Estrogen Hormones’ Implications on the Physiopathology of Temporomandibular Dysfunction
Abstract
1. Introduction
2. Materials and Methods
3. Results
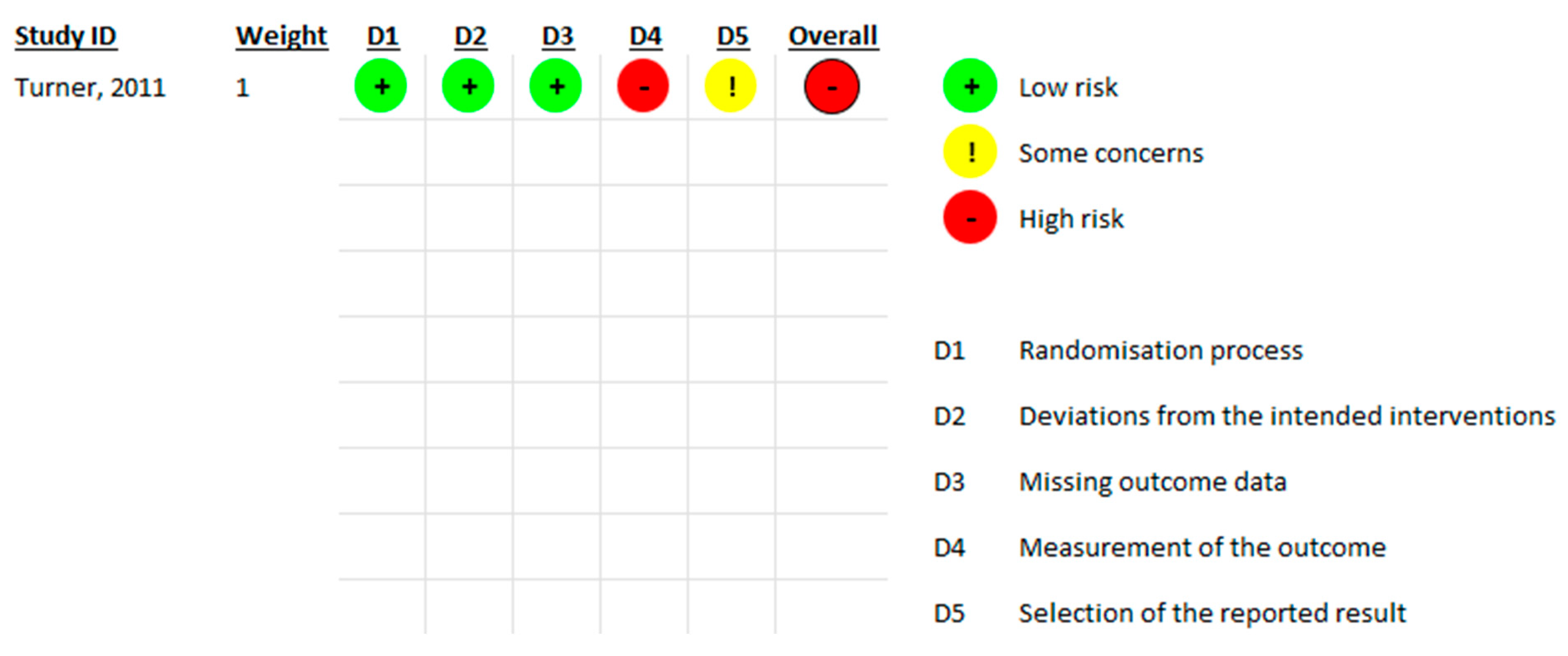
Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Berger, M.; Szalewski, L.; Bakalczuk, M.; Bakalczuk, G.; Bakalczuk, S.; Szkutnik, J. Association between estrogen levels and temporomandibular disorders: A systematic literature review. Prz. Menopauzalny 2015, 14, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Pardo, E.; Holland, C.A.; Cano, A. Sex Hormones and Healthy Psychological Aging in Women. Front. Aging Neurosci. 2018, 9, 439. [Google Scholar] [CrossRef] [PubMed]
- MacKendrick, N.A.; Troxel, H. Like a finely-oiled machine: Self-help and the elusive goal of hormone balance. Soc. Sci. Med. 2022, 309, 115242. [Google Scholar] [CrossRef]
- Cameron, J.L. Hormonal Mediation of Physiological and Behavioral Processes That Influence Fertility; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Okeson, J.P. Functional anatomy and biomechanics of the masticatory system. In Management of Temporomandibular Disorders and Occlusion, 8th ed.; Mosby: St. Louis, MO, USA, 2019. [Google Scholar]
- Dawson, P.E. The temporomandibular joint. In Functional Occlusion: From TMJ to Smile Design; Mosby: London, UK, 2007. [Google Scholar]
- Okeson, J.P. Etiology of functional disturbances in the masticatory system. In Management of Temporomandibular Disorders and Occlusion, 8th ed.; Mosby: St. Louis, MO, USA, 2019. [Google Scholar]
- Robinson, J.L.; Johnson, P.M.; Kister, K.; Yin, M.T.; Chen, J.; Wadhwa, S. Estrogen signaling impacts temporomandibular joint and periodontal disease pathology. Odontology 2020, 108, 153–165. [Google Scholar] [CrossRef]
- McDaniel, J.S.; Akula Suresh Babu, R.; Navarro, M.M.; LeBaron, R.G. Transcriptional regulation of proteoglycan 4 by 17beta-estradiol in immortalized baboon temporomandibular joint disc cells. Eur. J. Oral Sci. 2014, 122, 100–108. [Google Scholar] [CrossRef]
- Kapila, S.; Xie, Y. Targeted induction of collagenase and stromelysin by relaxin in unprimed and beta-estradiol-primed diarthrodial joint fibrocartilaginous cells but not in synoviocytes. Lab. Investig. 1998, 78, 925–938. [Google Scholar]
- Naqvi, T.; Duong, T.T.; Hashem, G.; Shiga, M.; Zhang, Q.; Kapila, S. Relaxin’s induction of metalloproteinases is associated with the loss of collagen and glycosaminoglycans in synovial joint fibrocartilaginous explants. Arthritis Res. Ther. 2005, 7, R1–R11. [Google Scholar] [CrossRef]
- Bi, R.Y.; Meng, Z.; Zhang, P.; Wang, X.D.; Ding, Y.; Gan, Y.H. Estradiol upregulates voltage-gated sodium channel 1.7 in trigeminal ganglion contributing to hyperalgesia of inflamed TMJ. PLoS ONE 2017, 12, e0178589. [Google Scholar] [CrossRef]
