Anterior Intercondylar Notch Geometry in Relation to the Native Anterior Cruciate Ligament Size
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. MRI Acquisition
2.3. Variables and Measurements
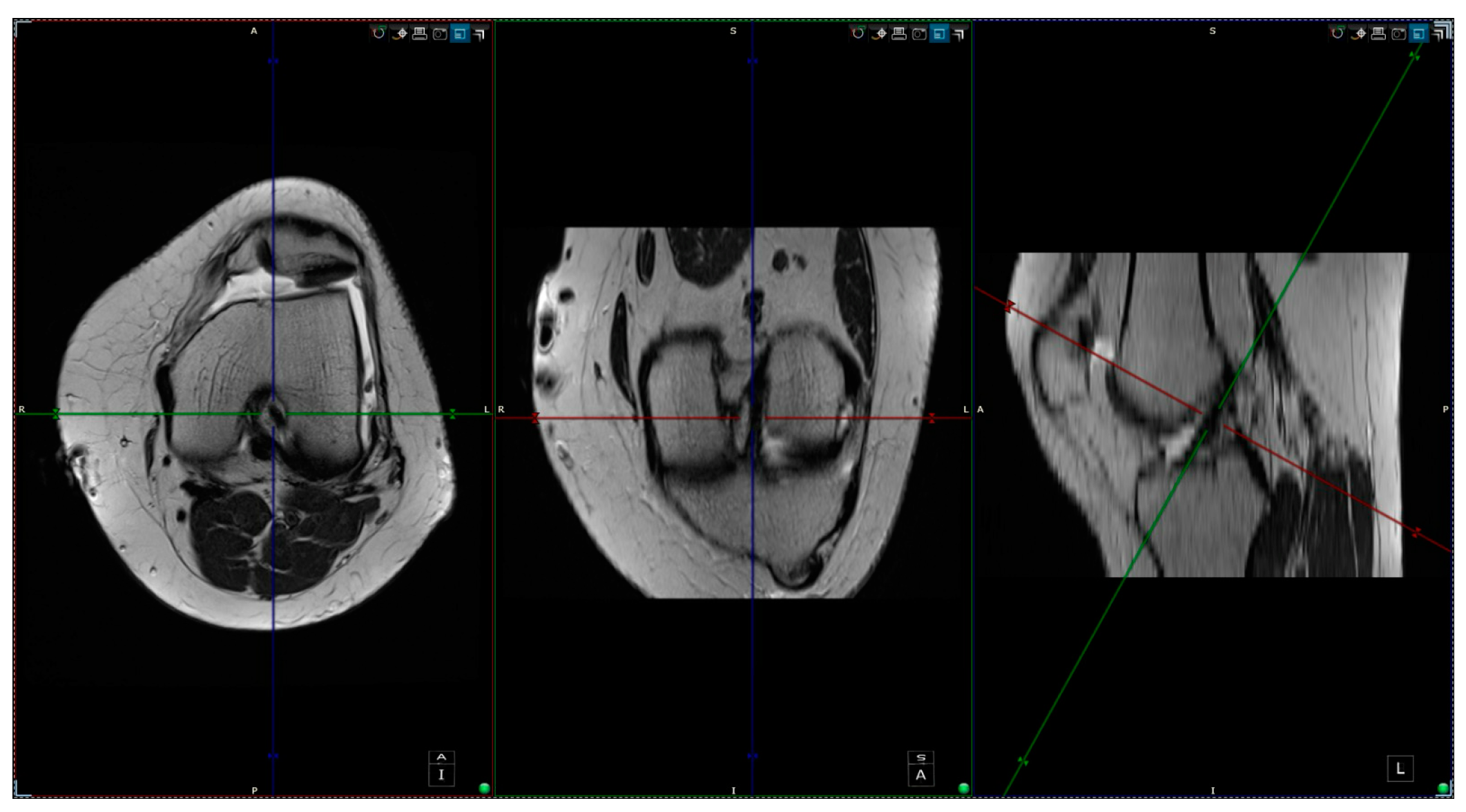
2.4. Measurements
- -
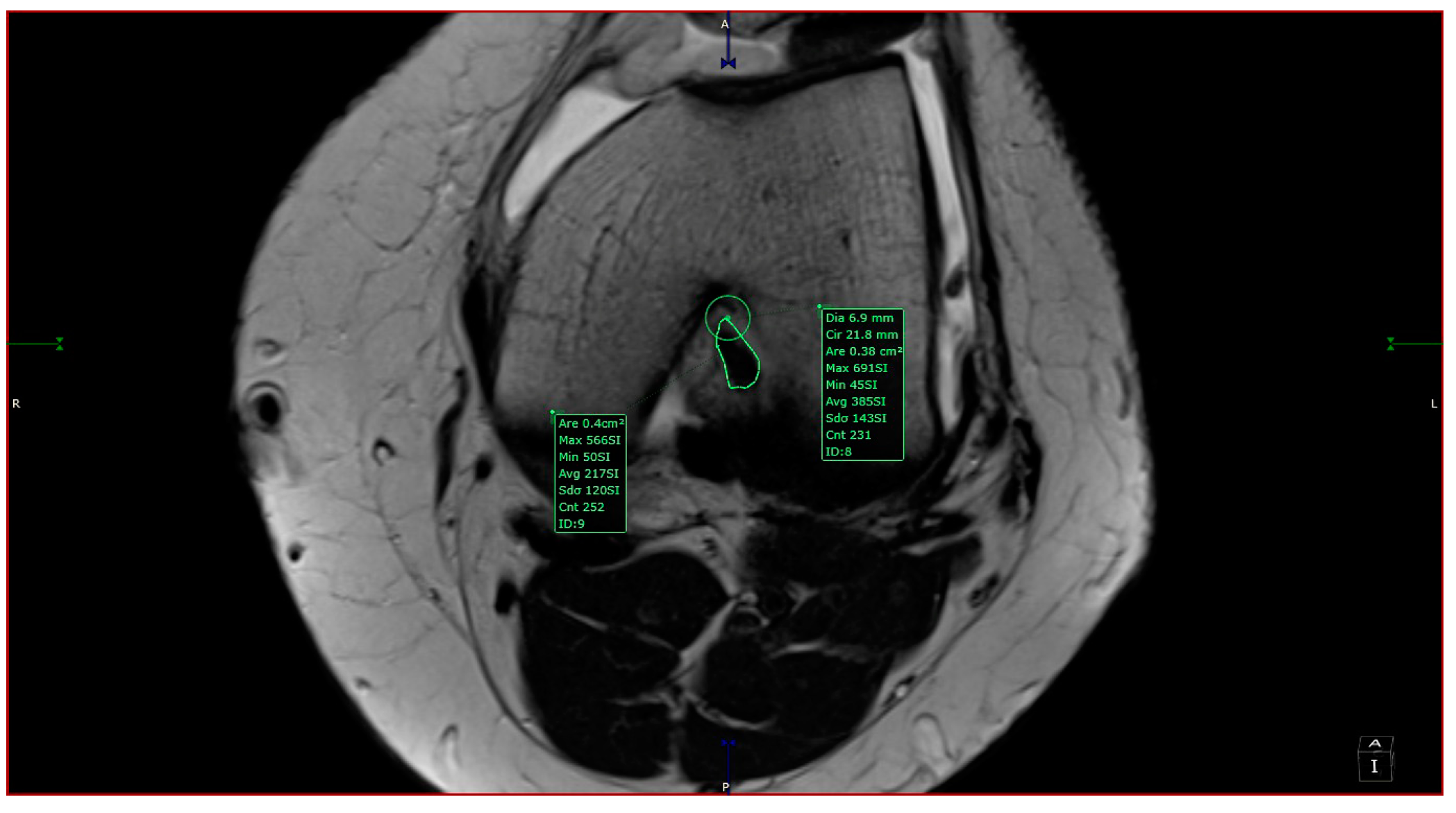
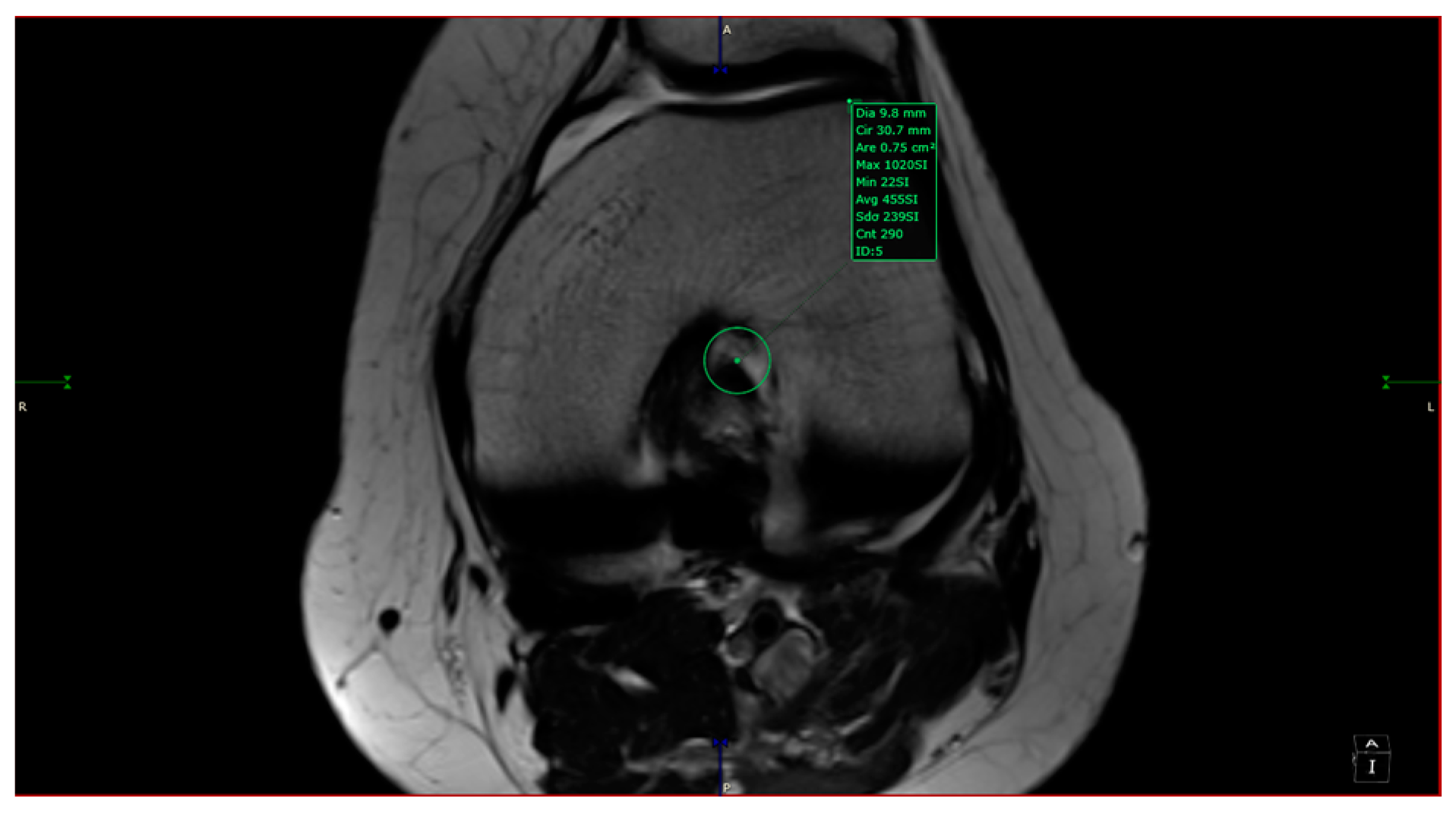
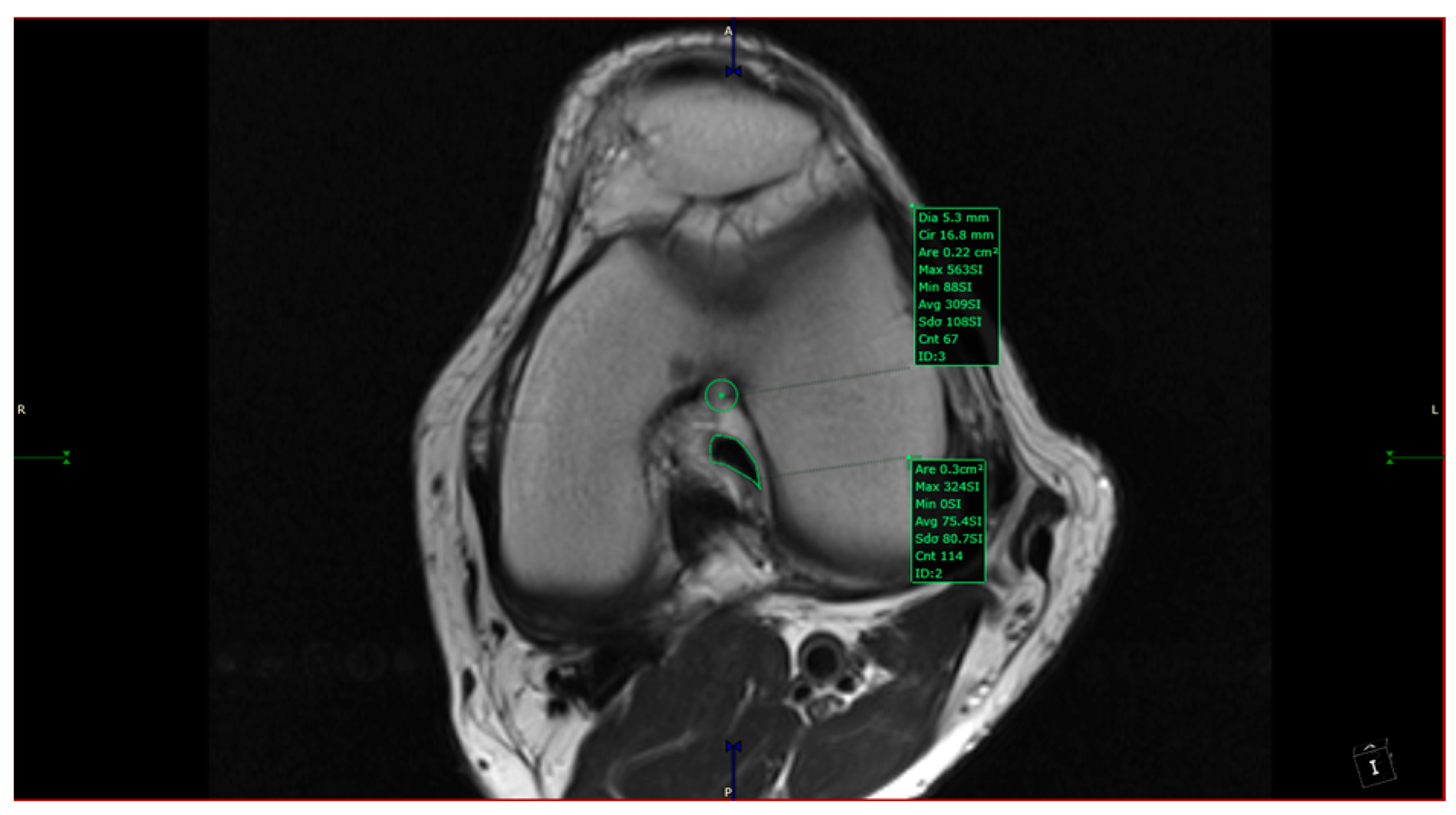
