Abstract
Background: This study aimed to analyze the effect of cardiac rehabilitation programs on the health-related quality of life of patients after a coronary cardiac event using patient-reported outcome measures (PROMs) for up to 6 months of evaluation. Methods: A comprehensive search was carried out in the MEDLINE, CINAHL, CENTRAL, and Web of Science databases for randomized controlled trials comparing the cardiac rehabilitation program with usual care. Two independent reviewers assessed the studies for inclusion, risk of bias using the Cochrane tool, and quality of evidence through the GRADE system. A meta-analysis was performed on studies assessing health-related quality of life with the SF-12 (Physical Component Summary and Mental Component Summary) up to 6 months after the program. Results: Twelve studies encompassed 2260 patients who participated in a cardiac rehabilitation program after a coronary event, with a mean age of 60.06 years. The generic PROMs used to assess quality of life were the SF-12, SF-36, EQ-5D-3L, EQ-5D-5L, and GHQ, and the specific coronary heart disease PROMs were MacNew and HeartQoL. There was a positive effect of participation in cardiac rehabilitation on the physical component of health-related quality of life at 6 months (MD [7.02]; p = 0.04] and on the mental component (MD [1.06]; p = 0.82) after applying the SF-12. Conclusions: This study highlights the significant benefits of cardiac rehabilitation programs on health-related quality of life, particularly in the physical domain at 6 months. Assessing outcomes over time through PROMs after coronary heart events is essential, thus making it possible to personalize patients’ care and improve their health status.
1. Introduction
Cardiovascular disease is a major public health problem associated with high mortality and morbidity, reduced exercise capacity, and lower quality of life [1]. It is particularly important to consider risk factors since the risk for cardiovascular disease combines the direct cause of disease with concepts of probability, prediction, and prognosis [2]. A cardiac rehabilitation (CR) program consists of a multidisciplinary intervention after a coronary cardiac event. This multidisciplinary intervention is aimed at lifestyle changes, smoking cessation, blood pressure control, adequate weight, a balanced diet, and encouraging physical activity [3]. To change lifestyles and control and optimize the prognosis of cardiac disease, and according to the guidelines reported by scientific societies, CR programs are recommended to achieve and maintain optimal health in these patients [3]. CR programs have grown and evolved in preventing and treating cardiovascular disease, demonstrating effectiveness, and contributing to participants’ quality of life [4,5]. Therefore, quality of life can be improved through psychosocial support facilitating a return to work, increased health literacy optimizing healthy behaviors, and encouraging physical activity to improve cardiac function and reduce anxiety levels.
Patient-reported outcome measures (PROMs) are used to assess the health-related quality of life (HRQoL) of patients, showing their health status and functional capacity and allowing for informed clinical and health decisions [6,7,8]. The assessment instruments used to standardize PROMs can be generic or specific [9]. Generic instruments make it possible to assess a particular pathology in the general population, while specific instruments assess the results of a particular population, making it possible to test the effectiveness of treatments for the same disease [9]. Given the quality of outcomes that PROMs can offer and individualized care from the patient’s perspective, there is growing interest in using PROMs. In this emerging area of research, the interest in studying PROMs in patients with cardiac pathology and the impact they may have on optimizing CR programs is noticeable [7].
However, despite the demonstrated benefits, there is a lack of comprehensive reviews focusing on the longitudinal impact of CR programs on both the physical and mental components of HRQoL. Some studies have already been conducted in this area, showing a positive effect on the quality of life of patients participating in this type of program through the assessment made using PROMs [10,11]. Other studies have demonstrated that HRQoL improved after participating in CR programs [12] or physical exercise programs [13]. However, some of these studies only used a physical intervention and did not address the mental and physical components according to the duration of the program and the type of PROM. Given this lack of knowledge and the importance of PROMs in assessing the effect of a CR program on HRQoL at 6 months [11], this systematic review with meta-analysis was carried out with the following aim: analyze the effect of CR programs (phase II) on the HRQoL of patients after a coronary cardiac event using PROMs for up to 6 months of evaluation. This study is important for the scientific and clinical community, as it allows us to understand the effect of CR on the physical and mental dimensions of the quality of life perceived by patients up to 6 months after an acute coronary event.
2. Methods
The protocol of this systematic review with meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the number CRD42022344240. A systematic review of peer-reviewed English language articles was undertaken according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) group [14], as shown in the PRISMA checklist.
