Improved Proteinuria May Attenuate the Risk of Atrial Fibrillation: A Nationwide Population-Based Cohort Study
Abstract
1. Introduction
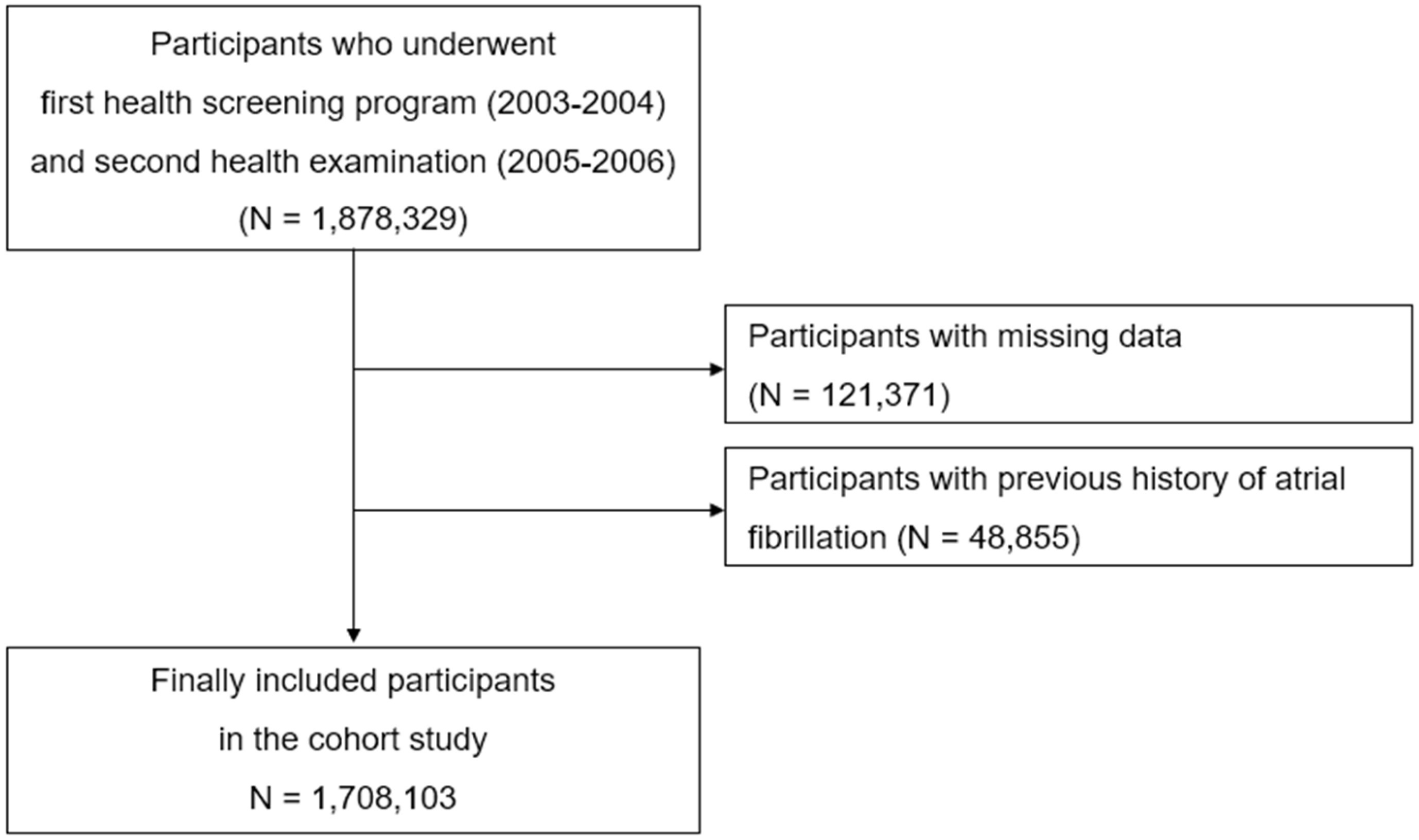
2. Materials and Methods
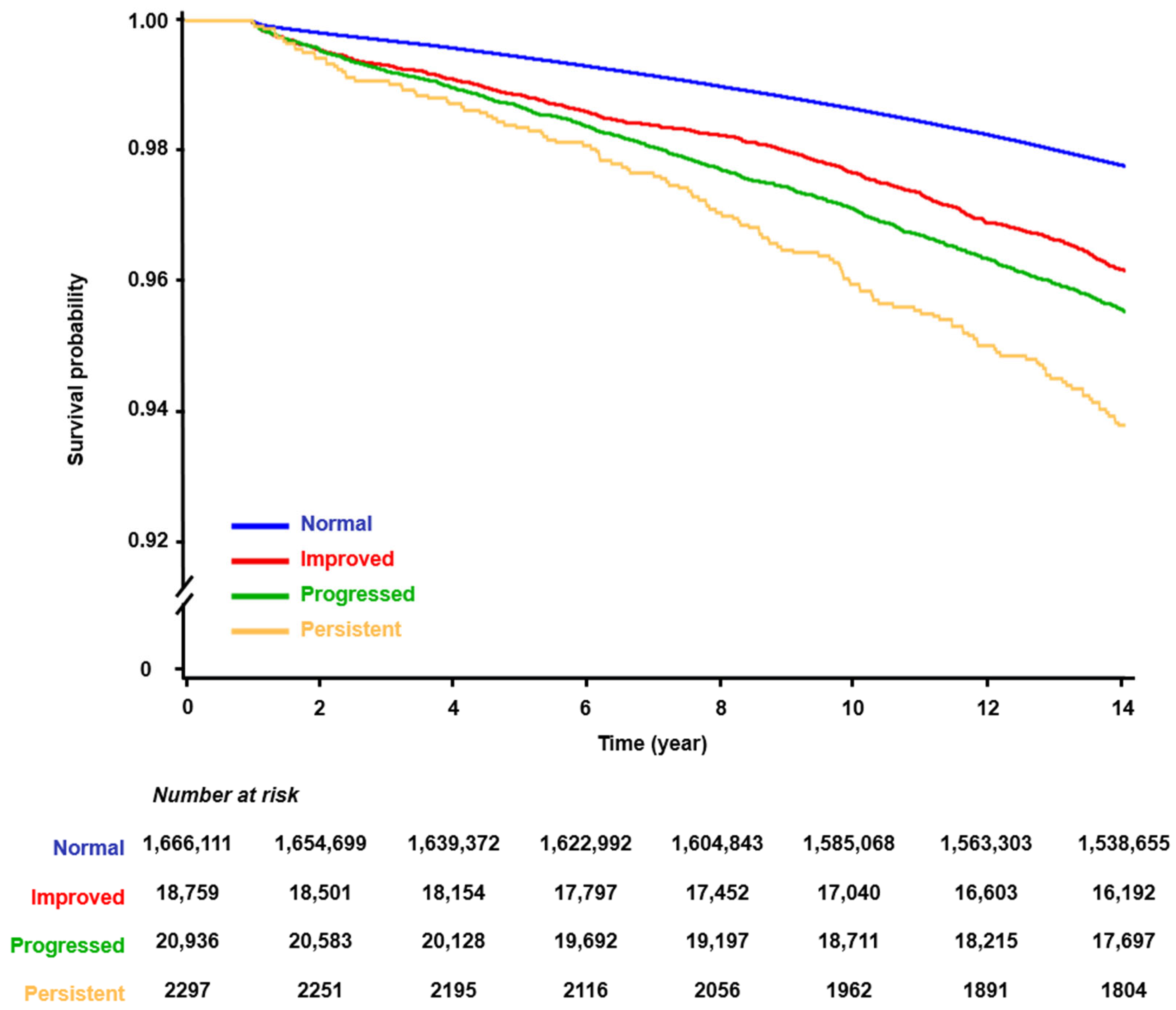
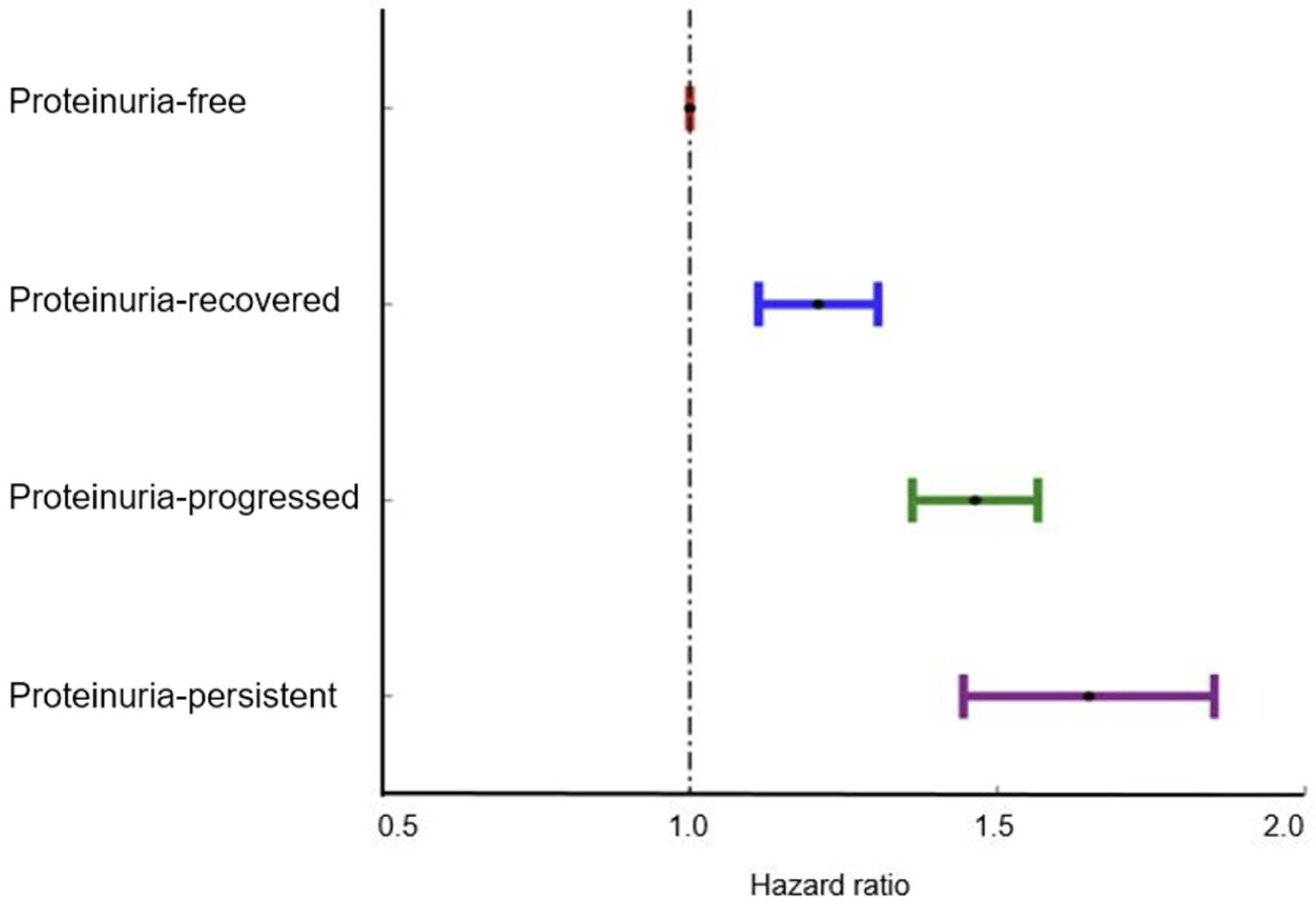
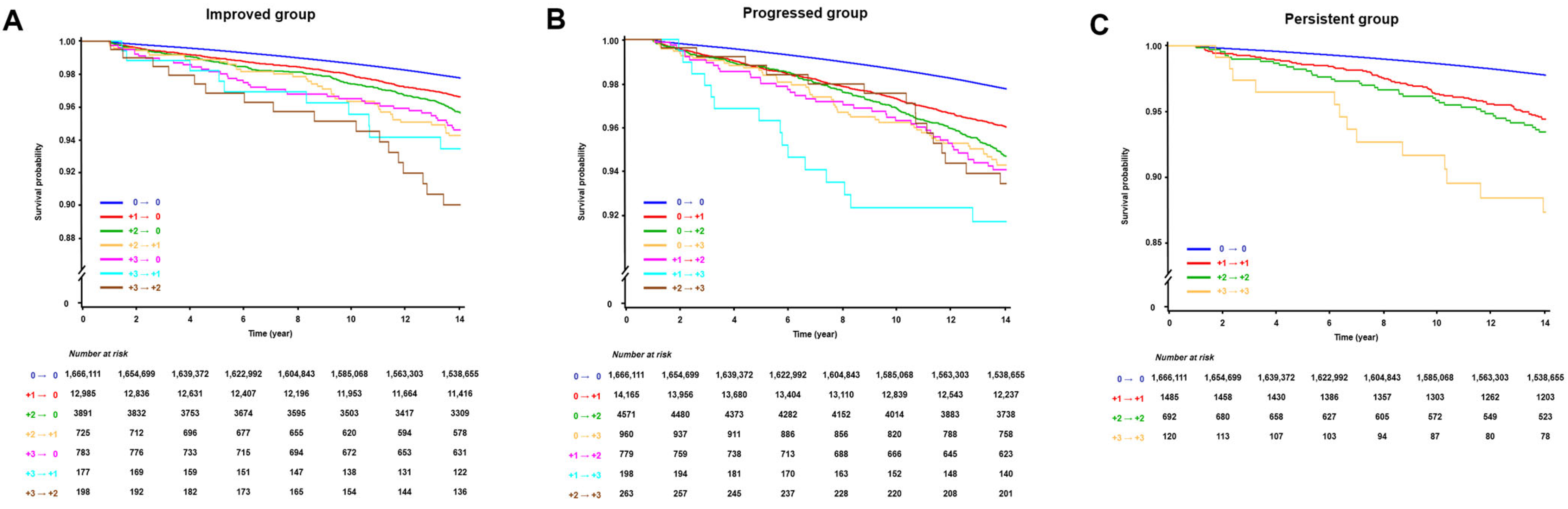
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kornej, J.; Börschel, C.S.; Benjamin, E.J.; Schnabel, R.B. Epidemiology of Atrial Fibrillation in the 21st Century: Novel Methods and New Insights. Circ. Res. 2020, 127, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Sanchis-Gomar, F.; Cervellin, G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int. J. Stroke 2021, 16, 217–221. [Google Scholar] [CrossRef]
- Meyre, P.; Blum, S.; Berger, S.; Aeschbacher, S.; Schoepfer, H.; Briel, M.; Osswald, S.; Conen, D. Risk of Hospital Admissions in Patients with Atrial Fibrillation: A Systematic Review and Meta-analysis. Can. J. Cardiol. 2019, 35, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.J.; Wolf, P.A.; Kelly-Hayes, M.; Beiser, A.S.; Kase, C.S.; Benjamin, E.J.; D’Agostino, R.B. Stroke severity in atrial fibrillation. The Framingham Study. Stroke 1996, 27, 1760–1764. [Google Scholar] [CrossRef] [PubMed]
- Brachmann, J.; Sohns, C.; Andresen, D.; Siebels, J.; Sehner, S.; Boersma, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Schunkert, H.; et al. Atrial Fibrillation Burden and Clinical Outcomes in Heart Failure: The CASTLE-AF Trial. JACC Clin. Electrophysiol. 2021, 7, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Tian, Y.; Wang, H.; Si, Q.; Wang, Y.; Lip, G.Y.H. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: New insights into the global burden of atrial fibrillation. Chest 2015, 147, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.J.; Lee, I.H.; Je, N.K. Inadequate stroke prevention in Korean atrial fibrillation patients in the post-warfarin era. Int. J. Cardiol. 2016, 220, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Elliott, A.D.; Middeldorp, M.E.; Van Gelder, I.C.; Albert, C.M.; Sanders, P. Epidemiology and modifiable risk factors for atrial fibrillation. Nat. Rev. Cardiol. 2023, 20, 404–417. [Google Scholar] [CrossRef] [PubMed]
