Client Oriented Scale of Improvement in First-Time and Experienced Hearing Aid Users: An Analysis of Five Predetermined Predictability Categories through Audiometric and Speech Testing
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Audiometric and Speech Assessment
2.3. Client-Oriented Scale of Improvement (COSI)
2.4. Statistical Analysis
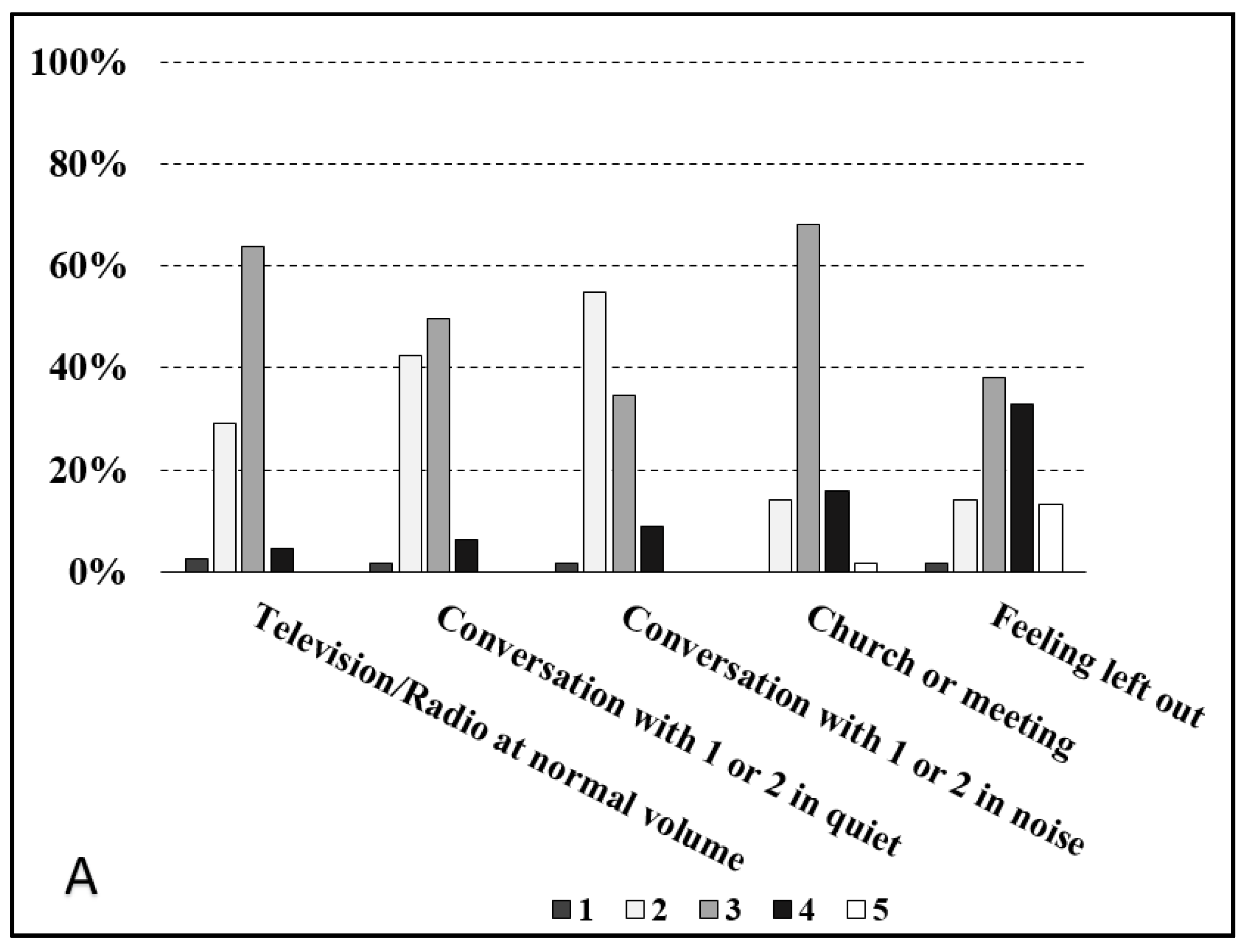
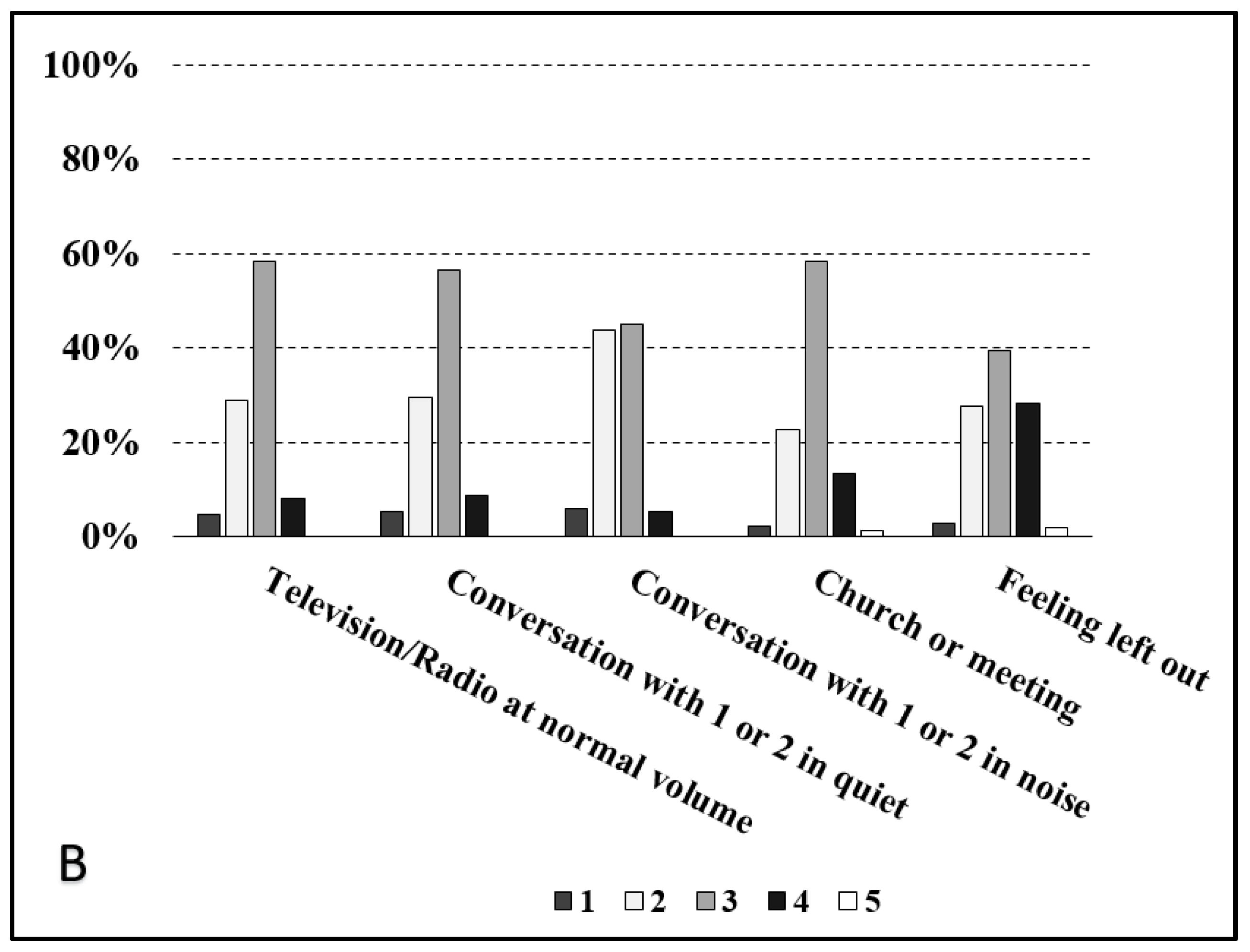
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Borre, E.D.; Kaalund, K.; Frisco, N.; Zhang, G.; Ayer, A.; Kelly-Hedrick, M.; Reed, S.D.; Emmett, S.D.; Francis, H.; Tucci, D.L.; et al. The Impact of Hearing Loss and Its Treatment on Health-Related Quality of Life Utility: A Systematic Review with Meta-analysis. J. Gen. Intern. Med. 2023, 38, 456–479. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Thorpe, R.; Gordon-Salant, S.; Ferrucci, L. Hearing loss prevalence and risk factors among older adults in the United States. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 582–590. [Google Scholar] [CrossRef]
- Jayakody, D.M.P.; Friedland, P.L.; Martins, R.N.; Sohrabi, H.R. Impact of Aging on the Auditory System and Related Cognitive Functions: A Narrative Review. Front. Neurosci. 2018, 12, 125. [Google Scholar] [CrossRef] [PubMed]
- Tu, N.C.; Friedman, R.A. Age-related hearing loss: Unraveling the pieces. Laryngoscope Investig. Otolaryngol. 2018, 3, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Gazia, F.; Portelli, D.; Lo Vano, M.; Ciodaro, F.; Galletti, B.; Bruno, R.; Freni, F.; Alberti, G.; Galletti, F. Extended wear hearing aids: A comparative, pilot study. Eur. Arch. Otorhinolaryngol. 2022, 279, 5415–5422. [Google Scholar] [CrossRef] [PubMed]
- Bruno, R.; Freni, F.; Portelli, D.; Alberti, G.; Gazia, F.; Meduri, A.; Galletti, F.; Galletti, B. Frequency-lowering processing to improve speech-in-noise intelligibility in patients with age-related hearing loss. Eur. Arch. Otorhinolaryngol. 2021, 278, 3697–3706. [Google Scholar] [CrossRef] [PubMed]
