Trends in the Incidence of Cardiovascular Diagnoses and Procedures over the Years 2012–2021 in Israel: The Impact of the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Source Population
2.2. Variables
2.3. Statistical Analysis
3. Results
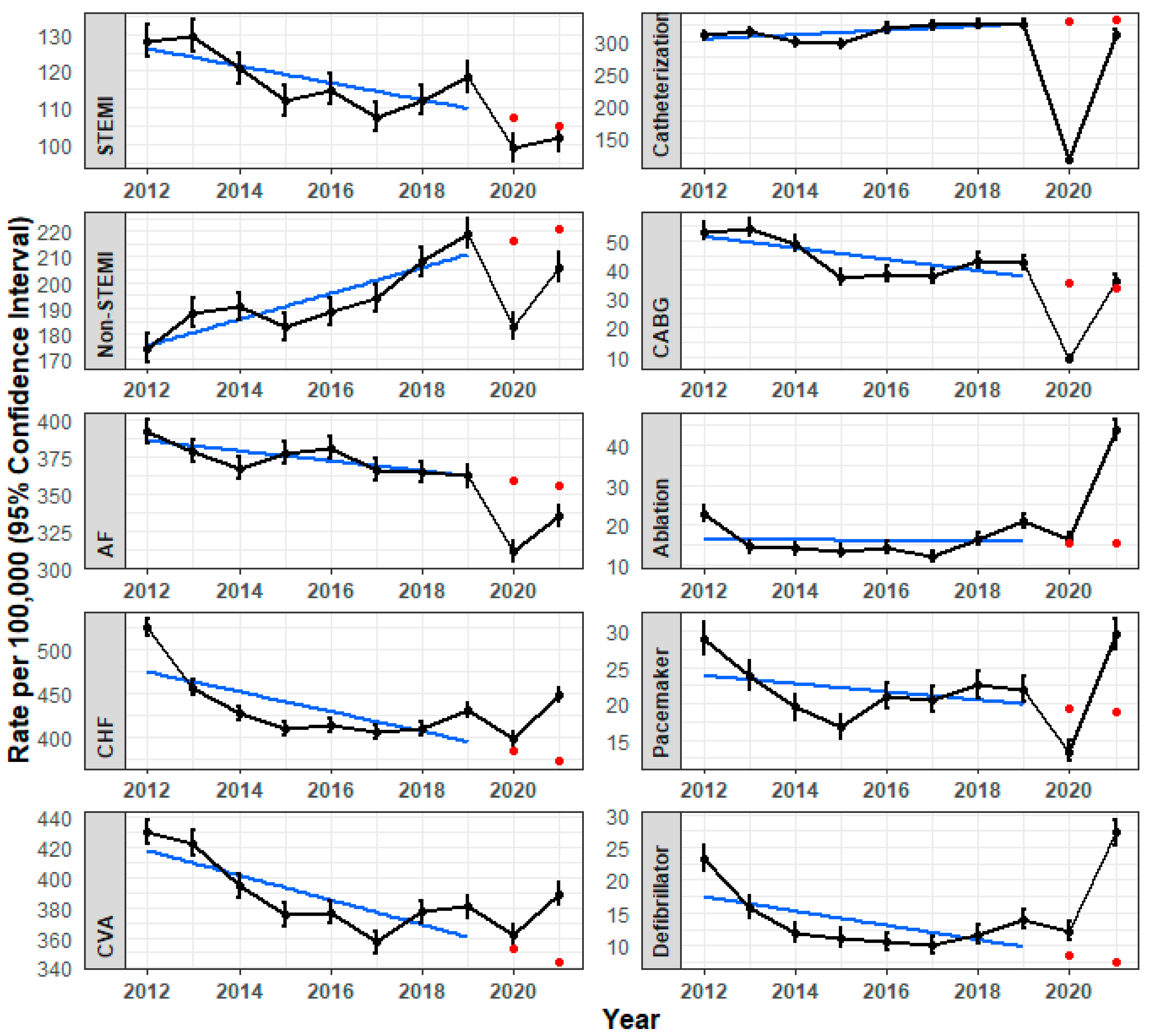
3.1. Pre-Pandemic Trends
3.2. The First Year of the COVID-19 Pandemic (Y1)
3.3. The Second Year of the COVID-19 Pandemic (Y2)
3.4. CVD Changes during the COVID-19 Pandemic in View of Pre-Pandemic Trends
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baum, A.; Kaboli, P.J.; Schwartz, M.D. Reduced In-Person and Increased Telehealth Outpatient Visits during the COVID-19 Pandemic. Ann. Intern. Med. 2021, 174, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Chatterji, P.; Li, Y. Effects of the COVID-19 Pandemic on Outpatient Providers in the United States. Med. Care 2021, 59, 58–61. [Google Scholar] [CrossRef]
- Reges, O.; Feldhamer, I.; Wolff Sagy, Y.; Lavie, G. Factors Associated with Using Telemedicine in the Primary Care Clinics during the COVID-19 Pandemic in Israel. Int. J. Environ. Res. Public Health 2022, 19, 13207. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzi, F.; Cameli, M.; Forni, S.; Gemmi, F.; Szasz, C.; Fabrizio, V.D.; Mechi, M.T.; Nocci, M.; Mondillo, S.; Valente, S. Reduction of Emergency Calls and Hospitalizations for Cardiac Causes: Effects of Covid-19 Pandemic and Lockdown in Tuscany Region. Front. Cardiovasc. Med. 2021, 8, 625569. [Google Scholar] [CrossRef]
- Zhang, J. Hospital avoidance and unintended deaths during the COVID-19 pandemic. Am. J. Health Econ. 2021, 7, 405–426. [Google Scholar] [CrossRef]
- Kiss, P.; Carcel, C.; Hockham, C.; Peters, S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: A systematic review. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 18–27. [Google Scholar] [CrossRef]
- Kodsi, M.; Bhat, A. Temporal trends in cardiovascular care: Insights from the COVID-19 pandemic. Front. Cardiovasc. Med. 2022, 9, 981023. [Google Scholar] [CrossRef]
- Russo, V.; Cante, L.; Imbalzano, E.; Di Micco, P.; Bottino, R.; Carbone, A.; D’Andrea, A. The Impact of COVID-19 Pandemic on Hospitalization and Interventional Procedures for Cardiovascular Diseases during the First Wave in Italy. Int. J. Environ. Res. Public Health 2022, 20, 472. [Google Scholar] [CrossRef]
