The Safety and Cost Analysis of Outpatient Laparoendoscopy in the Treatment of Cholecystocholedocholithiasis: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
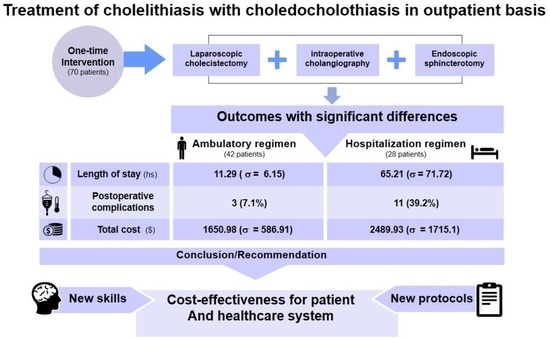
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ricci, C.; Pagano, N.; Taffurelli, G.; Pacilio, C.A.; Migliori, M.; Bazzoli, F.; Casadei, R.; Minni, F. Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: A Systematic Review and Network Meta-analysis. JAMA Surg. 2018, 153, e181167. [Google Scholar] [CrossRef] [PubMed]
- Bove, A.; Panaccio, P.; di Renzo, R.; Palone, G.; Ricciardiello, M.; Ciuffreda, S.; Bongarzoni, G. How to choose the most appropriate technique for the single-stage treatment of cholecysto-choledocolithiasis? Gastroenterol. Rep. 2019, 7, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Y.; Cheng, Y.; Li, T.; Cheng, B.; Jin, X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: A meta-analysis. Surg. Endosc. 2019, 33, 3275–3286. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Guo, Z.; Liu, Z.; Wang, Y.; Si, Y.; Jin, M. Preoperative versus intraoperative endoscopic sphincterotomy in patients with gallbladder and suspected common bile duct stones: System review and meta-analysis. Surg. Endosc. 2013, 27, 2454–2465. [Google Scholar] [CrossRef] [PubMed]
- Manes, G.; Paspatis, G.; Aabakken, L.; Ardeloni, A.; Arvanitakis, M.; Ah-Soune, P.; Barthet, M.; Domagk, D.; Domonceau, J.; Gigot, J.; et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019, 51, 472–491. [Google Scholar] [CrossRef] [PubMed]
- Buxbaum, J.L.; Abbas Fehmi, S.M.; Sultan, S.; Fishman, D.S.; Qumseya, B.J.; Cortessis, V.K.; Schilperoort, H.; Kysh, L.; Matsuoka, L.; Yachimski, P.; et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest. Endosc. 2019, 89, 1075–1105. [Google Scholar] [CrossRef]
- Santos, J.S.; Kemp, R.; Ardengh, J.C.; Elias, J., Jr. Conservative management of cholestasis with and without fever in acute biliary pancreatitis. World J. Gastrointest. Surg. 2012, 4, 55–61. [Google Scholar] [CrossRef]
- Costi, R.; Gnocchi, A.; Di Mario, F.; Sarli, L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J. Gastroenterol. 2014, 20, 13382–13401. [Google Scholar] [CrossRef]
- Ele, H.; Tan, C.; Wu, J.; Wu, J.G.; Dai, N.; Hu, W.; Zhang, Y.; Laine, L.; Scheiman, J.; Lim, J.J. Accuracy of ASGE high-risk criteria in evaluation of patients with suspected common bile duct stones. Gastrointest. Endosc. 2017, 86, 525–532. [Google Scholar]
- Dumange Chapuis-Roux, E.; Allart, K.; Delcenserie, R.; Braseiro, F.; Regimeau, J.-M. Single-stage management of cholelithiasis and choledocholithiasis: Laparoscopic cholecystectomy and intra-operative endoscopic sphincterotomy (with video). J. Visc. Surg. 2018, 155, 311–316. [Google Scholar] [CrossRef]
- Berci, G.; Sackier, J.M.; Paz-Partlow, M. Routine or selected intraoperative cholangiography during laparoscopic cholecystectomy? Am. J. Surg. 1991, 161, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Lella, F.; Bagnolo, F.; Rebuffat, C.; Rejeitada, C.; Scalambra, M.; Bonassi, U.; Colombo, E. Use of the laparoscopic-endoscopic approach, the so-called “rendezvous” technique, in cholecystocholedocholithiasis: A valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg. Endosc. 2006, 20, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Dallora, M.; Forster, A. The real importance of cost management in a teaching hospital—Theoretical considerations. Medicina 2008, 41, 135–142. [Google Scholar]