- Gazia, F.; Galletti, B.; Portelli, D.; Alberti, G.; Freni, F.; Bruno, R.; Galletti, F. Real ear measurement (REM) and auditory performances with open, tulip and double closed dome in patients using hearing aids. Eur. Arch. Otorhinolaryngol. 2020, 277, 1289–1295. [Google Scholar] [CrossRef] [PubMed]
- Dillon, H. Hearing Aids, 2nd ed.; Thieme: New York, NY, USA, 2012. [Google Scholar]
- Ferguson, M.A.; Kitterick, P.T.; Chong, L.Y.; Edmondson-Jones, M.; Barker, F.; Hoare, D.J. Hearing aids for mild to moderate hearing loss in adults. Cochrane Database Syst. Rev. 2017, 9, CD012023. [Google Scholar] [CrossRef] [PubMed]
- Portelli, D.; Ciodaro, F.; Loteta, S.; Alberti, G.; Bruno, R. Audiological assessment with Matrix sentence test of percutaneous vs transcutaneous bone-anchored hearing aids: A pilot study. Eur. Arch. Otorhinolaryngol. 2023, 280, 4065–4072. [Google Scholar] [CrossRef]
- Portelli, D.; Loteta, S.; Ciodaro, F.; Salvago, P.; Galletti, C.; Freni, L.; Alberti, G. Functional outcomes for speech-in-noise intelligibility of NAL-NL2 and DSL v.5 prescriptive fitting rules in hearing aid users. Eur. Arch. Otorhinolaryngol. 2024, 281, 3227–3235. [Google Scholar] [CrossRef]
- Kramer, S.E.; Kapteyn, T.S.; Festen, J.M.; Tobi, H. Factors in subjective hearing disability. Audiology 1995, 34, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Giordano, P.; Argentero, P.; Canale, A.; Lacilla, M.; Albera, R. Evaluation of hearing aid benefit through a new questionnaire: CISQ (Complete Intelligibility Spatiality Quality). Acta Otorhinolaryngol. Ital. 2013, 33, 329–336. [Google Scholar] [PubMed]
- Korkmaz, M.H.; Bayır, Ö.; Er, S.; Işık, E.; Saylam, G.; Tatar, E.Ç.; Özdek, A. Satisfaction and compliance of adult patients using hearing aid and evaluation of factors affecting them. Eur. Arch. Otorhinolaryngol. 2016, 273, 3723–3732. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.M.; Alexander, G.C. The abbreviated profile of hearing aid benefit. Ear Hear. 1995, 16, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Gatehouse, S.; Noble, W. The Speech, Spatial and Qualities of Hearing Scale (SSQ). Int. J. Audiol. 2004, 43, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Dillon, H.; James, A.; Ginis, J. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. J. Am. Acad. Audiol. 1997, 8, 27–43. [Google Scholar] [PubMed]
