Two Decades of CABG in the UK: A Propensity Matched Analysis of Outcomes by Conduit Choice
Abstract
1. Introduction
2. Materials and Methods
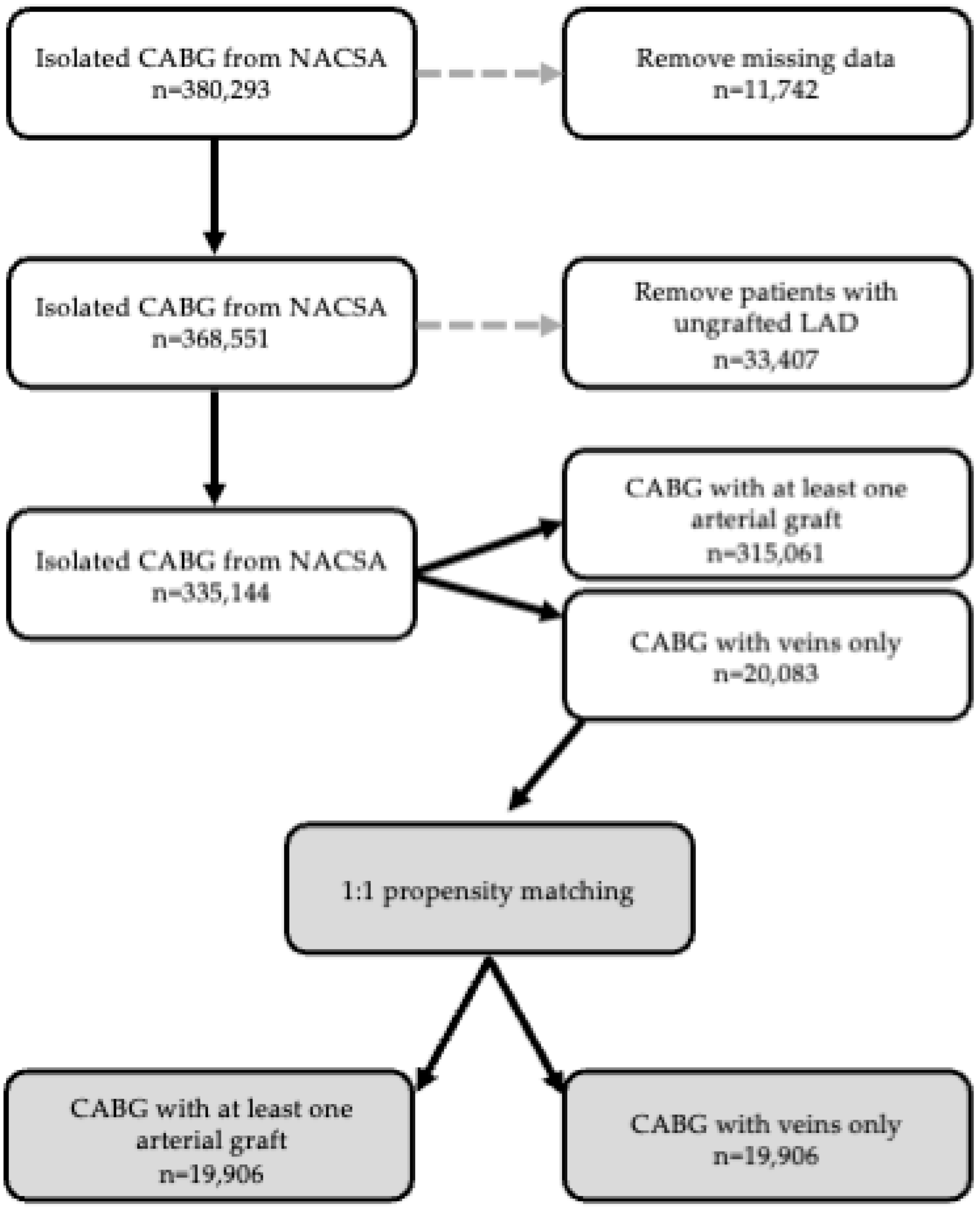
2.1. Participants
2.2. Ethics
2.3. Statistical Analysis
3. Results
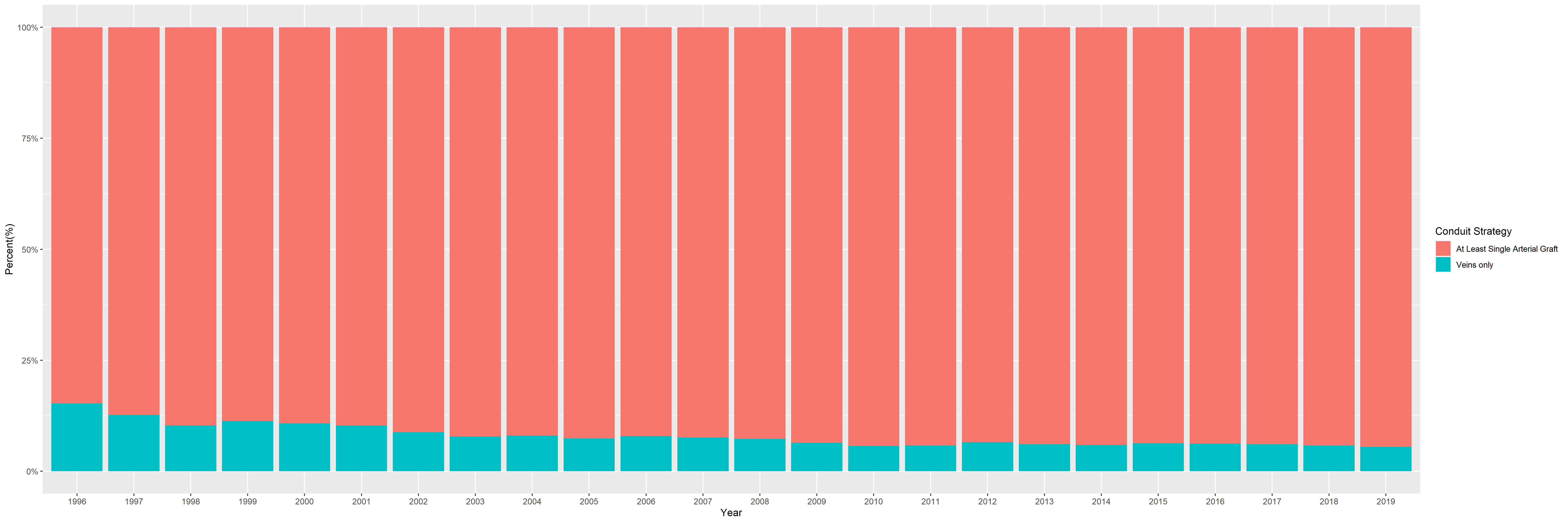
3.1. Unmatched Population Cohort
3.1.1. Baseline and Intra-Operative Patient Characteristics
3.1.2. In-Hospital Outcomes in the Whole Population
3.2. Matched Population Cohort
3.2.1. Baseline and Intra-Operative Patient Characteristics
3.2.2. In-Hospital Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guan, C.; Wu, S.; Xu, W.; Zhang, J. Global, regional, and national burden of ischaemic heart disease and its trends, 1990–2019. Public Health 2023, 223, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Sandner, S.; An, K.R.; Dimagli, A.; Di Franco, A.; Audisio, K.; Harik, L.; Perezgrovas-Olaria, R.; Soletti, G.; Fremes, S.E.; et al. Graft Failure After Coronary Artery Bypass Grafting and Its Association With Patient Characteristics and Clinical Events: A Pooled Individual Patient Data Analysis of Clinical Trials With Imaging Follow-Up. Circulation 2023, 148, 1305–1315. [Google Scholar] [CrossRef]
- Chan, J.; Dimagli, A.; Dong, T.; Fudulu, D.P.; Sinha, S.; Angelini, G.D. Trend and factors associated with multiple arterial revascularization in coronary artery bypass grafting in the UK. Eur. J. Cardio-Thorac Surg. 2022, 62, ezac284. [Google Scholar] [CrossRef]