- Solomon, M.D.; McNulty, E.J.; Rana, J.S.; Leong, T.K.; Lee, C.; Sung, S.H.; Ambrosy, A.P.; Sidney, S.; Go, A.S. The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N. Engl. J. Med. 2020, 383, 691–693. [Google Scholar] [CrossRef]
- Lavie, G.; Wolff Sagy, Y.; Hoshen, M.; Saliba, W.; Flugelman, M.Y. Continuous Decline in Myocardial Infarction and Heart Failure Hospitalizations during the First 12 Months of the COVID-19 Pandemic in Israel. J. Clin. Med. 2022, 11, 1577. [Google Scholar] [CrossRef]
- Solomon, M.D.; Nguyen-Huynh, M.; Leong, T.K.; Alexander, J.; Rana, J.S.; Klingman, J.; Go, A.S. Changes in Patterns of Hospital Visits for Acute Myocardial Infarction or Ischemic Stroke During COVID-19 Surges. JAMA 2021, 326, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Reges, O.; Weinberg, H.; Hoshen, M.; Greenland, P.; Rayyan-Assi, H.; Avgil Tsadok, M.; Bachrach, A.; Balicer, R.; Leibowitz, M.; Haim, M. Combining Inpatient and Outpatient Data for Diagnosis of Non-Valvular Atrial Fibrillation Using Electronic Health Records: A Validation Study. Clin. Epidemiol. 2020, 12, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, A.S.; Moscone, A.; McElrath, E.E.; Varshney, A.S.; Claggett, B.L.; Bhatt, D.L.; Januzzi, J.L.; Butler, J.; Adler, D.S.; Solomon, S.D.; et al. Fewer Hospitalizations for Acute Cardiovascular Conditions during the COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 76, 280–288. [Google Scholar] [CrossRef]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M.; Hollings, S.; Roebuck, C.; Gale, C.P.; Mamas, M.A.; et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Pessoa-Amorim, G.; Camm, C.F.; Gajendragadkar, P.; De Maria, G.L.; Arsac, C.; Laroche, C.; Zamorano, J.L.; Weidinger, F.; Achenbach, S.; Maggioni, A.P.; et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: A survey by the European Society of Cardiology. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 210–216. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabro, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Metzler, B.; Siostrzonek, P.; Binder, R.K.; Bauer, A.; Reinstadler, S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: The pandemic response causes cardiac collateral damage. Eur. Heart J. 2020, 41, 1852–1853. [Google Scholar] [CrossRef]
- Hernandez, I.; He, M.; Guo, J.; Tadrous, M.; Gabriel, N.; Swabe, G.; Gellad, W.F.; Essien, U.R.; Saba, S.; Benjamin, E.J.; et al. COVID-19 pandemic and trends in new diagnosis of atrial fibrillation: A nationwide analysis of claims data. PLoS ONE 2023, 18, e0281068. [Google Scholar] [CrossRef]
