Incidence of Cervical Kyphosis and Factors Associated with Improvement in Postoperative Cervical Spinal Alignment in Idiopathic Scoliosis with Major Thoracolumbar/Lumbar and Thoracic Curves
Abstract
1. Background
2. Methods
2.1. Ethics Approval
2.2. Baseline Characteristics of Patients with AIS
2.3. Surgical Procedure
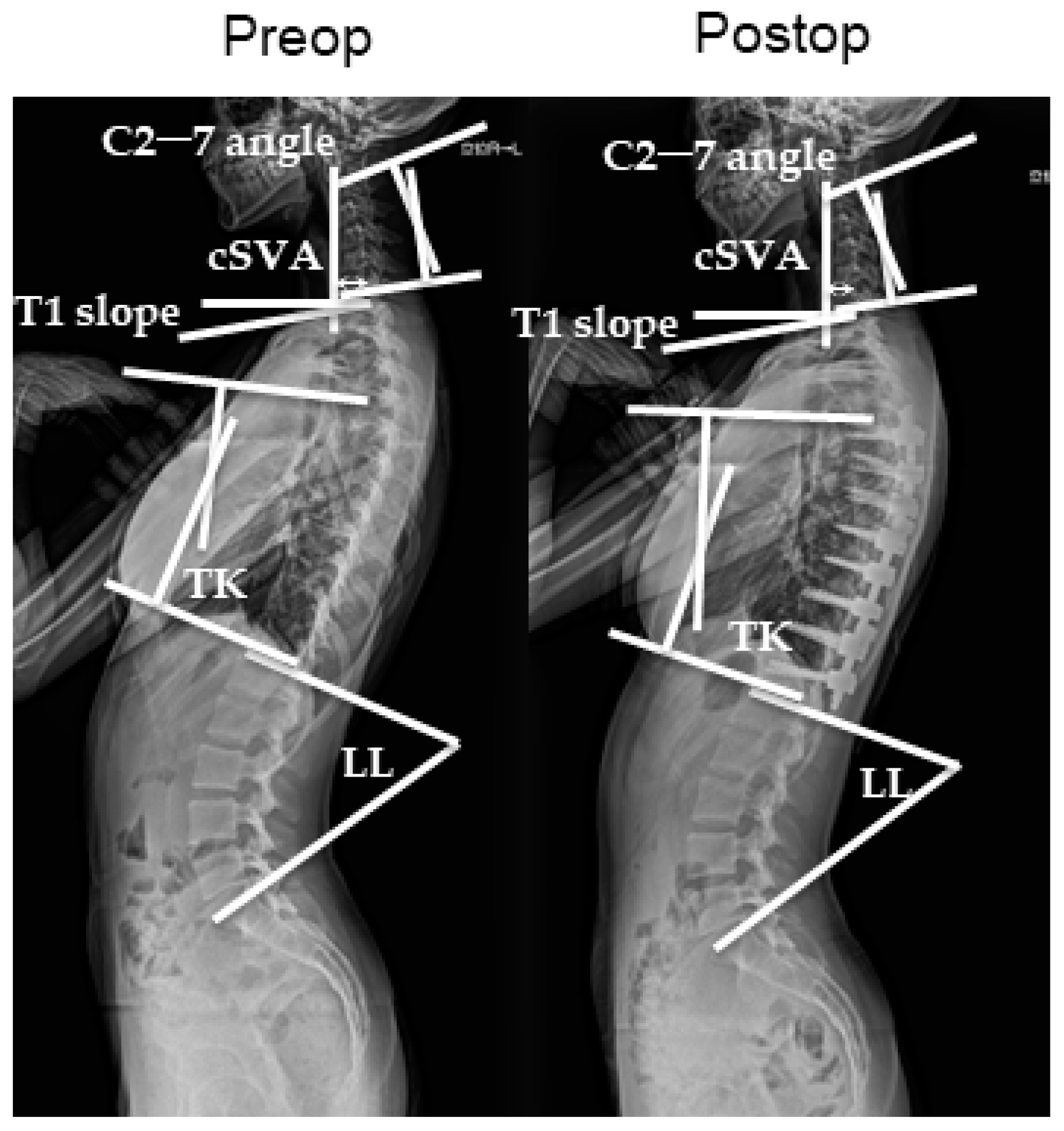
2.4. Radiographic Parameters
2.5. Statistical Analysis
3. Results
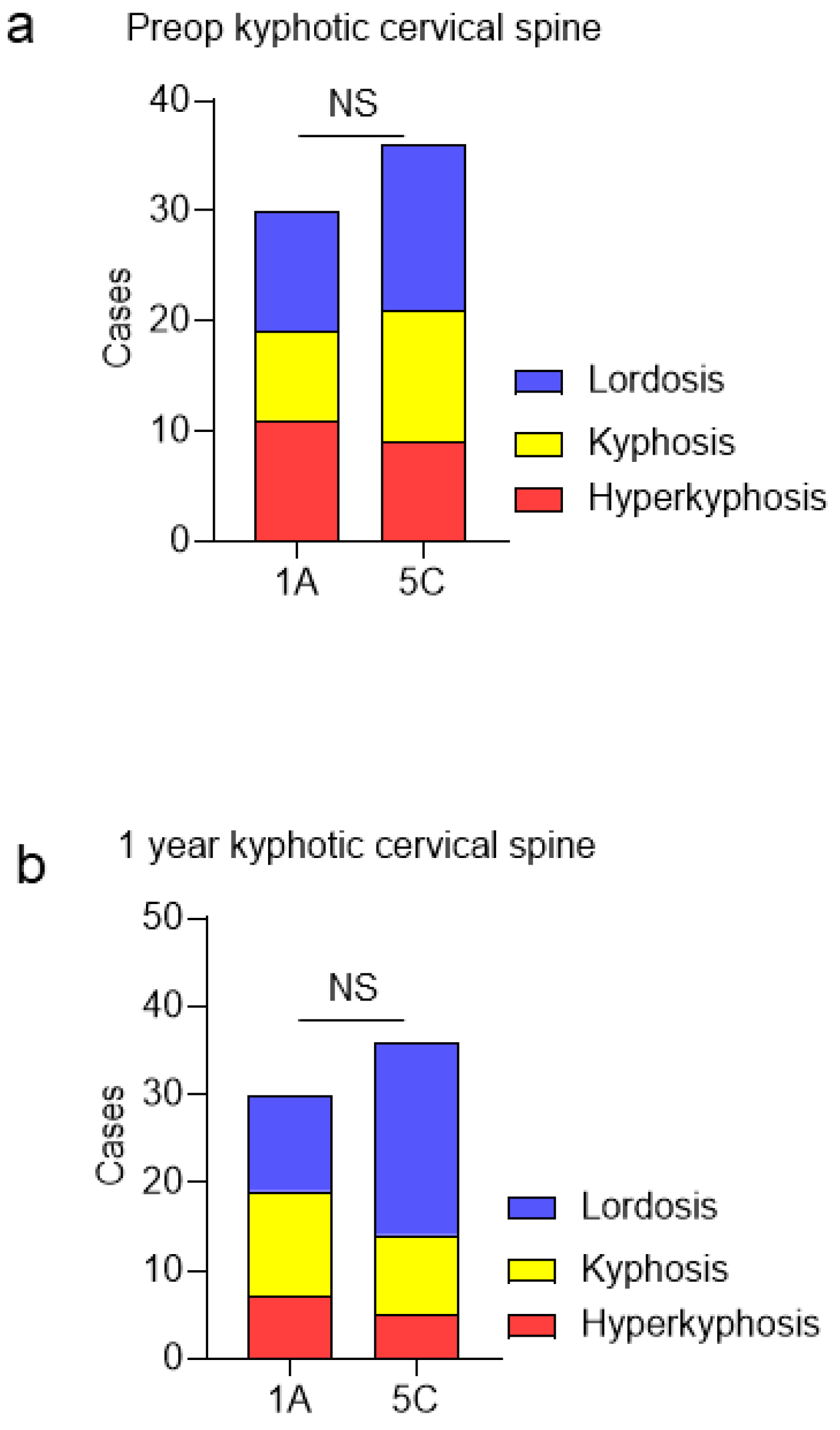
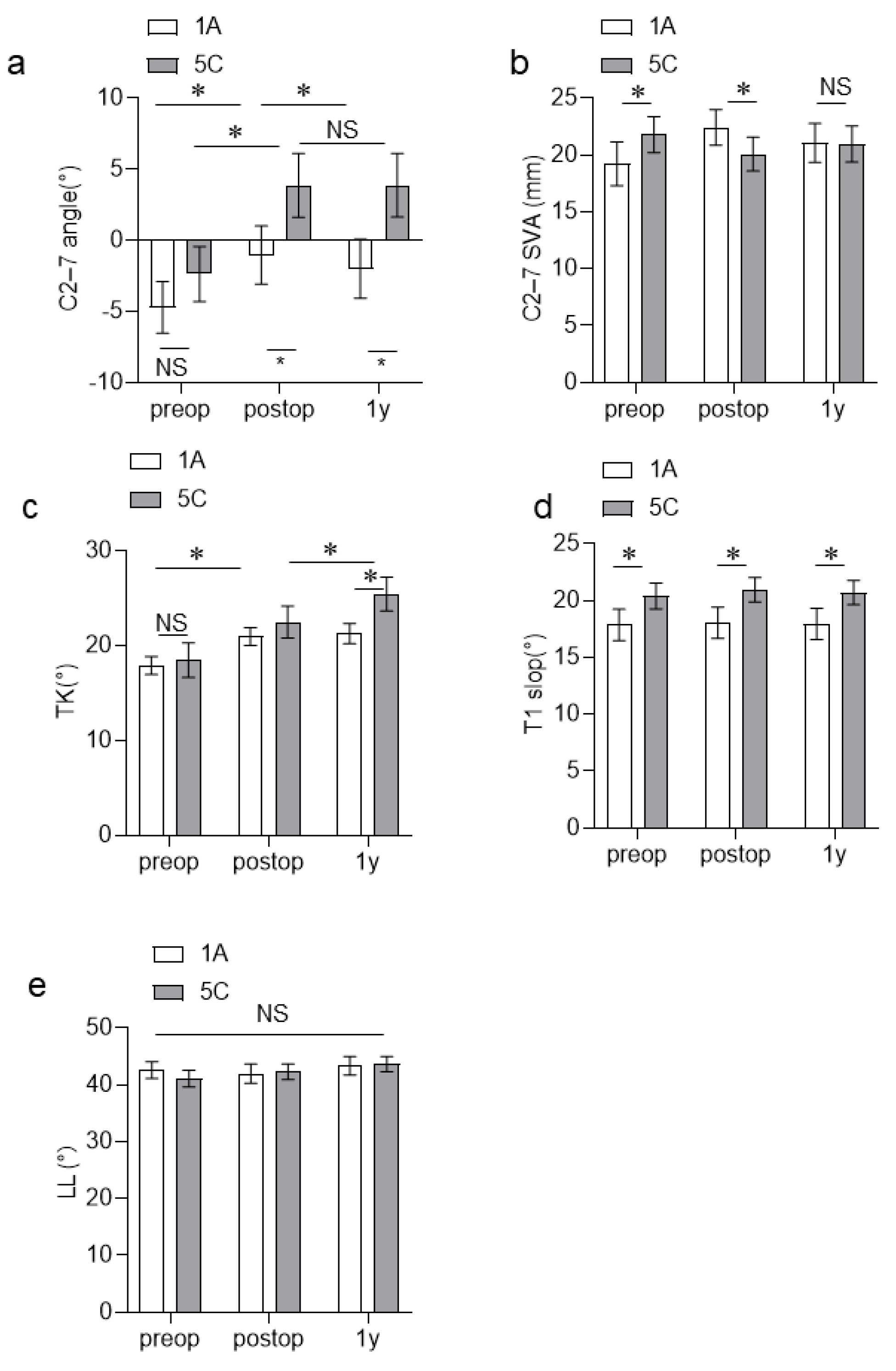
3.1. Radiographic Evaluations
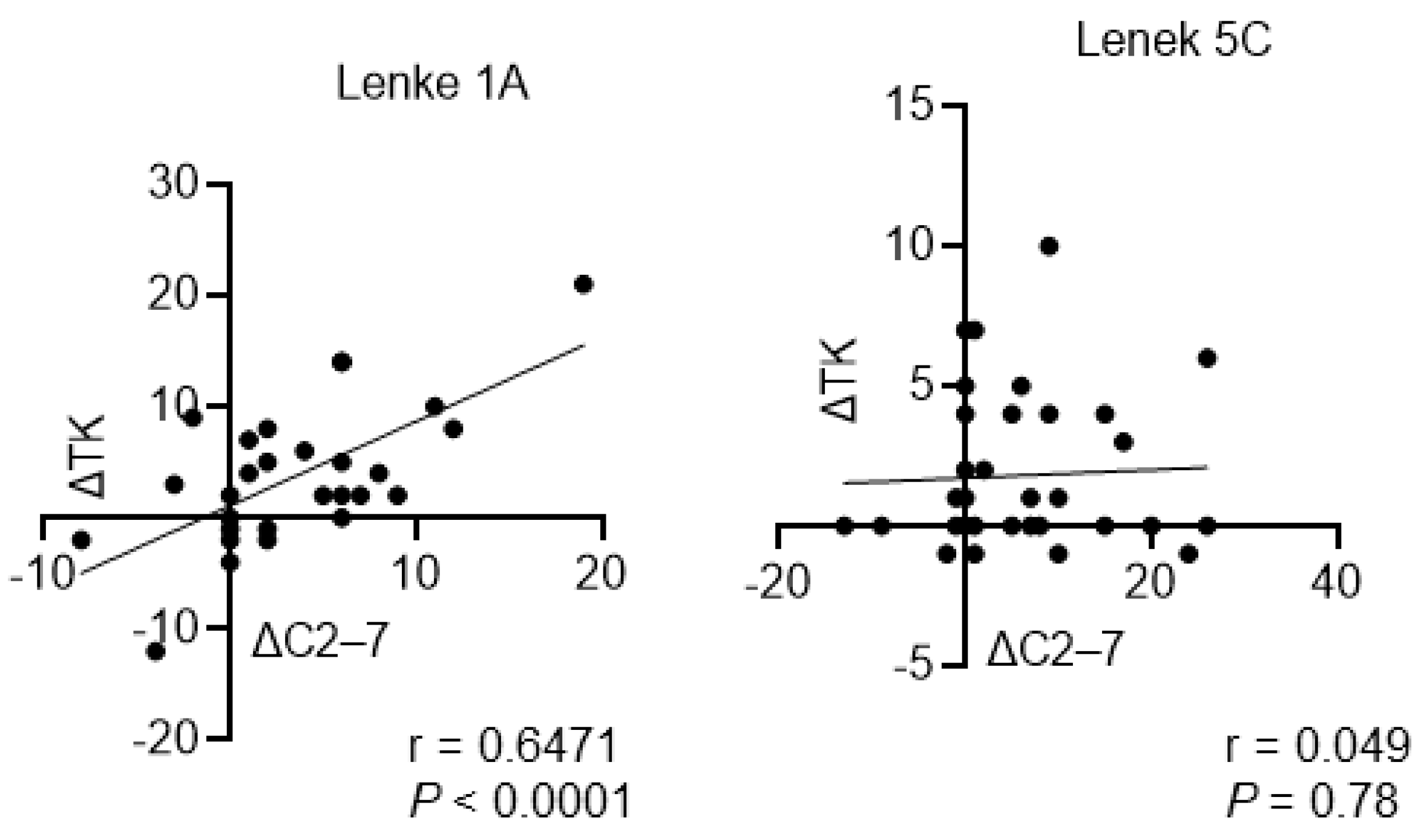
3.2. Association between C2–C7 Angle and Other Radiographic Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIS | adolescent idiopathic scoliosis |
| LL | lumbar lordosis |
| PSF | posterior spinal fusion |
| SVA | sagittal vertical axis |
| TK | thoracic kyphosis |
| TL | thoracolumbar |
References
- Watanabe, K.; Michikawa, T.; Yonezawa, I.; Takaso, M.; Minami, S.; Soshi, S.; Tsuji, T.; Okada, E.; Abe, K.; Takahashi, M.; et al. Physical Activities and Lifestyle Factors Related to Adolescent Idiopathic Scoliosis. J. Bone Jt. Surg. Am. 2017, 99, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- van Royen, B.J.B. Understanding the Lenke Classification for Adolescent Idiopathic Scoliosis (AIS). Curr. Probl. Diagn. Radiol. 2023, 52, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Ohrt-Nissen, S.; Cheung, J.P.Y.; Hallager, D.W.; Gehrchen, M.; Kwan, K.; Dahl, B.; Cheung, K.M.C.; Samartzis, D. Reproducibility of thoracic kyphosis measurements in patients with adolescent idiopathic scoliosis. Scoliosis Spinal Disord. 