- Neumann, F.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.; Benedetto, U.; Byrne, R.; Collet, J.; Falk, V.; Head, S.; et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Al-Ruzzeh, S.; George, S.; Bustami, M.; Nakamura, K.; Ilsley, C.; Amrani, M. Early clinical and angiographic outcome of the pedicled right internal thoracic artery graft to the left anterior descending artery. Ann. Thorac. Surg. 2002, 73, 1431–1435. [Google Scholar] [CrossRef]
- Kawata, T.; Taniguchi, S.; Nishioka, H.; Kobayashi, S.; Mizuguchi, K.; Kameda, Y.; Sakaguchi, S.; Tsuji, T.; Kitamura, S. Benefits accruing to grafting of the right internal thoracic artery to the left anterior descending artery in coronary artery bypass grafting. Jpn. J. Thorac. Cardiovasc. Surg. 1999, 47, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Ladak, S.S.; McQueen, L.W.; Layton, G.R.; Aujla, H.; Adebayo, A.; Zakkar, M. The Role of Endothelial Cells in the Onset, Development and Modulation of Vein Graft Disease. Cells 2022, 11, 3066. [Google Scholar] [CrossRef]
- Layton, G.R.; Ladak, S.S.; Abbasciano, R.; McQueen, L.W.; George, S.J.; Murphy, G.J.; Zakkar, M. The Role of Preservation Solutions upon Saphenous Vein Endothelial Integrity and Function: Systematic Review and UK Practice Survey. Cells 2023, 12, 815. [Google Scholar] [CrossRef] [PubMed]
- Goldman, S.; Zadina, K.; Moritz, T.; Ovitt, T.; Sethi, G.; Copeland, J.G.; Thottapurathu, L.; Krasnicka, B.; Ellis, N.; Anderson, R.J.; et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a Department of Veterans Affairs Cooperative Study. J. Am. Coll. Cardiol. 2004, 44, 2149–2156. [Google Scholar] [CrossRef]
