Primary Bladder Lymphoma with Extravesical Extension: A Case Report and Literature Review on Prognosis and Clinical Characteristics
Abstract
1. Introduction
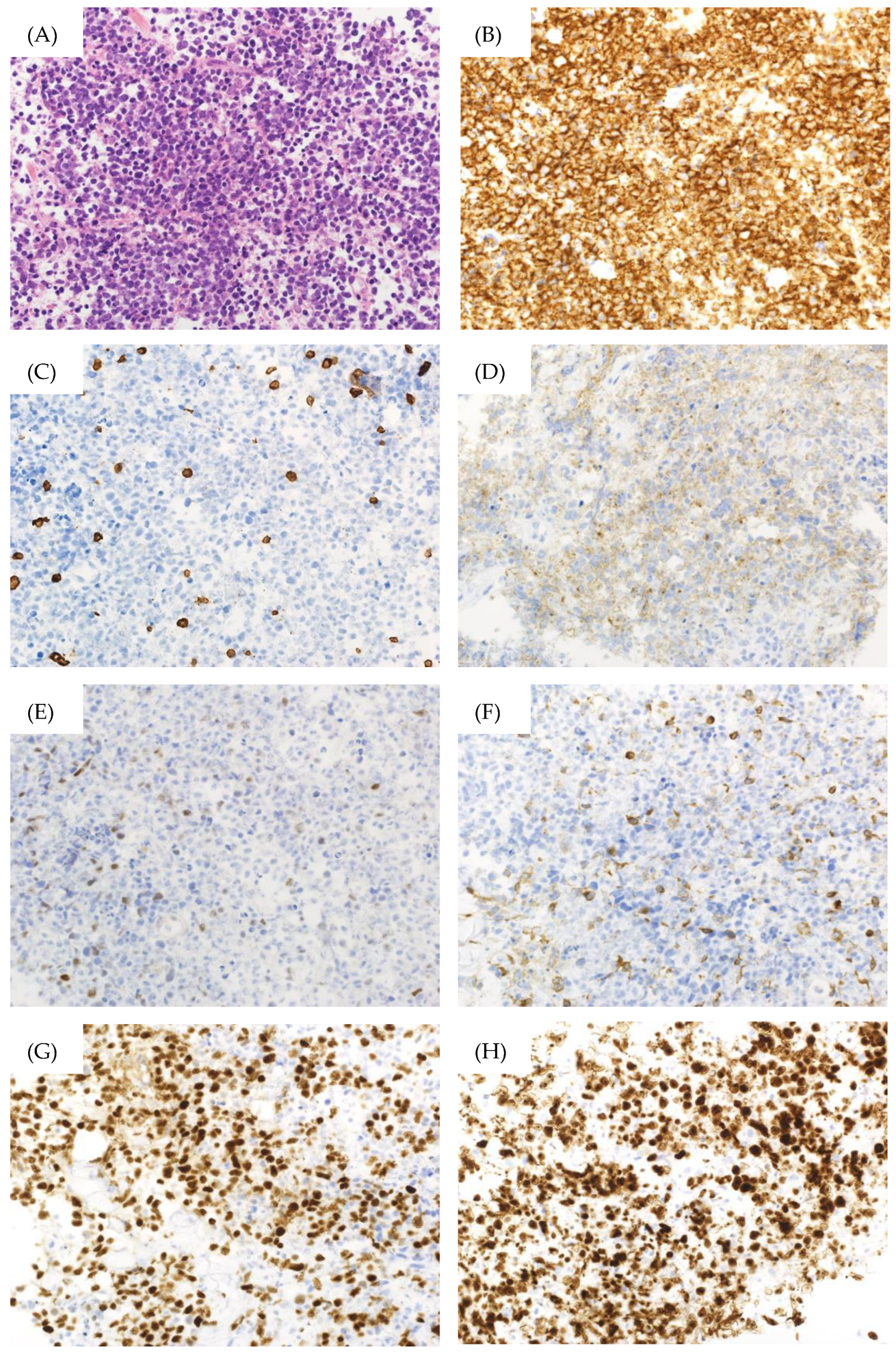
2. Case Presentation
3. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Campo, E.; Jaffe, E.S.; Cook, J.R.; Quintanilla-Martinez, L.; Swerdlow, S.H.; Anderson, K.C.; Brousset, P.; Cerroni, L.; de Leval, L.; Dirnhofer, S.; et al. The International Consensus Classification of Mature Lymphoid Neoplasms: A report from the Clinical Advisory Committee. Blood 2022, 140, 1229–1253, Erratum in Blood 2023, 141, 437–437. [Google Scholar] [CrossRef]
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; Araujo, I.B.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, S.H.; Campo, E.; Pileri, S.A.; Harris, N.L.; Stein, H.; Siebert, R.; Advani, R.; Ghielmini, M.; Salles, G.A.; Zelenetz, A.D.; et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016, 127, 2375–2390. [Google Scholar] [CrossRef] [PubMed]
- Al-Maghrabi, J.; Kamel-Reid, S.; Jewett, M.; Gospodarowicz, M.; Wells, W.; Banerjee, D. Primary low-grade B-cell lymphoma of mucosa-associated lymphoid tissue type arising in the urinary bladder: Report of 4 cases with molecular genetic analysis. Arch. Pathol. Lab. Med. 2001, 125, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Bates, A.W.; Norton, A.J.; Baithun, S.I. Malignant lymphoma of the urinary bladder: A clinicopathological study of 11 cases. J. Clin. Pathol. 2000, 53, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Kempton, C.L.; Kurtin, P.J.; Inwards, D.J.; Wollan, P.; Bostwick, D.G. Malignant lymphoma of the bladder: Evidence from 36 cases that low-grade lymphoma of the MALT-type is the most common primary bladder lymphoma. Am. J. Surg. Pathol. 1997, 21, 1324–1333. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Morrison, A.; Jackson, R. Primary bladder lymphoma: Management and outcome of 12 patients with a review of the literature. Leuk. Lymphoma 2005, 46, 873–877. [Google Scholar] [CrossRef] [PubMed]
- Armitage, J.O. Staging non-Hodgkin lymphoma. CA Cancer J. Clin. 2005, 55, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Mackman, N.; Falanga, A.; Pabinger, I.; Noble, S.; Ageno, W.; Moik, F.; Lee, A.Y.Y. Cancer-associated venous thromboembolism. Nat. Rev. Dis. Primers 2022, 8, 11. [Google Scholar] [CrossRef]
- Gervaso, L.; Dave, H.; Khorana, A.A. Venous and Arterial Thromboembolism in Patients With Cancer: JACC: CardioOncology State-of-the-Art Review. JACC CardioOncol. 2021, 3, 173–190. [Google Scholar] [CrossRef]
- Caruso, V.; Di Castelnuovo, A.; Meschengieser, S.; Lazzari, M.A.; de Gaetano, G.; Storti, S.; Iacoviello, L.; Donati, M.B. Thrombotic complications in adult patients with lymphoma: A meta-analysis of 29 independent cohorts including 18 018 patients and 1149 events. Blood 2010, 115, 5322–5328. [Google Scholar] [CrossRef] [PubMed]