2017, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K.; Sassi, D.; Verdun, S.; Roussouly, P. Sagittal classification in adolescent idiopathic scoliosis: Original description and therapeutic implications. Eur. Spine J. 2018, 27, 2192–2202. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Faundez, A.; Dominguez, D.; Hoffmeyer, P.; Aunoble, S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: A literature review. Int. Orthop. 2015, 39, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Qiu, Y.; Qian, B.P.; Zhu, Z.Z.; Wang, B.; Yu, Y. Compensatory modulation for severe global sagittal imbalance: Significance of cervical compensation on quality of life in thoracolumbar kyphosis secondary to ankylosing spondylitis. Eur. Spine J. 2016, 25, 3715–3722. [Google Scholar] [CrossRef] [PubMed]
- Youn, M.S.; Shin, J.K.; Goh, T.S.; Kang, S.S.; Jeon, W.K.; Lee, J.S. Relationship between cervical sagittal alignment and health-related quality of life in adolescent idiopathic scoliosis. Eur. Spine J. 2016, 25, 3114–3119. [Google Scholar] [CrossRef] [PubMed]
- Oe, S.; Togawa, D.; Yoshida, G.; Hasegawa, T.; Yamato, Y.; Kobayashi, S.; Yasuda, T.; Banno, T.; Mihara, Y.; Matsuyama, Y. Difference in Spinal Sagittal Alignment and Health-Related Quality of Life between Males and Females with Cervical Deformity. Asian Spine J. 2017, 11, 959–967. [Google Scholar] [CrossRef]
