Trends in Hospitalizations of Patients with Hepatitis C Virus in Poland between 2012 and 2022
Abstract
1. Introduction
2. Materials and Methods
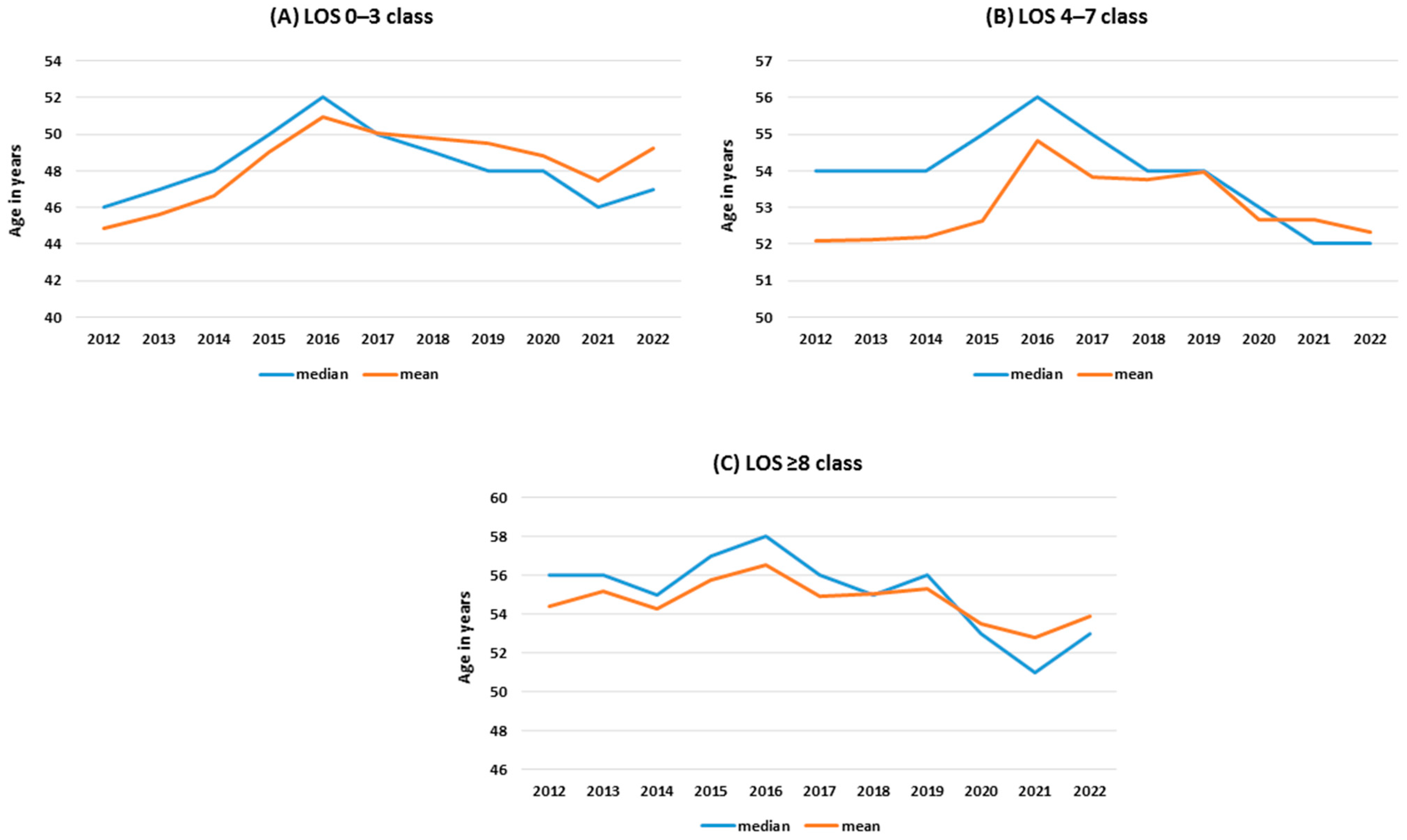
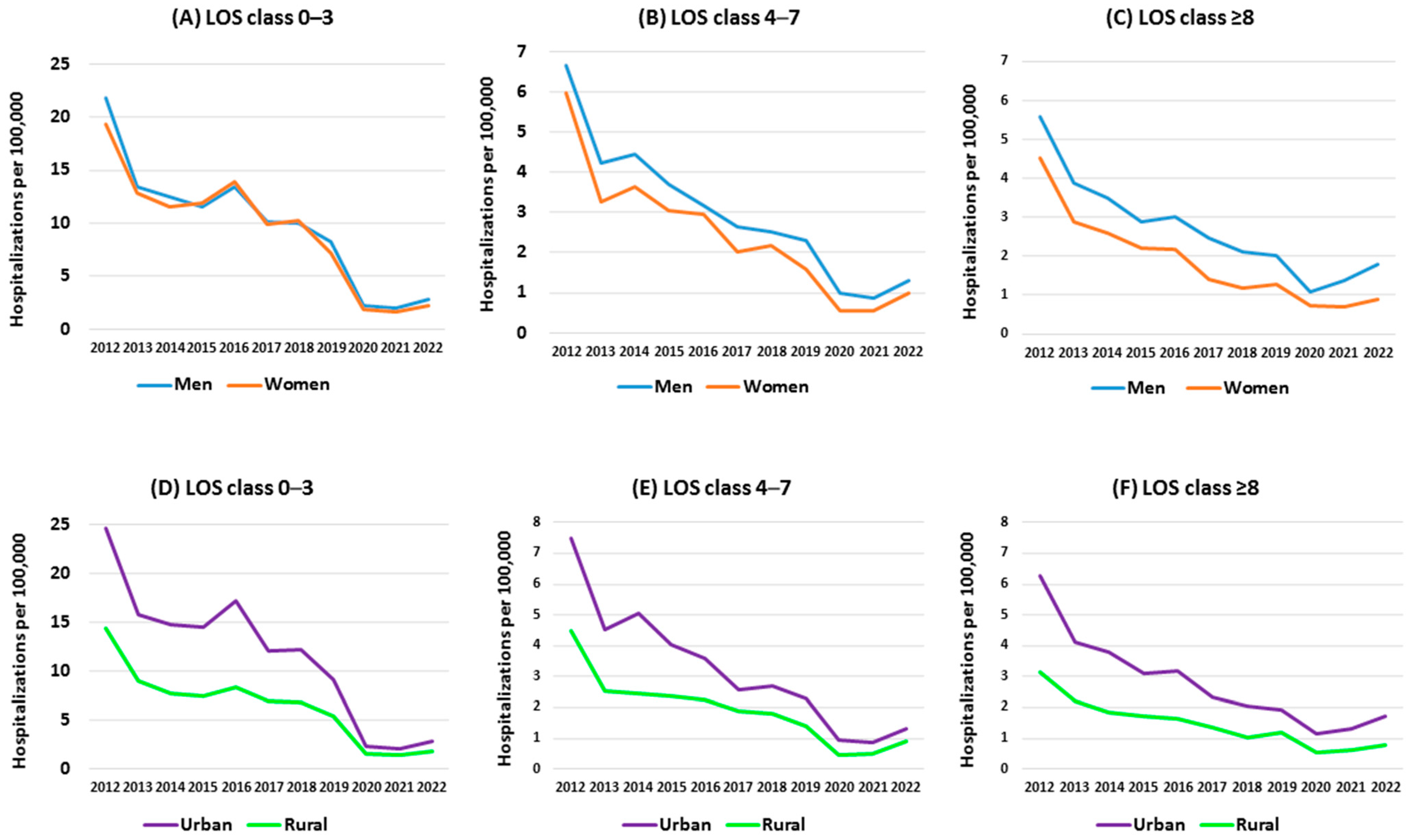
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Hepatitis C. Available online: https://www.who.int/news-room/fact-sheets/detail/hepatitis-c (accessed on 23 June 2024).
- Rzymski, P.; Jibril, A.T.; Rahmah, L.; Abarikwu, S.O.; Hashem, F.; Al Lawati, A.; Morrison, F.M.M.; Marquez, L.P.; Mohamed, K.; Khan, A.; et al. Is There Still Hope for the Prophylactic Hepatitis C Vaccine? A Review of Different Approaches. J. Med. Virol. 2024, 96, e29900. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Gastroenterology & Hepatology The Hunt for a Vaccine for Hepatitis C Virus Continues. Lancet Gastroenterol. Hepatol. 2021, 6, 253.
- Rzymski, P.; Brzdęk, M.; Dobrowolska, K.; Poniedziałek, B.; Murawska-Ochab, A.; Zarębska-Michaluk, D.; Flisiak, R. Like a Rolling Stone? A Review on Spontaneous Clearance of Hepatitis C Virus Infection. Viruses 2024, 16, 1386. [Google Scholar] [CrossRef]