- Hickey, G.L.; Bridgewater, B.; Grant, S.W.; Deanfield, J.; Parkinson, J.; Bryan, A.J.; Dalrymple-Hay, M.; Moat, N.; Buchan, I.; Dunning, J. National Registry Data and Record Linkage to Inform Postmarket Surveillance of Prosthetic Aortic Valve Models Over 15 Years. JAMA Intern. Med. 2017, 177, 79–86. [Google Scholar] [CrossRef]
- Benedetto, U.; Sinha, S.; Dimagli, A.; Cooper, G.; Mariscalco, G.; Uppal, R.; Moorjani, N.; Krasopoulos, G.; Kaura, A.; Field, M.; et al. Decade-long trends in surgery for acute Type A aortic dissection in England: A retrospective cohort study. Lancet Reg. Health Eur. 2021, 7, 100131. [Google Scholar] [CrossRef] [PubMed]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Austin, P.C. Comparing paired vs non-paired statistical methods of analyses when making inferences about absolute risk reductions in propensity-score matched samples. Stat. Med. 2011, 30, 1292–1301. [Google Scholar] [CrossRef] [PubMed]
- Greifer, N.; Stuart, E.A. Matching Methods for Confounder Adjustment: An Addition to the Epidemiologist’s Toolbox. Epidemiol. Rev. 2022, 43, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Greifer, N. Estimating Effects after Matching. Available online: https://cran.r-project.org/web/packages/MatchIt/vignettes/estimating-effects.html (accessed on 30 May 2024).
- Greifer, N. MatchIt: Getting Started. Available online: https://cran.r-project.org/web/packages/MatchIt/vignettes/MatchIt.html (accessed on 30 May 2024).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2010. [Google Scholar]
- Team, R. RStudio: Integrated Development for R Studio; PBC: Boston, MA, USA, 2020; Available online: www.rstudio.com (accessed on 30 May 2024).