- Nagata, K.; Ishimoto, Y.; Nakao, S.; Fujiwara, S.; Matsuoka, T.; Kitagawa, T.; Nakagawa, M.; Minetama, M.; Kawakami, M. Factors Associated with Neck and Shoulder Pain in Volunteers. Spine Surg. Relat. Res. 2018, 2, 177–185. [Google Scholar] [CrossRef]
- Okubo, T.; Yagi, M.; Suzuki, S.; Takahashi, Y.; Nori, S.; Tsuji, O.; Nagoshi, N.; Matsumoto, M.; Nakamura, M.; Watanabe, K. Cervical sagittal alignment is influenced by changes in thoracic and lumbar sagittal alignments after correction surgery in patients with lenke type 6 adolescent idiopathic scoliosis. N. Am. Spine Soc. J. 2022, 12, 100166. [Google Scholar] [CrossRef]
- Tang, Y.; Xu, X.; Zhu, F.; Chen, C.; Wang, F.; Lu, M.; Huang, X. Incidence and Risk Factors of Cervical Kyphosis in Patients with Adolescent Idiopathic Scoliosis. World Neurosurg. 2019, 127, e788–e792. [Google Scholar] [CrossRef]
- Han, S.M.; Wen, J.X.; Cao, L.; Wu, H.Z.; Liu, C.; Yang, C.; Yang, H.H.; Gao, B.L.; Wu, W.J. Sagittal morphology of the cervical spine in adolescent idiopathic scoliosis: A retrospective case-control study. Quant. Imaging Med. Surg. 2022, 12, 3049–3060. [Google Scholar] [CrossRef] [PubMed]
- Winter, R.B.; Lovell, W.W.; Moe, J.H. Excessive thoracic lordosis and loss of pulmonary function in patients with idiopathic scoliosis. J. Bone Jt. Surg. Am. 1975, 57, 972–977. [Google Scholar] [CrossRef]
- Lowenstein, J.E.; Matsumoto, H.; Vitale, M.G.; Weidenbaum, M.; Gomez, J.A.; Lee, F.Y.; Hyman, J.E.; Roye, D.P., Jr. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: A comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 2007, 32, 448–452. [Google Scholar] [CrossRef]
