Cognitive Function in Patients with Psychotic and Affective Disorders: Effects of Combining Pharmacotherapy with Cognitive Remediation
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Assessments
2.3. Cognitive Remediation Training
2.4. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Neurocognitive Performance
- SCIP total scores at baseline
- SCIP subscale scores at baseline
- Time interval between the two assessments
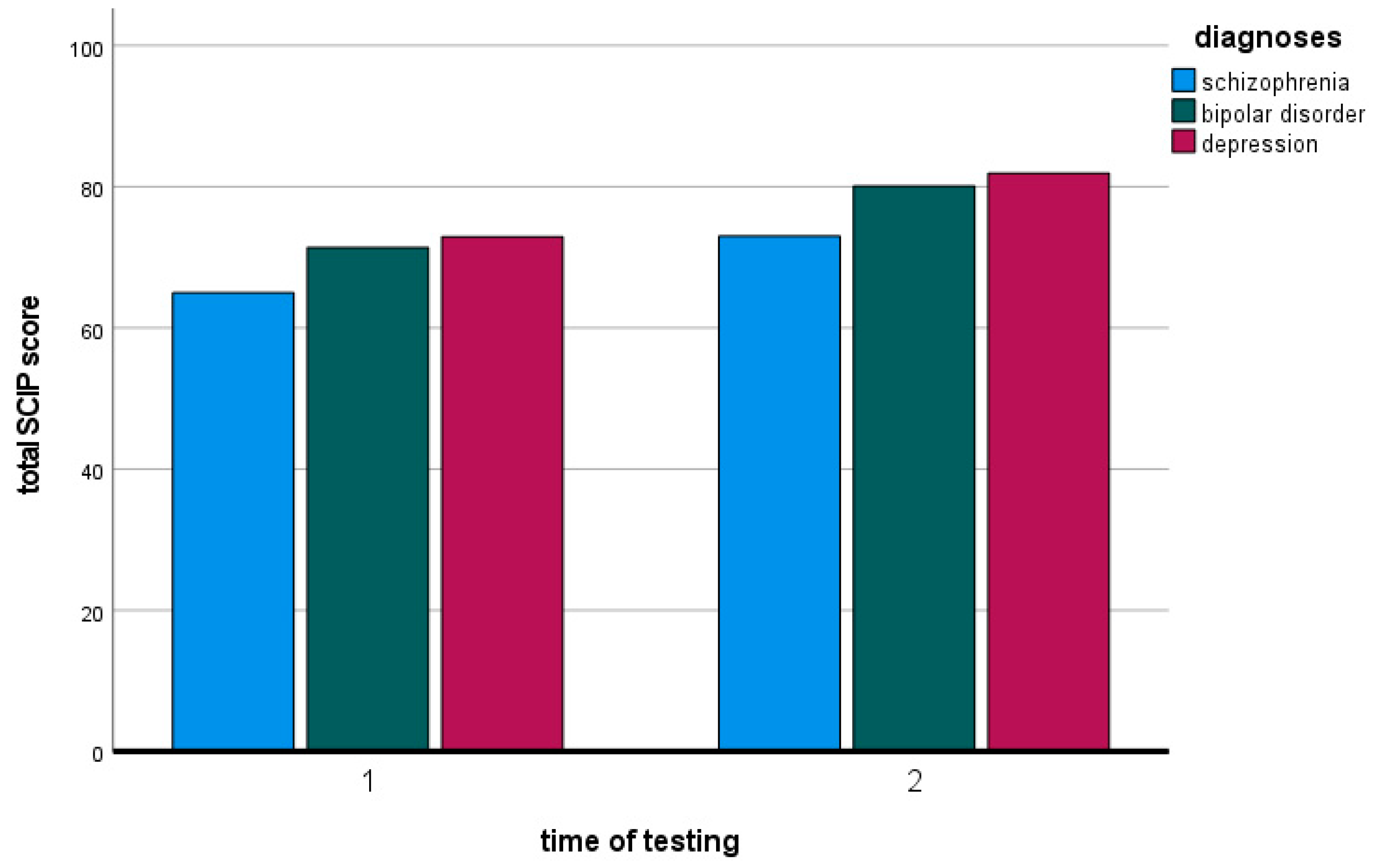
- Comparison of the SCIP total values at the two measurement time points
4. Discussion
- Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sachs, G.; Steger-Wuchse, D.; Kryspin-Exner, I.; Gur, R.C.; Katschnig, H. Facial recognition deficits and cognition in schizophrenia. Schizophr. Res. 2004, 68, 27–35. [Google Scholar] [CrossRef]
- Lee, J.; Altshuler, L.; Glahn, D.C.; Miklowitz, D.J.; Ochsner, K.; Green, M.F. Social and nonsocial cognition in bipolar disorder and schizophrenia: Relative levels of impairment. Am. J. Psychiatry 2013, 170, 334–341. [Google Scholar] [CrossRef]
- Green, M.F.; Harvey, P.D. Cognition in schizophrenia: Past, present, and future. Schizophr. Res. Cogn. 2014, 1, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- McCutcheon, R.A.; Keefe, R.S.E.; McGuire, P.K. Cognitive impairment in schizophrenia: Aetiology, pathophysiology, and treatment. Mol. Psychiatry 2023, 28, 1902–1918. [Google Scholar] [CrossRef]
- Sachs, G.; Erfurth, A. Kognitive Beeinträchtigung in Zusammenhang mit Schizophrenie (CIAS): Diagnostik und Therapie. psychopraxis. neuropraxis 2024, 27, 74–80. [Google Scholar] [CrossRef]
- Mana, L.; Schwartz-Pallejà, M.; Vila-Vidal, M.; Deco, G. Overview on cognitive impairment in psychotic disorders: From impaired microcircuits to dysconnectivity. Schizophr. Res. 2024, 269, 132–143. [Google Scholar] [CrossRef]
- Solé, B.; Jiménez, E.; Torrent, C.; Reinares, M.; Bonnin, C.D.M.; Torres, I.; Varo, C.; Grande, I.; Valls, E.; Salagre, E.; et al. Cognitive Impairment in Bipolar Disorder: Treatment and Prevention Strategies. Int. J. Neuropsychopharmacol. 2017, 20, 670–680. [Google Scholar] [CrossRef] [PubMed]
- Vieta, E.; Berk, M.; Schulze, T.G.; Carvalho, A.F.; Suppes, T.; Calabrese, J.R.; Gao, K.; Miskowiak, K.W.; Grande, I. Bipolar disorders. Nat. Rev. Dis. Primers 2018, 4, 18008. [Google Scholar] [CrossRef]
- Sachs, G.; Berg, A.; Jagsch, R.; Lenz, G.; Erfurth, A. Predictors of Functional Outcome in Patients with Bipolar Disorder: Effects of Cognitive Psychoeducational Group Therapy After 12 Months. Front. Psychiatry 2020, 11, 530026. [Google Scholar] [CrossRef]
- Lam, R.W.; Kennedy, S.H.; McIntyre, R.S.; Khullar, A. Cognitive dysfunction in major depressive disorder: Effects on psychosocial functioning and implications for treatment. Can. J. Psychiatry 2014, 59, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Sachs, G.; Erfurth, A. Kognition bei depressiven Störungen. psychopraxis. neuropraxis 2015, 18, 172–179. [Google Scholar] [CrossRef]
