Dysmorphic Uterus: More Questions than Answers
Abstract
1. Introduction
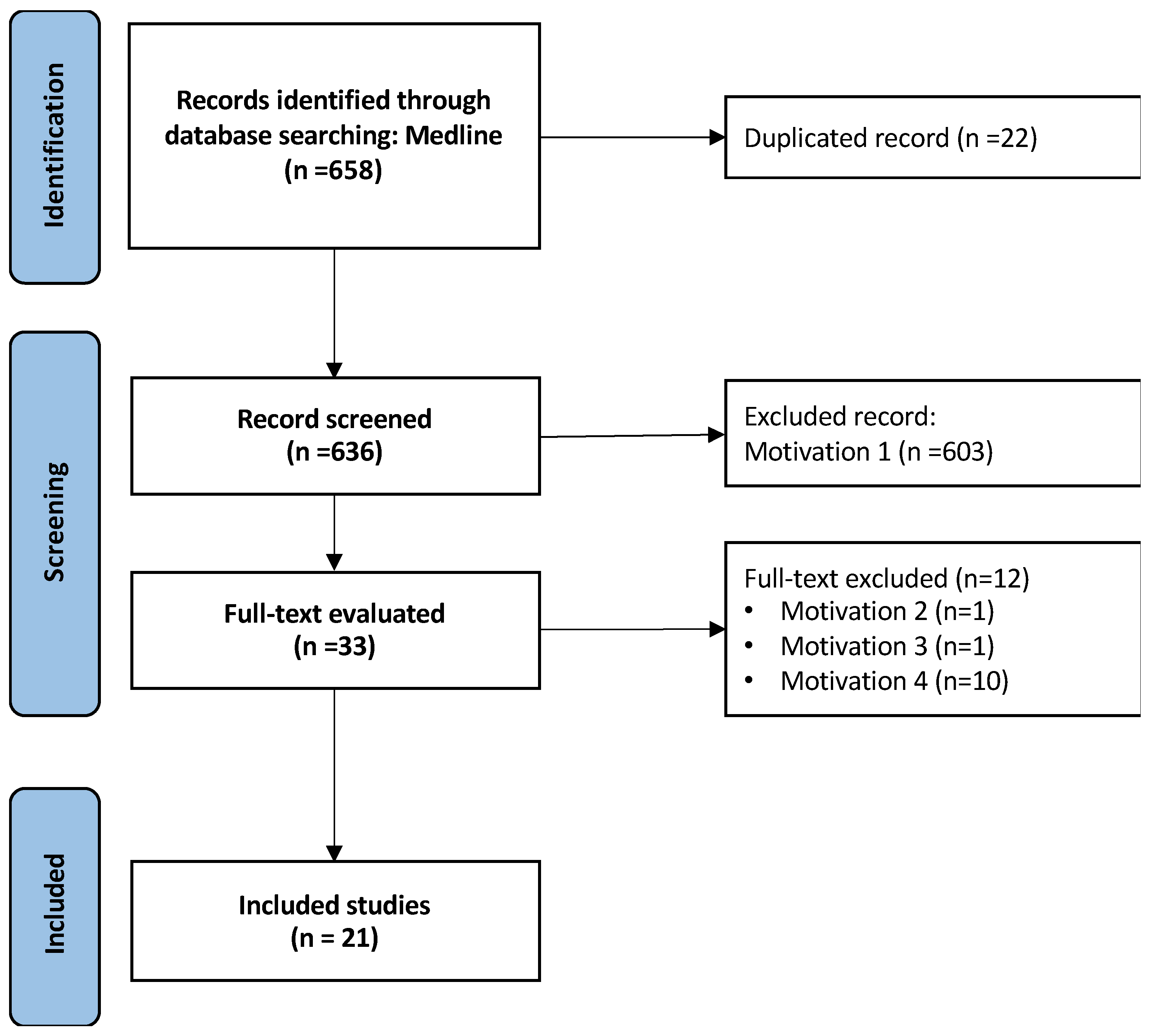
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Process and Data Collection
3. Results
3.1. Diagnostic Tools
3.2. Hysteroscopic Metroplasty and Reproductive Outcomes
4. Discussion
5. Conclusions
6. Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Alonso, L.; Haimovich, S.; Di Spiezio Sardo, A.; Carugno, J. Dysmorphic Uterus: Do We Need a T-Y-I Subclassification? J. Minim. Invasive Gynecol. 2020, 27, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, H.; Garbin, O.; Castaigne, V.; Gervaise, A.; Levaillant, J.-M. Surgical approach to and reproductive outcome after surgical correction of a T-shaped uterus. Hum. Reprod. 2011, 26, 1730–1734. [Google Scholar] [CrossRef] [PubMed]
- Ludwin, A.; Neto, M.A.C.; Ludwin, I.; Nastri, C.O.; Costa, W.; Acién, M.; Alcazar, J.L.; Benacerraf, B.; Condous, G.; DeCherney, A.; et al. Congenital Uterine Malformation by Experts (CUME): Diagnostic criteria for T-shaped uterus. Ultrasound Obstet. Gynecol. 2019, 55, 815–829. [Google Scholar] [CrossRef]
- Coelho Neto, M.A.; Ludwin, A.; Petraglia, F.; Martins, W.P. Definition, prevalence, clinical relevance and treatment of T-shaped uterus: Systematic review. Ultrasound Obstet. Gynecol. 2021, 57, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Seyhan, A.; Ertas, S.; Urman, B. Prevalence of T-shaped uterus among fertile women based on ESHRE/ESGE and Congenital Uterine Malformation by Experts (CUME) criteria. Reprod. Biomed. Online 2021, 43, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Antes, G.; Atkins, D.; PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Grimbizis, G.F.; Sardo, A.D.S.; Saravelos, S.H.; Gordts, S.; Exacoustos, C.; Van Schoubroeck, D.; Bermejo, C.; Amso, N.N.; Nargund, G.; Timmermann, D.; et al. The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. Gynecol. Surg. 2016, 13, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhu, Y.; Ge, B.; Sui, M.; Zheng, Z.; Sun, J. Reproductive outcome of hysteroscopic metroplasty for women with T-shaped uterus: A retrospective study. Reprod. Health 2022, 19, 78. [Google Scholar] [CrossRef] [PubMed]
- Acet, F.; Sahin, G.; Goker, E.N.T.; Tavmergen, E. Reproductive and ICSI outcomes after hysteroscopic metroplasty for T-shaped uterus, a prospective follow up study. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102450. [Google Scholar] [CrossRef]
- Bilgory, A.; Shalom-Paz, E.; Atzmon, Y.; Aslih, N.; Shibli, Y.; Estrada, D.; Haimovich, S. Diode Laser Hysteroscopic Metroplasty for Dysmorphic Uterus: A Pilot Study. Reprod. Sci. 2021, 29, 506–512. [Google Scholar] [CrossRef]