2.1. Research Question and Eligibility Criteria
The research question addressed in this study was as follows: What is the effect of CR programs on mental and physical components after a coronary cardiac event for up to 6 months of assessment with PROMs?
We included all RCTs comparing interventions in CR programs against usual care, focusing on assessing HRQoL through PROMs. We included studies comparing the group of adult participants with coronary cardiac events who took part in a CR intervention (telephone or supervised follow-up, health education, structured exercise, and dietary support) with control groups that received guideline-recommended medical treatment. These CR programs are comprehensive, including a supervised or unsupervised structured exercise component, with educational support on risk factors and pharmacological therapy, and informal follow-up or education on exercise, psychosocial support, and diet. The comparison group received usual care (a non-standard, unstructured intervention without follow-up by specialist health professionals). In addition to these aspects that make up the programs, those in which HRQoL was assessed through PROMs up to 6 months after the start of the program were considered.
2.2. Search Strategy and Selection of Studies
Comprehensive searches were conducted in MEDLINE via Ovid, CINAHL via EBSCO, the Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science (SciElo) from January 2017 up to September 2024. This period was set for the research because in 2016 the European guidelines on the prevention of cardiovascular diseases in clinical practice were updated [2], which has an impact on studies with results based on CR programs. For the development of this search strategy, we used the Mesh Medical Subject Heading (MeSH) terms and MeSH major topic, following the methods suggested by the Cochrane Handbook for Systematic Reviews of Interventions [15]. Studies that met the criteria defined by the PICO(D) framework and that reported data on outcomes related to the implementation of the CR program were included. The studies were selected by two reviewers, following the eligibility criteria: (1) adult patients with coronary heart disease; (2) CR program phase II—patients after coronary cardiac event; (3) usual care after coronary cardiac event treatment with assessment of HRQoL over time (baseline and follow-up during or after intervention); (4) generic PROMs for HRQoL assessment and specific PROMs to coronary heart disease; (5) randomized clinical trials. The exclusion criteria were as follows: (1) abstracts; (2) studies not in English; (3) non-explicit assessment moments with PROMs; (4) non-original studies (reviews and meta-analyses, study protocols, conference proceedings, letters, commentary, and reports). Grey literature was also searched, and the references of the included studies were reviewed, with the aim of making important contributions to our study and increasing the scope of this systematic review.
2.3. Data Extraction
After considering the inclusion criteria, software was used to remove duplicate articles and manage the articles included for the final review. After removing the duplicates, two authors independently screened all the titles and abstracts for possible inclusion according to the predefined eligibility criteria. Disagreements were resolved by consensus or by consulting a third author (an expert in CR) when needed. After reviewing the titles and abstracts, a full-text analysis was conducted.
2.4. Risk of Bias
Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) was used for this study. The evaluation was specific to the outcome of HRQoL for the effect of an intervention on the experimental and control groups. Through this tool structured in 5 domains, it was possible to evaluate the different types of bias that can affect the results of randomized trials. These are bias arising from the randomization process; bias due to deviations from intended interventions; bias due to missing outcome data; bias in measurement of the outcome; and bias in the selection of the reported result. The risk-of-bias assessment for each of the included studies was performed by one investigator then reviewed and validated by the second investigator (J.B.), and doubts were discussed in a final meeting.
2.5. Quality of Evidence Assessment
Evidence levels were evaluated using the Grading Recommendations Assessment, Development, and Evaluation (GRADE) methodology [16] for primary outcomes at 6 months of the CR program. The certainty of the evidence was classified as high, moderate, low, or very low, with randomized clinical trials considered as high-certainty evidence.
2.6. Data Synthesis and Analysis
The analysis of the different studies included the following information: author and year, method, sample size, exercise type, duration, intervention, and outcome measures. In addition to these results, we used the values that allow estimating the effect of the CR program on the physical and mental components of the participants up to 6 months after a coronary cardiac event. The values of Standard Error and Difference in Means (MD) (95% confidence intervals) with a statistical significance of p < 0.05 were then used for this meta-analysis by applying the SF-12 in the different studies that evaluated the effectiveness of the CR program in the different domains. This generic PROM (SF-12) was used because it is the one that best applies to this study, in which the scoring yields two summary measures: the Physical Component Summary (PCS) and the Mental Component Summary (MCS).