- Yu, M.; Silvestre, C.; Mouton, T.; Rachkidi, R.; Zeng, L.; Roussouly, P. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: A morphological classification of 120 cases. Eur. Spine J. 2013, 22, 2372–2381. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Sakai, D.; Watanabe, M.; Katoh, H.; Sato, M.; Mochida, J. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis: A comparative study of 42 adolescents with idiopathic scoliosis and 24 normal adolescents. Eur. Spine J. 2016, 25, 3226–3233. [Google Scholar] [CrossRef]
- Wang, L.; Liu, X. Cervical sagittal alignment in adolescent idiopathic scoliosis patients (Lenke type 1-6). J. Orthop. Sci. 2017, 22, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Akbar, M.; Almansour, H.; Lafage, R.; Diebo, B.G.; Wiedenhöfer, B.; Schwab, F.; Lafage, V.; Pepke, W. Sagittal alignment of the cervical spine in the setting of adolescent idiopathic scoliosis. J. Neurosurg. Spine 2018, 29, 506–514. [Google Scholar] [CrossRef]
- Guo, G.M.; Li, J.; Diao, Q.X.; Zhu, T.H.; Song, Z.X.; Guo, Y.Y.; Gao, Y.Z. Cervical lordosis in asymptomatic individuals: A meta-analysis. J. Orthop. Surg. Res. 2018, 13, 147. [Google Scholar] [CrossRef]
- Mladenov, K.V.; Vaeterlein, C.; Stuecker, R. Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: Effects on the sagittal alignment. Eur. Spine J. 2011, 20, 1114–1117. [Google Scholar] [CrossRef] [PubMed]