- Arda, K.; Ozdemir, G.; Güneş, Z.; Ozdemir, H. Primary malignant lymphoma of the bladder. A case report and review of the literature. Int. Urol. Nephrol. 1997, 29, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Mourad, W.A.; Khalil, S.; Radwi, A.; Peracha, A.; Ezzat, A. Primary T-cell lymphoma of the urinary bladder. Am. J. Surg. Pathol. 1998, 22, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Tasu, J.P.; Geffroy, D.; Rocher, L.; Eschwege, P.; Strohl, D.; Benoit, G.; Paradis, V.; Bléry, M. Primary malignant lymphoma of the urinary bladder: Report of three cases and review of the literature. Eur. Radiol. 2000, 10, 1261–1264. [Google Scholar] [CrossRef] [PubMed]
- Sönmezer, M.; Ensari, A.; Ustün, Y.; Güngör, M.; Ortaç, F. Primary lymphoma of the urinary bladder presenting as a large pelvic mass. J. Pak. Med. Assoc. 2002, 52, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Jeong, Y.Y.; Shin, S.S.; Lim, H.S.; Kang, H.K. Primary calcified T-cell lymphoma of the urinary bladder: A case report. Korean J. Radiol. 2003, 4, 252–254. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oh, K.C.; Zang, D.Y. Primary non-Hodgkin’s lymphoma of the bladder with bone marrow involvement. Korean J. Intern. Med. 2003, 18, 40–44. [Google Scholar] [CrossRef]
- Leite, K.R.; Bruschini, H.; Camara-Lopes, L.H. Primary lymphoma of the bladder. Int. Braz. J. Urol. 2004, 30, 37–39. [Google Scholar] [CrossRef]
- Froehner, M.; Haase, M.; Hakenberg, O.W.; Wirth, M.P. Urinary immunocytology for primary bladder B cell lymphoma. Urology 2004, 63, 381–383. [Google Scholar] [CrossRef]
- Riccioni, R.; Carulli, G.; de Maria, M.; Pacini, S.; Cagno, C.; Selli, C.; Petrini, M. Primary lymphoma of the bladder: Case report. Am. J. Hematol. 2006, 81, 77–78. [Google Scholar] [CrossRef]
- Evans, D.A.; Moore, A.T. The first case of vesico-vaginal fistula in a patient with primary lymphoma of the bladder—A case report. J. Med. Case Rep. 2007, 1, 105. [Google Scholar] [CrossRef] [PubMed]
- Terzic, T.; Radojevic, S.; Cemerikic-Martinovic, V.; Stevanovic, R.; Citlucanin, S.; Mitrovic, D.; Stojimirovic, B.; Markovic-Lipkovski, J. Primary non-hodgkin lymphoma of urinary bladder with nine years later renal involvement and absence of systemic lymphoma: A case report. Med. Oncol. 2008, 25, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Horasanli, K.; Kadihasanoglu, M.; Aksakal, O.T.; Ozagari, A.; Miroglu, C. A case of primary lymphoma of the bladder managed with multimodal therapy. Nat. Clin. Pract. Urol. 2008, 5, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, A.; Miyakawa, Y.; Bokuda, K.; Kimura, T.; Nakashima, E.; Irie, R.; Sugiura, H.; Suzuki, T.; Ohsone, Y.; Akizuki, S. Primary Diffuse Large B-Cell Lymphoma of the Bladder. Intern. Med. 2009, 48, 1403–1406. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Peromingo, J.A.; Tato-Rodríguez, J.; Pesqueira-Fontán, P.M.; Molinos-Castro, S.; Gayol-Fernández, M.C.; Struzik, J.P. Non-Hodgkin’s lymphoma presenting as a primary bladder tumor: A case report. J. Med. Case Rep. 2010, 4, 114. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cao, Z.Z.; Qi, L. Primary T-cell lymphoma of the urinary bladder presenting with haematuria and hydroureteronephrosis. J. Int. Med. Res. 2011, 39, 2027–2032. [Google Scholar] [CrossRef] [PubMed]
- Nerli, R.B.; Guntaka, A.K.; Das, S.; Hiremath, M.B. Primary non-Hodgkin lymphoma of the bladder. Indian J. Cancer 2013, 50, 296. [Google Scholar] [CrossRef] [PubMed]
- Mahfoud, T.; Tanz, R.; Mesmoudi, M.; Khmamouche, M.R.; El Khannoussi, B.; Ichou, M.; Errihani, H. Primary non-Hodgkin’s lymphoma of the bladder: Case report and literature review. Pan. Afr. Med. J. 2013, 15, 136. [Google Scholar] [CrossRef]
- Simpson, W.G.; Lopez, A.; Babbar, P.; Payne, L.F. Primary bladder lymphoma, diffuse large B-cell type: Case report and literature review of 26 cases. Urol. Ann. 2015, 7, 268–272. [Google Scholar] [CrossRef]
- Ogihara, K.; Kosaka, T.; Kikuchi, E.; Hongo, H.; Mikami, S.; Oya, M. Spontaneous Regression of Epstein-Barr Virus-Positive Primary Diffuse Large Cell B-Cell Lymphoma of the Urinary Bladder After the Cessation of Enzalutamide. Clin. Genitourin. Cancer 2016, 14, e215–e218. [Google Scholar] [CrossRef]
- Bhutani, D.N.; Goel, D.V.; Kajal, D.P.; Pawar, D.D.; Sharma, D.P.; Sen, D.R. Primary extra nodal Non-Hodgkin’s lymphoma of urinary bladder presenting as a bladder tumor: A case report. Ann. Med. Surg. 2020, 56, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Sain, B.; Blake, M.; Goyal, K.; Kaur, H.; Robinson, K. Epstein–Barr virus-positive primary diffuse large B-cell lymphoma of the urinary bladder: A case report. J. Surg. Case Rep. 2023, 2023, rjad111. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Du, H.; Liu, J. Primary Bladder Non-Hodgkin Lymphoma: A Case Report. Cureus 2024, 16, e52688. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]


| Complete Blood Count | ||
| White blood cell | 4300/μL | 3300–8600/μL |
| Red blood cell | 2.62 × 106/μL | 4.35–5.55 × 106/μL |
| Hemoglobin | 8.9 g/dL | 13.7–16.8 g/dL |
| Hematocrit | 28.70% | 40.7–50.1% |
| Mean corpuscular volume | 109.5 fL | 83.6–98.2 fL |
| Mean corpuscular hemoglobin concentration | 31.0% | 31.7–35.3% |
| Platelet | 180 × 103/μL | 158–348 × 103/μL |
| Coagulation | ||
| Prothrombin time | 12.1 s | 10–13 s |
| Prothrombin time international ratio | 0.95 | 0.85–1.15 |
| Activated partial thromboplastin time | 34.0 s | 22.4–39.2 s |
| Fibrinogen | 145 mg/dL | 190–330 mg/dL |
| Seroimmunological test | ||
| C-reactive protein | 4.48 mg/dL | 0.00–0.14 mg/dL |