- Culleton, B.F.; Larson, M.G.; Parfrey, P.S.; Kannel, W.B.; Levy, D. Proteinuria as a risk factor for cardiovascular disease and mortality in older people: A prospective study. Am. J. Med. 2000, 109, 1–8. [Google Scholar] [CrossRef]
- Kelly, D.M.; Rothwell, P.M. Proteinuria as an independent predictor of stroke: Systematic review and meta-analysis. Int. J. Stroke 2020, 15, 29–38. [Google Scholar] [CrossRef]
- Mok, Y.; Ballew, S.H.; Sang, Y.; Grams, M.E.; Coresh, J.; Evans, M.; Barany, P.; Ärnlöv, J.; Carrero, J.J.; Matsushita, K. Albuminuria as a Predictor of Cardiovascular Outcomes in Patients with Acute Myocardial Infarction. J. Am. Heart Assoc. 2019, 8, e010546. [Google Scholar] [CrossRef] [PubMed]
- Currie, G.; Delles, C. Proteinuria and its relation to cardiovascular disease. Int. J. Nephrol. Renovasc. Dis. 2013, 7, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Tada, H.; Hara, S.; Hayashi, K.; Patel, R.B.; Nishikawa, T.; Hashiba, A.; Takamura, M.; Greenland, P.; Kawashiri, M.A. Association of proteinuria with incident atrial fibrillation in the general Japanese population. J. Cardiol. 2021, 77, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.H.; Choi, E.K.; Han, K.D.; Rhee, T.M.; Lee, H.J.; Lee, S.R.; Kang, S.H.; Cha, M.J.; Oh, S. Proteinuria Detected by Urine Dipstick Test as a Risk Factor for Atrial Fibrillation: A Nationwide Population-Based Study. Sci. Rep. 2017, 7, 6324. [Google Scholar] [CrossRef] [PubMed]
- Song, S.O.; Jung, C.H.; Song, Y.D.; Park, C.Y.; Kwon, H.S.; Cha, B.S.; Park, J.Y.; Lee, K.U.; Ko, K.S.; Lee, B.W. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab. J. 2014, 38, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Seong, S.C.; Kim, Y.Y.; Park, S.K.; Khang, Y.H.; Kim, H.C.; Park, J.H.; Kang, H.J.; Do, C.H.; Song, J.S.; Lee, E.J.; et al. Cohort profile: The National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 2017, 7, e016640. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Woo, H.G.; Park, J.; Lee, J.S.; Song, T.J. Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: A nationwide population-based cohort study. Eur. J. Prev. Cardiol. 2020, 27, 1835–1845. [Google Scholar] [CrossRef] [PubMed]
- Song, T.J.; Kim, J.W.; Kim, J. Oral health and changes in lipid profile: A nationwide cohort study. J. Clin. Periodontol. 2020, 47, 1437–1445. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.G.; Chang, Y.; Lee, J.S.; Song, T.J. Association of Tooth Loss with New-Onset Parkinson’s Disease: A Nationwide Population-Based Cohort Study. Parkinson’s Dis. 2020, 2020, 4760512. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Woo, H.G.; Lee, J.S.; Song, T.J. Better oral hygiene is associated with lower risk of stroke. J. Periodontol. 2021, 92, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Lee, J.S.; Kim, J.; Lee, H.; Chang, Y.; Woo, H.G.; Kim, J.W.; Song, T.J. Oral health and gastrointestinal cancer: A nationwide cohort study. J. Clin. Periodontol. 2020, 47, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, H.J.; Jeon, J.; Song, T.J. Association between oral health and cardiovascular outcomes in patients with hypertension: A nationwide cohort study. J. Hypertens. 2022, 40, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.J.; Yang, P.S.; Yu, H.T.; Kim, T.H.; Jang, E.; Uhm, J.S.; Pak, H.N.; Lee, M.H.; Lip, G.Y.H.; Joung, B. Association of proteinuria and hypertension with incident atrial fibrillation in an elderly population: Nationwide data from a community-based elderly cohort. J. Hypertens. 2022, 40, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Yang, P.S.; Park, B.E.; Kang, T.S.; Lim, S.H.; Cho, S.; Lee, S.Y.; Lee, M.Y.; Lip, G.Y.H.; Kim, D.; et al. Association of proteinuria and incident atrial fibrillation in patients with diabetes mellitus: A population-based senior cohort study. Sci. Rep. 2021, 11, 17013. [Google Scholar] [CrossRef]