- aICN area: area of the circle defined by three cortical walls of the antero-superior notch (in the custom axial plane/CAP; Figure 3).
- -
- ICN width: notch width in the distal part
- -
- ACL area: area of the closed polygon defined by pointed dots around the cross-section of the anterior cruciate ligament (in the CAP; Figure 4).
- -
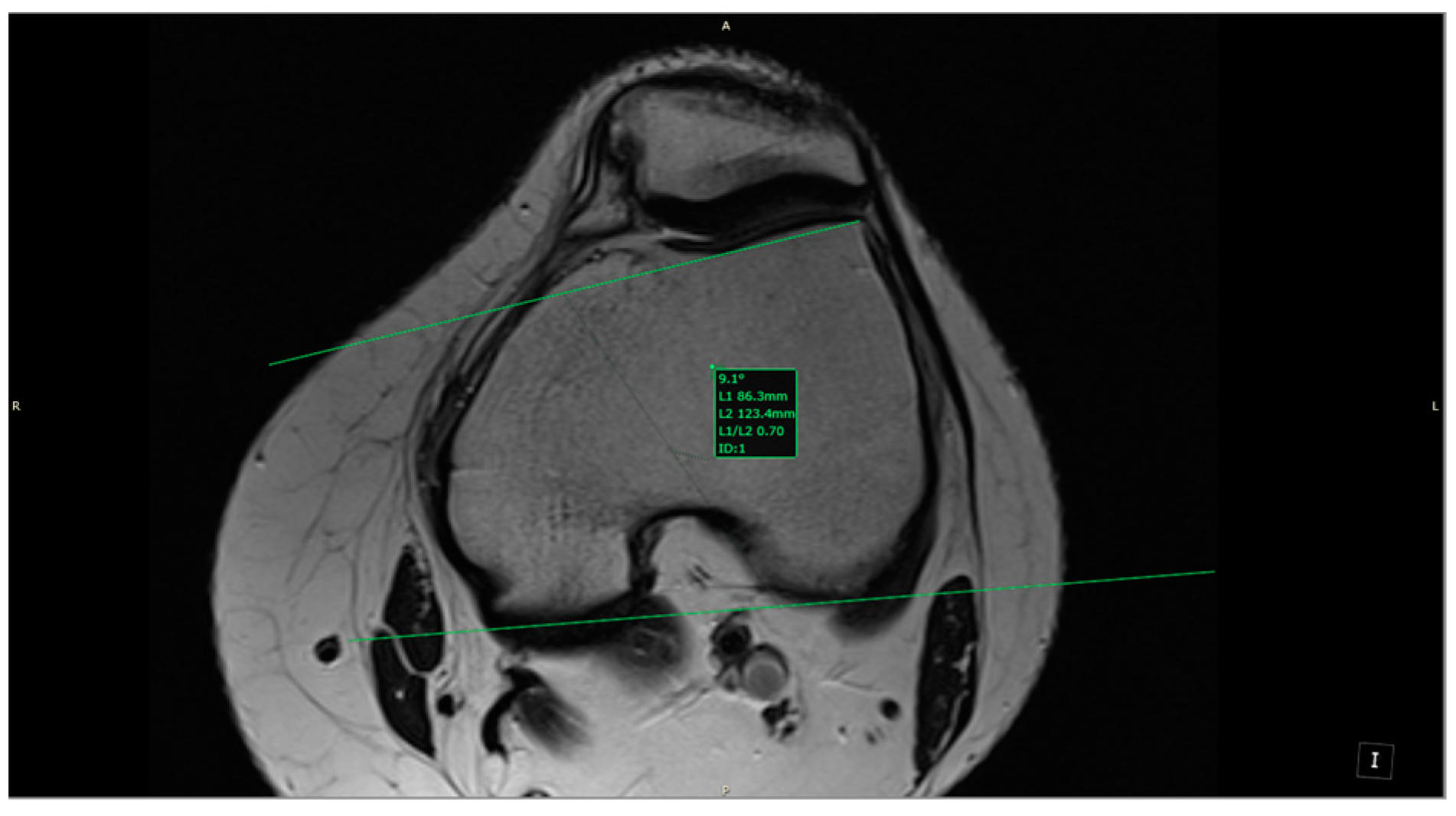
- LTI: inclination angle between the lateral femoral trochlea on the most proximal axial slice containing trochlear cartilage and a posterior condylar tangential line (in the axial plane; Figure 5).
- -
- Patella alta: Insall–Salvati index > 1.5 (in the sagittal plane).
- -
- Trochlear dysplasia: LTI < 11° (in the axial plane).
- -
- aICN area and ACL area (both appear in Figure 6).