- McGuigan, A.; Beattie, R.; Graham, A. Coronary Artery Bypass Grafting without a Left Anterior Descending Artery Graft—Is It Worth It?: 0254. Int. J. Surg. 2014, 12, S19–S20. [Google Scholar] [CrossRef][Green Version]
- Masroor, M.; Zhou, K.; Chen, C.; Fu, X.; Zhao, Y. All we need to know about internal thoracic artery harvesting and preparation for myocardial revascularization: A systematic review. J. Cardiothorac. Surg. 2021, 16, 354. [Google Scholar] [CrossRef] [PubMed]
- Pillai, V.V.; Sreekanthan, R.; Karunakaran, J. Quantitative estimation of LIMA blood flow between extraluminal papavarine vs extraluminal papavarine plus intraluminal vasodilator cocktail in CABG patients. Ann. Card. Anaesth. 2020, 23, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Li, B.; Zhang, W.; Wang, Z.; Ye, X.; Zhou, M.; Li, H.; Qiu, J.; Zhu, Y.; Zhao, Q. Risk factors for major adverse cardiovascular events after coronary artery bypass grafting using radial artery grafts. Front. Cardiovasc. Med. 2023, 10, 1238161. [Google Scholar] [CrossRef] [PubMed]
- Dion, R.; Glineur, D.; Derouck, D.; Verhelst, R.; Noirhomme, P.; El Khoury, G.; Degrave, E.; Hanet, C. Complementary saphenous grafting: Long-term follow-up. J. Thorac. Cardiovasc. Surg. 2001, 122, 296–304. [Google Scholar] [CrossRef][Green Version]
- Axelsson, T.A.; Mennander, A.; Malmberg, M.; Gunn, J.; Jeppsson, A.; Gudbjartsson, T. Is emergency and salvage coronary artery bypass grafting justified? The Nordic Emergency/Salvage coronary artery bypass grafting study. Eur. J. Cardio-Thoracic Surg. 2015, 49, 1451–1456. [Google Scholar] [CrossRef]
- Cuminetti, G.; Gelsomino, S.; Curello, S.; Lorusso, R.; Maessen, J.G.; Hoorntje, J.C. Contemporary use of arterial and venous conduits in coronary artery bypass grafting: Anatomical, functional and clinical aspects. Neth. Heart J. 2017, 25, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Kieser, T.M.; Rose, M.S.; Aluthman, U.; Narine, K. Quicker yet safe: Skeletonization of 1640 internal mammary arteries with harmonic technology in 965 patients. Eur. J. Cardio-Thoracic Surg. 2014, 45, e142–e150. [Google Scholar] [CrossRef]
- Deb, S.; Cohen, E.A.; Singh, S.K.; Une, D.; Laupacis, A.; Fremes, S.E. Radial artery and saphenous vein patency more than 5 years after coronary artery bypass surgery: Results from RAPS (Radial Artery Patency Study). J. Am. Coll. Cardiol. 2012, 60, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [PubMed]
| Conduit Strategy | |||||
|---|---|---|---|---|---|
| Characteristic | Overall, N = 335,144 1 | At Least Single Arterial Graft, N = 315,061 1 | Veins Only, N = 20,083 1 | p-Value 2 | Standardised Mean Difference |
| Age (years) | 49 (42, 55) | 48 (41, 55) | 53 (46, 59) | <0.001 | 0.429 |
| Gender | <0.001 | 0.262 | |||
| Female | 62,898 (19%) | 56,857 (18%) | 6041 (30%) | ||