- Gami, A.S.; Hodge, D.O.; Herges, R.M.; Olson, E.J.; Nykodym, J.; Kara, T.; Somers, V.K. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J. Am. Coll. Cardiol. 2007, 49, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Voskoboinik, A.; Kalman, J.M.; De Silva, A.; Nicholls, T.; Costello, B.; Nanayakkara, S.; Prabhu, S.; Stub, D.; Azzopardi, S.; Vizi, D.; et al. Alcohol Abstinence in Drinkers with Atrial Fibrillation. N. Engl. J. Med. 2020, 382, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.; Zhao, W.; Ye, K.; Li, Y.; He, M.; Lu, B.; Hu, R. Albuminuria is associated with left ventricular hypertrophy in patients with early diabetic kidney disease. Int. J. Endocrinol. 2014, 2014, 351945. [Google Scholar] [CrossRef] [PubMed]
- Seko, Y.; Kato, T.; Haruna, T.; Izumi, T.; Miyamoto, S.; Nakane, E.; Inoko, M. Association between atrial fibrillation, atrial enlargement, and left ventricular geometric remodeling. Sci. Rep. 2018, 8, 6366. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Gadegbeku, C.; Lipkowitz, M.S.; Rostand, S.; Lewis, J.; Wright, J.T.; Appel, L.J.; Greene, T.; Gassman, J.; Astor, B.C. Kidney function can improve in patients with hypertensive CKD. J. Am. Soc. Nephrol. 2012, 23, 706–713. [Google Scholar] [CrossRef]
- Vriesendorp, R.; Donker, A.J.; de Zeeuw, D.; de Jong, P.E.; van der Hem, G.K.; Brentjens, J.R. Effects of nonsteroidal anti-inflammatory drugs on proteinuria. Am. J. Med. 1986, 81, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Donia, T.; Khamis, A. Management of oxidative stress and inflammation in cardiovascular diseases: Mechanisms and challenges. Environ. Sci. Pollut. Res. Int. 2021, 28, 34121–34153. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Lee, C.M.; Kwon, H.T.; Oh, S.-W. Relationship between Obesity and Smoking in Korean Men: Data Analyses from the Third and Fourth Korea National Health and Nutrition Examination Surveys (KNHANES). J. Korean Soc. Res. Nicotine Tob. 2010, 1, 115–123. [Google Scholar] [CrossRef]