- Ayoub, H.H.; Chemaitelly, H.; Omori, R.; Abu-Raddad, L.J. Hepatitis C Virus Infection Spontaneous Clearance: Has It Been Underestimated? Int. J. Infect. Dis. 2018, 75, 60–66. [Google Scholar] [CrossRef]
- Page, K.; Melia, M.T.; Veenhuis, R.T.; Winter, M.; Rousseau, K.E.; Massaccesi, G.; Osburn, W.O.; Forman, M.; Thomas, E.; Thornton, K.; et al. Randomized Trial of a Vaccine Regimen to Prevent Chronic HCV Infection. N. Engl. J. Med. 2021, 384, 541–549. [Google Scholar] [CrossRef]
- Shiffman, M.L. The next Wave of Hepatitis C Virus: The Epidemic of Intravenous Drug Use. Liver Int. 2018, 38, 34–39. [Google Scholar] [CrossRef]
- Gezer, F.; Howard, K.A.; Litwin, A.H.; Martin, N.K.; Rennert, L. Identification of Factors Associated with Opioid-Related and Hepatitis C Virus-Related Hospitalisations at the ZIP Code Area Level in the USA: An Ecological and Modelling Study. Lancet Public Health 2024, 9, e354–e364. [Google Scholar] [CrossRef]
- CDC. Clinical Screening and Diagnosis for Hepatitis C. 2023. Available online: https://www.cdc.gov/hepatitis-c/hcp/diagnosis-testing/index.html (accessed on 29 June 2024).