The data obtained from the studies included in the meta-analysis were combined, and a statistical analysis was performed using a random effects model. This type of model allows for the effects of heterogeneity due to methodological differences in the studies included, the type of CR program, and a small number of participants in some studies, as well as robust statistical results [17]. The effect of heterogeneity can be seen with the relevant I squared (I2) and the statistically significant homogeneity test (p < 0.05).
The different variables of the included studies were compared at the time of assessment after the CR program. The effect size of this program on the HRQoL of participating patients was calculated for each of the studies according to the assessment at 6 months post-coronary event. A sensitivity analysis was performed to understand each study intervention’s effect size. Thus, it is possible to understand the significance of each study, where the MD of each study ranged from 1.60 to 6.70 in the physical domain and −7.81 to 8.83 in the mental domain. The publication bias of the studies that assessed the HRQoL at 6 months post-program was calculated by Egger’s test (using SPSS Version 28.0), and the respective bias was analyzed by the asymmetry in the funnel plot (statistical significance for p < 0.10) [18].
3. Results
From the results obtained after the initial electronic search (n = 533), 476 articles were analyzed once duplicates were removed. From this extraction, after duplicate removal and evaluation of titles and abstracts, 80 articles were reviewed. A screening of articles based on full-text assessment according to the eligibility criteria was performed, resulting in 12 RCTs [19,20,21,22,23,24,25,26,27,28,29,30] that were included in the systematic review, and 3 of them [22,23,25] were considered suitable for meta-analysis to assess the physical and mental components of HRQoL (SF-12) at 6 months of follow-up, as shown in Figure 1.
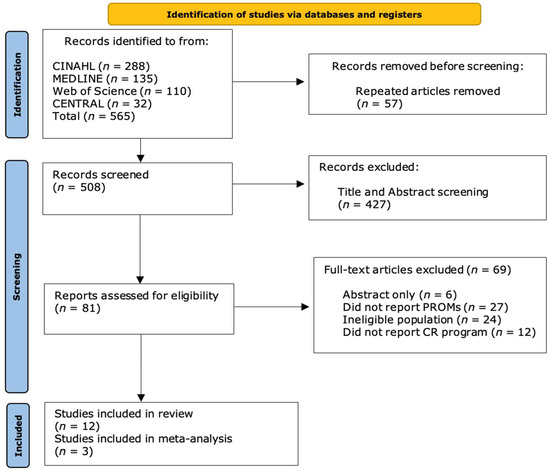
Figure 1.
Flow diagram of the literature search of this meta-analysis (according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses—PRISMA).
3.1. Characteristics of Studies and Participants
The studies selected were conducted in China (n = 3) [21,23,26], Pakistan (n = 2) [25,29], Germany (n = 1) [30], and one study each in Italy [19], Egypt [20], Israel [22], the UAE [27], and the UK [24]. All studies had an RCT design comparing outcomes in two groups. One group participated in a structured CR program with intervention by a multidisciplinary team, which was compared with the other group that received usual care after coronary cardiac event treatment. In the different studies, the intervention lasted from 3 weeks to 12 months. According to the specifications of the intervention in the different studies, we can report the following: supervised individualized exercise training or group intervention, strength and resistance exercises (walking, treadmill, and stationary cycling), education intervention, and psychological support, as shown in Table 1.

Table 1.
Characteristics of included studies.
Regarding the characteristics of the participants in this review, HRQoL was assessed in 2260 patients who participated in the CR programs after coronary cardiac event, with a mean age of 60.06 years. Of these participants, 69.29% were male, with one study reporting only men in the inclusion criteria.
3.2. Systematic Review
There is a variation in structure in some of the programs, which we note is typical of CR globally. However, in all studies selected for this meta-analysis, participants were supervised in exercise sessions throughout the intervention, and this was the most common type. Regarding follow-up, it took place in a mixed manner in most studies, i.e., at the health care facility and at home (telephonically). A CR program’s remaining session intervention (components) was delivered through health education sessions, medication management coaching, disease management, coaching to support self-efficacy through awareness of physiological and affective states, and social coaching.
Different PROMs were used throughout the follow-up of participants in the CR programs. The generic instruments used to assess HRQoL in the included studies were SF-12 (n = 5) [21,22,23,25,26], SF-36 (n = 1) [20], EQ-5D-3L (n = 1) [19], and EQ-5D-5L (n = 2) [24,30]. Those specific to cardiac conditions were the MacNew (n = 3) [24,25,29] and HeartQoL (n = 2) [27,28].