- Canavese, F.; Turcot, K.; De Rosa, V.; de Coulon, G.; Kaelin, A. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur. Spine J. 2011, 20, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Deng, K.; Tang, Y.; Yang, Z.; Liu, X.; Liu, Z.; Wei, F.; Wu, F.; Zhou, H.; Li, Y.; et al. Postoperative alterations of sagittal cervical alignment and risk factors for cervical kyphosis in 124 Lenke 1 adolescent idiopathic scoliosis patients. BMC Musculoskelet. Disord. 2021, 22, 1001. [Google Scholar] [CrossRef] [PubMed]
- Garg, B.; Mehta, N.; Gupta, A.; Sugumar, P.A.A.; Shetty, A.P.; Basu, S.; Jakkepally, S.; Gowda, S.D.; Babu, J.N.; Chhabra, H.S. Cervical s agittal alignment in Lenke 1 a dolescent i diopathic s coliosis and a ssessment of it’s a lteration with surgery: A retrospective, multi-centric study. Spine Deform. 2021, 9, 1559–1568. [Google Scholar] [CrossRef] [PubMed]
- Yan, P.; Zhang, Y.; Liu, S.; Shu, S.; Liu, Z.; Zhu, Z.; Qian, B.; Qiu, Y.; Bao, H. Sagittal Profile Response Cerv. Spine After Posterior Correct. Thorac. Lumbar Adolesc. Idiopathic Scoliosis: Correl. Thorac. Kyphosis? World Neurosurg. 2018, 120, e333–e341. [Google Scholar] [CrossRef]
- Shimizu, T.; Cerpa, M.; Lehman, R.A.; Sielatycki, J.A.; Pongmanee, S.; Lenke, L.G. Reciprocal Change in Sagittal Profiles After Adolescent Idiopathic Scoliosis Surgery With Segmental Pedicle Screw Construct: A Full-body X-ray Analysis. Spine 2019, 44, 1705–1714. [Google Scholar] [CrossRef] [PubMed]