- Cheng, P.; Ma, X.; Xue, Y.; Li, S.; Zhang, Z. Effects of estradiol on proliferation and metabolism of rabbit mandibular condylar cartilage cells in vitro. Chin. Med. J. 2003, 116, 1413–1417. [Google Scholar] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Ribeiro-Dasilva, M.C.; Peres Line, S.R.; Leme Godoy dos Santos, M.C.; Arthuri, M.T.; Hou, W.; Fillingim, R.B.; Rizzatti Barbosa, C.M. Estrogen Receptor-α Polymorphisms and Predisposition to TMJ Disorder. J. Pain 2009, 10, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Stemig, M.; Myers, S.L.; Kaimal, S.; Islam, M.S. Estrogen receptor-alpha polymorphism in patients with and without degenerative disease of the temporomandibular joint. Cranio 2015, 33, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Dalewski, B.; Kamińska, A.; Białkowska, K.; Jakubowska, A.; Sobolewska, E. Association of estrogen receptor 1 and tumor necrosis factor α polymorphisms with temporomandibular joint anterior disc displacement without reduction. Dis. Markers 2020, 2020, 6351817. [Google Scholar] [CrossRef]
- Doetzer, A.D.; Almeida, L.E.; de Alcântara Camejo, F.; de Noronha, L.; Olandoski, M.; Trevilatto, P.C. Association of estrogen receptor alpha 1 and TMJ dysfunction: A pilot study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 131, e89–e94. [Google Scholar] [CrossRef] [PubMed]
- Roudgari, H.; Najafi, S.; Khalilian, S.; Ghafarzadeh, Z.; Hahakzadeh, A.; Behazin, S.; Sheykhbahaei, N. Association of Catechol-O-Methyl-Transferase and estrogen receptors polymorphism with severity of Temporomandibular Disorder in Iranian patients. Avicenna J. Med. Biotechnol. 2023, 15, 245. [Google Scholar] [CrossRef]
- Turner, J.A.; Mancl, L.; Huggins, K.H.; Sherman, J.J.; Lentz, G.; LeResche, L. Targeting temporomandibular disorder pain treatment to hormonal fluctuations: A randomized clinical trial. Pain 2011, 152, 2074–2084. [Google Scholar] [CrossRef]
- Madani, A.S.; Shamsian, A.A.; Hedayati-Moghaddam, M.R.; Fathimoghadam, F.; Sabooni, M.R.; Mirmortazavi, A.; Golmohamadi, M. A cross-sectional study of the relationship between serum sexual hormone levels and internal derangement of temporomandibular joint. J. Oral Rehabil. 2013, 40, 569–573. [Google Scholar] [CrossRef]
- Vilanova, L.S.; Gonçalves, T.M.; Meirelles, L.; Garcia, R.C. Hormonal fluctuations intensify temporomandibular disorder pain without impairing masticatory function. Int. J. Prosthodont. 2015, 28, 72–74. [Google Scholar] [CrossRef]
- Ribeiro-Dasilva, M.C.; Fillingim, R.B.; Wallet, S.M. Estrogen-Induced Monocytic Response Correlates with TMD Pain: A Case Control Study. J. Dent. Res. 2017, 96, 285–291. [Google Scholar] [CrossRef]
- Yuan, M.; Xie, Q.; Shen, P.; Yang, C. Do sex hormone imbalances contribute to idiopathic condylar resorption? Int. J. Oral Maxillofac. Surg. 2021, 50, 1244–1248. [Google Scholar] [CrossRef]
- Vignolo, V.; Vedolin, G.M.; de Araujo, C.; dos, R.P.; Rodrigues Conti, P.C. Influence of the menstrual cycle on the pressure pain threshold of masticatory muscles in patients with masticatory myofascial pain. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Soydan, S.S.; Deniz, K.; Uckan, S.; Dogruk Unal, A.; Bascıl Tutuncu, N. Is the incidence of temporomandibular disorder increased in polycystic ovary syndrome? Br. J. Oral Maxillofac. Surg. 2014, 52, 822–826. [Google Scholar] [CrossRef] [PubMed]
- Fichera, G.; Polizzi, A.; Scapellato, S.; Palazzo, G.; Indelicato, F. Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. J. Funct. Morphol. Kinesiol. 2020, 5, 36. [Google Scholar] [CrossRef] [PubMed]