- Gonda, X.; Pompili, M.; Serafini, G.; Carvalho, A.F.; Rihmer, Z.; Dome, P. The role of cognitive dysfunction in the symptoms and remission from depression. Ann. Gen. Psychiatry 2015, 14, 27. [Google Scholar] [CrossRef]
- Knight, M.J.; Baune, B.T. Cognitive dysfunction in major depressive disorder. Curr. Opin. Psychiatry 2018, 31, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Möller, H.J. Systematic of psychiatric disorders between categorical and dimensional approaches: Kraepelin’s dichotomy and beyond. Eur. Arch. Psychiatry Clin. Neurosci. 2008, 258 (Suppl. S2), 48–73. [Google Scholar] [CrossRef]
- Erfurth, A.; Sachs, G. From Griesinger to DSM-V: Do we need the diagnosis of schizophrenia? Eur. Psychiatry 2016, 33, S65. [Google Scholar] [CrossRef]
- Guloksuz, S.; van Os, J. En attendant Godot: Waiting for the Funeral of “Schizophrenia” and the Baby Shower of the Psychosis Spectrum. Front. Psychiatry 2021, 12, 618842. [Google Scholar] [CrossRef] [PubMed]
- Aragona, M. Unitary psychosis (Einheitspsychose): A conceptual history. J. Affect. Disord. 2024, 359, 86–91. [Google Scholar] [CrossRef]
- Li, W.; Zhou, F.C.; Zhang, L.; Ng, C.H.; Ungvari, G.S.; Li, J.; Xiang, Y.T. Comparison of cognitive dysfunction between schizophrenia and bipolar disorder patients: A meta-analysis of comparative studies. J. Affect. Disord. 2020, 274, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, R.; Friedel, H.; Erfurth, A.; Angermayer, M.; Clouth, J.; Eichmann, F. Predisposing factors for early retirement in patients with schizophrenia in Germany. Eur. J. Health Econ. 2008, 9, 265–274. [Google Scholar] [CrossRef]
- Sachs, G.; Winklbaur, B.; Jagsch, R.; Lasser, I.; Kryspin-Exner, I.; Frommann, N.; Wölwer, W. Training of affect recognition (TAR) in schizophrenia—Impact on functional outcome. Schizophr. Res. 2012, 138, 262–267. [Google Scholar] [CrossRef]
- Schirmbeck, F.; van der Burg, N.C.; Blankers, M.; Vermeulen, J.M.; McGuire, P.; Valmaggia, L.R.; Kempton, M.J.; van der Gaag, M.; Riecher-Rössler, A.; Bressan, R.A.; et al. Impact of Comorbid Affective Disorders on Longitudinal Clinical Outcomes in Individuals at Ultra-high Risk for Psychosis. Schizophr. Bull. 2022, 48, 100–110. [Google Scholar] [CrossRef]
- Jiménez-López, E.; Villanueva-Romero, C.M.; Sánchez-Morla, E.M.; Martínez-Vizcaíno, V.; Ortiz, M.; Rodriguez-Jimenez, R.; Vieta, E.; Santos, J.L. Neurocognition, functional outcome, and quality of life in remitted and non-remitted schizophrenia: A comparison with euthymic bipolar I disorder and a control group. Schizophr. Res. 2022, 240, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Giordano, G.M.; Pezzella, P.; Mucci, A.; Austin, S.; Erfurth, A.; Glenthøj, B.; Hofer, A.; Hubenak, J.; Libiger, J.; Melle, I.; et al. Negative symptoms and social cognition as mediators of the relationship between neurocognition and functional outcome in schizophrenia. Front. Psychiatry 2024, 15, 1333711. [Google Scholar] [CrossRef]