- Frossard, J.L.; Morel, P.M. Detection and management of bile duct stones. Gastrointest. Endosc. 2010, 72, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Peery, A.F.; Crockett, S.D.; Barritt, A.S.; Dellon, E.S.; Eluri, S.; Gangarosa, L.M.; Jensen, E.T.; Lund, J.; Pasricha, S.; Runge, T.; et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology 2015, 149, 1731–1741.e3. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.X.; Kulaylat, A.N.; Hollenbeak, C.S.; Soybel, D.I. Cost-effective decisions in detecting silent common bile duct gallstones during laparoscopic cholecystectomy. Ann. Surg. 2016, 263, 1164–1172. [Google Scholar] [CrossRef]
- Lu, J.; Cheng, Y.; Xiong, X.Z.; Lin, Y.; Wu, S.; Cheng, N. Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J. Gastroenterol. 2012, 18, 3156–3166. [Google Scholar] [CrossRef]
- Jones, M.; Johnson, M.; Samourjian, E.; Schalauch, E.; Ozobia, N. ERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: A random comparison to the standard (two-step) procedure. Surg. Endosc. 2013, 27, 1907–1912. [Google Scholar] [CrossRef]
- Lei, C.; Lu, T.; Yang, W.; Yang, M.; Tian, H.; Song, S.; Gong, S.; Yang, J.; Jiang, W.; Yang, K.; et al. Comparison of intraoperative endoscopic retrograde cholangiopancreatography and laparoscopic common bile duct exploration combined with laparoscopic cholecystectomy for treating gallstones and common bile duct stones: A systematic review and meta-analysis. Surg. Endosc. 2021, 35, 5918–5935. [Google Scholar] [CrossRef]
- March, B.; Burnett, D.; Gani, J. Single-stage laparoscopic cholecystectomy and intraoperative endoscopic retrograde cholangiopancreatography: Is this strategy feasible in Australia? ANZ J. Surg. 2016, 86, 874–877. [Google Scholar] [CrossRef] [PubMed]
- Bansal, V.K.; Misra, M.C.; Rajan, K.; Kilambi, R.; Kumar, S.; Krishna, A.; Kumar, A.; Pandav, C.S.; Subramaniam, R.; Arora, M.K.; et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: A randomized controlled trial. Surg. Endosc. 2014, 28, 875–885. [Google Scholar] [PubMed]
- Donnellan, E.; Coulter, J.; Mathew, C.; Choynowski, M.; Flanagan, L.; Bucholc, M.; Johnston, A.; Sugrue, M. A meta-analysis of the use of intraoperative cholangiography; time to revisit our approach to cholecystectomy? Surg. Open Sci. 2020, 3, 8–15. [Google Scholar] [CrossRef]
- Kenny, R.; Richardson, J.; McGlone, E.R.; Reddy, M.; Khan, O.U. Laparoscopic common bile duct exploration versus pre or post-operative ERCP for common bile duct stones in patients undergoing cholecystectomy: Is there any difference? Int. J. Surg. 2014, 12, 989–993. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Su, Y.; Yan, J.; Li, X. Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis: A systemic review and meta-analysis. Surg. Endosc. 2020, 34, 4214–4224. [Google Scholar] [CrossRef] [PubMed]
- Vaccari, S.; Minghetti, M.; Lauro, A.; Bellini, M.I.; Ussia, A.; Khouzam, S.; Marino, I.R.; Cervellera, M.; D’Andrea, V.; Tonini, V. Destiny for rendezvous: Is cholecysto/choledocholithiasis better treated with dual or single-step procedures. Dig. Dis. Sci. 2020, 67, 1116–1127. [Google Scholar] [CrossRef]