- Yazici, H.; Islimye Taskin, M.; Guney, G.; Hismiogullari, A.A.; Arslan, E.; Tulaci, K.G. The novel relationship between polycystic ovary syndrome and temporomandibular joint disorders. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Jedynak, B.; Jaworska-Zaremba, M.; Grzechocińska, B.; Chmurska, M.; Janicka, J.; Kostrzewa-Janicka, J. TMD in Females with Menstrual Disorders. Int. J. Environ. Res. Public Health 2021, 18, 7263. [Google Scholar] [CrossRef]
- Nekora-Azak, A.; Evlioglu, G.; Ceyhan, A.; Keskin, H.; Berkman, S.; Issever, H. Estrogen Replacement Therapy Among Postmenopausal Women and Its Effects on Signs and Symptoms of Temporomandibular Disorders. CRANIO 2008, 26, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Chalkoo, A. Possible role of estrogen in temporomandibular disorders in female subjects: A research study. J. Indian Acad. Oral Med. Radiol. 2014, 26, 30. [Google Scholar] [CrossRef]
- Lora, V.R.M.M.; Canales, G.D.l.T.; Gonçalves, L.M.; Meloto, C.B.; Barbosa, C.M.R. Prevalence of temporomandibular disorders in postmenopausal women and relationship with pain and HRT. Braz. Oral Res. 2016, 30, e100. [Google Scholar] [CrossRef] [PubMed]
- Farzin, M.; Taghva, M.; Babooie, M. Comparison of temporomandibular disorders between menopausal and non-menopausal women. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 232. [Google Scholar] [CrossRef]
- Babouei, M.; Farzin, M.; Vejdani, M.; Moayedi, I. Evaluating the prevalence of temporomandibular joint abnormalities in postmenopausal women. Rev. Latinoam. Hipertens. 2019, 14, 518–524. [Google Scholar]
- Rosanto, Y.B.; Rahajoe, P.S. Effects of estradiol hormone in menopausal women on anterior disc displacement of temporomandibular joint. BIO Web Conf. 2020, 28, 02002. [Google Scholar] [CrossRef]
- Mursu, E.; Yu, J.; Karjalainen, E.; Savukoski, S.; Niinimäki, M.; Näpänkangas, R.; Pesonen, P.; Pirttiniemi, P.; Raustia, A. Association of climacterium with temporomandibular disorders at the age of 46 years—A cross-sectional study. Acta Odontol. Scand. 2022, 81, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Furquim, B.D.; Flamengui, L.M.S.P.; Repeke, C.E.P.; Cavalla, F.; Garlet, G.P.; Conti, P.C.R. Influence of TNF-α-308 G/A gene polymorphism on temporomandibular disorder. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Islander, U.; Erlandsson, M.C.; Hasséus, B.; Jonsson, C.A.; Ohlsson, C.; Gustafsson, J.-Å.; Dahlgren, U.; Carlsten, H. Influence of oestrogen receptor α and β on the immune system in aged female mice. Immunology 2003, 110, 149–157. [Google Scholar] [CrossRef]
- Puri, J.; Hutchins, B.; Bellinger, L.L.; Kramer, P.R. Estrogen and inflammation modulate estrogen receptor alpha expression in specific tissues of the temporomandibular joint. Reprod. Biol. Endocrinol. 2009, 7, 155. [Google Scholar] [CrossRef] [PubMed]
- Ren, K.; Wei, F.; Dubner, R.; Murphy, A.; Hoffman, G.E. Progesterone attenuates persistent inflammatory hyperalgesia in female rats: Involvement of spinal NMDA receptor mechanisms. Brain Res. 2000, 865, 272–277. [Google Scholar] [CrossRef] [PubMed]
- LeResche, L.; Mancl, L.; Sherman, J.J.; Gandara, B.; Dworkin, S.F. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain 2003, 106, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Vegeto, E.; Ghisletti, S.; Meda, C.; Etteri, S.; Belcredito, S.; Maggi, A. Regulation of the lipopolysaccharide signal transduction pathway by 17beta-estradiol in macrophage cells. J. Steroid Biochem. Mol. Biol. 2004, 91, 59–66. [Google Scholar] [CrossRef]