- Vita, A.; Gaebel, W.; Mucci, A.; Sachs, G.; Erfurth, A.; Barlati, S.; Zanca, F.; Giordano, G.M.; Birkedal Glenthøj, L.; Nordentoft, M.; et al. European Psychiatric Association guidance on assessment of cognitive impairment in schizophrenia. Eur. Psychiatry 2022, 65, e58. [Google Scholar] [CrossRef]
- Nuechterlein, K.H.; Green, M.F.; Kern, R.S.; Baade, L.E.; Barch, D.M.; Cohen, J.D.; Essock, S.; Fenton, W.S.; Frese, F.J., 3rd; Gold, J.M.; et al. The MATRICS Consensus Cognitive Battery, part 1: Test selection, reliability, and validity. Am. J. Psychiatry 2008, 165, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Keefe, R.S.; Goldberg, T.E.; Harvey, P.D.; Gold, J.M.; Poe, M.P.; Coughenour, L. The Brief Assessment of Cognition in Schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr. Res. 2004, 68, 283–297. [Google Scholar] [CrossRef]
- Sachs, G.; Winklbaur, B.; Jagsch, R.; Keefe, R.S. Validation of the German version of the brief assessment of cognition in Schizophrenia (BACS)—Preliminary results. Eur. Psychiatry 2011, 26, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Purdon, S.E. The Screen for Cognitive Impairment in Psychiatry (SCIP): Instructions and Three Alternate Forms; PNL Inc.: Edmonton, AB, Canada, 2005. [Google Scholar]
- Gómez-Benito, J.; Guilera, G.; Pino, Ó.; Rojo, E.; Tabarés-Seisdedos, R.; Safont, G.; Martínez-Arán, A.; Franco, M.; Cuesta, M.J.; Crespo-Facorro, B.; et al. The screen for cognitive impairment in psychiatry: Diagnostic-specific standardization in psychiatric ill patients. BMC Psychiatry 2013, 13, 127. [Google Scholar] [CrossRef]
- Sachs, G.; Lasser, I.; Purdon, S.E.; Erfurth, A. Screening for cognitive impairment in schizophrenia: Psychometric properties of the German version of the Screen for Cognitive Impairment in Psychiatry (SCIP-G). Schizophr. Res. Cogn. 2021, 25, 100197. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Czekaj, A.; Frick, J.; Steinert, T.; Purdon, S.E.; Uhlmann, C. The screen for cognitive impairment in psychiatry (SCIP) as a routinely applied screening tool: Pathology of acute psychiatric inpatients and cluster analysis. BMC Psychiatry 2021, 21, 494. [Google Scholar] [CrossRef]
- Marder, S.R. Drug initiatives to improve cognitive function. J. Clin. Psychiatry 2006, 67 (Suppl. S9), 31–35; discussion 36–42. [Google Scholar] [CrossRef] [PubMed]
- McGurk, S.R.; Mueser, K.T.; DeRosa, T.J.; Wolfe, R. Work, recovery, and comorbidity in schizophrenia: A randomized controlled trial of cognitive remediation. Schizophr. Bull. 2009, 35, 319–335. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, M.M.; Mueser, K.T.; Thime, W.R.; Corbera, S.; Wexler, B.E. Social skills training and computer-assisted cognitive remediation in schizophrenia. Schizophr. Res. 2015, 162, 35–41. [Google Scholar] [CrossRef]
- Vita, A.; Gaebel, W.; Mucci, A.; Sachs, G.; Barlati, S.; Giordano, G.M.; Nibbio, G.; Nordentoft, M.; Wykes, T.; Galderisi, S. European Psychiatric Association guidance on treatment of cognitive impairment in schizophrenia. Eur. Psychiatry 2022, 65, e57. [Google Scholar] [CrossRef] [PubMed]