- Tu, S.J.; Gallagher, C.; Elliott, A.D.; Linz, D.; Pitman, B.M.; Hendriks, J.M.; Lau, D.H.; Sanders, P.; Wong, C.X. Risk thresholds for total and beverage-specific alcohol consumption and incident atrial fibrillation. Clin. Electrophysiol. 2021, 7, 1561–1569. [Google Scholar] [CrossRef] [PubMed]
- Son, J.W.; Lee, S.; Kang, M.; Shin, Y.A.; Kim, J.H. Optimal Frequency Intensity of Physical Activity to Reduce the Risk of Hypertension in the Korean Population. Exerc. Sci. 2022, 31, 129–140. [Google Scholar] [CrossRef]
- Park, J.H.; Chang, Y.; Kim, J.W.; Song, T.J. Improved Oral Health Status Is Associated with a Lower Risk of Venous Thromboembolism: A Nationwide Cohort Study. J. Pers. Med. 2022, 13, 20. [Google Scholar] [CrossRef]
- Tent, H.; Waanders, F.; Krikken, J.A.; Lambers Heerspink, H.J.; Stevens, L.A.; Laverman, G.D.; Navis, G. Performance of MDRD study and CKD-EPI equations for long-term follow-up of nondiabetic patients with chronic kidney disease. Nephrol. Dial. Transplant. 2012, 27 (Suppl. S3), iii89–iii95. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H. Comorbidity Adjustment in Health Insurance Claim Database. Health Policy and Management. Health Policy Manag. 2016, 26, 71–78. [Google Scholar] [CrossRef]
| Variable | Total | Groups According to the Change in Proteinuria | ||||
|---|---|---|---|---|---|---|
| Proteinuria-Free | Proteinuria-Improved | Proteinuria-Progressed | Proteinuria-Persistent | p-Value | ||
| Number of participants (%) | 1,708,103 | 1,666,111 (97.54) | 18,759 (1.10) | 20,936 (1.23) | 2297 (0.13) | |
| Age, years | 44.0 ± 12.09 | 43.92 ± 12.06 | 47.01 ± 13.19 | 47.01 ± 13.05 | 49.43 ± 12.44 | <0.001 |
| Sex | <0.001 | |||||
| Male | 1,178,673 (69.00) | 1,150,995 (69.08) | 11,930 (63.6) | 13,943 (66.60) | 1816 (78.48) | |
| Female | 529,430 (31.00) | 515,116 (30.92) | 6829 (36.4) | 6993 (33.40) | 498 (21.52) | |