2.5. Statistical Analysis
2.6. Ethics
3. Results
3.1. Descriptive Data: General Characteristics of the Studied Group
3.2. Association between Intercondylar Notch Shape and ACL Size and Other Knee Lesions
3.3. Association between Anterior Cruciate Ligament Area and Knee Lesions
4. Discussion
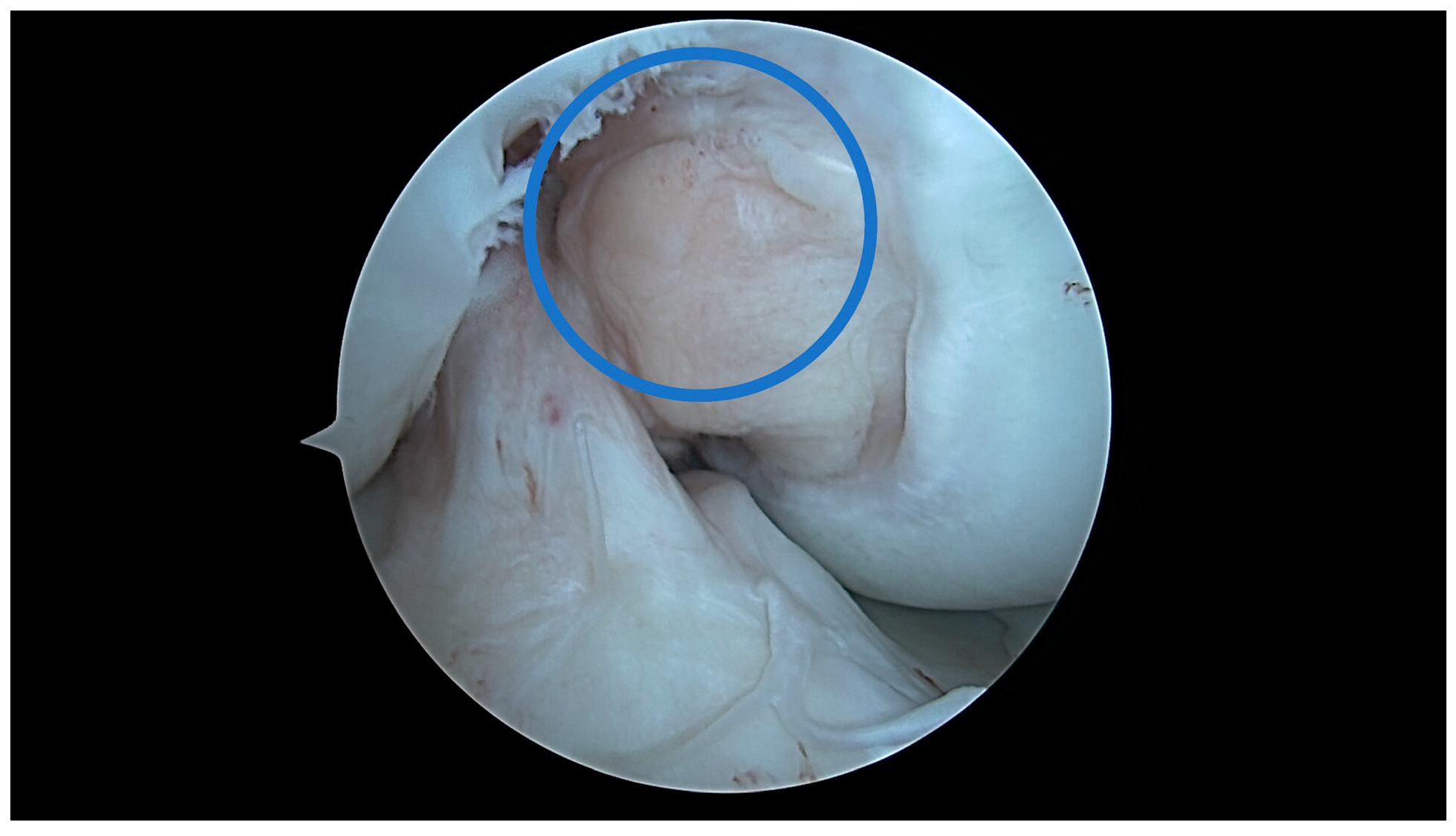
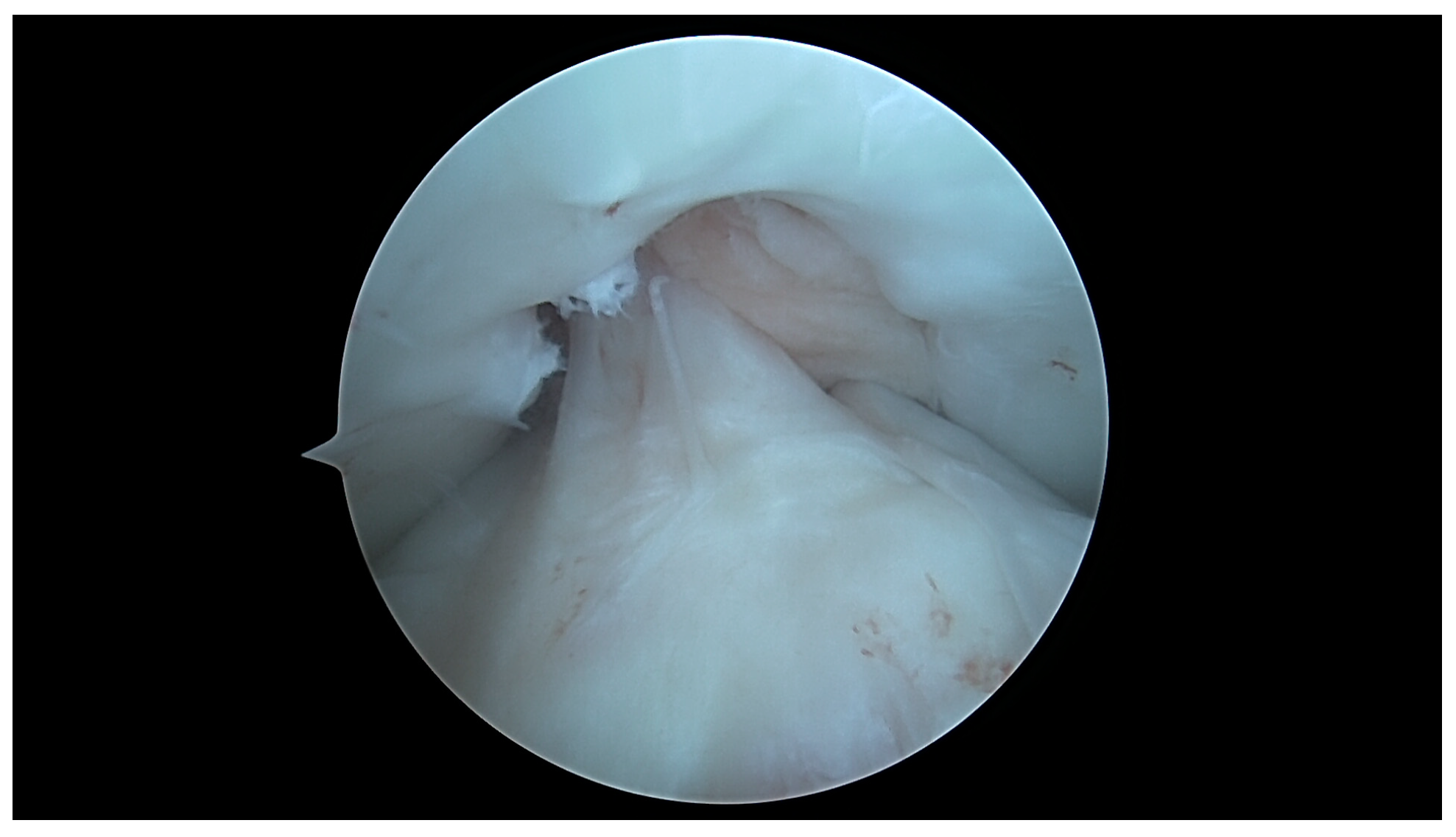
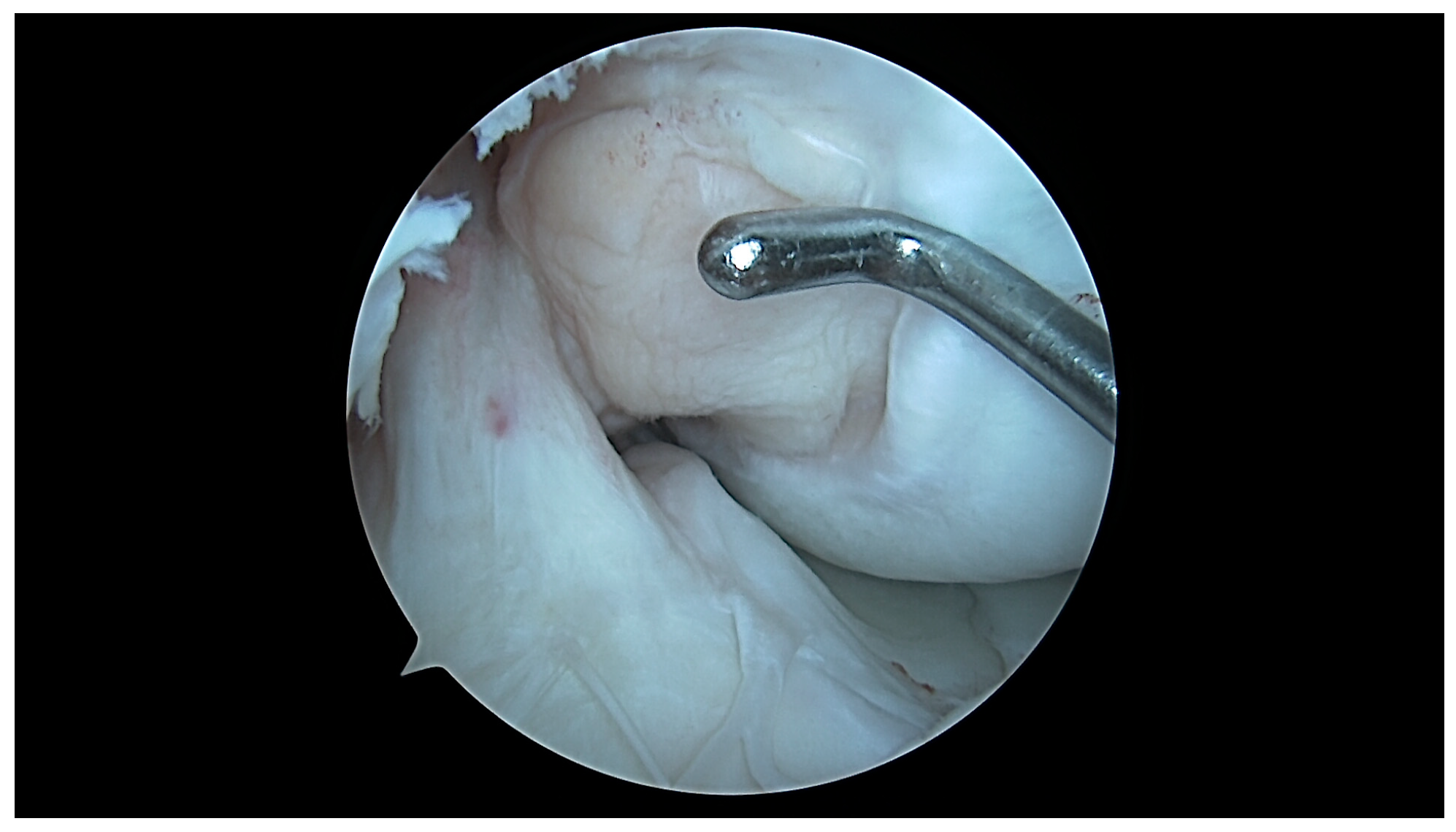
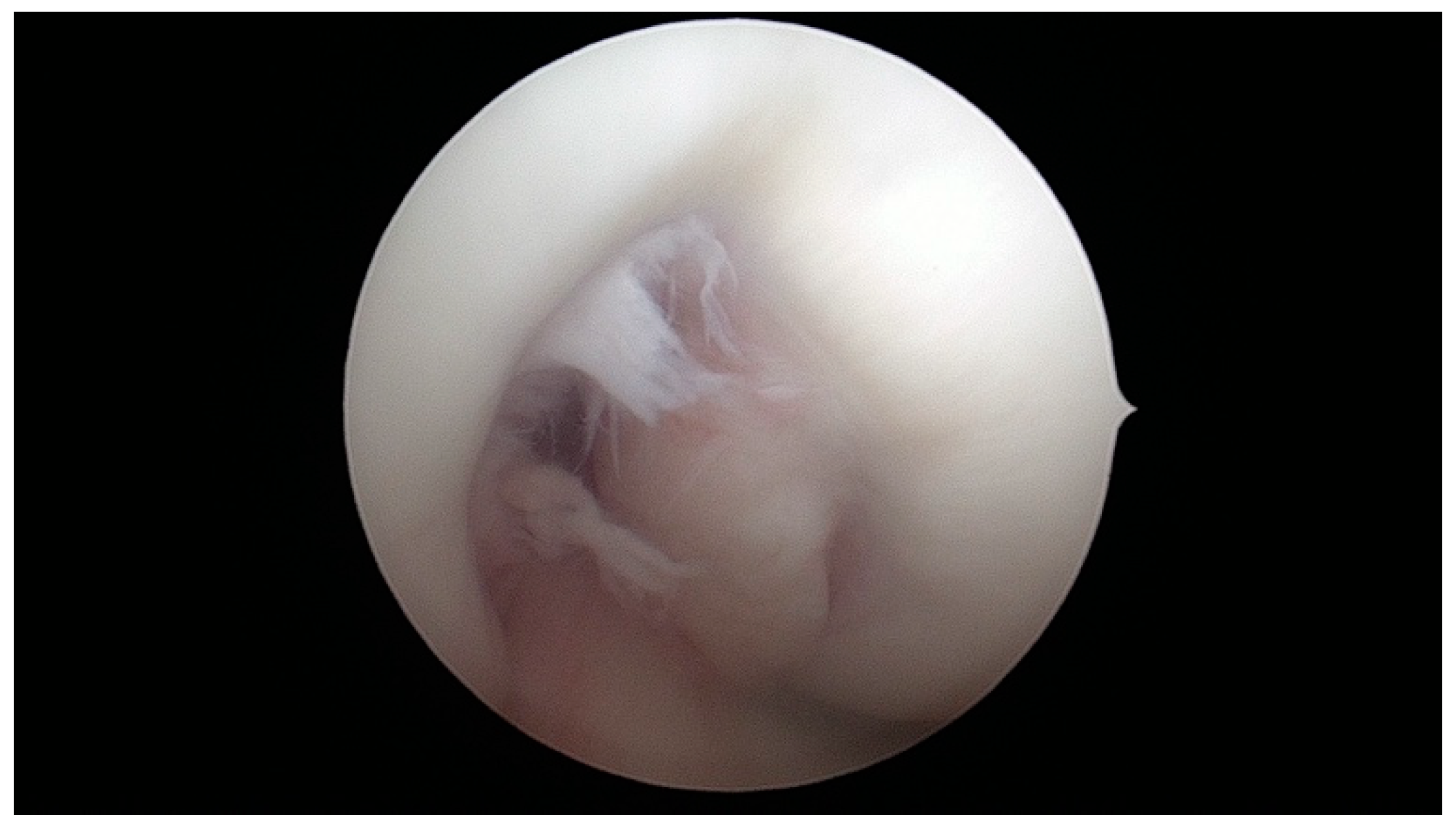
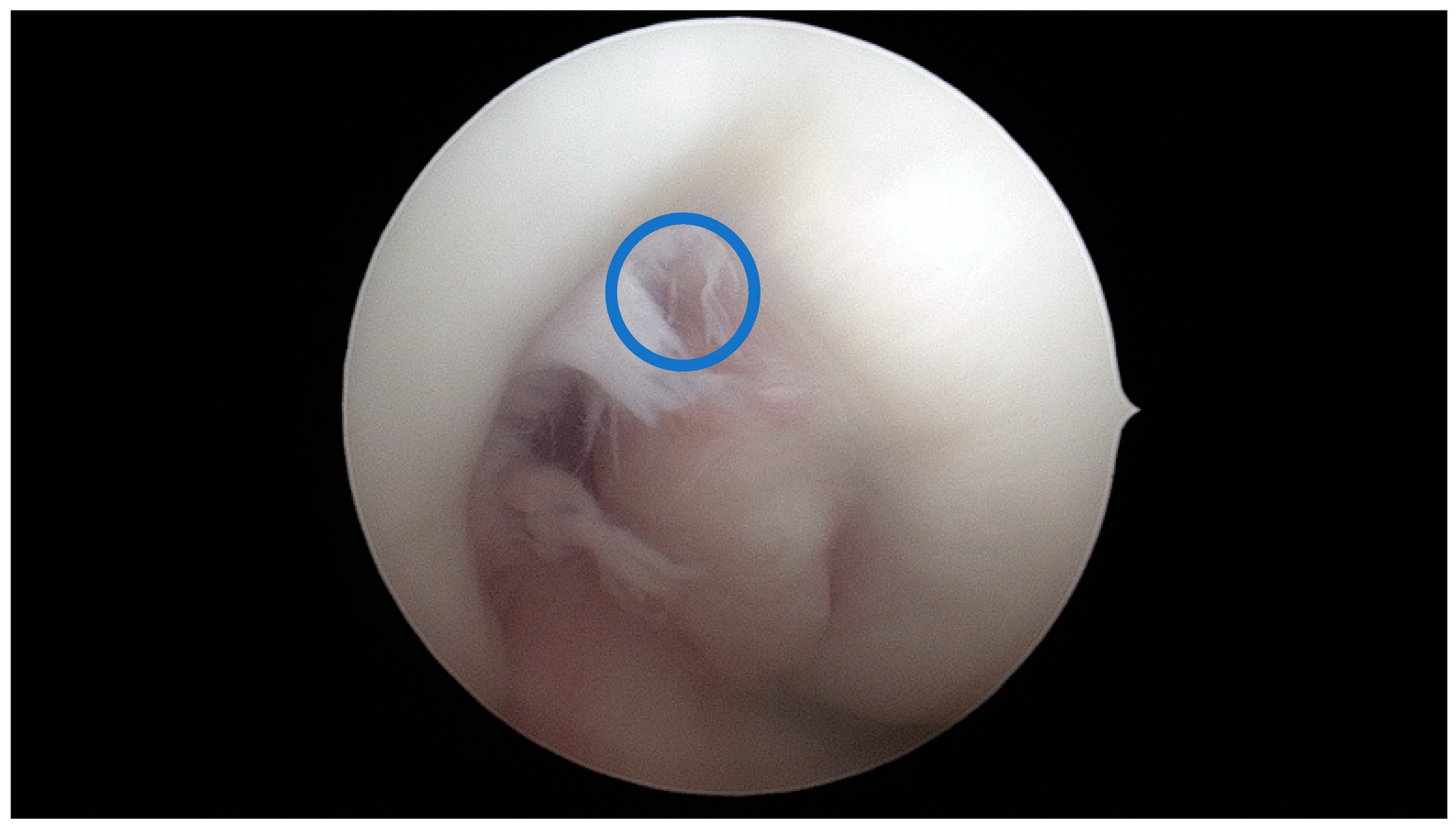
4.1. U-Shaped Notch
4.2. A/W Shaped Notch
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitney, D.C.; Sturnick, D.R.; Vacek, P.M.; DeSarno, M.J.; Gardner-Morse, M.; Tourville, T.W.; Smith, H.C.; Slauterbeck, J.R.; Johnson, R.J.; Shultz, S.J.; et al. Relationship between the risk of suffering a first-time noncontact ACL injury and geometry of the femoral notch and ACL: A prospective cohort study with a nested case-control analysis. Am. J. Sports Med. 2014, 42, 1796–1805. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Gao, F.; Sun, W.; Li, Z.; Wu, X.; Shi, L.; Xu, X.; Li, T.; Fan, X.; Li, C.; et al. Morphometric characteristics of the knee are associated with the injury of the meniscus. J. Orthop. Surg. Res. 2022, 17, 498. [Google Scholar] [CrossRef] [PubMed]
- Jaibaji, R.; Khaleel, F.; Jaibaji, M.; Volpin, A. Outcomes of Meniscal Repair in Patients Aged 40 and Above: A Systematic Review. J. Clin. Med. 2023, 12, 6922. [Google Scholar] [CrossRef] [PubMed]
- Iijima, H.; Shimoura, K.; Aoyama, T.; Takahashi, M. Biomechanical characteristics of stair ambulation in patients with knee OA: A systematic review with meta-analysis toward a better definition of clinical hallmarks. Gait Posture 2018, 62, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Schäfer, L.; Bell, A.; Weber, C.D.; Vecchio, G.; Maffulli, N. Meniscectomy is associated with a higher rate of osteoarthritis compared to meniscal repair following acute tears: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5485–5495. [Google Scholar] [CrossRef] [PubMed]
- Laible, C.; Stein, D.A.; Kiridly, D.N. Meniscal repair. J. Am. Acad. Orthop. Surg. 2013, 21, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-K.; Lin, L.-C.; Sun, Y.-N.; Lai, C.-S.; Chen, C.-H.; Kao, C.-Y. Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors. Diagnostics 2021, 11, 419. [Google Scholar] [CrossRef]