- Mueller, D.R. Editorial: Integrated therapy approaches in schizophrenia: Evidence and limitations. Front. Psychiatry 2023, 14, 1142493. [Google Scholar] [CrossRef] [PubMed]
- Horan, W.P.; Catalano, L.T.; Green, M.F. An Update on Treatment of Cognitive Impairment Associated with Schizophrenia. Curr. Top. Behav. Neurosci. 2023, 63, 407–436. [Google Scholar] [CrossRef] [PubMed]
- Wykes, T.; Huddy, V.; Cellard, C.; McGurk, S.R.; Czobor, P. A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. Am. J. Psychiatry 2011, 168, 472–485. [Google Scholar] [CrossRef]
- Mothersill, D.; Donohoe, G. Neural Effects of Cognitive Training in Schizophrenia: A Systematic Review and Activation Likelihood Estimation Meta-analysis. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2019, 4, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Furtner, J.; Schöpf, V.; Erfurth, A.; Sachs, G. An fMRI study of cognitive remediation in drug-naïve subjects diagnosed with first episode schizophrenia. Wien. Klin. Wochenschr. 2021, 134, 249–254. [Google Scholar] [CrossRef]
- Motter, J.N.; Pimontel, M.A.; Rindskopf, D.; Devanand, D.P.; Doraiswamy, P.M.; Sneed, J.R. Computerized cognitive training and functional recovery in major depressive disorder: A meta-analysis. J. Affect. Disord. 2016, 189, 184–191. [Google Scholar] [CrossRef]
- Mokhtari, S.; Mokhtari, A.; Bakizadeh, F.; Moradi, A.; Shalbafan, M. Cognitive rehabilitation for improving cognitive functions and reducing the severity of depressive symptoms in adult patients with Major Depressive Disorder: A systematic review and meta-analysis of randomized controlled clinical trials. BMC Psychiatry 2023, 23, 77. [Google Scholar] [CrossRef] [PubMed]
- Tsapekos, D.; Seccomandi, B.; Mantingh, T.; Cella, M.; Wykes, T.; Young, A.H. Cognitive enhancement interventions for people with bipolar disorder: A systematic review of methodological quality, treatment approaches, and outcomes. Bipolar Disord. 2020, 22, 216–230. [Google Scholar] [CrossRef] [PubMed]
- Carta, M.G.; Kurotschka, P.K.; Machado, S.; Erfurth, A.; Sancassiani, F.; Perra, A.; Tusconi, M.; Cossu, G.; Aviles Gonzalez, C.I.; Primavera, D. A Virtual Reality Cognitive Stimulation Program as an Effective Tool Against Residual/Prodromal Depressive Symptoms in Bipolar Disorders. J. Clin. Med. 2024, 13, 4714. [Google Scholar] [CrossRef]
- Sachs, G.; Bannick, G.; Maihofer, E.I.J.; Voracek, M.; Purdon, S.E.; Erfurth, A. Dimensionality analysis of the German version of the Screen for Cognitive Impairment in Psychiatry (SCIP-G). Schizophr. Res. Cogn. 2022, 29, 100259. [Google Scholar] [CrossRef] [PubMed]
- Marker, K.R. COGPACK. The Cognitive Training Package Manual; Marker software: Heidelberg, Germany; Ladenburg, Germany, 2002. [Google Scholar]
- Harada, C.N.; Natelson Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Lehrl, S. Mehrfachwahl-Wortschatz-Intelligenztest (MWT-B); Straube: Erlangen, Germany, 1997. [Google Scholar]
