years | ED visits or hospitalisations due to hypoglycaemia (ICD-9) | 37,343 patients out of 497,900 veterans with diabetes mellitus aged 65 and older (7.5%). |
| Tschöpe et al. (2012), Germany [25] | prospective, cohort | patients’ registry | June 2009–March 2010 (1) | T2DM | 66.8 (57.8–74.1) | hospitalisations due to hypoglycaemia (NA) | 13 patients out of 3347 patients with T2DM (0.4%). |
| Fu et al. (2014), US [26] | retrospective, cohort | administrative database | 2007–2010 (4) | T2DM | 30.7% ≥65 years | hospitalisations due to hypoglycaemia (ICD-9) | 0.006 per 1000 people in hospitalised T2DM patients. |
| Nazish et al. (2014), Pakistan [27] | prospective, prevalence | hospital medical record | 2010–2013 (4) | not specified | 60.46 (14.20) | ED visits or hospitalisations due to hypoglycaemia (NA) | 118 patients. |
| Liatis et al. (2014), Greece [28] | prospective, case-control | hospital medical record | Not reported (1.375) | T2DM | 76.7 (10.1) | ED visits due to hypoglycaemia (Whipple’s triad) | 268 patients. |
| Salutini et al. (2015), Italy [29] | retrospective, analytical, cross-sectional | hospital medical record | 2009–2013 (5) | T1DM and T2DM | 71 (16) | ED visits due to hypoglycaemia (ICD-9) | 500 episodes (401 patients). |
| Kim et al. (2016), Korea [30] | retrospective, analytical, cross-sectional | administrative database | 2013 (1) | not specified | 100% ≥65 years | ED visits or hospitalisations due to hypoglycaemia (ICD-10) | 9.93 per 1000 people in patients with diabetes. |
| Mantovani et al. (2016), Italy [31] | retrospective, analytical, cross-sectional | hospital medical record | 2010–2014 (5) | T2DM | 75 (13) | ED visits due to hypoglycaemia (NA) | 444 patients. |
| Hung et al. (2017), Taiwan [32] | retrospective, analytical, cross-sectional | administrative database | 2001–2009 (9) | T2DM | 70.1 (12.2) | ED visits or hospitalisations due to hypoglycaemia (ICD-9) | 2588 out of 87,029 patients with T2DM (2.97%) in the one million Taiwan administrative database. |
| Mazzi et al. (2017), Italy [33] | retrospective, analytical, cross-sectional | hospital medical record | 2011 (1) | T1DM and T2DM | 71.5 (16.8) | ED visits or hospitalisations due to hypoglycaemia (NA) | 1922 episodes of treated patients with diabetes. |
| Conceição et al. (2017), Portugal [35] | prospective, analytical, cross sectional | hospital medical record | Jan 2013–Jan 2014 (1) | T2DM | 77.5 (45; 97) | ED visits due to hypoglycaemia (Whipple’s triad) | 0.074% (95% CI 0.066–0.082) of all ED visits. |
| Namba et al. (2018), Japan [37] | retrospective, prevalence | hospital medical record | April 2014–March 2015 (5) | T1DM and T2DM | 71.5 (58.0–81.0) | ED visits due to hypoglycaemia (NA) | 2237 patients out of 346,939 patients with diabetes admitted to ED. |
