Anesthetic Approach for Non-Cardiac Procedures in Patients with a Left Ventricular Assist Device
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Non-cardiac Procedures and Type of Anesthesia
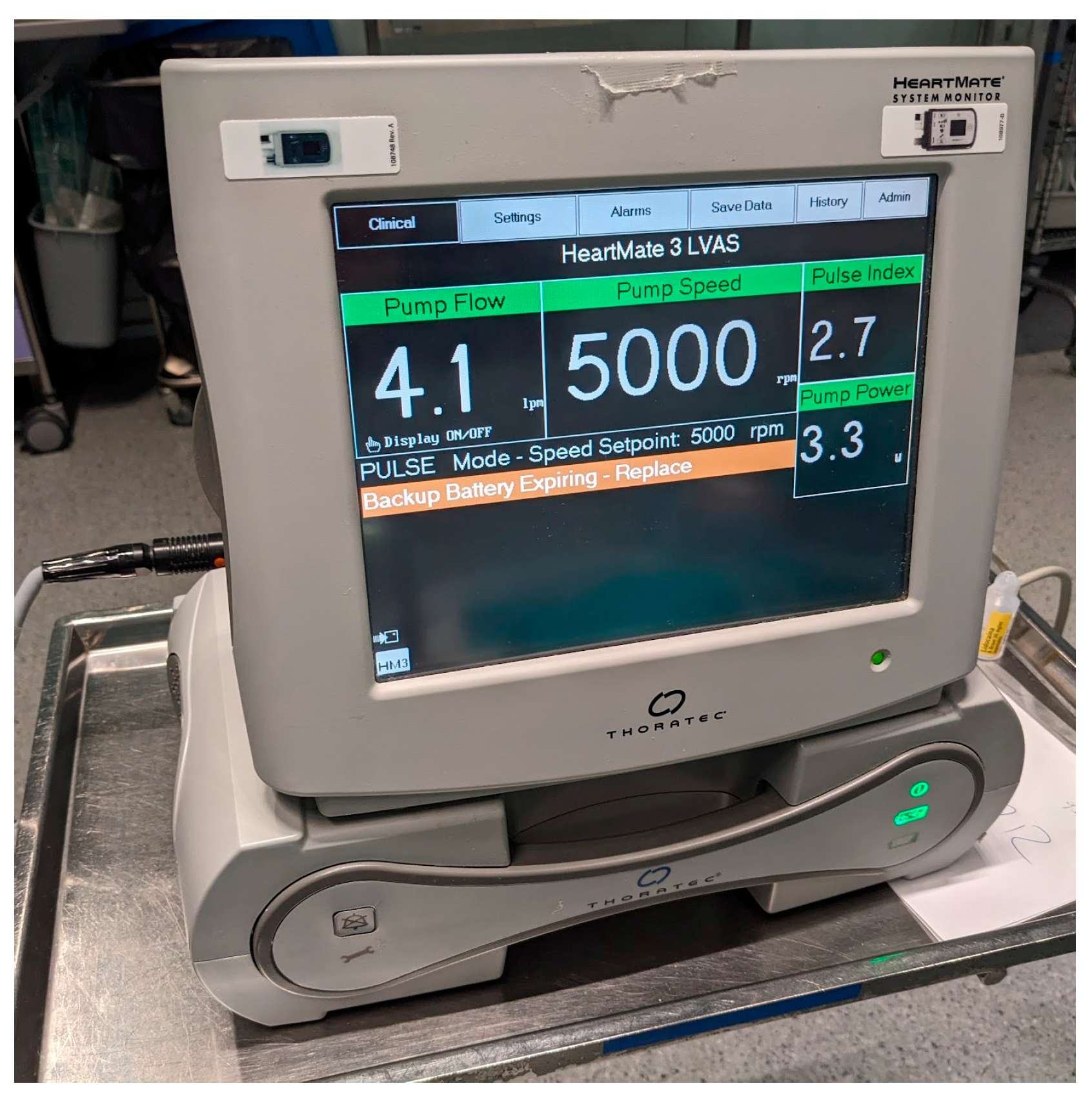
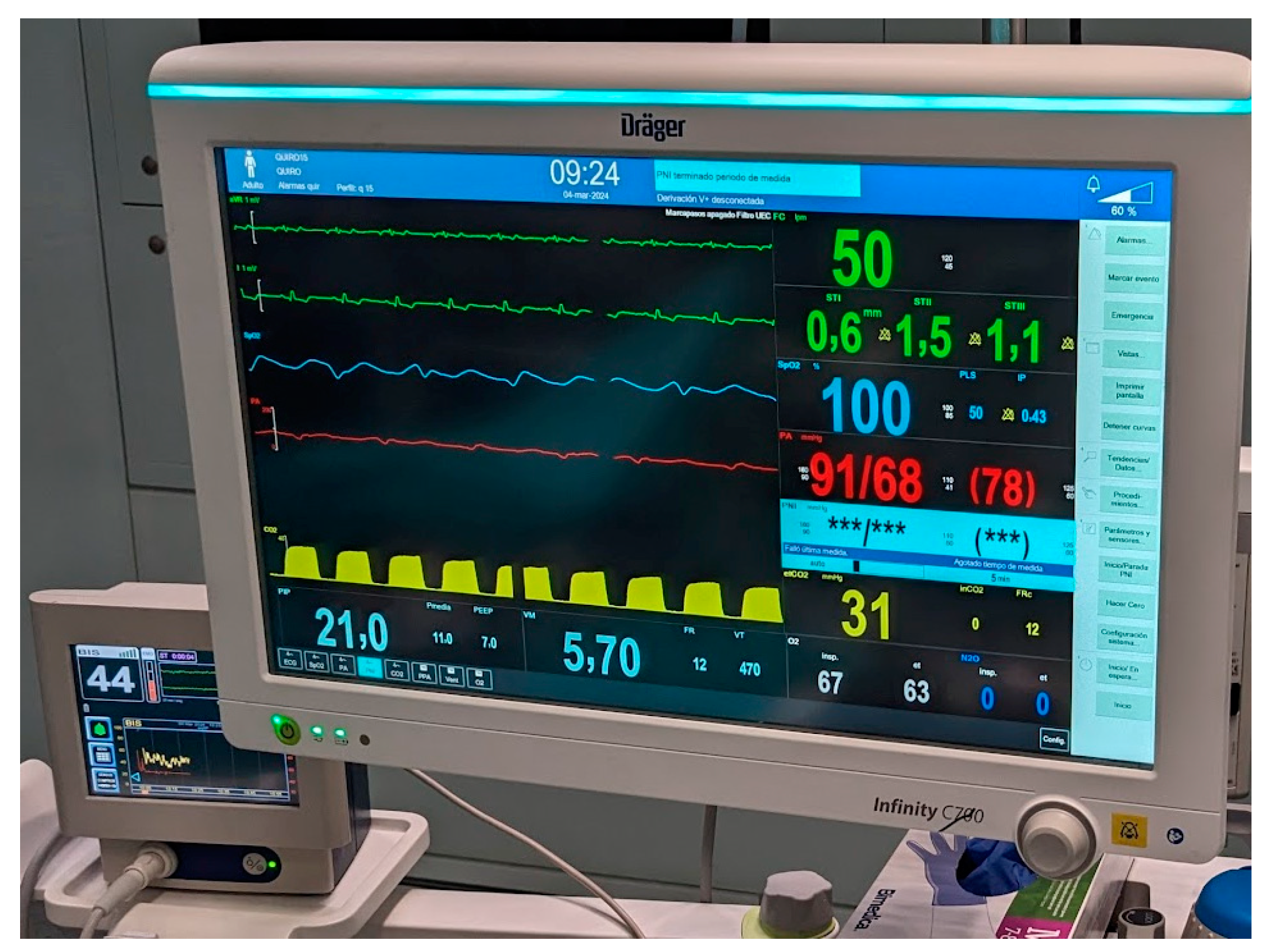
3.3. Monitoring
3.4. Hemostasis Management and Complications
3.5. Intraoperative Complications
3.6. Postoperative Period
3.7. Gastrointestinal Endoscopies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis treatment of acute chronic heart failure: The Task Force for the diagnosis treatment of acute chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [PubMed]
- Fang, J.C.; Ewald, G.A.; Allen, L.A.; Butler, J.; Westlake Canary, C.A.; Colvin-Adams, M.; Dickinson, M.G.; Levy, P.; Stough, W.G.; Sweitzer, N.K.; et al. Advanced (stage D) heart failure: A statement from the heart failure society of America guidelines committee. J. Card. Fail. 2015, 21, 519–534. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef] [PubMed]
- Ben Gal, T.; Ben Avraham, B.; Milicic, D.; Crespo-Leiro, M.G.; Coats, A.J.S.; Rosano, G.; Seferovic, P.; Ruschitzka, F.; Metra, M.; Anker, S.; et al. Guidance on the management of left ventricular assist device (LVAD) supported patients for the non-LVAD specialist healthcare provider: Executive summary. Eur. J. Heart Fail. 2021, 23, 1597–1609. [Google Scholar] [CrossRef] [PubMed]
- Dalia, A.A.; Cronin, B.; Stone, M.E.; Turner, K.; Hargrave, J.; Vidal Melo, M.F.; Essandoh, M. Anesthetic Management of Patients With Continuous-Flow Left Ventricular Assist Devices Undergoing Noncardiac Surgery: An Update for Anesthesiologists. J. Cardiothorac. Vasc. Anesth. 2018, 32, 1001–1012. [Google Scholar] [CrossRef] [PubMed]