- Lansbergen, S.; De Ronde-Brons, I.; Boymans, M.; Soede, W.; Dreschler, W.A. Evaluation of Auditory Functioning and Rehabilitation Using Patient-Reported Outcome Measures. Trends Hear. 2018, 22, 2331216518789022. [Google Scholar] [CrossRef] [PubMed]
- Windle, R. Trends in COSI responses associated with age and degree of hearing loss. Int. J. Audiol. 2022, 61, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Dornhoffer, J.R.; Meyer, T.A.; Dubno, J.R.; McRackan, T.R. Assessment of Hearing Aid Benefit Using Patient-Reported Outcomes and Audiologic Measures. Audiol. Neurootol. 2020, 25, 215–223. [Google Scholar] [CrossRef]
- Suresh, K.; Franck, K.; Arenberg, J.G.; Song, Y.; Lee, D.J.; Crowson, M.G. Development of a Predictive Model for Individualized Hearing Aid Benefit. Otol. Neurotol. 2023, 44, e1–e7. [Google Scholar] [CrossRef]
- Kapteyn, T.S. Factors in the appreciation of a prosthetic rehabilitation. Audiology 1977, 16, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Parving, A. The value of speech audiometry in hearing-aid rehabilitation. Scand. Audiol. 1991, 20, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Killion, M.C.; Gudmundsen, G.I. Fitting hearing aids using clinical prefitting speech measures: An evidence-based review. J. Am. Acad. Audiol. 2005, 16, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Munro, K.J.; Lutman, M.E. The effect of speech presentation level on measurement of auditory acclimatization to amplified speech. J. Acoust. Soc. Am. 2003, 114, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.C.; Davis, P.B.; Pogash, R. Multiple-channel non-linear power hearing instruments for children with severe hearing impairment: Long-term follow-up. Int. J. Audiol. 2004, 43, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Yund, E.W.; Roup, C.M.; Simon, H.J.; Bowman, G.A. Acclimatization in wide dynamic range multichannel compression and linear amplification hearing aids. J. Rehabil. Res. Dev. 2007, 43, 517–536. [Google Scholar] [CrossRef] [PubMed]