- Gornitzky, A.L.; Lott, A.; Yellin, J.L.; Fabricant, P.D.; Lawrence, J.T.; Ganley, T.J. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 2716–2723. [Google Scholar] [CrossRef]
- Heard, W.M.; VanSice, W.C.; Savoie, F.H., 3rd. Anterior cruciate ligament tears for the primary care sports physician: What to know on the field and in the office. Phys. Sportsmed. 2015, 43, 432–439. [Google Scholar] [CrossRef]
- Smith, H.C.; Vacek, P.; Johnson, R.J.; Slauterbeck, J.R.; Hashemi, J.; Shultz, S.; Beynnon, B.D. Risk factors for anterior cruciate ligament injury: A review of the literature. Part 1: Neuromuscular and anatomic risk. Sports Health 2012, 4, 69–78. [Google Scholar] [CrossRef]
- Javed Awan, M.; Mohd Rahim, M.S.; Salim, N.; Mohammed, M.A.; Garcia-Zapirain, B.; Abdulkareem, K.H. Efficient Detection of Knee Anterior Cruciate Ligament from Magnetic Resonance Imaging Using Deep Learning Approach. Diagnostics 2021, 11, 105. [Google Scholar] [CrossRef] [PubMed]
- Fontanella, C.G.; Belluzzi, E.; Pozzuoli, A.; Scioni, M.; Olivotto, E.; Reale, D.; Ruggieri, P.; De Caro, R.; Ramonda, R.; Carniel, E.L.; et al. Exploring Anatomo-Morphometric Characteristics of Infrapatellar, Suprapatellar Fat Pad, and Knee Ligaments in Osteoarthritis Compared to Post-Traumatic Lesions. Biomedicines 2022, 10, 1369. [Google Scholar] [CrossRef] [PubMed]
- Weninger, P.; Thallinger, C.; Chytilek, M.; Hanel, Y.; Steffel, C.; Karimi, R.; Feichtinger, X. Extracorporeal Shockwave Therapy Improves Outcome after Primary Anterior Cruciate Ligament Reconstruction with Hamstring Tendons. J. Clin. Med. 2023, 12, 3350. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Cigolotti, A.; Zonta, F.; Belluzzi, E.; Ruggieri, P. ACL reconstruction using a bone patellar tendon bone (BPTB) allograft or a hamstring tendon autograft (GST): A single-center comparative study. Acta Biomed. 2019, 90, 109–117. [Google Scholar] [CrossRef] [PubMed]
- MacDessi, S.J.; Griffiths-Jones, W.; Harris, I.A.; Bellemans, J.; Chen, D.B. Coronal Plane Alignment of the Knee (CPAK) classification. Bone Jt. J. 2021, 103, 329–337. [Google Scholar] [CrossRef]
- MacDessi, S.J.; Griffiths-Jones, W.; Harris, I.A.; Bellemans, J.; Chen, D.B. The arithmetic HKA (aHKA) predicts the constitutional alignment of the arthritic knee compared to the normal contralateral knee. Bone Jt. Open. 2020, 1, 339–345. [Google Scholar] [CrossRef]