| Pulmonary Disease | <0.001 | 0.156 | |||
| 38,300 (11%) | 34,896 (11%) | 3404 (17%) | |||
| Peripheral Vascular Disease | <0.001 | 0.166 | |||
| 42,983 (13%) | 39,177 (12%) | 3806 (19%) | |||
| Poor mobility pre-op | <0.001 | 0.068 | |||
| 7228 (2.2%) | 6563 (2.1%) | 665 (3.3%) | |||
| Creatinine > 200 μmol/L | <0.001 | 0.118 | |||
| 5651 (1.7%) | 4885 (1.6%) | 766 (3.8%) | |||
| Unstable angina | <0.001 | 0.296 | |||
| 59,649 (18%) | 53,491 (17%) | 6158 (31%) | |||
| Good LV Function | 289,028 (86%) | 272,139 (86%) | 16,889 (84%) | <0.001 | |
| Moderate LV Function | 0.016 | 0.173 | |||
| 39,301 (12%) | 36,839 (12%) | 2462 (12%) | |||
| Poor LV Function | <0.001 | 0.072 | |||
| 5266 (1.6%) | 4730 (1.5%) | 536 (2.7%) | |||
| Very poor LV Function | <0.001 | 0.056 | |||
| 1577 (0.5%) | 1377 (0.4%) | 200 (1.0%) | |||
| Redo | <0.001 | 0.257 | |||
| 6472 (1.9%) | 4711 (1.5%) | 1761 (8.8%) | |||
| Critical Pre-operative State | <0.001 | 0.237 | |||
| 7724 (2.3%) | 6010 (1.9%) | 1714 (8.5%) | |||
| Recent MI | <0.001 | 0.131 | |||
| 83,027 (25%) | 76,908 (24%) | 6119 (30%) | |||
| Pulmonary Hypertension | <0.001 | 0.051 | |||
| 1684 (0.5%) | 1488 (0.5%) | 196 (1.0%) | |||
| Elective case | 213,994 (64%) | 203,893 (65%) | 10,101 (50%) | <0.001 | |
| Urgent case | <0.001 | 0.113 | |||
| 113,138 (34%) | 105,310 (33%) | 7828 (39%) | |||
| Emergency case | <0.001 | 0.247 | |||
| 7161 (2.1%) | 5417 (1.7%) | 1744 (8.7%) | |||
| Salvage case | <0.001 | 0.133 | |||
| 555 (0.2%) | 181 (<0.1%) | 374 (1.9%) | |||
| NYHA I | <0.001 | - | |||
| 103,164 (31%) | 97,973 (31%) | 5191 (26%) | |||
| NYHA II | <0.001 | - | |||
| 152,847 (46%) | 144,602 (46%) | 8245 (41%) | |||
| NYHA III | <0.001 | - | |||
| 68,942 (21%) | 63,755 (20%) | 5187 (26%) | |||
| NYHA IV | <0.001 | 0.173 | |||
| 10,191 (3.0%) | 8731 (2.8%) | 1460 (7.3%) | |||
| CCS 0 | <0.001 | - | |||
| 33,417 (10.0%) | 31,578 (10%) | 1839 (9.2%) | |||
| CCS 1 | <0.001 | - | |||
| 29,928 (8.9%) | 28,514 (9.1%) | 1414 (7.0%) | |||
| CCS 2 | <0.001 | - | |||
| 117,837 (35%) | 112,404 (36%) | 5433 (27%) | |||
| CCS 3 | 0.006 | - | |||
| 105,607 (32%) | 99,103 (31%) | 6504 (32%) | |||
| CCS 4 | <0.001 | 0.246 | |||
| 48,355 (14%) | 43,462 (14%) | 4893 (24%) | |||
| BMI | 27.8 (25.4, 30.9) | 27.8 (25.4, 30.9) | 27.3 (24.6, 30.3) | <0.001 | 0.150 |
| Mechanical Support | <0.001 | 0.105 | |||
| Required | 2679 (0.8%) | 2220 (0.7%) | 459 (2.3%) | ||
| Pump Case | <0.001 | 0.344 | |||
| Off pump | 50,801 (15%) | 49,409 (16%) | 1392 (6.9%) | ||
| On pump | 284,343 (85%) | 265,652 (84%) | 18,691 (93%) | ||
| Diet controlled Diabetes | 13,830 (4.1%) | 12,754 (4.0%) | 1076 (5.4%) | <0.001 | - |
| Diabetes on oral medications | 46,153 (14%) | 43,403 (14%) | 2750 (14%) | 0.7 | - |
| Diabetes on insulin | <0.001 | 0.029 | |||
| 25,338 (7.6%) | 23,664 (7.5%) | 1674 (8.3%) | |||