- Mehra, M.R.; Cleveland, J.C., Jr.; Uriel, N.; Cowger, J.A.; Hall, S.; Horstmanshof, D.; Naka, Y.; Salerno, C.T.; Chuang, J.; Williams, C.; et al. Primary results of long-term outcomes in the MOMENTUM 3 pivotal trial and continued access protocol study phase: A study of 2200 HeartMate 3 left ventricular assist device implants. Eur. J. Heart Fail. 2021, 23, 1392–1400. [Google Scholar] [CrossRef]
- Gustafsson, F.; Ben Avraham, B.; Chioncel, O.; Hasin, T.; Grupper, A.; Shaul, A.; Nalbantgil, S.; Hammer, Y.; Mullens, W.; Tops, L.F.; et al. HFA of the ESC position paper on the management of LVAD-supported patients for the non-LVAD specialist healthcare provider Part 3: At the hospital and discharge. ESC Heart Fail. 2021, 8, 4425–4443. [Google Scholar] [CrossRef]
- Ahsan, I.; Faraz, A.; Mehmood, A.; Ullah, W.; Ghani, A.R. Clinical Approach to Manage Gastrointestinal Bleeding with a Left Ventricular Assist Device (LVAD). Cureus 2019, 11, e6341. [Google Scholar] [CrossRef]
- Taghavi, S.; Jayarajan, S.N.; Ambur, V.; Mangi, A.A.; Chan, E.; Dauer, E.; Sjoholm, L.O.; Pathak, A.; Santora, T.A.; Goldberg, A.J.; et al. Noncardiac surgical procedures after left ventricular assist device implantation. ASAIO J. 2016, 62, 370–374. [Google Scholar] [CrossRef]
- Mathis, M.R.; Sathishkumar, S.; Kheterpal, S.; Caldwell, M.D.; Pagani, F.D.; Jewell, E.S.; Engoren, M.C. Complications, Risk Factors, and Staffing Patterns for Noncardiac Surgery in Patients with Left Ventricular Assist Devices. Anesthesiology 2017, 126, 450–460. [Google Scholar] [CrossRef]