The results of our systematic review indicate a moderate overall quality of evidence, using the GRADE approach, when assessing HRQoL 6 months after intervention in a CR program (Supplementary Materials). There is a fair degree of confidence that clinical practice with multidisciplinary interventions in CR programs is associated with variations in HRQoL. There are some limitations to this review, including the heterogeneity of the study population, and different types of interventions: duration, frequency of physical training, education sessions, and social support. In addition, the very rigorous inclusion criteria in this analysis resulted in few studies on this topic, and therefore an improvement in other outcomes may not have been included.
3.3. Risk-of-Bias Assessment
The assessment of the risk of bias for the studies considered in our study was based on that recommended by Cochrane using the Rob2 tool [15]. After analysis of the studies, it was found that some did not detail methodological steps, and there were some considerations of possible bias (Supplementary Materials). Due to the clinical situation of each participant, it is sometimes necessary to adapt some aspects during the predefined program, with some risk of bias in terms of consistency in the implementation of the intervention planned in some studies [21,23,25,26,29]. The risk of reporting is low in all studies, as they presented the results of the PROMs used. The risk of bias in outcome selection is high in some studies [25,29], with some considerations in others [19,20,21,22,23,26,27,28]. This risk of bias is because the HRQoL assessment is through scales and questionnaires, and the authors did not indicate how this result was extracted. Overall, according to the risk of bias, more than 50% of the studies have low risk, and only 16.67% have high risk.
3.4. Meta-Analysis
The meta-analysis included studies that used PROMs to measure HRQoL. After the systematic review of the literature, the selected RCTs were used in the meta-analysis because they measured HRQoL over time after intervention in a CR program. Figure 2 presents the analysis of the RCTs, showing the quality of life of patients with coronary heart disease after intervention in a CR program.
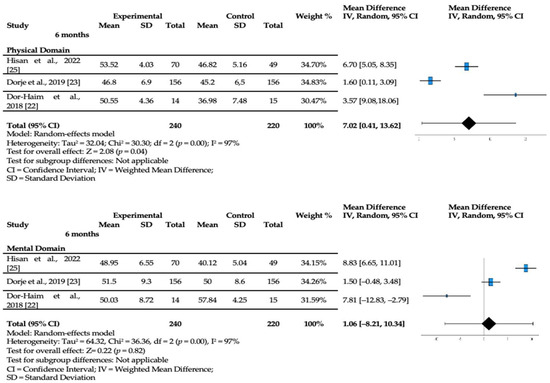
Figure 2.
SF-12 domains at 6 months (Physical Component Summary and Mental Component Summary) [22,23,25].
In the three RCTs of the meta-analysis, there was a positive effect on quality of life at 6 months after starting the CR program. When assessed for up to 6 months of the program, there was statistically significant evidence (p = 0.04) showing an increase in the physical domain score (MD [7.02]; 95% CI [0.41, 13.62]) after the intervention. In the mental domain, although there were improvements in CR program participants, they were not statistically significant (MD [1.06]; 95% CI [−8.21, 10.34]). The asymmetry in the funnel plot can be verified by considering the studies included in the meta-analysis, showing a result with publication bias justified by the heterogeneity of the different studies (Supplementary Materials).
4. Discussion
The positive effect of CR programs on HRQoL, particularly the physical component at 6 months, highlights the benefits of these interventions. After applying the different PROMs to assess the HRQoL of participants with ischemic coronary disease in CR programs, and in this meta-analysis the SF-12, an improvement was shown in the physical dimension at 6 months after the start of the intervention. RCTs that assessed participants’ HRQoL after CR programs for coronary events using the same instrument were combined, thus measuring the effect of the intervention on the experimental group. Several generic and coronary-disease-specific PROMs were used to assess the HRQoL of participants in CR programs, highlighting the SF-12, SF-36, EQ-5D-5L, EQ-5D-3L, MacNew, and HeartQoL. There is a knowledge gap regarding the assessment of health status and quality of life reported by participants through PROMs in rehabilitation programs, and it is essential to demonstrate their importance [31,32,33,34,35,36,37]. Many of the RCTs on cardiovascular disease do not measure the components of HRQoL [38], knowing that it is critical for individualized care. It is known that only 23% of RCTs included HRQoL as a primary outcome and only 70% considered this outcome important, underutilizing PROMs in clinical decision making [38]. Recent reviews have concluded that it is challenging to compare HRQoL outcomes in participants in CR programs due to the interventions’ complexity and each patient’s clinical situation leading to the heterogeneity of the instruments [34,39]. Although several instruments were analyzed, we found that for HRQoL, the most used was the SF-12. This instrument is essential for assessing the HRQoL of patients with coronary heart disease who participate in CR programs, since it refers to aspects of well-being that are influenced by the physical and mental domains [40].