| Biochemistry | ||
| Total protein | 6.2 g/dL | 6.6–8.1 g/dL |
| Albumin | 2.8 g/dL | 4.1–5.1 g/dL |
| Total bilirubin | 0.54 mg/dL | 0.40–1.50 mg/dL |
| Urea nitrogen | 28.3 mg/dL | 8.0–20.0 mg/dL |
| Uric acid | 5.1 mg/dL | 3.7–7.0 mg/dL |
| Creatinine | 5.26 mg/dL | 0.65–1.07 mg/dL |
| Estimated glomerular filtration rate | 9 mL/min/1.732 | >90 mL/min/1.732 |
| Sodium | 138 mmol/L | 138–145 mmol/L |
| Potassium | 4.2 mmol/L | 3.6–4.8 mmol/L |
| Chloride | 102 mg/dL | 101–108 mmol/L |
| Aspartate aminotransferase | 41 U/L | 13–30 U/L |
| Alanine aminotransferase | 6 U/L | 10–42 U/L |
| Lactate dehydrogenase | 608 U/L | 124–222 U/L |
| γ-glutamyl transpeptidase | 12 U/L | 13–64 U/L |
| Creatinine kinase | 15 U/L | 59–248 U/L |
| Soluble interleukin-2 receptor | 14,617 U/mL | 122–496 U/mL |
| Age, median (range), years | 66 (27–89) |
| Female-to-male ratio | 2.2:1 |
| Initial presentation, N (%) | |
| Hematuria | 24 (52) |
| Anuria/Oliguria/Hydronephrosis | 9 (19) |
| Urinary tract infection | 4 (10) |
| Urinary urgency | 2 (4) |
| Low back/abdominal pain | 7 (15) |
| Histological type, N (%) | |
| DLBCL | 20 (43) |
| MALT/MZL | 17 (36) |
| Others | 10 (21) |
| Treatment strategy | |
| Chemotherapy | 30 (64) |
| Radiotherapy | 15 (31) |
| Others | 2 (4) |
| Treatment respondence | |
| >PD | 22 (73) |
| <SD or NA | 8 (17) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seki, H.; Mizuno, S.; Saigusa, S.; Sugita, Y.; Iida, Y.; Shinohara, S.; Uchino, K.; Horio, T.; Hanamura, I.; Takami, A. Primary Bladder Lymphoma with Extravesical Extension: A Case Report and Literature Review on Prognosis and Clinical Characteristics. J. Clin. Med. 2024, 13, 4340. https://doi.org/10.3390/jcm13154340
Seki H, Mizuno S, Saigusa S, Sugita Y, Iida Y, Shinohara S, Uchino K, Horio T, Hanamura I, Takami A. Primary Bladder Lymphoma with Extravesical Extension: A Case Report and Literature Review on Prognosis and Clinical Characteristics. Journal of Clinical Medicine. 2024; 13(15):4340. https://doi.org/10.3390/jcm13154340
Chicago/Turabian StyleSeki, Hideshige, Shohei Mizuno, Sakura Saigusa, Yukie Sugita, Yusuke Iida, Saki Shinohara, Kaori Uchino, Tomohiro Horio, Ichiro Hanamura, and Akiyoshi Takami. 2024. "Primary Bladder Lymphoma with Extravesical Extension: A Case Report and Literature Review on Prognosis and Clinical Characteristics" Journal of Clinical Medicine 13, no. 15: 4340. https://doi.org/10.3390/jcm13154340
APA StyleSeki, H., Mizuno, S., Saigusa, S., Sugita, Y., Iida, Y., Shinohara, S., Uchino, K., Horio, T., Hanamura, I., & Takami, A. (2024). Primary Bladder Lymphoma with Extravesical Extension: A Case Report and Literature Review on Prognosis and Clinical Characteristics. Journal of Clinical Medicine, 13(15), 4340. https://doi.org/10.3390/jcm13154340