- Boza, A.; Akin, O.D.; Oguz, S.Y.; Misirlioglu, S.; Urman, B. Surgical correction of T-shaped uteri in women with reproductive failure: Long term anatomical and reproductive outcomes. J. Gynecol. Obstet. Hum. Reprod. 2018, 48, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Sardo, A.D.S.; Campo, R.; Zizolfi, B.; Santangelo, F.; Furst, R.M.; Di Cesare, C.; Bettocchi, S.; Vitagliano, A.; Ombelet, W. Long-Term Reproductive Outcomes after Hysteroscopic Treatment of Dysmorphic Uteri in Women with Reproductive Failure: An European Multicenter Study. J. Minim. Invasive Gynecol. 2020, 27, 755–762. [Google Scholar] [CrossRef]
- Sardo, A.D.S.; Florio, P.; Nazzaro, G.; Spinelli, M.; Paladini, D.; Di Carlo, C.; Nappi, C. Hysteroscopic outpatient metroplasty to expand dysmorphic uteri (HOME-DU technique): A pilot study. Reprod. Biomed. Online 2015, 30, 166–174. [Google Scholar] [CrossRef]
- Dilbaz, B.; Mert, S.A.; Diktas, E.G.; Kose, C.; Ustun, Y.E. The effect of hysteroscopic metroplasty on fertility in T-shaped and Y-shaped dysmorphic uterus. Eur. J. Contracept. Reprod. Health Care 2022, 27, 384–389. [Google Scholar] [CrossRef]
- Aslan, B.; Şükür, Y.E.; Özmen, B.; Sönmezer, M.; Berker, B.; Aytaç, R.; Atabekoğlu, C.S. Proposal for Diagnostic Criteria of Y-Shaped Dysmorphic Uterus Based on 3-Dimensional Transvaginal Ultrasound Measurements. J. Minim. Invasive Gynecol. 2024, 31, 504–510. [Google Scholar] [CrossRef]
- Ducellier-Azzola, G.; Lecointre, L.; Hummel, M.; Pontvianne, M.; Garbin, O. Hysteroscopic enlargement metroplasty for T-shaped uterus: 24 years’ experience at the Strasbourg Medico-Surgical and Obstetrical Centre (CMCO). Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 226, 30–34. [Google Scholar] [CrossRef]
- Haydardedeoğlu, B.; Durdağ, G.D.; Şimşek, S.; Aytaç, P.; Çok, T.; Kılıçdağ, E.B. Reproductive outcomes of office hysteroscopic metroplasty in women with unexplained infertility with dysmorphic uterus. J. Turk. Soc. Obstet. Gynecol. 2018, 15, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Ferro, J.; Labarta, E.; Sanz, C.; Montoya, P.; Remohi, J. Reproductive outcomes after hysteroscopic metroplasty for women with dysmorphic uterus and recurrent implantation failure. Facts Views Vis. ObGyn. 2018, 10, 63–68. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6516190/#:~:text=Conclusion,implantation%20failure%20and%20dysmorphic%20uterus. (accessed on 20 February 2019). [PubMed]
- Mutlu, A. IVF outcomes after T-shaped uterine metroplasty in patients with recurrent implantation failure. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102354. [Google Scholar] [CrossRef]
- Şükür, Y.E.; Yakıştıran, B.; Özmen, B.; Sönmezer, M.; Berker, B.; Atabekoğlu, C. Hysteroscopic Corrections for Complete Septate and T-Shaped Uteri Have Similar Surgical and Reproductive Outcome. Reprod. Sci. 2018, 25, 1649–1654. [Google Scholar] [CrossRef]
- Sánchez-Santiuste, M.; Ríos, M.; Calles, L.; de la Cuesta, R.; Engels, V.; Pereira, A.; Pérez-Medina, T. Dysmorphic Uteri: Obstetric Results after Hysteroscopic Office Metroplasty in Infertile and Recurrent Pregnancy Loss Patients. A Prospective Observational Study. J. Clin. Med. 2020, 9, 2857. [Google Scholar] [CrossRef]