- Calliess, T.; Bauer, K.; Stukenborg-Colsman, C.; Windhagen, H.; Budde, S.; Ettinger, M. Psi kinematic versus non-PSI mechanical alignment in total knee arthroplasty: A prospective, randomized study. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Hutt, J.R.B.; LeBlanc, M.-A.; Massé, V.; Lavigne, M.; Vendittoli, P.-A. Kinematic TKA using navigation: Surgical technique and initial results. Orthop. Traumatol. Surg. Res. 2016, 102, 99–104. [Google Scholar] [CrossRef]
- Bali, K.; Walker, P.; Bruce, W. Custom-fit total knee arthroplasty: Our initial experience in 32 knees. J. Arthroplast. 2012, 27, 1149–1154. [Google Scholar] [CrossRef]
- Howell, S.M.; Papadopoulos, S.; Kuznik, K.T.; Hull, M.L. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2271–2280. [Google Scholar] [CrossRef]
- Almaawi, A.M.; Hutt, J.R.B.; Masse, V.; Lavigne, M.; Vendittoli, P.-A. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J. Arthroplast. 2017, 32, 2133–2140. [Google Scholar] [CrossRef] [PubMed]
- McEwen, P.; Balendra, G.; Doma, K. Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Jt. J. 2019, 101, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Waterson, H.B.; Clement, N.D.; Eyres, K.S.; Mandalia, V.I.; Toms, A.D. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: A prospective randomised control trial. Bone Jt. J. 2016, 98, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Griffiths-Jones, W.; Chen, D.B.; Harris, I.A.; Bellemans, J.; MacDessi, S.J. Arithmetic hip-knee-ankle angle (aHKA): An algorithm for estimating constitutional lower limb alignment in the arthritic patient population. Bone Jt. Open 2021, 2, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Victor, J.M.K.; Bassens, D.; Bellemans, J.; Gürsu, S.; Dhollander, A.A.M.; Verdonk, P.C.M. Constitutional varus does not affect joint line orientation in the coronal plane. Clin. Orthop. Relat. Res. 2014, 472, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Moser, L.B.; Amsler, F.; Behrend, H.; Leclerq, V.; Hess, S. Functional knee phenotypes: A novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1394–1402. [Google Scholar] [CrossRef]
- Hutt, J.; Massé, V.; Lavigne, M.; Vendittoli, P.-A. Functional joint line obliquity after kinematic total knee arthroplasty. Int. Orthop. 2016, 40, 29–34. [Google Scholar] [CrossRef]