- Stone, M.; Hinchey, J.; Sattler, C.; Evans, A. Trends in the management of patients with left ventricular assist devices presenting for noncardiac surgery: A 10-year institutional experience. Semin. Cardiothorac. Vasc. Anesth. 2016, 20, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Nelson, E.W.; Heinke, T.; Finley, A.; Guldan, G.J.; Gaddy, P.; Matthew Toole, J.; Mims, R.; Abernathy, J.H., 3rd. Management of LVAD Patients for Noncardiac Surgery: A Single-Institution Study. J. Cardiothorac. Vasc. Anesth. 2015, 29, 898–900. [Google Scholar] [CrossRef] [PubMed]
- Degnan, M.; Brodt, J.; Rodriguez-Blanco, Y. Perioperative management of patients with left ventricular assist devices undergoing noncardiac surgery. Ann. Card. Anaesth. 2016, 19, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Min, J.J.; Cho, Y.H.; Lee, S.M.; Lee, J.H. Anesthetic Management for Non-Cardiac Surgery in the Patient with Left Ventricular Assistance Device. Korean J. Anesth. 2024, 77, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Briasoulis, A.; Chehab, O.; Alvarez, P. In-hospital Outcomes of Left Ventricular Assist Devices (LVAD) Patients Undergoing Noncardiac Surgery. ASAIO J. 2021, 67, 144–148. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. Medtronic HeartWare Ventricular Assist Device (HVAD) System [Internet]; FDA: Silver Spring, MD, USA, 2023; [Updated 25 August 2023]. Available online: https://www.fda.gov/medical-devices/cardiovascular-devices/medtronic-heartware-ventricular-assist-device-hvad-system (accessed on 9 September 2024).