| Body mass index (kg/m2) | 23.63 ± 3.03 | 23.61 ± 3.02 | 24.18 ± 3.33 | 24.25 ± 3.45 | 24.89 ± 3.34 | <0.001 |
| Household income | <0.001 | |||||
| First quartile, lowest | 255,667 (14.97) | 248,768 (14.93) | 3261 (17.38) | 3342 (15.96) | 297 (12.83) | |
| Second quartile | 633,817 (37.11) | 619,240 (37.17) | 6613 (35.25) | 7288 (34.81) | 680 (29.39) | |
| Third quartile | 564,014 (33.02) | 550,552 (33.04) | 5891 (31.4) | 6763 (32.3) | 815 (35.22) | |
| Fourth quartile, highest | 254,605 (14.91) | 247,551 (14.86) | 2994 (15.96) | 3543 (16.92) | 522 (22.56) | |
| Smoking status | <0.001 | |||||
| Never | 984,134 (57.62) | 958,655 (57.54) | 11,620 (61.94) | 12,625 (60.3) | 1246 (53.85) | |
| Former | 212,855 (12.46) | 207,726 (12.47) | 2216 (11.81) | 2546 (12.16) | 370 (15.99) | |
| Current | 511,114 (29.92) | 499,730 (29.99) | 4923 (26.24) | 5765 (27.54) | 698 (30.16) | |
| Alcohol consumption (days/week) | <0.001 | |||||
| <3 | 1,143,895 (66.97) | 1,115,187 (66.93) | 12,972 (69.15) | 14,239 (68.01) | 1512 (65.34) | |
| ≥3 | 564,208 (33.03) | 550,924 (33.07) | 5787 (30.85) | 6697 (31.99) | 802 (34.66) | |
| Regular exercise (days/week) | <0.001 | |||||
| <3 | 1,377,901 (80.67) | 1,344,948 (80.72) | 14,564 (77.64) | 16,603 (79.3) | 1800 (77.79) | |
| ≥3 | 330,202 (19.33) | 321,163 (19.28) | 4195 (22.36) | 4333 (20.7) | 514 (22.21) | |
| Comorbidities | ||||||
| Hypertension | 773,343 (45.27) | 748,007 (44.9) | 11,062 (58.97) | 12,529 (59.84) | 1762 (76.15) | <0.001 |
| Diabetes mellitus | 241,826 (14.16) | 230,155 (13.81) | 4991 (26.61) | 5775 (27.58) | 915 (39.54) | <0.001 |
| Dyslipidemia | 423,808 (24.81) | 408,103 (24.49) | 6932 (36.95) | 7674 (36.65) | 1113 (48.1) | <0.001 |
| Cancer | 31,617 (1.85) | 30,441 (1.83) | 536 (2.86) | 556 (2.66) | 85 (3.67) | <0.001 |
| Renal disease | 17,424 (1.02) | 15,207 (0.91) | 1002 (5.34) | 934 (4.46) | 283 (12.23) | <0.001 |
| Charlson Comorbidity Index | ||||||