- Goderie, T.P.M.; Stam, M.; Lissenberg-Witte, B.I.; Merkus, P.; Lemke, U.; Smits, C.; Kramer, S.E. 10-Year Follow-Up Results of The Netherlands Longitudinal Study on Hearing: Trends of Longitudinal Change in Speech Recognition in Noise. Ear Hear. 2020, 41, 491–499. [Google Scholar] [CrossRef]
- Miller, S.; Zhang, Y. Neural coding of phonemic fricative contrast with and without hearing aid. Ear Hear. 2014, 35, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Hällgren, M.; Larsby, B.; Lyxell, B.; Arlinger, S. Evaluation of a cognitive test battery in young and elderly normal-hearing and hearing-impaired persons. J. Am. Acad. Audiol. 2001, 12, 357–370. [Google Scholar] [CrossRef]
- Besser, J.; Koelewijn, T.; Zekveld, A.A.; Kramer, S.E.; Festen, J.M. How linguistic closure and verbal working memory relate to speech recognition in noise—A review. Trends Amplif. 2013, 17, 75–93. [Google Scholar] [CrossRef]
- Gatehouse, S.; Naylor, G.; Elberling, C. Benefits from hearing aids in relation to the interaction between the user and the environment. Int. J. Audiol. 2003, 42, S77–S85. [Google Scholar] [CrossRef] [PubMed]
- Lunner, T. Cognitive function in relation to hearing aid use. Int. J. Audiol. 2003, 42 (Suppl. S1), S49–S58. [Google Scholar] [CrossRef] [PubMed]
- Rönnberg, J.; Rudner, M.; Foo, C.; Lunner, T. Cognition counts: A working memory system for ease of language understanding (ELU). Int. J. Audiol. 2008, 47, S99–S105. [Google Scholar] [CrossRef] [PubMed]
- Lunner, T.; Rudner, M.; Rönnberg, J. Cognition and hearing aids. Scand. J. Psychol. 2009, 50, 395–403. [Google Scholar] [CrossRef]
- Wang, D. Time-frequency masking for speech separation and its potential for hearing aid design. Trends Amplif. 2008, 12, 332–353. [Google Scholar] [CrossRef] [PubMed]
- Ng, E.H.N.; Classon, E.; Larsby, B.; Arlinger, S.; Lunner, T.; Rudner, M.; Rönnberg, J. Dynamic Relation Between Working Memory Capacity and Speech Recognition in Noise During the First 6 Months of Hearing Aid Use. Trends Hear. 2014, 18, 2331216514558688. [Google Scholar] [CrossRef] [PubMed]