- Calippe, B.; Douin-Echinard, V.; Delpy, L.; Laffargue, M.; Lélu, K.; Krust, A.; Pipy, B.; Bayard, F.; Arnal, J.F.; Guéry, J.C.; et al. 17Beta-estradiol promotes TLR4-triggered proinflammatory mediator production through direct estrogen receptor alpha signaling in macrophages in vivo. J. Immunol. 2010, 185, 1169–1176. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Relevant topic studies | Studies published outside the 2008–2023 timeframe |
| Articles published within the last 15 years | |
| Articles published in English | Articles published in other languages |
| Full-text format | Review articles, systematic reviews |
| Studies involving human subjects | Studies involving animals |
| Database | Strategy | Results |
|---|---|---|
| PubMed | (“temporomandibular joint” OR “temporomandibular joint disease” OR “temporomandibular joint disk” OR “temporomandibular joint disorder” OR “temporomandibular joint syndrome” OR “TMJ syndrome” OR TMJ OR “Myofascial pain dysfunction syndrome” OR “TMJ disease” OR “TMJ disorder” OR “tmj disorder” OR tmj OR “tmj disease” OR “tmj syndrome” OR “muscle disorder” OR “temporomandibular articular disk” OR TMD OR “temporomandibular pain”) AND (estrogens OR “estrogen replacement therapy” OR “estrogenic hormones” OR “gonadal hormones” OR “sex hormones “ OR “polycystic ovary syndrome” OR “polycystic ovarian syndrome” OR “menstrual cycle” OR “menstruation disorder” OR “menstruation disturbance” OR postmenopause OR “hormonal oral contraceptive” OR “premenstrual syndrome” OR estradiol OR “estradiol levels” OR progesterone) | 368 |
| Scopus | TITLE-ABS-KEY (“TMD” OR “temporomandibular joint” OR “temporomandibular joint disorder”) AND (“estrogens”) | 260 |
| Embase | (‘tmd’ OR ‘temporomandibular joint’ OR ‘temporomandibular joint disorder’) AND (‘estrogens’ OR ‘gonadal hormones’ OR ‘sex hormones’ OR ‘menstrual disorders’ OR ‘postmenopause’ OR ‘oral contraceptive agent’) | 200 |
| Web of Science | (TS = (temporomandibular joint disorder) OR TS = (TMD) OR TS = (internal derangement)) AND (TS = (estrogens) OR TS = (gonadal hormones) OR TS = (sexual hormones) OR TS = (menstruation disorder) OR TS = (menstrual cycle)) | 202 |
| Reference | Year | Study Design and Subjects | Conclusion |
|---|---|---|---|
| Estrogen Receptor-α Polymorphisms and Predisposition to TMJ Disorder [15] | 2009 | Case–control 200 patients with TMD 100 healthy patients | The polymorphism of the estrogen receptor may play a role in the onset of temporomandibular disorders in women. |
| Estrogen receptor-alpha polymorphism in patients with and without degenerative disease of the temporomandibular joint [16] | 2015 | Case–control DNA samples from 42 patients with articular degenerative disease and 36 healthy patients | The presence of polymorphism in the estrogen receptor alpha gene could be involved in the degenerative effect on the joint bone within degenerative temporomandibular joint disease. |
| Association of Estrogen Receptor 1 and Tumor Necrosis Factor α Polymorphisms with Temporo-mandibular Joint Anterior Disc Displacement without Reduction [17] | 2020 | Case–control 124 patients with ADD (anterior disc displacement) 126 healthy patients | ESR1 could be involved in the pathogenesis of synovitis and degenerative pathology of temporomandibular joint cartilage and bone |