- WHO. New Recommendation on Hepatitis C Virus Testing and Treatment for People at Ongoing Risk of Infection. Available online: https://www.who.int/publications/i/item/9789240071872 (accessed on 13 September 2024).
- Stepanova, M.; Younossi, Z.M. Economic Burden of Hepatitis C Infection. Clin. Liver Dis. 2017, 21, 579–594. [Google Scholar] [CrossRef]
- Lam, L.; Carrieri, P.; Hejblum, G.; Bellet, J.; Bourlière, M.; Carrat, F. Real-world Economic Burden of Hepatitis C and Impact of Direct-acting Antivirals in France: A Nationwide Claims Data Analysis. Liver Int. 2024, 44, 1233–1242. [Google Scholar] [CrossRef]
- Hafez, T.A. Public Health and Economic Burden of Hepatitis C Infection in Developing Countries. In Hepatitis C in Developing Countries; Elsevier: Amsterdam, The Netherlands, 2018; pp. 25–32. ISBN 9780128032336. [Google Scholar]
- Bhattacharya, D.; Aronsohn, A.; Price, J.; Lo Re, V.; AASLD-IDSA HCV Guidance Panel. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin. Infect. Dis. 2023, ciad319. [Google Scholar] [CrossRef]
- Tomasiewicz, K.; Flisiak, R.; Jaroszewicz, J.; Małkowski, P.; Pawłowska, M.; Piekarska, A.; Simon, K.; Zarębska-Michaluk, D. Recommendations of the Polish Group of Experts for HCV for the Treatment of Hepatitis C in 2023. Clin. Exp. Hepatol. 2023, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Petkevičienė, J.; Voeller, A.; Čiupkevičienė, E.; Razavi-Shearer, D.; Liakina, V.; Jančorienė, L.; Kazėnaitė, E.; Zaksas, V.; Urbonas, G.; Kupčinskas, L. Hepatitis C Screening in Lithuania: First-Year Results and Scenarios for Achieving WHO Elimination Targets. BMC Public Health 2024, 24, 1055. [Google Scholar] [CrossRef] [PubMed]
- Walewska-Zielecka, B.; Religioni, U.; Juszczyk, G.; Wawrzyniak, Z.M.; Czerw, A.; Soszyński, P.; Fronczak, A. Anti-Hepatitis C Virus Seroprevalence in the Working Age Population in Poland, 2004 to 2014. Euro Surveill. 2017, 22, 30441. [Google Scholar] [CrossRef]
- Razavi, H.; Sanchez Gonzalez, Y.; Yuen, C.; Cornberg, M. Global Timing of Hepatitis C Virus Elimination in High-income Countries. Liver Int. 2020, 40, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Tronina, O.; Panczyk, M.; Zarębska-Michaluk, D.; Gotlib, J.; Małkowski, P. Global Elimination of HCV—Why Is Poland Still so Far from the Goal? Viruses 2023, 15, 2067. [Google Scholar] [CrossRef]
- Genowska, A.; Zarębska-Michaluk, D.; Strukcinskiene, B.; Razbadauskas, A.; Moniuszko-Malinowska, A.; Jurgaitis, J.; Flisiak, R. Changing Epidemiological Patterns of Infection and Mortality Due to Hepatitis C Virus in Poland. J. Clin. Med. 2023, 12, 3922. [Google Scholar] [CrossRef]
- John-Baptiste, A.A.; Tomlinson, G.; Hsu, P.C.; Krajden, M.; Heathcote, E.J.; Laporte, A.; Yoshida, E.M.; Anderson, F.H.; Krahn, M.D. Sustained Responders Have Better Quality of Life and Productivity Compared with Treatment Failures Long after Antiviral Therapy for Hepatitis C. Am. J. Gastroenterol. 2009, 104, 2439–2448. [Google Scholar] [CrossRef]
- Su, J.; Brook, R.A.; Kleinman, N.L.; Corey-Lisle, P. The Impact of Hepatitis C Virus Infection on Work Absence, Productivity, and Healthcare Benefit Costs. Hepatology 2010, 52, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, H.; Silva, M. Health-Related Quality of Life in Chronic Hepatitis C. GE Port. J. Gastroenterol. 2017, 24, 55–57. [Google Scholar] [CrossRef]
- Chen, S.L.; Morgan, T.R. The Natural History of Hepatitis C Virus (HCV) Infection. Int. J. Med. Sci. 2006, 3, 47–52. [Google Scholar] [CrossRef]
- Aly, A.; Ronnebaum, S.; Patel, D.; Doleh, Y.; Benavente, F. Epidemiologic, Humanistic and Economic Burden of Hepatocellular Carcinoma in the USA: A Systematic Literature Review. Hepat. Oncol. 2020, 7, HEP27. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Picchio, C.A.; Colombo, M. Hepatocellular Carcinoma Prevention in the Era of Hepatitis C Elimination. Int. J. Mol. Sci. 2023, 24, 14404. [Google Scholar] [CrossRef] [PubMed]