- Chow, J.C.; Breslauer, L. The use of intraoperative sensors significantly increases the patient-reported rate of improvement in primary total knee arthroplasty. Orthopedics 2017, 40, e648–e651. [Google Scholar] [CrossRef]
- Nag, H.L.; Jain, G.; Vijayakumar, V.; Jacob, T.G.; Sonai, M.; Lalwani, S. Femoral Intercondylar Notch: Gross Anatomy and Histology of the Connective Tissue Lining of its Roof: A Pilot Study. Surg. Radiol. Anat. 2021, 43, 1659–1666. [Google Scholar] [CrossRef]


| Parameter | Total N = 65 | Male Gender N = 33 | Female Gender N = 32 | p-Value |
|---|---|---|---|---|
| Age, years | 35 (18–50) | 34 (18–50) | 35 (18–50) | 0.680 |
| ACL area, cm2 | 0.48 (0.2–0.8) | 0.55 (0.3–0.8) | 0.41 (0.2–0.7) | 0.0002 |
| aICN area, cm2 | 0.75 (0.15–3.60) | 0.96 (0.22–3.60) | 0.52 (0.15–1.68) | 0.0008 |
| ICN width, mm | 22.23 (12.80–31.00) | 23.87 (19.00–31.00) | 20.53 (12.80–28.00) | <0.0001 |
| ICN A form, N (%) | 23 (35.38%) | 6 (26.09%) | 17 (73.91%) | 0.004 |
| ICN W form, N (%) | 17 (26.15%) | 8 (47.05%) | 9 (52.95%) | 0.720 |
| ICN U form, N (%) | 25 (38.46%) | 19 (76%) | 6 (24%) | 0.020 |
| LTI, ° | 19.15 (3.00–31.00) | 21.58 (10.00–30.00) | 16.66 (3.00–31.00) | 0.0009 |
| Intercondylar Notch | ACL Area | aICN Area | Rho | p-Value |
|---|---|---|---|---|
| Total group (N = 65) | ||||
| A-shape (n1 = 23; 35.4%), cm2 | 0.40 (0.20–0.80) | 0.47 (0.15–0.95) | 0.820 | <0.001 |
| W-shape (n2 = 17; 26.2%), cm2 | 0.40 (0.30–0.80) | 0.37 (0.15–0.81) | 0.608 | 0.010 |
| U-shape (n3 = 25; 38.5%), cm2 | 0.50 (0.20–0.80) | 1.16 (0.57–3.60) | 0.416 | 0.036 |
| Parameter | A-Shape (N = 23) | W-Shape (N = 17) | U-Shape (N = 25) | p-Value | Post-Hoc |
|---|---|---|---|---|---|
| Age, median, years | 33 | 32 | 37 | 0.877 | - |
| ACL area, cm2 | 0.40 (0.20–0.80) | 0.40 (0.30–0.80) | 0.50 (0.20–0.80) | 0.011 | A-U |
| aICN area, cm2 | 0.47 (0.15–0.95) | 0.37 (0.15–0.81) | 1.16 (0.57–3.60) | <0.001 | A-U, W-U |
| ICN width, mm | 22 (13–28) | 22 (15–26) | 24 (17–31) | 0.001 | A-U, W-U |
| LTI, ° | 18 (7–30) | 22 (7–31) | 20 (3–29) | 0.308 | - |
| Parameter | A-Shape (N = 23) | W-Shape (N = 17) | U-Shape (N = 25) | p-Value |
|---|---|---|---|---|
| Male gender, (%) | (26.1) | (47.1) | (76.0) | 0.002 |
| Internal chondral lesions, (%) | (21.7) | (5.9) | (20.0) | 0.364 |
| External chondral lesions,(%) | (0.0) | (17.6) | (12.0) | 0.135 |