| Association of estrogen receptor alpha 1 and TMJ dysfunction: A pilot study [18] | 2021 | Pilot study 40 articular disc specimens from 27 patients suffering from ADDwRand ADDwoR (anterior disc displacement with and without reduction) | There is no association between the expression of the estrogen receptor alpha gene and age in patients with condylar fracture, ADDwR and ADDwoR |
| Association of Catechol-O-Methyl-Transferase and Estrogen Receptors polymorphism with Severity of Temporo-mandibular Disorder in Iranian Patients [19] | 2023 | Case–control Blood samples taken from 100 TMD patients and 103 healthy patients | The ESR1 and ESR2 genes are involved in the risk of developing temporomandibular disorders. The relationship between COMT and TMD was not statistically significant. |
| Reference | Year | Study Design and Subjects | Conclusion |
|---|---|---|---|
| Targeting Temporo-mandibular Disorder Pain Treatment to Hormonal Fluctuations: A Randomized Clinical Trial [20] | 2011 | Randomized clinical trial 147 female participants | Long-term benefits of self-applied therapeutic interventions for TMD pain by patients at the recommendation of the dental hygienist have been observed. |
| A cross-sectional study of the relationship between serum sexual hormone levels and internal derangement of temporomandibular joint [21] | 2013 | Cross-sectional 47 patients with ADDwR 95 patients without TMD | Low levels of serum progesterone could be associated with internal derangements of the temporomandibular joint. No difference was found for estrogen serum levels. |
| Hormonal Fluctuations Intensify Temporo-mandibular Disorder Pain Without Impairing Masticatory Function [22] | 2015 | Case–control 1 group (n = 25) evaluated for menstrual cycle and 1 group (n = 25) evaluated for OC (oral contraceptives) intake | The level of temporomandibular joint pain in women is influenced by hormonal fluctuations (lower pain level in ovulatory phase). The menstrual cycle does not interfere with masticatory function. |
| Estrogen-Induced Monocytic Response Correlates with Temporo-mandibular Disorder Pain: A Case Control Study [23] | 2017 | Case–control Blood samples taken from 18 patients (9 with TMD, and 9 controls) | Women with TMD had a systemic hyperinflammatory phenotype, as seen by increased monocytic cytokine release following an inflammatory insult, amplified by estrogen. Monocytes from participants who reported more pain on the VAS scale produced higher levels of IL6 than those from people who indicated lesser pain sensitivity. |
| Do sex hormone imbalances contribute to idiopathic condylar resorption? [24] | 2021 | Case–control 94 patients with ICR (idiopathic condylar resorption) 324 patients with DD (disc displacement) | There is no contribution of low estrogen levels in ICR in females, but higher testosterone and estrogen levels in men is related to ICR. |