- Holt, A.; Gislason, G.H.; Schou, M.; Zareini, B.; Biering-Sorensen, T.; Phelps, M.; Kragholm, K.; Andersson, C.; Fosbol, E.L.; Hansen, M.L.; et al. New-onset atrial fibrillation: Incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur. Heart J. 2020, 41, 3072–3079. [Google Scholar] [CrossRef]
- Desai, S.M.; Guyette, F.X.; Martin-Gill, C.; Jadhav, A.P. Collateral damage—Impact of a pandemic on stroke emergency services. J. Stroke Cerebrovasc. Dis. 2020, 29, 104988. [Google Scholar] [CrossRef]
- Etherton, M.R.; Zachrison, K.S.; Yan, Z.; Sveikata, L.; Bretzner, M.; Estrada, J.; Viswanathan, A.; Singhal, A.B.; Schwamm, L.H. Regional Changes in Patterns of Stroke Presentation During the COVID-19 Pandemic. Stroke 2021, 52, 1398–1406. [Google Scholar] [CrossRef]
- Gabet, A.; Grave, C.; Tuppin, P.; Chatignoux, E.; Bejot, Y.; Olie, V. Impact of the COVID-19 pandemic and a national lockdown on hospitalizations for stroke and related 30-day mortality in France: A nationwide observational study. Eur. J. Neurol. 2021, 28, 3279–3288. [Google Scholar] [CrossRef]
- Pop, R.; Quenardelle, V.; Hasiu, A.; Mihoc, D.; Sellal, F.; Dugay, M.H.; Lebedinsky, P.A.; Schluck, E.; Porta, L.A.; Courtois, S.; et al. Impact of the COVID-19 outbreak on acute stroke pathways—Insights from the Alsace region in France. Eur. J. Neurol. 2020, 27, 1783–1787. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Mensah, N.O.; Opoku, F.A.; Adusei-Mensah, N.; Ampofo, M.; Ovbiagele, B. COVID-19 and stroke: Experience in a Ghanaian healthcare system. J. Neurol. Sci. 2020, 416, 117044. [Google Scholar] [CrossRef]
- Leyva, F.; Zegard, A.; Okafor, O.; Stegemann, B.; Ludman, P.; Qiu, T. Cardiac operations and interventions during the COVID-19 pandemic: A nationwide perspective. Europace 2021, 23, 928–936. [Google Scholar] [CrossRef]
- Garcia, S.; Albaghdadi, M.S.; Meraj, P.M.; Schmidt, C.; Garberich, R.; Jaffer, F.A.; Dixon, S.; Rade, J.J.; Tannenbaum, M.; Chambers, J.; et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States during COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 75, 2871–2872. [Google Scholar] [CrossRef]
- Wong, E.; Rosamond, W.; Patel, M.D.; Waller, A.E. Statewide declines in myocardial infarction and stroke emergency department visits during COVID-19 restrictions in North Carolina. Am. J. Emerg. Med. 2022, 56, 288–289. [Google Scholar] [CrossRef]