Regarding the timing of PROMs, most of the studies included in this review assessed HRQoL at baseline (at the beginning of the program) and over the following 6 months, even when the intervention period was conducted over a few weeks. A meta-analysis assessing HRQoL in patients with coronary syndrome showed significant improvements in physical performance and general health 6 months after applying different PROMs [13]. Monitoring the HRQoL of patients who participate in CR programs over time is important, since improvements are not only short term but also over a longer period due to the benefits of physical exercise. Physical exercise improves health and is one of the main components of CR programs [41]. Despite some heterogeneity, the studies included in this review included the dimension of physical exercise in the structure of the program carried out in a supervised manner at an early stage. Early-onset supervised exercise is positive because it improves physical function and exercise tolerance, allowing exercise to be continuously adapted to individual needs and abilities [42,43,44]. In this study, a positive effect on HRQoL was observed in the physical component 6 months after starting the program. In a review that studied the relationship of quality of life with exercise-based CR, the authors highlighted that the improvement in physical function translates into increased performance of activities of daily living, and patients with coronary disease reported higher scores in the assessment of their quality of life [13].
In the mental domain, the effect was also positive up to 6 months after starting the CR program compared to the control group, but without statistical significance. Anxiety and depression are common after acute myocardial infarction, may persist for a few months or even years, and may affect the dynamics and adherence to the CR program [44]. One of the studies conducted on quality of life in patients who suffered an acute myocardial infarction showed that these patients have a higher likelihood of negative psycho-emotional effects, leading to a deterioration in HRQoL [44]. Another study justifies this result, finding only a positive effect on the physical functioning of the participants [45].
In addition to the benefits for the mental and physical condition of patients who participate in CR programs, it is also important to mention in the discussion other benefits of implementing these programs. The health system also gains from the implementation of CR programs. Monitoring the outcomes associated with these programs in coronary pathology makes it possible to reduce the costs inherent in this syndrome and the associated burden and mortality [46]. The economic implications of these programs, compared to their benefits, are demonstrable and have a good cost-effectiveness ratio. A study of 601.099 patients ≥ 65 years hospitalized for coronary heart disease compared 5-year mortality in users and nonusers of CR, and it showed that CR improved mortality by 8.0% (p < 0.001) [47]. It also indicated that 1.344 QALYs (95% CI, 0.543–2.144) were added, showing improvements in quality of life and reducing the cost of treatment from USD 32,996 (95% CI, USD 21,942–66,494)/QALY to USD 30,188 (95% CI, USD 18,175–74,484)/QALY over a lifetime [47]. In fact, CR is a cost-effective treatment option for health services, and although it is underutilized, care providers should encourage patients to participate with the aim of improving quality of life and reducing health costs.
The main limitation of this meta-analysis is the limited number of studies, and some studies had small samples due to the complexity of the patient’s clinical condition and the known barriers to adherence to the programs. Another limitation is the inherent nature of cardiac rehabilitation interventions in the treatment group compared to the control group. Patients enrolled in the treatment arm may inadvertently receive multidisciplinary and more personalized care in some studies compared to their counterparts in the control group, potentially skewing outcomes.
5. Conclusions
Although the assessment of HRQoL in CR participants after coronary cardiac events is known, few studies include HRQoL as a primary outcome in the evaluation of the effect of CR. This study develops knowledge in CR by showing the different PROMs applied in the assessment of HRQoL and by demonstrating the importance of time in the assessment of the different components of HRQoL. This study shows the positive effect of CR on the physical and mental components of HRQoL after assessment by the same PROM, with the intervention of multidisciplinary teams. The importance of time in assessing HRQoL was demonstrated by the SF-12 during the follow-up period, with statistically significant results in the physical domain at 6 months.
Given the importance of these results, HRQoL improvement, regardless of the underlying disease or the CR program implemented, is important, and it is vital that health organizations implement PROMs by investing more time and resources in an implementation strategy.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/jcm13185576/s1.