- Brzdęk, M.; Zarębska-Michaluk, D.; Invernizzi, F.; Cilla, M.; Dobrowolska, K.; Flisiak, R. Decade of Optimizing Therapy with Direct-Acting Antiviral Drugs and the Changing Profile of Patients with Chronic Hepatitis C. World J. Gastroenterol. 2023, 29, 949–966. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, T.; Miyaaki, H.; Miuma, S.; Motoyoshi, Y.; Yamashima, M.; Yamamichi, S.; Koike, M.; Nakano, Y.; Honda, T.; Yajima, H.; et al. Direct-Acting Antivirals Improved the Quality of Life, Ameliorated Disease-Related Symptoms, and Augmented Muscle Volume Three Years Later in Patients with Hepatitis C Virus. Intern. Med. 2020, 59, 2653–2660. [Google Scholar] [CrossRef] [PubMed]
- Roguljic, H.; Nincevic, V.; Bojanic, K.; Kuna, L.; Smolic, R.; Vcev, A.; Primorac, D.; Vceva, A.; Wu, G.Y.; Smolic, M. Impact of DAA Treatment on Cardiovascular Disease Risk in Chronic HCV Infection: An Update. Front. Pharmacol. 2021, 12, 678546. [Google Scholar] [CrossRef] [PubMed]
- Terrault, N.A. Care of Patients Following Cure of Hepatitis C Virus Infection. Gastroenterol. Hepatol. 2018, 14, 629–634. [Google Scholar]
- Lynch, E.N.; Russo, F.P. Outcomes and Follow-up after Hepatitis C Eradication with Direct-Acting Antivirals. J. Clin. Med. 2023, 12, 2195. [Google Scholar] [CrossRef]
- Negro, F. Residual Risk of Liver Disease after Hepatitis C Virus Eradication. J. Hepatol. 2021, 74, 952–963. [Google Scholar] [CrossRef]
- Leal, C.; Strogoff-de-Matos, J.; Theodoro, C.; Teixeira, R.; Perez, R.; Guaraná, T.; de Tarso Pinto, P.; Guimarães, T.; Artimos, S. Incidence and Risk Factors of Hepatocellular Carcinoma in Patients with Chronic Hepatitis C Treated with Direct-Acting Antivirals. Viruses 2023, 15, 221. [Google Scholar] [CrossRef]
- Torre, P.; Coppola, R.; Masarone, M.; Persico, M. Country-Wide HCV Elimination Strategies Need to Reach Older Patients in the General Population: The Italian Experience. Viruses 2023, 15, 2199. [Google Scholar] [CrossRef]
- Lin, T.-Y.; Jen, H.-H.; Hu, T.-H.; Yao, Y.-C.; Chen, T.H.-H.; Yen, A.M.-F.; Yeh, Y.-P. Planning, Implementing, and Evaluating Hepatitis C Virus Elimination via Collaborative Community-Based Care Cascade: Age–Period–Cohort Model for Estimating Demand from Antecedent Anti-HCV Survey. Hepatol. Int. 2024, 18, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Rincon, J.-M.; Pinargote-Celorio, H.; de Mendoza, C.; Ramos-Belinchón, C.; Barreiro, P.; Gómez-Gallego, F.; Corral, O.; Soriano, V. Hepatitis C Hospitalizations in Spain and Impact of New Curative Antiviral Therapies. J. Viral Hepat. 2022, 29, 777–784. [Google Scholar] [CrossRef] [PubMed]
- GUS Publications. Available online: https://stat.gov.pl/en/publications/search.html (accessed on 29 August 2024).
- Brzdęk, M.; Zarębska-Michaluk, D.; Rzymski, P.; Lorenc, B.; Kazek, A.; Tudrujek-Zdunek, M.; Janocha-Litwin, J.; Mazur, W.; Dybowska, D.; Berak, H.; et al. Changes in Characteristics of Patients with Hepatitis C Virus-Related Cirrhosis from the Beginning of the Interferon-Free Era. World J. Gastroenterol. 2023, 29, 2015–2033. [Google Scholar] [CrossRef]
- Flisiak, R.; Zarębska-Michaluk, D.; Frankova, S.; Grgurevic, I.; Hunyady, B.; Jarcuska, P.; Kupčinskas, L.; Makara, M.; Simonova, M.; Sperl, J.; et al. Is Elimination of HCV in 2030 Realistic in Central Europe. Liver Int. 2021, 41, 56–60. [Google Scholar] [CrossRef]
- ECDC. Annual Epidemiological Report for 2022. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/HEPC_AER_2022.pdf (accessed on 29 August 2024).