- Buttram, V.C.; Gomel, V.; Siegler, A.; DeCherney, A.; Gibbons, W.; March, C. The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril. 1988, 49, 944. [Google Scholar]
- Grimbizis, G.F.; Gordts, S.; Sardo, A.D.S.; Brucker, S.; De Angelis, C.; Gergolet, M.; Li, T.-C.; Tanos, V.; Brölmann, H.; Gianaroli, L.; et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum. Reprod. 2013, 28, 2032–2044. [Google Scholar] [CrossRef] [PubMed]
- Küçük, T.; Ata, B. Infantile or hypoplastic uterus? A proposal for a modification to the ESHRE/ESGE classification of female genital tract congenital abnormalities. Facts Views Vis. ObGyn 2022, 14, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, L.A.; Laganà, A.S.; Ghezzi, F.; Haimovich, S.; Gómez, P.A.; Carugno, J. Subtypes of T-shaped uterus. Fertil Steril. 2019, 112, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Pleş, L.; Alexandrescu, C.; Ionescu, C.A.; Arvătescu, C.A.; Vladareanu, S.; Moga, M.A. Three-dimensional scan of the uterine cavity of infertile women before assisted reproductive technology use. Medicine 2018, 97, e12764. [Google Scholar] [CrossRef] [PubMed]
- Marianna, A.; Karine, T.; Armine, C.; Anna, K.; Hripsime, G. The impact of T-shaped uterine cavity anomaly on IVF outcomes: More questions than answers. J. Gynecol. Obstet. Hum. Reprod. 2021, 51, 102293. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xia, X.; Yan, J.; Yan, L.; Lu, C.; Zhu, X.; Wang, T.; Yin, T.; Li, R.; Chang, H.-M.; et al. Mesenchymal stem cell-derived angiogenin promotes primodial follicle survival and angiogenesis in transplanted human ovarian tissue. Reprod. Biol. Endocrinol. 2017, 15, 18. [Google Scholar] [CrossRef] [PubMed]
- Grigore, M.; Popovici, R.; Himiniuc, L.M.; Scripcariu, I.S.; Toma, B.F.; Grigore, A.M.; Micu, R. The added value of three-dimensional ultrasonography in uterine pathology. Exp. Ther. Med. 2021, 22, 1261. [Google Scholar] [CrossRef]
- Salim, R.; Riris, S.; Saab, W.; Abramov, B.; Khadum, I.; Serhal, P. Adenomyosis reduces pregnancy rates in infertile women undergoing IVF. Reprod. Biomed. Online 2012, 25, 273–277. [Google Scholar] [CrossRef]
- Kougioumtsidou, A.; Mikos, T.; Grimbizis, G.F.; Karavida, A.; Theodoridis, T.D.; Sotiriadis, A.; Tarlatzis, B.C.; Athanasiadis, A.P. Three-dimensional ultrasound in the diagnosis and the classification of congenital uterine anomalies using the ESHRE/ESGE classification: A diagnostic accuracy study. Arch. Gynecol. Obstet. 2019, 299, 779–789. [Google Scholar] [CrossRef]
- Bermejo, C.; Ten, P.M.; Cantarero, R.; Diaz, D.; Pedregosa, J.P.; Barrón, E.; Labrador, E.; López, L.R. Three-dimensional ultrasound in the diagnosis of Müllerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet. Gynecol. 2010, 35, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Garzon, S.; Laganà, A.S.; Sardo, A.D.S.; Pacheco, L.A.; Haimovich, S.; Carugno, J.; Vitale, S.G.; Casarin, J.; Raffaelli, R.; Andrisani, A.; et al. Hysteroscopic Metroplasty for T-Shaped Uterus: A Systematic Review and Meta-analysis of Reproductive Outcomes. Obstet. Gynecol. Surv. 2020, 75, 431–444. [Google Scholar] [CrossRef]