| EuroScore II | 1.05 (0.75, 1.64) | 1.02 (0.74, 1.58) | 1.66 (1.03, 2.99) | <0.001 | - |
| CPB Time(mins) | 78 (58, 99) | 78 (58, 98) | 80 (61, 104) | <0.001 | - |
| Missing | 36,256 | 34,657 | 1599 | ||
| Cross Clamp Time(mins) | 44 (31, 59) | 44 (31, 59) | 38 (27, 54) | <0.001 | - |
| Missing | 36,594 | 34,943 | 1651 | ||
| Preop IABP | <0.001 | - | |||
| Used | 2653 (0.8%) | 2200 (0.7%) | 453 (2.3%) | ||
| Conduit Strategy | ||||
|---|---|---|---|---|
| Characteristic | Overall, N = 335,144 1 | At Least Single Arterial Graft, N = 315,061 1 | Veins Only, N = 20,083 1 | p-Value 2 |
| Mortality | 5847 (1.8%) | 4711 (1.5%) | 1136 (5.7%) | <0.001 |
| Missing | 2007 | 1910 | 97 | |
| CVA | <0.001 | |||
| 5447 (1.7%) | 4973 (1.7%) | 474 (2.6%) | ||
| Missing | 21,617 | 19,963 | 1654 | |
| TIA | <0.001 | |||
| 11,246 (3.6%) | 10,326 (3.5%) | 920 (5.0%) | ||
| Missing | 21,617 | 19,963 | 1654 | |
| Dialysis | 6330 (2.1%) | 5555 (2.0%) | 775 (4.4%) | <0.001 |
| Missing | 38,497 | 35,888 | 2609 | |
| Intraoperative/postoperative IABP insertion | <0.001 | |||
| Used | 2687 (0.8%) | 2272 (0.7%) | 415 (2.1%) | |
| Return to theatre for bleeding/tamponade | 9821 (2.9%) | 9022 (2.9%) | 799 (4.0%) | <0.001 |
| Return to theatre for graft complications | 425 (0.1%) | 391 (0.1%) | 34 (0.2%) | 0.081 |
| Return to theatre for rhythm issues | 34 (<0.1%) | 34 (<0.1%) | 0 (0%) | 0.3 |
| Pre-op Length of Stay (days) | 1.0 (1.0, 2.0) | 1.0 (1.0, 2.0) | 1.0 (1.0, 4.0) | <0.001 |
| Missing | 7038 | 6507 | 531 | |
| Post-op Length of Stay (days) | 6.0 (5.0, 9.0) | 6.0 (5.0, 8.0) | 7.0 (6.0, 11.0) | <0.001 |
| Missing | 5869 | 5379 | 490 | |
| Total Length of Stay(days) | 8 (7, 13) | 8 (7, 12) | 10 (7, 17) | <0.001 |
| Missing | 9566 | 8777 | 789 | |
| Characteristic | After Matching | ||
|---|---|---|---|
| At Least Single Arterial Graft, N = 19,906 1 | Veins Only, N = 19,906 1 | Standardised Mean Difference | |
| Age (years) | 53 (47, 58) | 53 (46, 59) | 0.023 |
| Gender | 6122 (31%) | 5966 (30%) | 0.017 |
| Pulmonary Disease | 3500 (18%) | 3374 (17%) | 0.016 |
| Peripheral Vascular Disease | 3800 (19%) | 3763 (19%) | 0.004 |
| Poor mobility pre-op | 693 (3.5%) | 657 (3.3%) | 0.010 |
| Creatinine > 200 μmol/L | 757 (3.8%) | 739 (3.7%) | 0.004 |
| Unstable angina | 6108 (31%) | 6021 (30%) | 0.009 |
| Moderate LV Function | 2433 (12%) | 2447 (12%) | 0.002 |
| Poor LV Function | 540 (2.7%) | 525 (2.6%) | 0.004 |
| Very poor LV Function | 187 (0.9%) | 187 (0.9%) | 0.000 |
| Diabetes on insulin | 1659 (8.3%) | 1659 (8.3%) | 0.000 |
| Redo | 1673 (8.4%) | 1698 (8.5%) | 0.004 |
| Critical Pre-operative State | 1417 (7.1%) | 1557 (7.8%) | 0.025 |
| Recent MI | 5947 (30%) | 6018 (30%) | 0.007 |
| Pulmonary Hypertension | 217 (1.1%) | 191 (1.0%) | 0.013 |
| Preoperative IABP | 415 (2.1%) | 437 (2.2%) | 0.007 |