| Park et al. (2018), Korea [38] | retrospective, cohort | administrative database | 2011–2013 (3) | T2DM | 60.79 (12.20) | ED visits or hospitalisations due to hypoglycaemia (KCD-7) | 0.96% among pharmacologically treated patients with T2DM. |
| Caballero-Corchuelo et al. (2019), Spain [39] | retrospective, analytical, cross-sectional | hospital medical record | 2012–2014 (3) | T2DM | 75.4 | ED visits due to hypoglycaemia (NA) | 122 patients. |
| Kaewput et al. (2019), Thailand [40] | retrospective, analytical, cross-sectional | patients’ registry | 2014 (1) | T2DM | 100% ≥65 years | hospitalisations due to hypoglycaemia (NA) | 356 patients out of 11,404 older adult patients with T2DM (3.1%). |
| Andreano et al. (2020), Italy [41] | retrospective, cohort | administrative database and hospital medical record | 2015–2017 (3) | T1DM and T2DM | 76.2% ≥65 years | ED visits due to hypoglycaemia (ICD-9) | 2137 patients out of 168,285 residents recorded with DM and treated with antidiabetic medications (1.27%) (or 4.7 per 1000 patient-years). |
| McCoy et al. (2020), US [42] | retrospective, cohort | administrative database | 2014–2016 (3) | T1DM and T2DM | 65.8 (12.1) | ED visits or hospitalisations due to hypoglycaemia (ICD-9 and 10) | 9.06 per 1000 people in patients with diabetes. |
| Lacy et al. (2021), US [47] | retrospective, cohort | hospital medical record | 2012–2017 (6) | T2DM | 60.9 (15.2) | ED visits or hospitalisations due to hypoglycaemia (ICD-10) | 22.6 per 1000 people in treated patients with T2DM. |
| Chen et al. (2022), Taiwan [50] ** | retrospective, cohort | hospital medical record | 2001–2018 (18) | T2DM | 77.5 (8.9) | ED visits (ICD-9) | 494 patients out of 3877 patients with Alzheimer’s Dementia (AD) and with concomitant T2DM (12.74%) |
| Galea et al. (2022), Malta [51] | retrospective, cross-sectional | hospital medical record | 2018 (1) | T1DM and T2DM | 71.5 (15.5) | ED visits or hospitalisations due to hypoglycaemia (NA) | 167 episodes out of 21,589 medical admissions (0.77%). |
| Nuzzo et al. (2022), Italy [53] | retrospective, analytical, cross-sectional | hospital medical record | 2013–2017 (5) | T1DM and T2DM | 75 (17) | ED visits due to hypoglycaemia (ICD-9) | 302 patients. |
| Poret et al. (2022), France [54] | retrospective, prevalence | hospital medical record | 2015–2018 (4) | T1DM and T2DM | 68 (58–75) | ED visits or hospitalisations due to hypoglycaemia (ICD-10) | 178 patients. |
| Horii et al. (2023), Japan [56] | retrospective, cross-sectional | administrative database | April 2014-October 2019 (5) | T2DM | 70.4 (12.3) | hospitalisations due to hypoglycaemia (ICD-10) | 10,376 patients out of 703,745 (1.47%). |
| Associated Factors | Increased Risk [Odd Ratio (OR)/Incidence Rate Ratios (IRR)/Hazard Ratio (95% CI)] | Decreased Risk [Odd Ratio (OR)/Incidence Rate Ratios (IRR) (95% CI)] |