- Hwang, K.Y.; Hwang, N.C. Facilitating noncardiac surgery for the patient with left ventricular assist device: A guide for the anesthesiologist. Ann. Card. Anaesth. 2018, 21, 351–362. [Google Scholar] [CrossRef]
- Milicic, D.; Ben Avraham, B.; Chioncel, O.; Barac, Y.D.; Goncalvesova, E.; Grupper, A.; Altenberger, J.; Frigeiro, M.; Ristic, A.; De Jonge, N.; et al. Heart Failure Association of the European Society of Cardiology position paper on the management of left ventricular assist device-supported patients for the non-left ventricular assist device specialist healthcare provider: Part 2: At the emergency department. ESC Heart Fail. 2021, 8, 4409–4424. [Google Scholar]
- Chung, M. Perioperative Management of the Patient With a Left Ventricular Assist Device for Noncardiac Surgery. Anesth. Analg. 2018, 126, 1839–1850. [Google Scholar] [CrossRef]
- Chang, M.G.; Miller, M.; Dalia, A.A. Intraoperative Management of Left Ventricular Assist Device Explantation: Complications and Lessons Learned. J. Cardiothorac. Vasc. Anesth. 2020, 34, 1002–1004. [Google Scholar] [CrossRef]
- Gayam, S.; Staab, J.; Shih, G.; Stoops, S. Cesarean delivery in a parturient with a left ventricular assist device. Int. J. Obstet. Anesth. 2020, 44, 53–55. [Google Scholar] [CrossRef]
- Fegley, M.W.; Gupta, R.G.; Elkassabany, N.; Augoustides, J.G.; Werlhof, H.; Gutsche, J.T.; Kornfield, Z.N.; Patel, N.; Sanders, J.; Fernando, R.J.; et al. Elective Total Knee Replacement in a Patient With a Left Ventricular Assist Device–Navigating the Challenges with Spinal Anesthesia. J. Cardiothorac. Vasc. Anesth. 2021, 35, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Kollmar, J.P.; Colquhoun, D.A.; Huffmyer, J.L. Anesthetic challenges for posterior spine surgery in a patient with left ventricular assist device: A case report. A A Case Rep. 2017, 9, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Chacon, M.M.; Hattrup, E.A.; Shillcutt, S.K. Perioperative Management of Two Patients with Left Ventricular Assist Devices Presenting for Noncardiac Surgery in the Prone Position. A A Case Rep. 2014, 2, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.; Pamboukian, S.V.; Teuteberg, J.J.; Birks, E.; Lietz, K.; Moore, S.A.; Morgan, J.A.; Arabia, F.; Bauman, M.E.; Buchholz, H.W.; et al. The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support: Executive summary. J. Heart Lung Transpl. 2013, 32, 157–187. [Google Scholar] [CrossRef]
- Sheu, R.; Joshi, B.; High, K.; Thinh Pham, D.; Ferreira, R.; Cobey, F. Perioperative management of patients with left ventricular assist devices undergoing noncardiac procedures: A survey of current practices. J. Cardiothorac. Vasc. Anesth. 2015, 29, 17–26. [Google Scholar] [CrossRef]
| Demographic Data | Variable | n (%) of Patients 1 |
|---|---|---|
| Total patients | 16 | |
| Mean age (years) | 60.2 ± 13.2 | |
| Sex | Male | 16 (100.0) |
| Female | 0 (0.0) | |
| LVAD type | HMII | 2 (12.5) |
| HM3 | 14 (87.5) | |
| Indication of LVAD | Ischemic heart disease | 11 (68.8) |
| Dilated cardiomyopathy | 4 (25.0) | |
| Fallot tetralogy | 1 (6.3) | |
| Goal of LVAD | Bridge to transplantation | 9 (56.3) |
| Destination therapy | 7 (43.7) | |
| Patients with implantable cardioverter-defibrillator | 9 (56.3) |
| Type of Procedure | n (%) of Procedures |
|---|---|
| Total procedures | 22 |
| Gastrointestinal endoscopy | 13 (59.1) |
| Esophagogastroduodenoscopy 1 | 3 (13.6) |
| Colonoscopy 1 | 10 (45.5) |
| LVAD driveline debridement | 1 (4.5) |
| Rectal neoplasia resection | 1 (4.5) |
| Colostomy | 1 (4.5) |
| Cerebral thrombectomy | 2 (4.5) |
| Cerebral arteriography | 1 (9.1) |
| Cystoscopy | 1 (4.5) |
| Bronchial artery embolization | 1 (4.5) |