- Whaley, C.M.; Pera, M.F.; Cantor, J.; Chang, J.; Velasco, J.; Hagg, H.K.; Sood, N.; Bravata, D.M. Changes in Health Services Use Among Commercially Insured US Populations During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2024984. [Google Scholar] [CrossRef]
- Hyder, S.A.; Schoenl, S.A.; Kesiena, O.; Ali, S.H.; Davis, K.; Murrow, J.R. A 3-year analysis of the impact of COVID-19 pandemic on NSTEMI incidence, clinical characteristics, management, and outcomes. Catheter. Cardiovasc. Interv. 2022, 101, 276–286. [Google Scholar] [CrossRef]
- Cader, F.A.; Chowdhury, I.Z.; Haq, M.M.; Khan, S.R. Impact of the COVID-19 Pandemic on Cardiology Services and Catheterization Volumes in the Second Year: A Comparison of 2020 and 2021 at a South Asian Cardiac Centre. Cardiovasc. Revasc. Med. 2022, 40, 45–59. [Google Scholar] [CrossRef]
- Tien, M.; Saddic, L.A.; Neelankavil, J.P.; Shemin, R.J.; Williams, T.M. The Impact of COVID-19 on Racial and Ethnic Disparities in Cardiac Procedural Care. J. Cardiothorac. Vasc. Anesth. 2023, 37, 732–747. [Google Scholar] [CrossRef] [PubMed]
- Muhsen, K.; Cohen, D. COVID-19 vaccination in Israel. Clin. Microbiol. Infect. 2021, 27, 1570–1574. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomstrom-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Marijon, E.; Karam, N.; Jost, D.; Perrot, D.; Frattini, B.; Derkenne, C.; Sharifzadehgan, A.; Waldmann, V.; Beganton, F.; Narayanan, K.; et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: A population-based, observational study. Lancet Public Health 2020, 5, e437–e443. [Google Scholar] [CrossRef]
- Reynolds, K.; Go, A.S.; Leong, T.K.; Boudreau, D.M.; Cassidy-Bushrow, A.E.; Fortmann, S.P.; Goldberg, R.J.; Gurwitz, J.H.; Magid, D.J.; Margolis, K.L.; et al. Trends in Incidence of Hospitalized Acute Myocardial Infarction in the Cardiovascular Research Network (CVRN). Am. J. Med. 2017, 130, 317–327. [Google Scholar] [CrossRef]
| Year | N * (Millions) | Women (%) | Mean Age (SD) |
|---|---|---|---|
| 2012 | 2.43 | 52.1% | 49.7 (0.03) |
| 2013 | 2.48 | 52.1% | 49.7 (0.03) |
| 2014 | 2.52 | 52.1% | 49.7 (0.03) |
| 2015 | 2.56 | 52.0% | 49.7 (0.03) |
| 2016 | 2.59 | 52.0% | 49.7 (0.02) |
| 2017 | 2.63 | 52.0% | 49.8 (0.02) |
| 2018 | 2.66 | 52.0% | 49.9 (0.01) |
| 2019 | 2.69 | 52.0% | 50.0 (0.03) |
| 2020 | 2.73 | 51.9% | 50.1 (0.02) |
| 2021 | 2.76 | 51.9% | 50.1 (0.02) |
| Year | STEMI | Non-STEMI | AF | CHF | CVA |