|---|---|---|
| Medications | ||
| Insulin analogues | 14.40 (13.50–15.50) [43] | |
| Basal insulin | 12.53 (8.90–17.64) [42] | |
| Basal insulin | 23.21 (15.71–34.27) [42] | |
| Mixed insulin | 13.50 (12.70–14.50) [43] | |
| 27.65 (20.32–37.63) [42] | ||
| Human insulin | 11.20 (10.50–12.00) [43] | |
| Insulin | 2.13 (1.67–2.73) [49], 2.77 (1.98–3.89) [36] | |
| 7.44 (6.63–8.36) [38], 2.00 (1.31–3.05) [41] | ||
| 6.59 (4.43–9.79) [25], 4.51 (3.49–5.83) [48] | ||
| 1.73 (1.67–1.79) [55], 2.35 (1.42–3.95) [28] | ||
| 4.20 (3.39–5.19) [26], 4.68 (3.84–5.71) [50] | ||
| 13.92 (11.23–17.27) [30], 3.41 (1.69–6.86) [47] | ||
| 3.44 (3.25–3.64) [56] | ||
| 0.66 (0.50–0.88) [33] | ||
| Insulin and sulfonylureas | 4.74 (3.67–6.06) [26], 15.09 (13.60–16.74) [38] | |
| Sulfonylureas | 5.70 (5.30–6.10) [43], 2.49 (1.92–3.22) [36] | |
| 3.29 (2.61–4.14) [48], 6.73 (4.93–9.22) [42] | ||
| 1.94 (1.53–2.47) [55], 4.00 (2.51–6.36) [28] | ||
| 5.71 (2.92–11.17) [35] *, 3.94 (3.42–4.55) [26] | ||
| 1.98 (1.79–2.18) [38], 13.92 (11.23–17.27) [30] | ||
| 2.27 (2.18–2.37) [46] | ||
| Non- Sulfonylureas secretagogues (Glinides) | 2.23 (1.79–2.18) [38], 1.38 (1.22–156) [56] | |
| Thiazolidinediones | 1.82 (1.27–2.61) [48], 1.58 (1.24–2.00) [55] | |
| 1.92 (1.35–2.74) [50] | ||
| DPP-4 inhibitor | 0.51 (0.35–0.74) [36], 0.97 (0.75–1.23) [26] | |
| 0.44 (0.38–0.49) [46], 0.52 (0.26–1.03) [25] | ||
| DPP-4 inhibitor (linagliptin) | 1.62 (1.55–1.69) [56] | |
| DPP-4 inhibitor (sitagliptin)) | 1.05 (1.01–1.10) [56] | |
| DPP-4 inhibitor (teneligliptin) | 1.23 (1.16–1.31) [56] | |
| DPP-4 inhibitor (vildagliptin) | 1.29 (1.23–1.36) [56] | |
| GLP-1 agonist | 1.59 (1.44–1.77) [56] | |
| 0.23 (0.08–0.62) [36], 0.51 (0.44–0.58) [46] | ||
| 0.62 (0.36–0.99) [26] | ||
| Metformin | 0.43 (0.32–0.58) [36], 0.69 (0.54–0.87) [55] | |
| 0.39 (0.16–0.93) [47], 0.72 (0.69–0.72) [56] | ||
| SGLT2 inhibitor | 0.43 (0.33–0.56) [46], 0.65 (0.58–0.74) [56] | |
| Non-diabetic medications | ||
| Diazoxide | 15.49 (4.87–49.31) [56] | |
| Methylphenidate | 5.15 (1.53–17.28) [56] | |
| Disulfiram | 4.21 (2.05–8.62) [56] | |
| Corticosteroid | 2.03 (1.70–2.44) [56] | |
| 0.78 (0.74–0.83) [46] | ||
| Antidepressants | 1.11 (1.02–1.21) [46] | |
| Opioids | 0.84 (0.80–0.88) [46] |
| Associated Factors | Increased Risk [Odd Ratio (OR)/Incidence Rate Ratios (IRR)/Hazard Ratio (95% CI)] | Decreased Risk [Odd Ratio (OR)/Incidence Rate Ratios (IRR) (95% CI)] |
|---|---|---|
| Gender (female) | 1.13 (1.10–1.20) [43], 1.32 (1.08–1.61) [49] | |
| 1.05 (1.02–1.08) [55], 1.63 (1.04–2.56) [40] | ||
| 1.12 (1.04–1.21) [30], 1.05 (1.01–1.10) [56] | ||
| 1.09 (1.06–1.12) [52] | ||
| Older age | 1.58 (1.23–2.02) [42], 1.80 (1.37–2.35) [40] | |
| 1.30 (1.20–1.45) [28], 3.00 (2.64–3.41) [30] | ||