- Clement, J.L.; Le Goff, L.; Oborocianu, I.; Rosello, O.; Bertoncelli, C.; Solla, F.; Rampal, V. Surgical increase in thoracic kyphosis predicts increase of cervical lordosis after thoracic fusion for adolescent idiopathic scoliosis. Eur. Spine J. 2021, 30, 3550–3556. [Google Scholar] [CrossRef]
- Charles, Y.P.; Sfeir, G.; Matter-Parrat, V.; Sauleau, E.A.; Steib, J.P. Cervical sagittal alignment in idiopathic scoliosis treated by posterior instrumentation and in situ bending. Spine 2015, 40, E419–E427. [Google Scholar] [CrossRef]
| Variables | Patients with AIS (n = 66) | ||
|---|---|---|---|
| Lenke Classification | Lenke Type 1A Group (n = 30) | Lenke Type 5C Group (n = 36) | p Values |
| Age (years) | 16.3 ± 2.5 | 16.0 ± 2.7 | NS |
| Female/male patients (n) | 27/3 | 35/1 | NS |
| Risser grade (n) | NS | ||
| 1 | 1 | 1 | |
| 2 | 1 | 2 | |
| 3 | 0 | 4 | |
| 4 | 14 | 13 | |
| 5 | 14 | 16 | |
| Height (cm) | 157.6 ± 3.8 | 158.1 ± 5.1 | NS |
| Weight (kg) | 47.4 ± 4.4 | 48.1 ± 5.1 | NS |
| BMI (kg/m2) | 19.1 ± 1.7 | 18.8 ± 1.9 | NS |
| Coronal parameters | |||
| MT Cobb angles (°) | 46.4 ± 8.1 | ||
| TL/L Cobb angles (°) | 39.1 ± 8.5 | ||
| Number of fixed vertebrae | 5.17 ± 2.2 | 7.71 ± 1.1 | p < 0.05 |
| UIV, n (%) | |||
| T4 | 2 | ||
| T5 | 19 | ||
| T6 | 9 | ||
| T7 | 1 | ||
| T8 | |||
| T9 | 4 | ||
| T10 | 8 | ||
| T11 | 17 | ||
| T12 | 7 | ||
| LIV, n (%) | |||
| T11 | 4 | ||
| T12 | 11 | ||
| L1 | 13 | ||
| L2 | 2 | 2 | |
| L3 | 32 | ||
| L4 | 2 | ||
| Variable | Lenke Type 1A | Lenke Type 5C | p Value |
|---|---|---|---|
| C2–7 angle, ° | −1.99 ± 1.43 | 3.88 ± 2.24 | p < 0.005 * |
| C2–7 SVA, mm | 21.1 ± 1.71 | 20.9 ± 1.58 | p < 0.005 * |