| Tracheostomy bleeding | 1 (4.5) |
| Procedural Characteristics | n (%) of Procedures |
|---|---|
| Type of anesthesia | |
| Sedation | 16 (72.7) |
| General anesthesia with endotracheal tube | 3 (13.6) |
| General anesthesia with laryngeal mask | 1 (4.5) |
| General anesthesia with tracheostomy | 1 (4.5) |
| Regional block + sedation | 1 (4.5) |
| Location of the procedure | |
| Endoscopy unit | 13 (59.1) |
| Operating room | 5 (22.7) |
| Interventional radiology unit | 4 (18.2) |
| Monitoring | |
| Standard | 22 (100.0) |
| Capnography | 10 (45.5) |
| Bispectral index scale | 4 (18.2) |
| Arterial catheter | 6 (27.3) |
| Central venous line | 5 (22.7) |
| Transesophageal ultrasound | 2 (9.1) |
| Regional cerebral oxygen saturation | 1 (4.5) |
| Care provided by cardiac anesthesiologist | |
| Yes | 0 (0.0) |
| No | 22 (100.0) |
| Urgency of procedure | |
| Elective | 13 (59.1) |
| Emergent | 9 (40.9) |
| Procedure during LVAD implantation admission | |
| Yes | 6 (27.3) |
| No | 16 (72.7) |
| Number of patients with complications | |
| Intraoperative | 0 (0.0) |
| Postoperative | 8 (36.4) |
| Complications | |
| Gastrointestinal bleeding | 6 (27.3) |
| Ischemic stroke | 1 (4.5) |
| Postoperative vasopressor dependence | 1 (4.5) |
| Acute kidney injury | 1 (4.5) |
| Blood transfusion | |
| Intraoperative | 3 (13.6) |
| Postoperative | 2 (9.1) |
| Use of vasopressors | 5 (22.7) |
| Anticoagulation management | |
| Bridge therapy with heparin | 7 (31.8) |
| Argatroban infusion | 4 (18.2) |
| No bridge therapy | 11 (50.0) |
| Postoperative care | |
| Ward | 13 (59.1) |
| During ICU admission | 5 (22.7) |
| ICU | 2 (9.1) |
| Outpatient | 2 (9.1) |
| Mortality during admission for the procedure | 0 (0.0) |
| Mortality at 30 days after the procedure | 0 (0.0) |
| Procedural Characteristics | n (%) of Procedures |
|---|---|
| Total gastrointestinal endoscopies | 13 |
| Colonoscopy | 10 (45.5) |
| Esophagogastroduodenoscopy | 3 (13.6) |
| Total of patients undergoing endoscopic procedures | 5 (23.3) |
| Indication 1 | |
| Gastrointestinal bleeding | 6 (46.2) |
| Evaluation of a suspected neoplasia | 4 (30.8) |
| Pre-transplant study | 2 (15.4) |
| Follow-up | 1 (7.7) |
| Invasive procedure | 9 (69.2) |
| Length of stay | |
| ≤3 days | 7 (53.8) |
| 4–17 days | 6 (46.2) |
| Monitoring | |
| Standard | 13 (100.0) |
| Capnography | 1 (7.7) |
| Complications | |
| Gastrointestinal bleeding | 6 (46.2) |
| Other | 0 (0.0) |
| Blood transfusion | |
| Postoperative | 2 (15.4) |
| Intraoperative | 0 (0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comino-Trinidad, O.; M. Baltar, I.; Sandoval, E.; Castel, M.Á.; Giménez-Milá, M. Anesthetic Approach for Non-Cardiac Procedures in Patients with a Left Ventricular Assist Device. J. Clin. Med. 2024, 13, 5475. https://doi.org/10.3390/jcm13185475
Comino-Trinidad O, M. Baltar I, Sandoval E, Castel MÁ, Giménez-Milá M. Anesthetic Approach for Non-Cardiac Procedures in Patients with a Left Ventricular Assist Device. Journal of Clinical Medicine. 2024; 13(18):5475. https://doi.org/10.3390/jcm13185475
Chicago/Turabian StyleComino-Trinidad, Oscar, Iria M. Baltar, Elena Sandoval, María Ángeles Castel, and Marc Giménez-Milá. 2024. "Anesthetic Approach for Non-Cardiac Procedures in Patients with a Left Ventricular Assist Device" Journal of Clinical Medicine 13, no. 18: 5475. https://doi.org/10.3390/jcm13185475
APA StyleComino-Trinidad, O., M. Baltar, I., Sandoval, E., Castel, M. Á., & Giménez-Milá, M. (2024). Anesthetic Approach for Non-Cardiac Procedures in Patients with a Left Ventricular Assist Device. Journal of Clinical Medicine, 13(18), 5475. https://doi.org/10.3390/jcm13185475