- Levinsson, A.; Zolopa, C.; Vakili, F.; Udhesister, S.; Kronfli, N.; Maheu-Giroux, M.; Bruneau, J.; Valerio, H.; Bajis, S.; Read, P.; et al. Sex and Gender Differences in Hepatitis C Virus Risk, Prevention, and Cascade of Care in People Who Inject Drugs: Systematic Review and Meta-Analysis. EClinicalMedicine 2024, 72, 102596. [Google Scholar] [CrossRef]
- Hofmeister, M.G.; Zhong, Y.; Moorman, A.C.; Samuel, C.R.; Teshale, E.H.; Spradling, P.R. Temporal Trends in Hepatitis C–Related Hospitalizations, United States, 2000–2019. Clin. Infect. Dis. 2023, 77, 1668–1675. [Google Scholar] [CrossRef] [PubMed]
- Janik-Koncewicz, K.; Zatoński, W.; Zatońska, K.; Stępnicka, Z.; Basiak-Rasała, A.; Zatoński, M.; Połtyn-Zaradna, K. Cigarette Smoking in Poland in 2019: The Continuing Decline in Smoking Prevalence. J. Health Inequal. 2020, 6, 87–94. [Google Scholar] [CrossRef]
- Klimkiewicz, A.; Jakubczyk, A.; Mach, A.; Abramowska, M.; Szczypiński, J.; Berent, D.; Skrzeszewski, J.; Witkowski, G.; Wojnar, M. Psychometric Properties of the Polish Version of the Alcohol Use Disorders Identification Test (AUDIT). Drug Alcohol Depend. 2021, 218, 108427. [Google Scholar] [CrossRef] [PubMed]
- Llamosas-Falcón, L.; Shield, K.D.; Gelovany, M.; Hasan, O.S.M.; Manthey, J.; Monteiro, M.; Walsh, N.; Rehm, J. Impact of Alcohol on the Progression of HCV-Related Liver Disease: A Systematic Review and Meta-Analysis. J. Hepatol. 2021, 75, 536–546. [Google Scholar] [CrossRef]
- Chuang, S.-C.; Lee, Y.-C.A.; Hashibe, M.; Dai, M.; Zheng, T.; Boffetta, P. Interaction between Cigarette Smoking and Hepatitis B and C Virus Infection on the Risk of Liver Cancer: A Meta-Analysis. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1261–1268. [Google Scholar] [CrossRef]
- Hezode, C. Impact of Smoking on Histological Liver Lesions in Chronic Hepatitis C. Gut 2003, 52, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Gajewska, D.; Harton, A. Current Nutritional Status of the Polish Population—Focus on Body Weight Status. J. Health Inequal. 2023, 9, 154–160. [Google Scholar] [CrossRef]
- Ohki, T.; Tateishi, R.; Sato, T.; Masuzaki, R.; Imamura, J.; Goto, T.; Yamashiki, N.; Yoshida, H.; Kanai, F.; Kato, N.; et al. Obesity Is an Independent Risk Factor for Hepatocellular Carcinoma Development in Chronic Hepatitis C Patients. Clin. Gastroenterol. Hepatol. 2008, 6, 459–464. [Google Scholar] [CrossRef]
- Aisyah, D.N.; Shallcross, L.; Hully, A.J.; O’Brien, A.; Hayward, A. Assessing Hepatitis C Spontaneous Clearance and Understanding Associated Factors—A Systematic Review and Meta-analysis. J. Viral Hepat. 2018, 25, 680–698. [Google Scholar] [CrossRef] [PubMed]
- Bakr, I. Higher Clearance of Hepatitis C Virus Infection in Females Compared with Males. Gut 2005, 55, 1183–1187. [Google Scholar] [CrossRef]
- Guy, J.; Peters, M.G. Liver Disease in Women: The Influence of Gender on Epidemiology, Natural History, and Patient Outcomes. Gastroenterol. Hepatol. 2013, 9, 633–639. [Google Scholar]
- Seeff, L.B. Natural History of Chronic Hepatitis C. Hepatology 2002, 36, s35–s46. [Google Scholar]
- Duncan, I.; Habecker, P.; Hautala, D.; Khan, B.; Dombrowski, K. Injection-Related Hepatitis C Serosorting Behaviors among People Who Inject Drugs: An Urban/Rural Comparison. J. Ethn. Subst. Abus. 2019, 18, 578–593. [Google Scholar] [CrossRef]
- Wenz, B.; the DRUCK Study Group; Nielsen, S.; Gassowski, M.; Santos-Hövener, C.; Cai, W.; Ross, R.S.; Bock, C.-T.; Ratsch, B.-A.; Kücherer, C.; et al. High Variability of HIV and HCV Seroprevalence and Risk Behaviours among People Who Inject Drugs: Results from a Cross-Sectional Study Using Respondent-Driven Sampling in Eight German Cities (2011–2014). BMC Public Health 2016, 16, 927. [Google Scholar] [CrossRef]
- Thomadakis, C.; Gountas, I.; Duffell, E.; Gountas, K.; Bluemel, B.; Seyler, T.; Pericoli, F.M.; Kászoni-Rückerl, I.; El-Khatib, Z.; Busch, M.; et al. Prevalence of Chronic HCV Infection in EU/EEA Countries in 2019 Using Multiparameter Evidence Synthesis. Lancet Reg. Health Eur. 2024, 36, 100792. [Google Scholar] [CrossRef]