| Urgent case | 8046 (40%) | 7821 (39%) | 0.023 |
| Emergency case | 1659 (8.3%) | 1697 (8.5%) | 0.006 |
| Salvage case | 150 (0.8%) | 251 (1.3%) | 0.037 |
| NYHA IV | 1405 (7.1%) | 1393 (7.0%) | 0.002 |
| CCS 4 | 27.3 (24.7, 30.2) | 27.3 (24.6, 30.3) | 0.008 |
| BMI | 27.3 (24.7, 30.2) | 27.3 (24.6, 30.3) | 0.004 |
| Mechanical Support | 421 (2.1%) | 443 (2.2%) | 0.004 |
| Pump Case | 18,524 (93%) | 18,516 (93%) | 0.001 |
| Conduit Strategy | |||
|---|---|---|---|
| Characteristic | At Least Single Arterial Graft, N = 19,906 1 | Veins Only, N = 19,906 1 | p-Value 2 |
| CPB Time(mins) 3 | 80 (61, 100) | 80 (61, 104) | <0.001 |
| Missing | 1261 | 1594 | |
| Cross Clamp Time(mins) 3 | 45 (33, 59) | 38 (27, 54) | <0.001 |
| Missing | 1314 | 1634 | |
| Mortality | <0.001 | ||
| 746 (3.8%) | 1054 (5.3%) | ||
| Missing | 127 | 96 | |
| CVA | 0.072 | ||
| 437 (2.4%) | 473 (2.6%) | ||
| Missing | 1512 | 1639 | |
| TIA | 0.5 | ||
| 890 (4.8%) | 911 (5.0%) | ||
| Missing | 1512 | 1639 | |
| Dialysis | 0.042 | ||
| 653 (3.8%) | 749 (4.3%) | ||
| Missing | 2544 | 2574 | |
| Intraoperative/postoperative IABP insertion | <0.001 | ||
| Used | 330 (5.5%) | 402 (8.4%) | |
| Missing | 13,905 | 15,104 | |
| Return to theatre for bleeding/tamponade | 0.2 | ||
| Yes | 733 (3.7%) | 779 (3.9%) | |
| Return to theatre for graft complications | 0.8 | ||
| Yes | 35 (0.2%) | 32 (0.2%) | |
| Return to theatre for rhythm issues | |||
| Yes | 4 (<0.1%) | 0 (0%) | |
| Pre-op Length of Stay (days) | 1.0 (1.0, 4.0) | 1.0 (1.0, 4.0) | 0.8 |
| Missing | 416 | 529 | |
| Post-op Length of Stay (days) | 7 (6, 10) | 7 (6, 11) | 0.002 |
| Missing | 336 | 488 | |
| Total Length of Stay(days) | 9 (7, 16) | 10 (7, 17) | <0.001 |
| Missing | 566 | 786 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Layton, G.R.; Sinha, S.; Caputo, M.; Angelini, G.D.; Fudulu, D.P.; Zakkar, M. Two Decades of CABG in the UK: A Propensity Matched Analysis of Outcomes by Conduit Choice. J. Clin. Med. 2024, 13, 4717. https://doi.org/10.3390/jcm13164717
Layton GR, Sinha S, Caputo M, Angelini GD, Fudulu DP, Zakkar M. Two Decades of CABG in the UK: A Propensity Matched Analysis of Outcomes by Conduit Choice. Journal of Clinical Medicine. 2024; 13(16):4717. https://doi.org/10.3390/jcm13164717
Chicago/Turabian StyleLayton, Georgia R., Shubhra Sinha, Massimo Caputo, Gianni D. Angelini, Daniel P. Fudulu, and Mustafa Zakkar. 2024. "Two Decades of CABG in the UK: A Propensity Matched Analysis of Outcomes by Conduit Choice" Journal of Clinical Medicine 13, no. 16: 4717. https://doi.org/10.3390/jcm13164717
APA StyleLayton, G. R., Sinha, S., Caputo, M., Angelini, G. D., Fudulu, D. P., & Zakkar, M. (2024). Two Decades of CABG in the UK: A Propensity Matched Analysis of Outcomes by Conduit Choice. Journal of Clinical Medicine, 13(16), 4717. https://doi.org/10.3390/jcm13164717