|---|---|---|---|---|---|
| 2012 | 128.3 (123.8, 132.8) | 174.4 (169.2–179.8) | 392.4 384.6–400.4 | 525.0 (516.0, 534.2) | 430.1 (421.9, 438.4) |
| 2013 | 129.5 (125.1, 134.1) | 188.2 (182.8–193.7) | 379 (371.4, 386.8) | 456.1 (447.7, 464.6) | 422.6 (414.5, 430.8) |
| 2014 | 120.7 (116.4, 125.1) | 190.7 (185.4, 196.2) | 367.6 (360.2, 375.2) | 426.9 (418.9, 435.1) | 394 (386.2, 401.8) |
| 2015 | 112 (107.9, 116.2) | 182.6 (177.4, 187.9) | 377.6 (370.1, −385.2) | 409.4 (401.6, 417.3) | 375 (367.5, 382.6) |
| 2016 | 114.9 (110.8, 119.1) | 188.8 (183.5–194.2) | 381 (373.6, 388.6) | 412.9 (405.2, 420.9) | 376.6 (369.1, 384.1) |
| 2017 | 107.4 (103.5, 111.5) | 193.6 (188.4, 199.0) | 366.5 (359.2, 373.9) | 405.3 (397.7, 413.1) | 356.9 (349.7, 364.2) |
| 2018 | 112 (108.0, 116.1) | 208.2 (202.7, 213.7) | 364.8 (357.6, 372.2) | 409.7 (402.0, 417.4) | 376.9 (369.6, 384.4) |
| 2019 (baseline) | 118.2 (114.1, 122.3) | 218.8 (213.3, 224.5) | 362.1 (354.9, 369.4) | 431.1 (423.3, 439.0) | 380.3 (372.9, 387.7) |
| 2020 (Y1) | 98.9 (95.2, 102.7) | 182.9 (177.9, 188.1) | 311.1 (304.5, 317.8) | 397.5 (390.0, 405.0) | 361.3 (354.2, 368.5) |
| 2021 (Y2) | 101.8 (98.1, 105.6) | 206 (200.7, 211.4) | 334.9 (328.1, 341.8) | 447.5 (439.6, 455.4) | 388.7 (381.4, 396.1) |
| Y1 vs. baseline | |||||
| n | −19.3 (−24.8, −13.7) | −35.9 (−43.4, −28.4) | −51.0 (−60.7, −41.2) | −33.6 (−44.4, −22.8) | −19.0 (−29.2, −8.7) |
| % | −16.3% (−16.6, −16.1) | −16.4% (−16.6, −16.2) | −14.1% (−14.2, −14.0) | −7.8% (−7.9, −7.7) | −5.0% (−5.0, −4.9) |
| Y2 vs. baseline | |||||
| n | −16.4 (−22.0, −10.8) | −12.8 (−20.6, 5.1) | −27.2 (−37.1, −17.3) | 16.4 (5.3, 27.2) | 8.4 (−2.0, 18.8) |
| % | −13.9% (−14.1, −13.7) | −5.9% (−5.9, −5.8) | −7.5% (−7.6, −7.5) | 3.8% (3.8, 3.9) | 2.2% (2.2, 2.3) |
| Year | Catheterization | CABG | Ablation | Pacemaker | Defibrillator |
|---|---|---|---|---|---|
| 2012 | 309.7 (302.7, 316.8) | 53.2 (50.3, 56.2) | 22.7 (20.8, 24.6) | 28.9 (26.8, 31.1) | 23.3 (21.4, 25.3) |
| 2013 | 314.9 (308.0, 322.0) | 54.3 (51.5, 57.3) | 14.4 (13.0, 16.0) | 23.7 (21.9, 25.7) | 15.8 (14.3, 17.5) |
| 2014 | 299.1 (292.4, 306.0) | 49.1 (46.4, 51.9) | 13.9 (12.5, 15.5) | 19.4 (17.8, 21.2) | 12.0 (10.7, 13.4) |
| 2015 | 296.3 (289.7, 303.1) | 37.4 (35.0, 39.8) | 13.3 (11.9, 14.7) | 16.7 (15.2, 18.4) | 11.2 (10.0, 12.6) |
| 2016 | 321.0 (314.2, 328) | 38.6 (36.2, 41.1) | 14.2 (12.8, 15.7) | 21.0 (19.3, 22.8) | 10.6 (9.4, 12.0) |