| 0 | 677,173 (39.64) | 663,858 (39.84) | 5941 (31.67) | 6762 (32.3) | 612 (26.45) | <0.001 |
| 1 | 692,943 (40.57) | 677,737 (40.68) | 6794 (36.22) | 7706 (36.81) | 710 (30.68) | <0.001 |
| ≥2 | 337,987 (19.79) | 324,516 (19.48) | 6024 (32.11) | 6468 (30.89) | 992 (42.87) | <0.001 |
| Number of Events | Event Rate (%) | Incidence Rate (Per 1000 Person Years) | Unadjusted | Multivariable Adjusted (1) | Multivariable Adjusted (2) | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | ||||
| Atrial Fibrillation | 40,654 | 2.38 | 1.68 | ||||||
| Proteinuria-Free: 0 → 0 | 38,857 | 2.33 | 1.64 | 1 (Ref) | 1 (Ref) | 1 (Ref) | |||
| Proteinuria-Improved | |||||||||
| +1 → 0 | 438 | 3.37 | 2.43 | 1.48 (1.35, 1.63) | <0.001 | 1.11 (1.01, 1.22) | 0.035 | 1.10 (1.00, 1.21) | 0.053 |
| +2 → 0 | 172 | 4.42 | 3.23 | 1.98 (1.70, 2.29) | <0.001 | 1.43 (1.23, 1.66) | <0.001 | 1.40 (1.21, 1.63) | <0.001 |
| +2 → +1 | 41 | 5.66 | 4.25 | 2.63 (1.93, 3.57) | <0.001 | 1.59 (1.17, 2.16) | 0.003 | 1.56 (1.15, 2.12) | 0.004 |
| +3~4 → 0 | 43 | 5.49 | 4.15 | 2.55 (1.89, 3.44) | <0.001 | 1.83 (1.36, 2.47) | <0.001 | 1.80 (1.33, 2.42) | <0.001 |
| +3~4 → +1 | 10 | 5.65 | 4.59 | 2.87 (1.54, 5.33) | 0.009 | 1.54 (1.03, 2.04) | 0.017 | 1.53 (1.02, 2.04) | 0.0191 |
| +3~4 → +2 | 18 | 9.09 | 7.34 | 4.59 (2.89, 7.29) | <0.001 | 2.53 (1.59, 4.02) | <0.001 | 2.48 (1.56, 3.93) | 0.001 |
| Proteinuria-Progressed | |||||||||
| 0 → +1 | 566 | 4 | 2.91 | 1.78 (1.63, 1.93) | <0.001 | 1.36 (1.26, 1.48) | <0.001 | 1.36 (1.25, 1.47) | <0.001 |
| 0 → +2 | 238 | 5.21 | 3.87 | 2.38 (2.09, 2.70) | <0.001 | 1.64 (1.44, 1.86) | <0.001 | 1.62 (1.43, 1.84) | <0.001 |
| 0 → +3~4 | 55 | 5.73 | 4.35 | 2.69 (2.06, 3.50) | <0.001 | 2.07 (1.59, 2.69) | <0.001 | 2.06 (1.58, 2.68) | <0.001 |
| +1 → +2 | 46 | 5.91 | 4.46 | 2.74 (2.06, 3.66) | <0.001 | 1.45 (1.09, 1.94) | 0.011 | 1.44 (1.08, 1.93) | 0.013 |
| +1 → +3~4 | 17 | 8.59 | 6.93 | 4.33 (2.69, 6.96) | <0.001 | 2.37 (1.48, 3.82) | 0.004 | 2.32 (1.44, 3.74) | 0.005 |