- World Health Organization. Internationale Klassifikation psychischer Störungen: ICD-10 Kapitel V (F). Diagnostische Kriterien für Forschung und Praxis; Dilling, H., Mombour, W., Schmidt, M.H., Schulte-Markwort, E., Eds.; 5 überarbeitete Auflage; Hans Huber: Bern, Switzerland, 2011; ISBN 978-3456849560. [Google Scholar]
- Cuesta, M.J.; Pino, O.; Guilera, G.; Rojo, J.E.; Gómez-Benito, J.; Purdon, S.E.; Franco, M.; Martínez-Arán, A.; Segarra, N.; Tabarés-Seisdedos, R.; et al. Brief cognitive assessment instruments in schizophrenia and bipolar patients, and healthy control subjects: A comparison study between the Brief Cognitive Assessment Tool for Schizophrenia (B-CATS) and the Screen for Cognitive Impairment in Psychiatry (SCIP). Schizophr. Res. 2011, 130, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Esan, O.; Oladele, O.; Adediran, K.I.; Abiona, T.O. Neurocognitive Impairments (NCI) in bipolar disorder: Comparison with schizophrenia and healthy controls. J. Affect. Disord. 2020, 277, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Jabben, N.; Arts, B.; van Os, J.; Krabbendam, L. Neurocognitive functioning as intermediary phenotype and predictor of psychosocial functioning across the psychosis continuum: Studies in schizophrenia and bipolar disorder. J. Clin. Psychiatry 2010, 71, 764–774. [Google Scholar] [CrossRef]
- Terachi, S.; Yamada, T.; Pu, S.; Yokoyama, K.; Matsumura, H.; Kaneko, K. Comparison of neurocognitive function in major depressive disorder, bipolar disorder, and schizophrenia in later life: A cross-sectional study of euthymic or remitted, non-demented patients using the Japanese version of the Brief Assessment of Cognition in Schizophrenia (BACS-J). Psychiatry Res. 2017, 254, 205–210. [Google Scholar] [CrossRef]
- Mucci, A.; Vignapiano, A.; Bitter, I.; Austin, S.F.; Delouche, C.; Dollfus, S.; Erfurth, A.; Fleischhacker, W.W.; Giordano, G.M.; Gladyshev, I.; et al. A large European, multicenter, multinational validation study of the Brief Negative Symptom Scale. Eur. Neuropsychopharmacol. 2019, 29, 947–959. [Google Scholar] [CrossRef]
- Dollfus, S.; Mucci, A.; Giordano, G.M.; Bitter, I.; Austin, S.F.; Delouche, C.; Erfurth, A.; Fleischhacker, W.W.; Movina, L.; Glenthøj, B.; et al. European validation of the Self-evaluation of Negative Symptoms (SNS): A large multinational and multicenter study. Front. Psychiatry 2022, 13, 826465. [Google Scholar] [CrossRef] [PubMed]
- Marder, S.R.; Umbricht, D. Negative symptoms in schizophrenia: Newly emerging measurements, pathways, and treatments. Schizophr. Res. 2023, 258, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Huang, C.L.; Chang, Y.C.; Chen, P.W.; Lin, C.Y.; Tsai, G.E.; Lane, H.Y. Clinical symptoms, mainly negative symptoms, mediate the influence of neurocognition and social cognition on functional outcome of schizophrenia. Schizophr. Res. 2013, 146, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Oldham, J.M.; Golden, W.E.; Rosof, B.M. Quality improvement in psychiatry: Why measures matter. J Psychiatr Pr. 2008, 14 (Suppl. S2), 8–17. [Google Scholar] [CrossRef] [PubMed]