| TK, ° | 21.2 ± 1.05 | 25.4 ± 1.77 | p < 0.005 * |
| T1 slop, ° | 17.9 ± 1.37 | 20.7 ± 1.06 | p < 0.005 * |
| LL, ° | 43.3 ± 1.64 | 43.6 ± 1.36 | NS |
| Lenke Type 1A C2–C7 Angles (°) | Preoperatively | At 1 Year Postoperatively | |
|---|---|---|---|
| C2–C7 SVA (mm) Preoperatively | r | ||
| p value | 0.065 | 0.215 | |
| At 1 year postoperatively | r | ||
| p value | 0.502 | 0.588 | |
| T1 slope (°) Preoperatively | r | 0.367 | 0.427 |
| p value | 0.046 * | 0.023 * | |
| At 1 year postoperatively | r | 0.374 | 0.454 |
| p value | 0.048 * | 0.015 * | |
| TK (°) Preoperatively | r | 0.301 | 0.381 |
| p value | 0.048 * | 0.041 * | |
| At 1 year postoperatively | r | 0.424 | |
| p value | 0.677 | 0.021 * | |
| LL (°) Preoperatively | r | ||
| p value | 0.413 | 0.242 | |
| At 1 year postoperatively | r | ||
| p value | 0.622 | 0.3929 |
| Lenke Type 5C C2–C7 Angles (°) | Preoperatively | At 1 Year Postoperatively | |
|---|---|---|---|
| C2–C7 SVA (mm) Preoperatively | r | ||
| p value | 0.359 | 0.767 | |
| At 1 year postoperatively | r | ||
| p value | 0.734 | 0.856 | |
| T1 slope (°) Preoperatively | r | 0.599 | 0.564 |
| p value | 0.0001 * | 0.0004 * | |
| At 1 year postoperatively | r | ||
| p value | 0.215 | 0.268 | |
| TK (°) Preoperatively | r | ||
| p value | 0.879 | 0.841 | |
| At 1 year postoperatively | r | ||
| p value | 0.709 | 0.951 | |
| LL (°) Preoperatively | r | ||
| p value | 0.421 | 0.223 | |
| At 1 year postoperatively | r | ||