Author Contributions
J.M. and J.B. designed the study and developed the search strategy; J.M. identified the records and removed duplicate records; J.M. and J.B. conducted the critical appraisal of all studies; J.M., J.B., P.A. and P.B. were involved in the systematic review process and analyzed and interpreted the data; A.R., B.D. and P.B. reviewed the initial manuscript and approved the final manuscript as submitted. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by national funds through the Foundation for Science and Technology under the project UIDP/04923/2020.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Nacional School of Public Health—NOVA University of Lisbon and was approved (CEENSP n°3/2022).
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 10 August 2024).
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, 596–646. [Google Scholar] [CrossRef]
- Winnige, P.; Vysoky, R.; Dosbaba, F.; Batalik, L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J. Clin. Cases 2021, 9, 1761–1784. [Google Scholar] [CrossRef] [PubMed]
- Moreira, J.M.A.; Grilo, E.N. Quality of life after coronary artery bypass graft surgery—Results of cardiac rehabilitation programme. J. Exerc. Rehabil. 2019, 15, 715–722. [Google Scholar] [CrossRef]
- Blumer, V.; Greene, S.J.; Wu, A.; Butler, J.; Ezekowitz, J.A.; Lindenfeld, J.; Alhanti, B.; Hernandez, A.F.; O’Connor, C.M.; Mentz, R.J. Sex Differences in Clinical Course and Patient-Reported Outcomes among Patients Hospitalized for Heart Failure. Heart Fail. 2021, 9, 336–345. [Google Scholar] [CrossRef]
- Dawson, J.; Doll, H.; Fitzpatrick, R.; Jenkinson, C.; Carr, A.J. The routine use of patient reported outcome measures in healthcare settings. BMJ 2010, 340, 186. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Ware, P.; Gardner, W.; Witter, J.; Bingham, C.O.; Kairy, D.; Bartlett, S.J. Montreal Accord on Patient-Reported Outcomes (PROs) use series—Paper 8: Patient-reported outcomes in electronic health records can inform clinical and policy decisions. J. Clin. Epidemiol. 2017, 89, 160–167. [Google Scholar] [CrossRef]
- McKenna, S.P. Measuring patient-reported outcomes: Moving beyond misplaced common sense to hard science. BMC Med. 2011, 14, 86. [Google Scholar] [CrossRef]
- McMurray, J.; McNeil, H.; Gordon, A.; Elliott, J.; Stolee, P. Psychometric Testing of a Rehabilitative Care Patient Experience Instrument. Arch. Phys. Med. Rehabil. 2018, 99, 1840–1847. [Google Scholar] [CrossRef]
- Salzwedel, A.; Koran, I.; Langheim, E.; Schlitt, A.; Nothroff, J.; Bongarth, C.; Wrenger, M.; Sehner, S.; Reibis, R.; Wegscheider, K.; et al. Patient-reported outcomes predict return to work and health-related quality of life six months after cardiac rehabilitation: Results from a German multi-centre registry (OutCaRe). PLoS ONE 2020, 15, e0232752. [Google Scholar] [CrossRef]
- Mansilla-Chacón, M.; Gómez-Urquiza, J.L.; Martos-Cabrera, M.B.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De La Fuente, G.A.; Suleiman-Martos, N. Effects of Supervised Cardiac Rehabilitation Programmes on Quality of Life among Myocardial Infarction Patients: A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2021, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Candelaria, D.; Randall, S.; Ladak, L.; Gallagher, R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: A systematic review and meta-analysis. Qual. Life Res. 2020, 29, 579–592. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Vist, G.E.; Falck-Ytter, Y.; Schünemann, H.J. What is “quality of evidence” and why is it important to clinicians? BMJ 2008, 336, 995–998. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Campo, G.; Tonet, E.; Chiaranda, G.; Sella, G.; Maietti, E.; Bugani, G.; Vitali, F.; Serenelli, M.; Mazzoni, G.; Ruggiero, R.; et al. Exercise intervention improves quality of life in older adults after myocardial infarction: Randomised clinical trial. Heart 2020, 106, 1658–1664. [Google Scholar] [CrossRef] [PubMed]