- Neal, S.A.; Morin, S.J.; Werner, M.D.; Gueye, N.-A.; Pirtea, P.; Scott, R.T.; Goodman, L.R. Three-dimensional ultrasound diagnosis of T-shaped uterus is associated with adverse pregnancy outcomes after embryo transfer. Reprod. Biomed. Online 2019, 39, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Neal, S.; Morin, S.; Werner, M.; Gueye, N.; Pirtea, P.; Patounakis, G.; Scott, R.; Goodman, L. Three-dimensional ultrasound diagnosis of adenomyosis is not associated with adverse pregnancy outcome following single thawed euploid blastocyst transfer: Prospective cohort study. Ultrasound Obstet. Gynecol. 2020, 56, 611–617. [Google Scholar] [CrossRef]
- Menge, T.; Zhao, Y.; Zhao, J.; Wataha, K.; Gerber, M.; Zhang, J.; Letourneau, P.; Redell, J.; Shen, L.; Wang, J.; et al. Mesenchymal Stem Cells Regulate Blood-Brain Barrier Integrity Through TIMP3 Release After Traumatic Brain Injury. Sci. Transl. Med. 2012, 4, 161ra150. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, L.A.; López, C.B.; Carugno, J.; Gómez, P.A.; Martinez-Ten, P.; Laganà, A.S.; Garzon, S. The Rule of 10: A simple 3D ultrasonographic method for the diagnosis of T-shaped uterus. Arch. Gynecol. Obstet. 2021, 304, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Pellicer, A.; Galliano, D. Hysteroscopy before IVF: Can it improve outcomes? Lancet 2016, 387, 2578–2579. [Google Scholar] [CrossRef]
- Galliano, D.; Bellver, J.; Díaz-García, C.; Simón, C.; Pellicer, A. Art and uterine pathology: How relevant is the maternal side for implantation? Hum. Reprod. Update 2015, 21, 13–38. [Google Scholar] [CrossRef]
| Current Classifications | T-Shaped | Borderline T-Shaped | Y-Shaped |
|---|---|---|---|
| ASRM, 1988 | Class VII-DES * related. Letter T based on hysterosalpingography imaging | NA * | NA |
| CUME, 2020 | All of three:
| At least two of three | NA |
| ESHRE/ESGE, 2013 | Class U1a narrow uterine cavity due to thickened lateral walls with a correlation 2/3 uterine corpus and 1/3 cervix. | NA | NA |
| ESHRE/ESGE modified, 2022 | Class U1a narrow uterine cavity due to thickened lateral walls with a correlation 2/3 uterine corpus and 1/3 cervix. | NA | U1b narrow uterine cavity due to thickened lateral walls and a fundal indentation of <50% of the uterine wall thickness at the midline level, with a correlation 2/3 uterine corpus and 1/3 cervix |
| Pacheco, 2021- Rule of 10 | R10 ≤ 10 mm | NA | NA |
| Aslan, 2024 | All of three:
| NA | All of three:
|