- Humes, L.E.; Krull, V. Hearing aids for adults. In Evidence-Based Practice in Audiology: Evaluating Interventions or Children and Adults with Hearing Impairment; Wong, L., Hickson, L., Eds.; Plural Publishing: San Diego, CA, USA, 2012; pp. 61–92. [Google Scholar]
- Chang, Y.S.; Choi, J.; Moon, J.I.; Hong, S.H.; Chung, W.H.; Cho, Y.S. Factors associated with self-reported outcome in adaptation of hearing aid. Acta Oto-Laryngol. 2016, 136, 905–911. [Google Scholar] [CrossRef]
- Humes, L.E. Modeling and predicting hearing aid outcome. Trends Amplif. 2003, 7, 41–75. [Google Scholar] [CrossRef] [PubMed]
- Humes, L.E.; Wilson, D.L.; Humes, A.C. Examination of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss and gender. Int. J. Audiol. 2003, 42, 432–441. [Google Scholar] [CrossRef]
- Moberly, A.C.; Harris, M.S.; Boyce, L.; Vasil, K.; Wucinich, T.; Pisoni, D.B.; Baxter, J.; Ray, C.; Shafiro, V. Relating quality of life to outcomes and predictors in adult cochlear implant users: Are we measuring the right things? Laryngoscope 2018, 128, 959–966. [Google Scholar] [CrossRef]
- McRackan, T.R.; Bauschard, M.; Hatch, J.L.; Franko-Tobin, E.; Droghini, H.R.; Nguyen, S.A.; Dubno, J.R. Meta-analysis of quality-of-life improvement after cochlear implantation and associations with speech recognition abilities. Laryngoscope 2018, 128, 982–990. [Google Scholar] [CrossRef] [PubMed]


| Total Cohort N (%) | First Time HA Users (G1) N (%) | Experienced HA Users (G2) N (%) | Statistical Analysis (p) | |
|---|---|---|---|---|
| Sex | 0.75 | |||
| Male | 140 (48.95) | 54 (47.78) | 86 (49.71) | |
| Female | 146 (51.05) | 59 (52.22) | 87 (50.29) | |
| Age | 0.009 | |||
| ≤60 years | 31 (10.85) | 7 (6.2) | 24 (13.89) | |
| 61–79 years | 155 (54.19) | 73 (64.6) | 82 (47.39) | |
| ≥80 years | 100 (34.96) | 33 (29.20) | 67 (38.72) | |
| Hearing loss type | 0.54 | |||
| Sensorineural | 495 (86.53) | 198 (87.61) | 297 (85.83) | |
| Mixed | 77 (13.47) | 28 (12.39) | 49 (14.17) | |
| Hearing loss degree | 0.00001 | |||
| Mild | 34 (5.94) | 22 (9.73) | 14 (4.05) | |
| Medium | 397 (69.4) | 182 (80.53) | 225 (65.03) | |
| Severe | 110 (19.23) | 19 (8.41) | 90 (26.01) | |
| Profound | 31 (5.43) | 3 (1.33) | 17 (4.91) | |