- Vettoretto, N.; Arezzo, A.; Famiglietti, F.; Cirocchi, R.; Moja, L.; Morino, M. Laparoscopic-endoscopic rendezvous versus preoperative endoscopic sphincterotomy in people undergoing laparoscopic cholecystectomy for stones in the gallbladder and bile duct. Cochrane Database Syst. Rev. 2018, 4, CD010507. [Google Scholar] [CrossRef]
- Cianci, P.; Restini, E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J. Gastroenterol. 2021, 27, 4536–4554. [Google Scholar] [CrossRef]
- Barreras Gonzalez, J.E.; Torres Pena, R.; Ruiz Torres, J.; Alfonso, M.Á.; Quintanilla, R.; Perez, M. Endoscopic versus laparoscopic treatment for choledocholithiasis: A prospective randomized controlled trial. Endosc. Int. Open 2016, 4, E1188–E1193. [Google Scholar] [CrossRef]
- Testoni, P.A.; Mariani, A.; Aabakken, L.; Arvanitakis, M.; Bories, E.; Costamagna, G.; Deviere, J.; Dinis-Ribeiro, M.; Dumonceau, J.; Giovannini, M.; et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 657–683. [Google Scholar] [CrossRef]
- Brown, L.M.; Rogers, S.J.; Violoncelo, J.P.; Brasel, K.J.; Inadomi, J.M. Cost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stones. J. Am. Coll. Surg. 2011, 212, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Tzovaras, G.; Baloyiannis, I.; Zachari, E.; Symeonidis, D.; Zacharoulis, D.; Kapsoritakis, A.; Paroutoglou, G.; Potamianos, D. Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: Interim analysis of a controlled randomized trial. Ann. Surg. 2012, 255, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Swahn, F.; Nilsson, M.; Arnelo, U.; Lohr, M.; Persson, G.; Enochsson, L. Rendezvous cannulation technique reduces post-ERCP pancreatitis: A prospective nationwide study of 12,718 ERCP procedures. Am. J. Gastroenterol. 2013, 108, 552–559. [Google Scholar] [CrossRef] [PubMed]


| LE Treatment | |||||
|---|---|---|---|---|---|
| Variables | N = 70 | AR = 42 | HR = 28 | ||
| Mean (SD) | Mean (SD) | Mean (SD) | p | ||
| Age (years) | 47.5 (19.12) | 43.52 (19.04) | 53.46 (17.96) | 0.03 * | |
| n/% | n/% | n/% | p | ||
| Gender | Male | 23 (32.9%) | 15 (35.7%) | 8 (28.6%) | 0.61 |
| Female | 47 (67.1%) | 27 (64.3%) | 20 (71.4%) | ||
| ASA | I | 29 (41.4%) | 25 (59.5%) | 4 (14.3%) | <0.01 * |
| II | 31 (44.3%) | 13 (31%) | 18 (64.3%) | ||
| III | 10 (14.3%) | 4 (9.5%) | 6 (21.4%) | ||
| Risk of choledocholitiasis | High | 55 (78.6%) | 33 (78.6%) | 22 (78.6%) | 0.99 |
| Intermediate | 15 (21.4%) | 9 (21.4%) | 6 (21.4%) | ||
| Low | 0 (0%) | 0 (0%) | 0 (0%) | ||
| MBD diameter | mm | 11.44 (2.1) | 11.38 (2) | 11.54 (2.27) | 0.76 |
| Stone diameter | mm | 7.92 (3.25) | 7.97 (3.13) | 7.84 (3.5) | 0.87 |
| Access to the MBD | Sphincterotomy | 17 (24.3%) | 11 (26.2%) | 6 (21.4%) | 0.91 |
| Rendezvous | 9 (12.9%) | 6 (14.3%) | 3 (10.7%) | ||
| Infundibulotomy | 42 (60%) | 24 (57.1%) | 18 (64.3%) | ||
| Fistulotomy | 2 (2.9%) | 1 (2.4%) | 1 (3.6%) | ||
| Manipulation of the MPD | Yes | 16 (22.9%) | 9 (21.4%) | 7 (25%) | 0.78 |
| No | 54 (77.1%) | 33 (78.6%) | 21 (75%) | ||
| Pancreatography | Yes | 2 (2.9%) | 1 (2.4%) | 1 (3.6%) | 0.99 |
| No | 68 (97.1%) | 41 (97.6%) | 27 (96.4%) | ||
| Surgical time | Minutes | 128.76 (39.31) | 122.9 (31.02) | 137.54 (48.52) | 0.16 |
| Lenght of stay | Hours | 32.86 (52.38) | 11.29 (6.15) | 65.21 (71.72) | <0.01 |
| Effectiveness | Yes | 64 (98.5%) | 41 (100%) | 23 (95.8%) | 0.37 |
| No | 1 (1.5%) | 0 (0%) | 1 (4.2%) | ||