| +2 → +3~4 | 16 | 6.08 | 4.71 | 2.92 (1.79, 4.77) | <0.001 | 1.80 (1.10, 2.93) | 0.019 | 1.75 (1.07, 2.86) | 0.024 |
| Proteinuria-Persistent | |||||||||
| +1 → +1 | 81 | 5.45 | 4.05 | 2.49 (2.01, 3.1) | <0.001 | 1.45 (1.17, 1.8) | 0.008 | 1.43 (1.15, 1.78) | 0.001 |
| +2 → +2 | 43 | 6.21 | 4.78 | 2.96 (2.20, 3.99) | <0.001 | 1.65 (1.23, 2.23) | 0.001 | 1.64 (1.22, 2.22) | 0.001 |
| +3~4 → +3~4 | 13 | 10.83 | 9.18 | 5.79 (3.36, 9.96) | <0.001 | 3.53 (2.05, 6.08) | <0.001 | 3.47 (2.01, 5.97) | <0.001 |
| Status of Proteinuria | Multivariable Adjusted | |
|---|---|---|
| HR (95% CI) | p Value | |
| Improved vs. Free (reference) | 1.233 (1.142, 1.333) | <0.001 |
| Progressed vs. Free (reference) | 1.474 (1.383, 1.575) | <0.001 |
| Persistent vs. Free (reference) | 1.595 (1.345, 1.886) | <0.001 |
| Improved vs. Persistent (reference) | 0.804 (0.673, 0.974) | 0.019 |
| Progressed vs. Persistent (reference) | 0.947 (0.786, 1.126) | 0.466 |
| Improved vs. Progressed (reference) | 0.847 (0.767, 0.938) | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.; Kang, M.K.; Song, T.-J. Improved Proteinuria May Attenuate the Risk of Atrial Fibrillation: A Nationwide Population-Based Cohort Study. J. Clin. Med. 2024, 13, 4648. https://doi.org/10.3390/jcm13164648
Chang Y, Kang MK, Song T-J. Improved Proteinuria May Attenuate the Risk of Atrial Fibrillation: A Nationwide Population-Based Cohort Study. Journal of Clinical Medicine. 2024; 13(16):4648. https://doi.org/10.3390/jcm13164648
Chicago/Turabian StyleChang, Yoonkyung, Min Kyoung Kang, and Tae-Jin Song. 2024. "Improved Proteinuria May Attenuate the Risk of Atrial Fibrillation: A Nationwide Population-Based Cohort Study" Journal of Clinical Medicine 13, no. 16: 4648. https://doi.org/10.3390/jcm13164648
APA StyleChang, Y., Kang, M. K., & Song, T.-J. (2024). Improved Proteinuria May Attenuate the Risk of Atrial Fibrillation: A Nationwide Population-Based Cohort Study. Journal of Clinical Medicine, 13(16), 4648. https://doi.org/10.3390/jcm13164648