| p value | 0.526 | 0.268 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizukami, K.; Ohba, T.; Tanaka, N.; Oda, K.; Katsu, M.; Takei, H.; Go, G.; Haro, H. Incidence of Cervical Kyphosis and Factors Associated with Improvement in Postoperative Cervical Spinal Alignment in Idiopathic Scoliosis with Major Thoracolumbar/Lumbar and Thoracic Curves. J. Clin. Med. 2024, 13, 3811. https://doi.org/10.3390/jcm13133811
Mizukami K, Ohba T, Tanaka N, Oda K, Katsu M, Takei H, Go G, Haro H. Incidence of Cervical Kyphosis and Factors Associated with Improvement in Postoperative Cervical Spinal Alignment in Idiopathic Scoliosis with Major Thoracolumbar/Lumbar and Thoracic Curves. Journal of Clinical Medicine. 2024; 13(13):3811. https://doi.org/10.3390/jcm13133811
Chicago/Turabian StyleMizukami, Kai, Tetsuro Ohba, Nobuki Tanaka, Kotaro Oda, Marina Katsu, Hayato Takei, Goto Go, and Hirotaka Haro. 2024. "Incidence of Cervical Kyphosis and Factors Associated with Improvement in Postoperative Cervical Spinal Alignment in Idiopathic Scoliosis with Major Thoracolumbar/Lumbar and Thoracic Curves" Journal of Clinical Medicine 13, no. 13: 3811. https://doi.org/10.3390/jcm13133811
APA StyleMizukami, K., Ohba, T., Tanaka, N., Oda, K., Katsu, M., Takei, H., Go, G., & Haro, H. (2024). Incidence of Cervical Kyphosis and Factors Associated with Improvement in Postoperative Cervical Spinal Alignment in Idiopathic Scoliosis with Major Thoracolumbar/Lumbar and Thoracic Curves. Journal of Clinical Medicine, 13(13), 3811. https://doi.org/10.3390/jcm13133811