| 1.03 (1.02–1.04) [33], 2.99 (2.71–3.30) [46] | ||
| 1.1 (1.04–1.16) [56] | ||
| Longer duration of diabetes | 1.02 (1.01–1.03) [47], 2.45 (2.29–2.61) [46] | |
| Increased number of diabetes medications | 1.56 (1.36–1.79) [36], 4.00 (2.87–5.58) [48] | 1.10 (0.51–2.46) [53] |
| Duration of insulin use | 0.62 (0.52–0.74) [41] | |
| HbA1c < 6% | 1.95 (1.44–2.65) [36], 2.00 (1.33–2.94) [49] | |
| 1.45 (1.12–1.87) [42] | ||
| HbA1C (≥8.5) | 1.49 (1.06–2.09) [40], 2.01 (1.31–3.07) [47] | |
| 1.56 (1.05–2.33) [49] | ||
| Previous hypoglycaemia | 3.01 (2.09–4.34) [36], 8.47 (8.16–8.80) [55] | |
| 6.60 (5.77–7.56) [42], 5.34 (3.93–7.26) [41] | ||
| 3.30 (1.89–5.35) [26], 7.74 (6.82–8.79) [38] | ||
| Lower BMI | 1.61 (1.54–1.69) [56] | |
| Higher BMI | 0.44 (0.33–0.60) [40], 0.96 (0.94–0.98) [36] | |
| Higher number of comorbidities | 1.74 (1.34–2.27) [28], 1.56 (1.41–1.73) [33] | |
| 1.79 (1.37–2.3) [47], 4.12 (3.07–5.51) [42] | ||
| Increased Charlson comorbidity index | 1.15 (1.10–1.21) [36], 2.76 (1.82–4.18) [48] 8.84 (6.85–11.40) [38] | |
| Cardiovascular disease | 1.68 (1.24–2.28) [36], 1.20 (1.15–1.25) [38] | |
| 2.21 (1.71–284) [50] | ||
| Hypertension | 1.29 (1.25–1.34) [55], 1.63 (1.04–2.56) [40] | |
| Kidney disease | 10.30 (10.10–10.60) [43], 2.86 (2.33–3.57) [49] | |
| 1.59 (1.12–2.11) [40], 2.96 (1.51–6.11) [53] | ||
| 4.53 (2.59–7.95) [28], 1.38 (1.20–1.57) [26] | ||
| 2.52 (2.26–2.82) [30], 2.03 (1.09–4.20) [31] | ||
| 1.71 (1.62–1.81) [38], 2.96 (2.01–4.35) [47] | ||
| 1.56 (1.22–1.98) [33], 2.98 2.46–3.62) [50] | ||
| Cognitive impairment/dementia | 2.57 (1.85–3.56) [49], 6.98 (1.80–26.98) [40] | |
| 1.93 (1.76–2.12) [30], 10.16 (3.40–30.36) [28] | ||
| 1.45 (1.08–1.95) [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vonna, A.; Salahudeen, M.S.; Peterson, G.M. Medication-Related Hospital Admissions and Emergency Department Visits in Older People with Diabetes: A Systematic Review. J. Clin. Med. 2024, 13, 530. https://doi.org/10.3390/jcm13020530
Vonna A, Salahudeen MS, Peterson GM. Medication-Related Hospital Admissions and Emergency Department Visits in Older People with Diabetes: A Systematic Review. Journal of Clinical Medicine. 2024; 13(2):530. https://doi.org/10.3390/jcm13020530
Chicago/Turabian StyleVonna, Azizah, Mohammed S. Salahudeen, and Gregory M. Peterson. 2024. "Medication-Related Hospital Admissions and Emergency Department Visits in Older People with Diabetes: A Systematic Review" Journal of Clinical Medicine 13, no. 2: 530. https://doi.org/10.3390/jcm13020530
APA StyleVonna, A., Salahudeen, M. S., & Peterson, G. M. (2024). Medication-Related Hospital Admissions and Emergency Department Visits in Older People with Diabetes: A Systematic Review. Journal of Clinical Medicine, 13(2), 530. https://doi.org/10.3390/jcm13020530