| Influence of the menstrual cycle on the pressure pain threshold of masticatory muscles in patients with masticatory myofascial pain [25] | 2008 | Case–control 36 patients divided into 4 groups: 7 with TMD and no OC intake, 8 with TMD and OC intake, 13 healthy with no OC intake, 8 healthy with OC intake | The menstrual cycle phases do not have a significant impact on the masticatory muscle tenderness, but reported pain is slightly increased during the menstrual phase. The use of oral contraceptives is associated with an increased pain threshold to pressure. |
| Reference | Year | Study Design and Subjects | Conclusion |
|---|---|---|---|
| Is the incidence of temporo-mandibular disorder increased in polycystic ovary syndrome? [26] | 2014 | Case–control 100 premenopausal women divided into 1 group with PCOS (polycystic ovary syndrome) and 1 healthy group | The incidence and severity of TMD are higher in patients with polycystic ovary syndrome compared to asymptomatic patients. |
| Cranio-mandibular Disorders in Pregnant Women: An Epidemiological Survey [27] | 2020 | Case–control 108 pregnant women 90 control women | Pregnant women are more susceptible to TMD |
| The novel relationship between polycystic ovary syndrome and temporomandibular joint disorders [28] | 2020 | Case–control 45 PCOS patients 30 healthy patients | There is a significant relationship between PCOS and TMD. The PCOS group had lower mid-luteal progesterone and higher TNF-alpha, matrix metalloproteinase (MMP) 1, 8. No significant differences were found between PCOS with TMD and without TMD concerning estrogen, MMP 1, 8, TNF-alpha, IL-1b. |
| TMD in Females with Menstrual Disorders [29] | 2021 | Observational 65 women with menstrual disorders aged between 18 and 40 years and 61 matched by age and gender healthy controls | TMD was more frequent in females with menstrual disorders compared to the control group. |
| Reference | Year | Study Design and Subjects | Conclusion |
|---|---|---|---|
| Estrogen Replacement Therapy Among Postmenopausal Women and Its Effects on Signs and Symptoms of Temporomandibular Disorders [30] | 2008 | Case–control 91 postmenopausal women with HRT (hormonal replacement therapy) 89 women without HRT | There is no significant association between the use of hormone therapy in postmenopausal women and signs and symptoms of TMD. |
| Possible role of estrogen in temporomandibular disorders in female subjects: A research study [31] | 2014 | Case–control 195 patients divided into 2 groups: with TMD and without TMD, and further divided in pre and postmenopausal women. | There is a significant association between estrogen levels and TMD. |
| Prevalence of temporomandibular disorders in postmenopausal women and relationship with pain and HRT [32] | 2016 | Case–control 129 TMD patients 155 healthy patients | The use of hormone replacement therapy is not associated with TMD in postmenopausal women. The prevalence of TMD is increased during the reproductive age. |
| Comparison of temporomandibular disorders between menopausal and non-menopausal women [33] | 2018 | Case–control 69 premenopausal patients 71 postmenopausal patients | The prevalence of TMD was significantly higher in women in postmenopause compared to those before menopause. |
| Evaluating the prevalence of temporomandibular joint abnormalities in postmenopausal women [34] | 2019 | Case–control 69 premenopausal patients 71 postmenopausal patients | Postmenopausal women have a higher prevalence of TMD symptoms. |