- Chromy, D.; Bauer, D.J.M.; Simbrunner, B.; Jachs, M.; Hartl, L.; Schwabl, P.; Schwarz, C.; Rieger, A.; Grabmeier-Pfistershammer, K.; Trauner, M.; et al. The “Viennese Epidemic” of Acute HCV in the Era of Direct-Acting Antivirals. J. Viral Hepat. 2022, 29, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Jin, F.; Dore, G.J.; Matthews, G.; Luhmann, N.; Macdonald, V.; Bajis, S.; Baggaley, R.; Mathers, B.; Verster, A.; Grulich, A.E. Prevalence and Incidence of Hepatitis C Virus Infection in Men Who Have Sex with Men: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 39–56. [Google Scholar] [CrossRef] [PubMed]
- Binson, D.; Michaels, S.; Stall, R.; Coates, T.J.; Gagnon, J.H.; Catania, J.A. Prevalence and Social Distribution of Men Who Have Sex with Men: United States and Its Urban Centers. J. Sex Res. 1995, 32, 245–254. [Google Scholar]
- Kakietek, J.; Sullivan, P.S.; Heffelfinger, J.D. You’ve Got Male: Internet Use, Rural Residence, and Risky Sex in Men Who Have Sex with Men Recruited in 12 U.s. Cities. AIDS Educ. Prev. 2011, 23, 118–127. [Google Scholar] [CrossRef]
- Charest, M.; Razmjou, S.; O’Byrne, P.; MacPherson, P. A Survey Study to Determine Health Disparities among Men Who Have Sex with Men in Eastern Ontario: Looking beyond Sexual Risk and the Gay, Urban Core. J. Mens Health 2023, 19, 58–69. [Google Scholar] [CrossRef]
- Mahajan, R.; Midha, V.; Goyal, O.; Mehta, V.; Narang, V.; Kaur, K.; Singh, A.; Singh, D.; Bhanot, R.; Sood, A. Clinical Profile of Hepatitis C Virus Infection in a Developing Country: India. J. Gastroenterol. Hepatol. 2018, 33, 926–933. [Google Scholar] [CrossRef]
- Flisiak, R.; Frankova, S.; Grgurevic, I.; Hunyady, B.; Jarcuska, P.; Kupčinskas, L.; Makara, M.; Simonova, M.; Sperl, J.; Tolmane, I.; et al. How Close Are We to Hepatitis C Virus Elimination in Central Europe? Clin. Exp. Hepatol. 2020, 6, 1–8. [Google Scholar] [CrossRef]
- Dobrowolska, K.; Brzdęk, M.; Rzymski, P.; Flisiak, R.; Pawłowska, M.; Janczura, J.; Brdzęk, K.; Zarębska-Michaluk, D. Revolutionizing Hepatitis C Treatment: Next-Gen Direct-Acting Antivirals. Expert Opin. Pharmacother. 2024, 25, 833–852. [Google Scholar] [CrossRef]
- Manns, M.P.; Maasoumy, B. Breakthroughs in Hepatitis C Research: From Discovery to Cure. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 533–550. [Google Scholar] [CrossRef]
- Zakrzewska, K.; Szmulik, K.; Stępień, M.; Rosińska, M. Hepatitis C in Poland in 2015. Przegl. Epidemiol. 2015, 71, 363–371. [Google Scholar]
- Sander, G.; Shirley-Beavan, S.; Stone, K. The Global State of Harm Reduction in Prisons. J. Correct. Health Care 2019, 25, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, M.; Poojari, P.G.; Rashid, M.; Nair, S.; Pulikkel Chandran, V.; Thunga, G. Impact of COVID-19 Pandemic on Medicine Supply Chain for Patients with Chronic Diseases: Experiences of the Community Pharmacists. Clin. Epidemiol. Glob. Health 2023, 20, 101243. [Google Scholar] [CrossRef] [PubMed]
- Mrożek-Gąsiorowska, M.; Tambor, M. How COVID-19 Has Changed the Utilization of Different Health Care Services in Poland. BMC Health Serv. Res. 2024, 24, 105. [Google Scholar] [CrossRef]
- Rzymski, P.; Zarębska-Michaluk, D.; Parczewski, M.; Genowska, A.; Poniedziałek, B.; Strukcinskiene, B.; Moniuszko-Malinowska, A.; Flisiak, R. The Burden of Infectious Diseases throughout and after the COVID-19 Pandemic (2020–2023) and Russo-Ukrainian War Migration. J. Med. Virol. 2024, 96, e29651. [Google Scholar] [CrossRef]
- Anjum, M.R.; Chalmers, J.; Hamid, R.; Rajoriya, N. COVID-19: Effect on Gastroenterology and Hepatology Service Provision and Training: Lessons Learnt and Planning for the Future. World J. Gastroenterol. 2021, 27, 7625–7648. [Google Scholar] [CrossRef]
- Boettler, T.; Marjot, T.; Newsome, P.N.; Mondelli, M.U.; Maticic, M.; Cordero, E.; Jalan, R.; Moreau, R.; Cornberg, M.; Berg, T. Impact of COVID-19 on the Care of Patients with Liver Disease: EASL-ESCMID Position Paper after 6 Months of the Pandemic. JHEP Rep. 2020, 2, 100169. [Google Scholar] [CrossRef]
- Tuczyńska, M.; Staszewski, R.; Matthews-Kozanecka, M.; Żok, A.; Baum, E. Quality of the Healthcare Services during COVID-19 Pandemic in Selected European Countries. Front. Public Health 2022, 10, 870314. [Google Scholar] [CrossRef] [PubMed]
- Kondili, L.A.; Buti, M.; Riveiro-Barciela, M.; Maticic, M.; Negro, F.; Berg, T.; Craxì, A. Impact of the COVID-19 Pandemic on Hepatitis B and C Elimination: An EASL Survey. JHEP Rep. 2022, 4, 100531. [Google Scholar] [CrossRef]
- Polish Government. Coronavirus: Information and Recommendations. Available online: https://www.gov.pl/web/coronavirus/temporary-limitations (accessed on 5 February 2024).