- Correll, C.U.; Arango, C.; Fagiolini, A.; Giordano, G.M.; Leucht, S.; Salazar de Pablo, G. Finding the Right Setting for the Right Treatment During the Acute Treatment of Individuals with Schizophrenia: A Narrative Review and Clinical Practice Guideline. Neuropsychiatr. Dis. Treat. 2024, 20, 1293–1307. [Google Scholar] [CrossRef]
- Fleischhacker, W.W.; Allen, C.; Erfurth, A.; Hofer, A.; Lehofer, M.; Marksteiner, J.; Musalek, M.; Psota, G.; Rothenhäusler, H.B.; Schöny, W.; et al. Therapieadhärenz bei Schizophrenie-Patienten. Psychiatr Psychother 2011, 7, 98–109. [Google Scholar] [CrossRef]
- Garriga, M.; Pacchiarotti, I.; Kasper, S.; Zeller, S.L.; Allen, M.H.; Vázquez, G.; Baldaçara, L.; San, L.; McAllister-Williams, R.H.; Fountoulakis, K.N.; et al. Assessment and management of agitation in psychiatry: Expert consensus. World J. Biol. Psychiatry 2016, 17, 86–128. [Google Scholar] [CrossRef]
- Erfurth, A. Agitation: A central challenge in psychiatry. World J. Biol. Psychiatry 2017, 18, 3–4. [Google Scholar] [CrossRef]
- Chiu, M.Y.; Davidson, L.; Lo, W.T.; Yiu, M.G.; Ho, W.W. Modeling self-agency among people with schizophrenia: Empirical evidence for consumer-based recovery. Psychopathology 2013, 46, 413–420. [Google Scholar] [CrossRef]
- Vauth, R.; Kleim, B.; Wirtz, M.; Corrigan, P.W. Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Res. 2007, 150, 71–80. [Google Scholar] [CrossRef]

| ICD-10 Code | Diagnosis | n | % |
|---|---|---|---|
| F20.0 | Paranoid schizophrenia | 30 | 55.6 |
| F20.1 | Hebephrenic schizophrenia | 2 | 3.7 |
| F20.3 | Undifferentiated schizophrenia | 1 | 1.9 |
| F22.0 | Delusional disorder | 1 | 1.9 |
| F23.0 | Acute polymorphic psychotic disorder without symptoms of schizophrenia | 1 | 1.9 |
| F23.1 | Acute polymorphic psychotic disorder with symptoms of schizophrenia | 4 | 7.4 |
| F23.8 | Other acute and transient psychotic disorders | 1 | 1.9 |
| F25.0 | Schizoaffective disorder, manic type | 3 | 5.6 |
| F25.1 | Schizoaffective disorder, depressive type | 7 | 13.0 |
| F25.2 | Schizoaffective disorder, mixed type | 4 | 7.4 |
| F2 total | Schizophrenia, schizotypal and delusional disorders | 54 | 100.0 |
| F30.2 | Mania with psychotic symptoms | 3 | 7.7 |
| F31.0 | Bipolar affective disorder, current episode hypomanic | 4 | 10.3 |
| F31.1 | Bipolar affective disorder, current episode manic without psychotic symptoms | 2 | 5.1 |
| F31.2 | Bipolar affective disorder, current episode manic with psychotic symptoms | 12 | 30.8 |
| F31.8 | Other bipolar affective disorders (Recurrent manic episodes) | 1 | 2.6 |
| Mania subtotal | 22 | 56.4 | |
| F31.3 | Bipolar affective disorder, current episode mild or moderate depression | 6 | 15.4 |
| F31.4 | Bipolar affective disorder, current episode severe depression without psychotic symptoms | 7 | 17.9 |
| F31.5 | Bipolar affective disorder, current episode severe depression with psychotic symptoms | 2 | 5.1 |
| Bipolar depressed subtotal | 15 | 38.5 | |
| F31.6 | Bipolar affective disorder, current episode mixed | 2 | 5.1 |
| F30/31 total | Manic episode/Bipolar affective disorder | 39 | 100.0 |