| Postoperative complications | None | 56 (80%) | 39 (92.86%) | 17 (60.71%) | <0.01 * |
| Wound infection | 2 (2.86%) | 0 (0%) | 2 (7.14%) | ||
| ERCP pancreatitis | 3 (4.29%) | 2 (4.76%) | 1 (3.57%) | ||
| Papillary hemorrhage | 2 (2.86%) | 1 (2.38%) | 1 (3.57%) | ||
| Duodenal perforation | 1 (1.43%) | 0 (0%) | 1 (3.57%) | ||
| Umbilical hernia | 1 (1.43%) | 0 (0%) | 1 (3.57%) | ||
| Wound dehiscence | 1 (1.43%) | 0 (0%) | 1 (3.57%) | ||
| CRI becoming acute | 1 (1.43%) | 0 (0%) | 1 (3.57%) | ||
| Renal dysfunction | 1 (1.43%) | 0 (0%) | 1 (3.57%) | ||
| Abdominal collection | 2 (2.86%) | 0 (0%) | 2 (7.14%) | ||
| Clavien–Dindo | Grade I | 7 (10%) | 1 (2.4%) | 6 (21.4%) | < 0.01 * |
| Grade II | 2 (2.9%) | 1 (2.4%) | 1 (3.6%) | ||
| Grade IIIa | 1 (1.4%) | 0 (0%) | 1 (3.6%) | ||
| Grade IIIb | 2 (2.9%) | 0 (0%) | 2 (7.1%) | ||
| Grade IVa | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Grade IVb | 1 (1.4%) | 0 (0%) | 1 (3.6%) | ||
| Grade V | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Variable | LE Treatment | Estimated Difference (95% CI) | p-Value | |
|---|---|---|---|---|
| AR (n = 42) | HR (n = 28) | |||
| Mean (SD) | Mean (SD) | |||
| Cost of hospitalization | 305.03 (458.38) | 874.12 (1148.38) | −569.08 (−1033.59; −104.58) | 0.02 * |
| Cost of medication | 9.88 (16.84) | 46.18 (92.59) | −36.3 (−72.53; −0.08) | 0.05 |
| Cost of surgery | 930.15 (206.55) | 1133.27 (445.56) | −203.12 (−360.54; −45.7) | 0.01 * |
| Cost of the ARR | 56.91 (47.95) | 52.22 (47.41) | 4.7 (−18.54; 27.94) | 0.69 |
| Cost of exams | 45.91 (89.34) | 81.05 (146.56) | −35.14 (−91.37; 21.1) | 0.22 |
| Total cost | 1650.98 (586.91) | 2489.93 (1715.1) | −838.95 (−1525.09; −152.8) | 0.02 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos, J.S.; Kemp, R.; Orquera, A.G.M.; Gaspar, A.F.; Júnior, J.R.L.; Queiroz, L.T.A.; Avezum, V.A.P.A.F.; Ardengh, J.C.; Sankarankutty, A.K.; Lima, L.S. The Safety and Cost Analysis of Outpatient Laparoendoscopy in the Treatment of Cholecystocholedocholithiasis: A Retrospective Study. J. Clin. Med. 2024, 13, 460. https://doi.org/10.3390/jcm13020460
dos Santos JS, Kemp R, Orquera AGM, Gaspar AF, Júnior JRL, Queiroz LTA, Avezum VAPAF, Ardengh JC, Sankarankutty AK, Lima LS. The Safety and Cost Analysis of Outpatient Laparoendoscopy in the Treatment of Cholecystocholedocholithiasis: A Retrospective Study. Journal of Clinical Medicine. 2024; 13(2):460. https://doi.org/10.3390/jcm13020460
Chicago/Turabian Styledos Santos, José Sebastião, Rafael Kemp, Alicia Guadalupe Mendoza Orquera, Alberto Facury Gaspar, Jorge Resende Lopes Júnior, Lucas Tobias Almeida Queiroz, Víctor Antônio Peres Alves Ferreira Avezum, José Celso Ardengh, Ajith Kumar Sankarankutty, and Leonardo Santos Lima. 2024. "The Safety and Cost Analysis of Outpatient Laparoendoscopy in the Treatment of Cholecystocholedocholithiasis: A Retrospective Study" Journal of Clinical Medicine 13, no. 2: 460. https://doi.org/10.3390/jcm13020460
APA Styledos Santos, J. S., Kemp, R., Orquera, A. G. M., Gaspar, A. F., Júnior, J. R. L., Queiroz, L. T. A., Avezum, V. A. P. A. F., Ardengh, J. C., Sankarankutty, A. K., & Lima, L. S. (2024). The Safety and Cost Analysis of Outpatient Laparoendoscopy in the Treatment of Cholecystocholedocholithiasis: A Retrospective Study. Journal of Clinical Medicine, 13(2), 460. https://doi.org/10.3390/jcm13020460