- Duszczyk, M.; Górny, A.; Kaczmarczyk, P.; Kubisiak, A. War Refugees from Ukraine in Poland—One Year after the Russian Aggression. Socioeconomic Consequences and Challenges. Reg. Sci. Policy Pract. 2023, 15, 181–200. [Google Scholar] [CrossRef]
- Prusaczyk, A.; Bogdan, M.; Vinker, S.; Gujski, M.; Żuk, P.; Kowalska-Bobko, I.; Karczmarz, S.; Oberska, J.; Lewtak, K. Health Care Organization in Poland in Light of the Refugee Crisis Related to the Military Conflict in Ukraine. Int. J. Environ. Res. Public Health 2023, 20, 3831. [Google Scholar] [CrossRef]
- Devi, S. Ukrainian Health Authorities Adopt Hepatitis C Project. Lancet 2020, 396, 228. [Google Scholar] [CrossRef] [PubMed]
- Yakovleva, A.; Kovalenko, G.; Redlinger, M.; Smyrnov, P.; Tymets, O.; Korobchuk, A.; Kotlyk, L.; Kolodiazieva, A.; Podolina, A.; Cherniavska, S.; et al. Hepatitis C Virus in People with Experience of Injection Drug Use Following Their Displacement to Southern Ukraine before 2020. BMC Infect. Dis. 2023, 23, 446. [Google Scholar] [CrossRef] [PubMed]
- Fursa, O.; Reekie, J.; Kuzin, I.; Hetman, L.; Kryshchuk, A.; Starychenko, O.; Hrytsaiuk, N.; Khodus, I.; Nyzhnyk, A.; Rakhuba, V.; et al. Cross-sectional HIV and HCV Cascades of Care across the Regions of Ukraine between 2019 and 2020: Findings from the CARE Cohort. J. Int. AIDS Soc. 2023, 26, e26166. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, S.; Citarella, A.; Guida, A.; Conti, V.; Iannaccone, T.; Flacco, M.E.; Bravi, F.; Naccarato, C.; Piscitelli, A.; Piscitelli, R.; et al. The Inpatient Hospital Burden of Comorbidities in HCV-Infected Patients: A Population-Based Study in Two Italian Regions with High HCV Endemicity (The BaCH Study). PLoS ONE 2019, 14, e0219396. [Google Scholar] [CrossRef]

| Year | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | |
| N | 12,312 | 7785 | 7338 | 6798 | 7426 | 5539 | 5411 | 4318 | 1424 | 1337 | 1882 |
| Rate per 100,000 | 31.91 | 20.19 | 19.04 | 17.65 | 19.30 | 14.23 | 14.07 | 11.21 | 3.72 | 3.51 | 4.95 |
| LOS (Days) | Characteristics | ||||||
|---|---|---|---|---|---|---|---|
| N | % | Per 100,000 | n | % | Per 100,000 | Per 100,000 Ratio | |
| Sex | Men | Women | Men /Women | ||||
| 0–3 | 20,065 | 63.3 | 9.84 | 20,334 | 68.4 | 9.34 | 1.05 |
| 4–7 | 6096 | 19.2 | 2.99 | 4077 | 13.7 | 1.87 | 1.60 |
| ≥8 | 5524 | 17.4 | 2.71 | 5304 | 17.9 | 2.44 | 1.11 |
| Residence | Urban | Rural | Urban /Rural | ||||
| 0–3 | 29,583 | 65.9 | 11.66 | 10,816 | 65.6 | 6.44 | 1.81 |
| 4–7 | 8191 | 18.2 | 3.23 | 3209 | 19.5 | 1.91 | 1.69 |
| ≥8 | 7149 | 15.9 | 2.82 | 2452 | 14.9 | 1.46 | 1.93 |
| Year | LOS 0–3 | LOS 4–7 | LOS ≥8 |
|---|---|---|---|
| 2012 | 20.56 | 6.30 | 5.04 |
| 2013 | 13.09 | 3.73 | 3.37 |
| 2014 | 11.98 | 4.03 | 3.03 |
| 2015 | 11.74 | 3.37 | 2.54 |
| 2016 | 13.69 | 3.04 | 2.57 |
| 2017 | 9.99 | 2.31 | 1.93 |
| 2018 | 10.10 | 2.33 | 1.64 |
| 2019 | 7.66 | 1.94 | 1.62 |
| 2020 | 2.06 | 0.76 | 0.90 |
| 2021 | 1.77 | 0.71 | 1.03 |
| 2022 | 2.48 | 1.13 | 1.33 |
| ICD-10 Group | LOS 0–3 Days | LOS 4–7 Days | LOS ≥ 8 Days | Total | p-Value * | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | N | % | n | % | ||