| Effects of estradiol hormone in menopausal women on anterior disc displacement of temporomandibular joint [35] | 2020 | Case–control 40 postmenopausal women divided into 2 groups: healthy TMJ and ADD | Estradiol influences the incidence of anterior disc displacement, and the average levels of this hormone are higher in menopausal women with anterior disc displacement, but not statistically significant. |
| Association of climacterium with temporomandibular disorders at the age of 46 years—a cross-sectional study [36] | 2022 | Cross-sectional 71 climacteric patients 956 preclimacteric patients | The onset of climacteric phase in women is associated with the presence of TMD signs and symptoms. |
| Study | Is the Case Definition Adequate? | Representativeness of the Cases | Selection of Controls | Definition of Controls | Comparability of Cases and Controls on the Basis of the Design or Analysis | Ascertainment of Exposure | Same Method of Ascertainment for Cases and Controls | Non-Response Rate |
|---|---|---|---|---|---|---|---|---|
| Ribeiro-dasilva, 2009 [15] | * | - | * | * | * (age matched) | * | * | * |
| Stemig, 2015 [16] | * | - | * | * | - | * | * | * |
| Dalewski, 2020 [17] | * | - | - | * | - | * | * | * |
| Doetzer, 2020 [18] | * | - | * | * | - | * | * | * |
| Roudgari, 2023 [19] | * | - | - | * | - (gender matched) | * | * | * |
| Madani, 2013 [21] | * | * | * | * | - | * | * | * |
| Vilanova, 2015 [22] | * | - | * | * | - | */- | * | * |
| Ribeiro-Dasilva, 2017 [23] | * | - | - | * | - | * | * | * |
| Yuan, 2021 [24] | * | * | * | * | - | * | * | * |
| Vignolo, 2008 [25] | * | - | * | * | - | * | * | * |
| Soydan, 2014 [26] | * | - | - | * | - | * | * | * |
| Fichera, 2020 [27] | * | - | * | * | - | * | * | * |
| Yazici, 2020 [28] | * | - | * | * | - | * | * | * |
| Jedynak, 2021 [29] | * | - | - | * | * (age, gender matched) | * | * | * |
| Nekora-Azak, 2008 [30] | * | - | * | * | - | * | * | * |
| Ahmad, 2014 [31] | - | - | * | - | - | * | * | * |
| Lora, 2016 [32] | * | - | * | * | - | * | * | * |
| Farzin, 2018 [33] | - | - | * | - | - | * | * | * |
| Babouei, 2019 [34] | - | * | * | - | - | * | * | * |
| Murusu, 2022 [35] | * | * | * | * | * adjusted body mass index (BMI), smoking, parity, and interaction | * | * | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leucuța, D.-C.; Anton, D.; Almășan, O. Estrogen Hormones’ Implications on the Physiopathology of Temporomandibular Dysfunction. J. Clin. Med. 2024, 13, 4406. https://doi.org/10.3390/jcm13154406
Leucuța D-C, Anton D, Almășan O. Estrogen Hormones’ Implications on the Physiopathology of Temporomandibular Dysfunction. Journal of Clinical Medicine. 2024; 13(15):4406. https://doi.org/10.3390/jcm13154406
Chicago/Turabian StyleLeucuța, Daniel-Corneliu, Damaris Anton, and Oana Almășan. 2024. "Estrogen Hormones’ Implications on the Physiopathology of Temporomandibular Dysfunction" Journal of Clinical Medicine 13, no. 15: 4406. https://doi.org/10.3390/jcm13154406
APA StyleLeucuța, D.-C., Anton, D., & Almășan, O. (2024). Estrogen Hormones’ Implications on the Physiopathology of Temporomandibular Dysfunction. Journal of Clinical Medicine, 13(15), 4406. https://doi.org/10.3390/jcm13154406