- Casper, E.A.; El Wakeel, L.M.; Saleh, M.A.; El-Hamamsy, M.H. Management of pharmacotherapy-related problems in acute coronary syndrome: Role of clinical pharmacist in cardiac rehabilitation unit. Basic Clin. Pharmacol. Toxicol. 2019, 125, 44–53. [Google Scholar] [CrossRef]
- Deng, B.; Shou, X.; Ren, A.; Liu, X.; Wang, Q.; Wang, B.; Wang, Y.; Yan, T.; Zhao, X.; Zhu, L. Effect of aerobic training on exercise capacity and quality of life in patients older than 75 years with acute coronary syndrome undergoing percutaneous coronary intervention. Physiother. Theory Pract. 2022, 38, 1135–1144. [Google Scholar] [CrossRef]
- Dor-Haim, H.; Barak, S.; Horowitz, M.; Yaakobi, E.; Katzburg, S.; Swissa, M.; Lotan, C. Improvement in cardiac dysfunction with a novel circuit training method combining simultaneous aerobic-resistance exercises. A randomized trial. PLoS ONE 2018, 13, e0188551. [Google Scholar] [CrossRef]
- Dorje, T.; Zhao, G.; Tso, K.; Wang, J.; Chen, Y.; Tsokey, L.; Tan, B.K.; Scheer, A.; Jacques, A.; Li, Z.; et al. Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): A parallel-group, single-blind, randomised controlled trial. Lancet Digit. Health 2019, 1, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Herring, L.Y.; Dallosso, H.; Schreder, S.; Smith, E.J.; Waheed, G.; Gray, L.J.; Khunti, K.; Yates, T.; Highton, P.J.; Rowlands, A.V.; et al. Physical Activity after Cardiac EventS (PACES): A group education programme with subsequent text message support designed to increase physical activity in individuals with diagnosed coronary heart disease: A randomised controlled trial. Open Heart 2021, 8, e001351. [Google Scholar] [CrossRef] [PubMed]
- Hisam, A.; Haq, Z.U.; Aziz, S.; Doherty, P.; Pell, J. Effectiveness of Mobile Health Augmented Cardiac Rehabilitation (MCard) on health-related quality of life among post-acute coronary syndrome patients: A randomized controlled trial. Pak. J. Med. Sci. 2022, 38, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Deng, L.; Yu, H. The effects of a comprehensive rehabilitation and intensive education program on anxiety, depression, quality of life, and major adverse cardiac and cerebrovascular events in unprotected left main coronary artery disease patients who underwent coronary artery bypass grafting. Ir. J. Med. Sci. 2020, 189, 477–488. [Google Scholar] [CrossRef]
- Muthukrishnan, R.; Malik, G.S.; Gopal, K.; Shehata, M.A. Power walking based outpatient cardiac rehabilitation in patients with post-coronary angioplasty: Randomized control trial. Physiother. Res. Int. 2021, 26, e1919. [Google Scholar] [CrossRef]
- Pedersen, C.G.; Nielsen, C.V.; Lynggaard, V.; Zwisler, A.D.; Maribo, T. Cardiac rehabilitation: Pedagogical education strategies have positive effect on long-term patient-reported outcomes. Health Educ. Res. 2023, 38, 597–609. [Google Scholar] [CrossRef]
- Ul-Haq, Z.; Khan, D.; Hisam, A.; Yousafzai, Y.M.; Hafeez, S.; Zulfiqar, F.; Gul, A.M.; Hafizullah, M.; Pell, J. Effectiveness of Cardiac Rehabilitation on Health-related Quality of Life in Patients with Myocardial Infarction in Pakistan. J. Coll. Physicians Surg. Pak. 2019, 29, 803–809. [Google Scholar] [CrossRef]
- Wienbergen, H.; Fach, A.; Meyer, S.; Meyer, J.; Stehmeier, J.; Backhaus, T.; Michel, S.; Krämer, K.; Osteresch, R.; Schmucker, J.; et al. Effects of an intensive long-term prevention programme after myocardial infarction—A randomized trial. Eur. J. Prev. Cardiol. 2019, 26, 522–530. [Google Scholar] [CrossRef]
- Dibben, G.O.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.D.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: A meta-analysis. Eur. Heart J. 2023, 44, 452–469. [Google Scholar] [CrossRef]
- Foster, A.; Croot, L.; Brazier, J.; Harris, J.; O’Cathain, A. The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: A systematic review of reviews. J. Patient Rep. Outcomes 2018, 2, 46. [Google Scholar] [CrossRef]