| Certain infectious and parasitic diseases (A00–B99) | 1739 | 8.42 | 970 | 7.32 | 1734 | 10.62 | 4443 | 8.85 | <0.00001 |
| Neoplasms (C00–D48) | 1038 | 5.03 | 701 | 5.29 | 824 | 5.05 | 2563 | 5.10 | 0.51437 |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50–D89) | 2444 | 11.84 | 1888 | 14.25 | 1903 | 11.66 | 6235 | 12.42 | <0.00001 |
| Endocrine, nutritional and metabolic diseases (E00–E90) | 3093 | 14.98 | 1466 | 11.07 | 1396 | 8.55 | 5955 | 11.86 | <0.00001 |
| Mental, behavioral and Neurodevelopmental disorders (F00–F99) | 575 | 2.78 | 317 | 2.39 | 558 | 3.42 | 1450 | 2.89 | <0.00001 |
| Diseases of the nervous system (G00–G99) | 310 | 1.50 | 234 | 1.77 | 391 | 2.40 | 935 | 1.86 | <0.00001 |
| Diseases of the eye and adnexa and the ear and mastoid process (H00–H95) | 121 | 0.59 | 55 | 0.42 | 47 | 0.29 | 223 | 0.44 | 0.00009 |
| Diseases of the circulatory system (I00–I99) | 4258 | 20.62 | 2185 | 16.50 | 2617 | 16.03 | 9060 | 18.04 | <0.00001 |
| Diseases of the respiratory system (J00–J99) | 555 | 2.69 | 433 | 3.27 | 1025 | 6.28 | 2013 | 4.01 | <0.00001 |
| Diseases of the digestive system (K00–K93) | 4339 | 21.01 | 3499 | 26.42 | 3965 | 24.29 | 11,803 | 23.50 | <0.00001 |
| Diseases of the skin and subcutaneous tissue (L00–L99) | 260 | 1.26 | 232 | 1.75 | 288 | 1.76 | 780 | 1.55 | 0.00005 |
| Diseases of the musculoskeletal system and connective tissue (M00–M99) | 566 | 2.74 | 367 | 2.77 | 540 | 3.31 | 1473 | 2.93 | 0.00253 |
| Diseases of the genitourinary system (N00–N99) | 1350 | 6.54 | 898 | 6.78 | 1035 | 6.34 | 3283 | 6.54 | 0.31538 |
| Total | 20,648 | 100 | 13,245 | 100 | 16,323 | 100 | 50,216 | 100 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genowska, A.; Zarębska-Michaluk, D.; Dobrowolska, K.; Kanecki, K.; Goryński, P.; Tyszko, P.; Lewtak, K.; Rzymski, P.; Flisiak, R. Trends in Hospitalizations of Patients with Hepatitis C Virus in Poland between 2012 and 2022. J. Clin. Med. 2024, 13, 5618. https://doi.org/10.3390/jcm13185618
Genowska A, Zarębska-Michaluk D, Dobrowolska K, Kanecki K, Goryński P, Tyszko P, Lewtak K, Rzymski P, Flisiak R. Trends in Hospitalizations of Patients with Hepatitis C Virus in Poland between 2012 and 2022. Journal of Clinical Medicine. 2024; 13(18):5618. https://doi.org/10.3390/jcm13185618
Chicago/Turabian StyleGenowska, Agnieszka, Dorota Zarębska-Michaluk, Krystyna Dobrowolska, Krzysztof Kanecki, Paweł Goryński, Piotr Tyszko, Katarzyna Lewtak, Piotr Rzymski, and Robert Flisiak. 2024. "Trends in Hospitalizations of Patients with Hepatitis C Virus in Poland between 2012 and 2022" Journal of Clinical Medicine 13, no. 18: 5618. https://doi.org/10.3390/jcm13185618
APA StyleGenowska, A., Zarębska-Michaluk, D., Dobrowolska, K., Kanecki, K., Goryński, P., Tyszko, P., Lewtak, K., Rzymski, P., & Flisiak, R. (2024). Trends in Hospitalizations of Patients with Hepatitis C Virus in Poland between 2012 and 2022. Journal of Clinical Medicine, 13(18), 5618. https://doi.org/10.3390/jcm13185618