| Internal meniscal lesions, (%) | (26.1) | (29.4) | (64.0) | 0.014 |
| External meniscal lesions, (%) | (0.0) | (35.3) | (16.0) | 0.009 |
| Patellar chondral lesions, (%) | (13.0) | (11.8) | (28.0) | 0.291 |
| Patella alta, (%) | (13.0) | (5.9) | (8.0) | 0.715 |
| Trochlear dysplasia, (%) | (13.0) | (17.6) | (12.0) | 0.865 |
| No Lesions | Lesions Detected | p-Value | |
|---|---|---|---|
| Internal chondral lesions | (N = 54) | (N = 11) | |
| 0.39 (0.23–0.69) | 0.44 (0.31–0.59) | 0.128 | |
| External chondral lesions | (N = 59) | (N = 6) | |
| 0.40 (0.23–0.69) | 0.42 (0.30–0.61) | 0.691 | |
| Internal meniscal injuries | (N = 38) | (N = 27) | |
| 0.38 (0.23–0.69) | 0.46 (0.29–0.61) | 0.002 | |
| External meniscal injuries | (N = 55) | (N = 10) | |
| 0.40 (0.23–0.69) | 0.37 (0.30–0.61) | 0.730 | |
| Patellar chondral lesions | (N = 53) | (N = 12) | |
| 0.39 (0.23–0.69) | 0.47 (0.29–0.61) | 0.097 | |
| Patella alta | (N = 59) | (N = 6) | |
| 0.40 (0.24–0.69) | 0.40 (0.23–0.50) | 0.650 | |
| Trochlear dysplasia | (N = 56) | (N = 9) | |
| 0.40 (0.23–0.69) | 0.41 (0.24–0.61) | 0.887 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cernat, E.M.; Dima, A.; Popescu, C.; Neagu, A.; Betianu, C.; Moga, M.; Manolescu, L.S.C.; Barbilian, A. Anterior Intercondylar Notch Geometry in Relation to the Native Anterior Cruciate Ligament Size. J. Clin. Med. 2024, 13, 309. https://doi.org/10.3390/jcm13020309
Cernat EM, Dima A, Popescu C, Neagu A, Betianu C, Moga M, Manolescu LSC, Barbilian A. Anterior Intercondylar Notch Geometry in Relation to the Native Anterior Cruciate Ligament Size. Journal of Clinical Medicine. 2024; 13(2):309. https://doi.org/10.3390/jcm13020309
Chicago/Turabian StyleCernat, Eduard M., Alina Dima, Claudiu Popescu, Andrei Neagu, Cezar Betianu, Marius Moga, Loredana Sabina Cornelia Manolescu, and Adrian Barbilian. 2024. "Anterior Intercondylar Notch Geometry in Relation to the Native Anterior Cruciate Ligament Size" Journal of Clinical Medicine 13, no. 2: 309. https://doi.org/10.3390/jcm13020309
APA StyleCernat, E. M., Dima, A., Popescu, C., Neagu, A., Betianu, C., Moga, M., Manolescu, L. S. C., & Barbilian, A. (2024). Anterior Intercondylar Notch Geometry in Relation to the Native Anterior Cruciate Ligament Size. Journal of Clinical Medicine, 13(2), 309. https://doi.org/10.3390/jcm13020309