| F32.1 | Moderate depressive episode | 6 | 12.0 |
| F32.2 | Severe depressive episode without psychotic symptoms | 11 | 22.0 |
| F32.3 | Severe depressive episode with psychotic symptoms | 5 | 10.0 |
| F33.1 | Recurrent depressive disorder, current episode moderate | 6 | 12.0 |
| F33.2 | Recurrent depressive disorder, current episode severe without psychotic symptoms | 20 | 40.0 |
| F33.3 | Recurrent depressive disorder, current episode severe with psychotic symptoms | 2 | 4.0 |
| F32/33 total | Depressive episode/Recurrent depressive disorder | 50 | 100.0 |
| Diagnosis | Total n | Female n | Male n | Age Mean (SD) | MWT-B Mean (SD) | Years of Education Mean (SD) |
|---|---|---|---|---|---|---|
| psychotic disorders | 54 | 30 | 24 | 35.41 (10.93) | 27.11 (5.67) | 14.26 (3.51) |
| bipolar disorder | 39 | 25 | 14 | 40.56 (14.56) | 28.85 (4.49) | 14.99 (3.65) |
| depression | 50 | 29 | 21 | 38.70 (12.45) | 28.50 (4.99) | 13.94 (3.29) |
| Timepoint 1 | Timepoint 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | n | Mean Value | Standard Deviation | Range | Mean Value | Standard Deviation | Range | Improvement of Mean Values between Timepoints |
| psychotic disorders | 54 | 64.98 | 12.872 | 36–89 | 73.00 | 11.808 | 42–100 | 8.02 |
| bipolar disorder | 39 | 71.38 | 10.946 | 52–95 | 80.10 | 11.805 | 58–107 | 8.72 |
| depression | 50 | 72.92 | 9.710 | 45–90 | 81.90 | 11.379 | 61–109 | 8.98 |
| Diagnosis | Verbal Learning Mean (SD) | Working Memory Mean (SD) | Verbal Fluency Mean (SD) | Verbal Learning—Delayed Mean (SD) | Processing Speed Mean (SD) |
|---|---|---|---|---|---|
| psychotic disorders | 21.35 (4.344) *# | 17.48 (4.437) # | 11.04 (4.273) * | 6.76 (2.363) # | 8.59 (2.716) # |
| bipolar disorder | 23.49 (4.019) * | 18.64 (3.166) | 13.23 (4.457) * | 7.41 (2.035) | 8.82 (2.827) |
| depression | 23.57 (3.266) # | 19.55 (3.163) # | 12.37 (3.712) | 8.08 (2.029) # | 9.84 (2.946) # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maihofer, E.I.J.; Sachs, G.; Erfurth, A. Cognitive Function in Patients with Psychotic and Affective Disorders: Effects of Combining Pharmacotherapy with Cognitive Remediation. J. Clin. Med. 2024, 13, 4843. https://doi.org/10.3390/jcm13164843
Maihofer EIJ, Sachs G, Erfurth A. Cognitive Function in Patients with Psychotic and Affective Disorders: Effects of Combining Pharmacotherapy with Cognitive Remediation. Journal of Clinical Medicine. 2024; 13(16):4843. https://doi.org/10.3390/jcm13164843
Chicago/Turabian StyleMaihofer, Eva I. J., Gabriele Sachs, and Andreas Erfurth. 2024. "Cognitive Function in Patients with Psychotic and Affective Disorders: Effects of Combining Pharmacotherapy with Cognitive Remediation" Journal of Clinical Medicine 13, no. 16: 4843. https://doi.org/10.3390/jcm13164843
APA StyleMaihofer, E. I. J., Sachs, G., & Erfurth, A. (2024). Cognitive Function in Patients with Psychotic and Affective Disorders: Effects of Combining Pharmacotherapy with Cognitive Remediation. Journal of Clinical Medicine, 13(16), 4843. https://doi.org/10.3390/jcm13164843