| Study | Population Groups | Study Design | N | Diagnosis | Metroplasty | PR * | SPR * | IVF PR * | LBR * | MR * | PD * | Ectopic Pregnancy | Placentation Problems | Complications | CS * |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acet et al., 2022 [9] | prospective | 182 | HSG + HSC * | Monopolar and bipolar hook needle | NR * | NR | NR | NR | none | NR | |||||
| Primary infertility | 74 | 32% (24/74) | 51% (28/55) | 54% (40/74) | NR | NR | NR | NR | none | NR | |||||
| Reccurent miscarriage | 60 | 37% (22/60) | 71% (30/42) | 76% (46/60) | NR | NR | NR | NR | none | NR | |||||
| Repeated implantation failure | 48 | 0 | 40% (19/48) | 40% (19/48) | NR | NR | NR | NR | none | NR | |||||
| Bilgory et al., 2021 [10] | retrospective | 15 | 3D TVS * | Diode laser | 60% (9/15) | NR | 60% (9/15) | 78% (7/9) | 22% (2/9) | 29% (2/7) | 0 | 1 placenta previa | none | 67% (4/6) | |
| Boza et al., 2018 [11] | prospective | 56 | HSG+ 3D-TVS | Bipolar hook needle | 66% (37/56) | 30% (17/56) | 36% (20/56) | 52% (29/56) | 22% (8/37) | 10% (3/29) | 0 | 0 | none | NR | |
| Primary infertility | 32 | 63% (20/32) | 28% (9/32) | 34% (11/32) | 53% (17/32) | 9% (3/32) | NR | NR | NR | NR | |||||
| Reccurent miscarriage | 10 | 80% (8/10) | 40% (4/10) | 40% (4/10) | 60% (6/10) | 20% (2/10) | NR | NR | NR | NR | |||||
| Repeated implantation failure | 14 | 64% (9/14) | 28% (4/14) | 36% (5/14) | 43% (6/14) | 21% (3/14) | NR | NR | NR | NR | |||||
| Di Spiezio Sardo et al., 2020 [12] | retrospective multicenter | 214 | 3D-TVS +HSC | Bipolar electrode or scissors | 73% (156/214) | 47% (74/156) | 53% (82/156) | 80% (125/156) | 19% (31/156) | 14% (17/125) | 0 | 6% (8/125) | none | 54% (68/125) | |
| Primary infertility | 166 | 72% (119/166) | 45% (53/119) | 55% (66/119) | 81% (96/119) | 19% (23/119) | 10% (9/96) | 0 | none | 55% (52/96) | |||||
| Reccurent miscarriage | 48 | 77% (37/48) | 57% (21/37) | 43% (16/37) | 78% (29/37) | 22% (8/37) | 28% (8/29) | 0 | none | 55% (16/29) | |||||
| Di Spiezio, 2015 [13] | prospective | 30 | 3D-TVS +HSC | HOME-DU technique | 57% (17/30) | 71% (12/17) | 35% (6/17) | 58% (7/12) | |||||||
| Primary infertility | 22 | 55% (12/2) | 75% (9/12) | 25% (3/12) | 25% (3/12) | NR | NR | none | |||||||
| Recurrent miscarriage | 9 | 71% (5/7) | 60% (3/5) | 40% (2/5) | 60% (3/5) | NR | NR | none | |||||||
| Preterm birth | 1 | 0% (0/1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Dilbaz et al., 2022 [14] | retrospective | 92 | 3D-TVS +HSC | Monopolar hook needle | 54% (50/92) | 56% (28/50) | 44% (22/50) | 76% (38/50) | 16% (8/50) | 18% (9/50) | 8% (4/50) | 0 | none | NR | |
| T-shaped | 30 | 37% (11/30) | 37% (11/30) | 36% (8/22) | 53% (16/30) | 10% (3/30) | 13% (2/30) | 0% | 0 | none | NR | ||||
| Y-shaped | 62 | 50% (31/62) | 55% (17/62) | 64% (14/22) | 36% (22/62) | 8% (5/62) | 32% (7/62) | 7% (4/62) | 0 | none | NR | ||||
| Ducellier-Azzola et al., 2018 [16] | retrospective | 112 | HSG or 3D TVS or HSC | Monopolar and bipolar hook needle | 62% (100/161) | 49% (24/49) | 49% (24/49) | 60% (60/100) | 22% (22/100) | 20% (12/60) | NR | NR | 2% (2/112) | NR | |