| 2017 | 325.7 (318.8, 332.7) | 37.5 (35.2, 39.9) | 12.0 (10.7, 13.4) | 20.5 (18.8,22.3) | 10.1 (8.9, 11.4) |
| 2018 | 326.6 (319.8, 333.6) | 43.2 (40.8, 45.8) | 16.2 (14.8, 17.9) | 22.5 (20.8, 24.4) | 11.7 (10.5, 13.1) |
| 2019 (baseline) | 327.2 (320.4, 334.1) | 42.3 (39.9, 44.8) | 20.8 (19.1, 22.6) | 22.0 (20.3, 23.8) | 14.0 (12.6, 15.5) |
| 2020 (Y1) | 115.5 (111.5, 119.6) | 9.4 (8.3, 10.7) | 16.4 (14.9, 18.0) | 13.4 (12.0, 14.8) | 12.3 (11.0, 13.6) |
| 2021 (Y2) | 311.4 (304.9, 318.1) | 36.0 (33.8, 38.3) | 43.9 (41.5, 46.5) | 29.5 (27.5, 31.6) | 27.2 (25.3, 29.2) |
| Y1 vs. baseline | |||||
| n | −211.7 (−219.7, −203.7) | −32.9 (−35.6, −30.2) | −4.4 (−6.7, −2.1) | −8.6 (−10.4, −6.4) | −1.7 (−3.7, 0.3) |
| % | −64.7% (−65.2, −64.2) | −77.7% (−79.2, −76.2) | −21.2% (−22.0, −20.4) | −39.3% (−40.7, −37.9) | −12.5% (−13.1, −12.0) |
| Y2 vs. baseline | |||||
| n | −15.8 (−25.3, −6.3) | −6.3 (−9.6, −3.0) | 23.1 (20.1, 26.2) | 7.5 (4.8, 10.2) | 13.2 (10.8, 15.6) |
| % | −4.8% (−4.9, −4.8) | −15.0% (−15.4, −14.6) | 111.1% (105.6, 116.9) | 34.2% (32.6, 35.8) | 94.0% (88.5, 100.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reges, O.; Abu Ahmad, W.; Battat, E.; Saliba, W.; Wolff Sagy, Y.; Danon, A.; Lavie, G. Trends in the Incidence of Cardiovascular Diagnoses and Procedures over the Years 2012–2021 in Israel: The Impact of the COVID-19 Pandemic. J. Clin. Med. 2024, 13, 476. https://doi.org/10.3390/jcm13020476
Reges O, Abu Ahmad W, Battat E, Saliba W, Wolff Sagy Y, Danon A, Lavie G. Trends in the Incidence of Cardiovascular Diagnoses and Procedures over the Years 2012–2021 in Israel: The Impact of the COVID-19 Pandemic. Journal of Clinical Medicine. 2024; 13(2):476. https://doi.org/10.3390/jcm13020476
Chicago/Turabian StyleReges, Orna, Wiessam Abu Ahmad, Erez Battat, Walid Saliba, Yael Wolff Sagy, Asaf Danon, and Gil Lavie. 2024. "Trends in the Incidence of Cardiovascular Diagnoses and Procedures over the Years 2012–2021 in Israel: The Impact of the COVID-19 Pandemic" Journal of Clinical Medicine 13, no. 2: 476. https://doi.org/10.3390/jcm13020476
APA StyleReges, O., Abu Ahmad, W., Battat, E., Saliba, W., Wolff Sagy, Y., Danon, A., & Lavie, G. (2024). Trends in the Incidence of Cardiovascular Diagnoses and Procedures over the Years 2012–2021 in Israel: The Impact of the COVID-19 Pandemic. Journal of Clinical Medicine, 13(2), 476. https://doi.org/10.3390/jcm13020476