- Johnston, B.C.; Patrick, D.L.; Busse, J.W.; Schünemann, H.J.; Agarwal, A.; Guyatt, G.H. Patient-reported outcomes in meta-analyses—Part 1: Assessing risk of bias and combining outcomes. Health Qual. Life Outcomes 2013, 11, 109. [Google Scholar] [CrossRef] [PubMed]
- Cornélio, M.E.; Alexandre, N.M.; São-João, T.M. Measuring instruments in cardiology adapted into Portuguese language of Brazil: A systematic review. Rev. Esc. Enferm. USP 2014, 48, 368–376. [Google Scholar] [CrossRef]
- Moreira, J.; Miguel, S.; Delgado, B.; Boto, P. Patient-reported outcome measures in rehabilitation after knee surgery: A rapid systematic review. J. Public Health. 2024, 1–15. [Google Scholar] [CrossRef]
- Moreira, J.; Mesquita, M.; Flamínio, J.; Almeida, M.; Delgado, B.; Boto, P. Patient-reported outcome measures in knee injuries rehabilitation: A protocol for intervention. MethodsX 2024, 12, 102647. [Google Scholar] [CrossRef]
- Maruszczyk, K.; McMullan, C.; Aiyegbusi, O.L.; Keeley, T.; Wilson, R.; Collis, P.; Bottomley, C.; Calvert, M.J. Paving the way for patient centricity in real-world evidence (RWE): Qualitative interviews to identify considerations for wider implementation of patient-reported outcomes in RWE generation. Heliyon 2023, 9, e20157. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, K.; Malhotra, A.; Banning, A.P.; Jenkinson, C. Outcome selection and role of patient reported outcomes in contemporary cardiovascular trials: Systematic review. BMJ 2010, 341, c5707. [Google Scholar] [CrossRef]
- Snoek, J.A.; Prescott, E.I.; van der Velde, A.E.; Eijsvogels, T.M.; Mikkelsen, N.; Prins, L.F.; Bruins, W.; Meindersma, E.; González-Juanatey, J.R.; Peña-Gil, C.; et al. Effectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol. 2021, 6, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Francis, T.; Kabboul, N.; Rac, V.; Mitsakakis, N.; Pechlivanoglou, P.; Bielecki, J.; Alter, D.; Krahn, M. The Effect of Cardiac Rehabilitation on Health-Related Quality of Life in Patients with Coronary Artery Disease: A Meta-analysis. Can. J. Cardiol. 2019, 35, 352–364. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Health benefits of physical activity: A systematic review of current systematic reviews. Health Qual. Life Outcomes 2007, 32, 541–556. [Google Scholar] [CrossRef]
- Shibata, A.; Oka, K.; Nakamura, Y.; Muraoka, I. Recommended level of physical activity and health-related quality of life among Japanese adults. Health Qual. Life Outcomes 2007, 5, 64. [Google Scholar] [CrossRef]
- Rumsfeld, J.S.; Alexander, K.P.; Goff, D.C., Jr.; Graham, M.M.; Ho, P.M.; Masoudi, F.A.; Moser, D.K.; Roger, V.L.; Slaughter, M.S.; Smolderen, K.G.; et al. Cardiovascular health: The importance of measuring patient-reported health status: A scientific statement from the American Heart Association. Circulation 2013, 127, 2233–2249. [Google Scholar] [CrossRef]
- Houle, J.; Doyon, O.; Vadeboncoeur, N.; Turbide, G.; Diaz, A.; Poirier, P. Effectiveness of a pedometer-based program using a socio-cognitive intervention on physical activity and quality of life in a setting of cardiac rehabilitation. Can. J. Cardiol. 2012, 28, 27–32. [Google Scholar] [CrossRef]
- Ladak, L.A.; Hasan, B.S.; Gullick, J.; Gallagher, R. Health-related quality of life in congenital heart disease surgery in children and young adults: A systematic review and meta-analysis. Arch. Dis. Child. 2019, 104, 340–347. [Google Scholar] [CrossRef]
- Salzwedel, A.; Völler, H. Cardiac rehabilitation: Patient-reported outcomes are decisive for success. Dtsch. Ärzteblatt Int. 2021, 118, 505–506. [Google Scholar] [CrossRef]
- Shepard, D.S.; Zakir, S.; Gaalema, D.E.; Ades, P.A. Cost-Effectiveness of Cardiac Rehabilitation in Older Adults with Coronary Heart Disease. J. Cardiopulm. Rehabil. Prev. 2024, 44, 107–114. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).