| Mean PTA (dB HL) | ||||
| Left | 59.97 ± 18.76 | 54.77 ± 16.31 | 63.38 ± 19.44 | 0.15 |
| Right | 60.37 ± 18.77 | 55.30 ± 16.46 | 63.69 ± 19.37 | 0.14 |
| SDT (dB HL) | ||||
| Left | 47.30 ± 15.25 | 43.18 ± 14.83 | 50.05 ± 14.95 | 0.00012 |
| Right | 49.48 ± 16.28 | 44.24 ± 16.31 | 52.95 ± 15.41 | 0.00001 |
| SRT (dB HL) | ||||
| Left | 64.78 ± 14.63 | 60.98 ± 12.95 | 67.32 ± 15.1 | 0.0003 |
| Right | 64.05 ± 13.32 | 61.11 ± 13.19 | 65.97 ± 13.1 | 0.003 |
| SIT (dB HL) | ||||
| Left | 74.65 ± 13.15 | 72.04 ± 12.24 | 80 ± 13.59 | 0.014 |
| Right | 72.77 ± 11.22 | 71.77 ± 10.93 | 74.79 ± 11.74 | 0.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvago, P.; Vaccaro, D.; Plescia, F.; Vitale, R.; Cirrincione, L.; Evola, L.; Martines, F. Client Oriented Scale of Improvement in First-Time and Experienced Hearing Aid Users: An Analysis of Five Predetermined Predictability Categories through Audiometric and Speech Testing. J. Clin. Med. 2024, 13, 3956. https://doi.org/10.3390/jcm13133956
Salvago P, Vaccaro D, Plescia F, Vitale R, Cirrincione L, Evola L, Martines F. Client Oriented Scale of Improvement in First-Time and Experienced Hearing Aid Users: An Analysis of Five Predetermined Predictability Categories through Audiometric and Speech Testing. Journal of Clinical Medicine. 2024; 13(13):3956. https://doi.org/10.3390/jcm13133956
Chicago/Turabian StyleSalvago, Pietro, Davide Vaccaro, Fulvio Plescia, Rossana Vitale, Luigi Cirrincione, Lucrezia Evola, and Francesco Martines. 2024. "Client Oriented Scale of Improvement in First-Time and Experienced Hearing Aid Users: An Analysis of Five Predetermined Predictability Categories through Audiometric and Speech Testing" Journal of Clinical Medicine 13, no. 13: 3956. https://doi.org/10.3390/jcm13133956
APA StyleSalvago, P., Vaccaro, D., Plescia, F., Vitale, R., Cirrincione, L., Evola, L., & Martines, F. (2024). Client Oriented Scale of Improvement in First-Time and Experienced Hearing Aid Users: An Analysis of Five Predetermined Predictability Categories through Audiometric and Speech Testing. Journal of Clinical Medicine, 13(13), 3956. https://doi.org/10.3390/jcm13133956