| Haydardedeoğlu et al., 2018 [17] | retrospective | 272 | |||||||||||||
| Primary infertility | 162 | 46% (74/162) | 19% (30/162) | 20% (33/162) | 14% (10/74) | 3% (2/74) | 1% (1/74) | ||||||||
| Secindary infertility | 110 | 55% (61/110) | 34% (37/110) | 22% (24/110) | 10% (6/61) | 0 | 2% (1/61) | ||||||||
| J. Ferro [18] | RIF ≥ 5 preembryos transferred | retrospective | 190 | HSC | Scissors and bipolar hook needle | 80% (152/190) | 3% (6/190) | 77% (146/190) | 77% (147/190) | 11% (17/190) | 22% (34/152) | none | 57% (86) | ||
| Mutlu, 2022 [19] | RIF ≥ 3 preembryos transferred | retrospective | 90 | HSG | Monopolar hook needle | 5% (4/85) | 0 | none | 88% (15/17) | ||||||
| T-shaped and metroplasty | 48 | 42% (18/43) | 10% (5/48) | 30% (13/43) | 12% (5/43) | ||||||||||
| T-shaped without metroplasty | 42 | 17% (7/42) | 7% (3/42) | ||||||||||||
| Şükür, et al., 2018 [20] | Infertility | retrospective | 97 | HSG or MRI | Monopolar needle electrode | ||||||||||
| T-shaped (U1a) | 43 | 37% (16/43) | 76% (13/16) | 18% (3/43) | 12% (2/43) | 3% | |||||||||
| Septate uetrus (U2b) | 54 | 35% (19/54) | 84% (16/19) | 21% (4/54) | 11% (2/54) | 0% | |||||||||
| Sánchez-Santiuste, 2020 [21] | prospective | 63 | HSC | HOME-DU technique | 76% (48/63) | 36% (13/36) | 33% (12/36) | 64% (36/63) | 8% (5/63) | 28% (5/18) | NR | 21% (3/36) | none | 39% (14/36) | |
| Infertility | 30 | 67% (20/30) | 33% (6/18) | 22% (4/18) | 62% (18/29) | 3% (1/30) | 11% (2/18) | NR | NR | none | 33% (6/18) | ||||
| Recurrent miscarriage | 33 | 85% (28/33) | 39% (7/18) | 44% (8/18) | 67% (18/27) | 12% (4/33) | 17% (3/18) | NR | NR | none | 44% (8/18) | ||||
| Zhang et al., 2022 [8] | retrospective | 111 | HSC | Microscissors | none | ||||||||||
| Congenital T-shaped uterus | 46 | 87% (40/46) | 33% (15/45) | 67% (30/45) | 78% (35/44) | 20% (9/44) | NR | NR | NR | none | 63% (22/35) | ||||
| Acquired T-shaped uterus | 65 | 72% (47/65) | 56% (29/52) | 44% (23/52) | 67% (35/47) | 23% (12/47) | NR | NR | NR | none | 60% (21/35) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Selntigia, A.; Pellegrini, L.; Gebbia, F.; Galliano, D. Dysmorphic Uterus: More Questions than Answers. J. Clin. Med. 2024, 13, 4333. https://doi.org/10.3390/jcm13154333
Selntigia A, Pellegrini L, Gebbia F, Galliano D. Dysmorphic Uterus: More Questions than Answers. Journal of Clinical Medicine. 2024; 13(15):4333. https://doi.org/10.3390/jcm13154333
Chicago/Turabian StyleSelntigia, Aikaterini, Livia Pellegrini, Francesco Gebbia, and Daniela Galliano. 2024. "Dysmorphic Uterus: More Questions than Answers" Journal of Clinical Medicine 13, no. 15: 4333. https://doi.org/10.3390/jcm13154333
APA StyleSelntigia, A., Pellegrini, L., Gebbia, F., & Galliano, D. (2024). Dysmorphic Uterus: More Questions than Answers. Journal of Clinical Medicine, 13(15), 4333. https://doi.org/10.3390/jcm13154333






