Changes in Working Situations of Employed Long COVID Patients: Retrospective Study in Japanese Outpatient Clinic
Abstract
1. Introduction
2. Subjects and Methods
2.1. Study Design and Clinical Assessment of Long COVID
2.2. Inclusion and Exclusion Criteria
2.3. Impact of Long COVID on Working Situations
2.4. Setting for the Periods of COVID-19 Viral Variants
2.5. Evaluation of Quality of Life and Mental Condition
2.6. Statistical Analysis
2.7. Ethical Approval
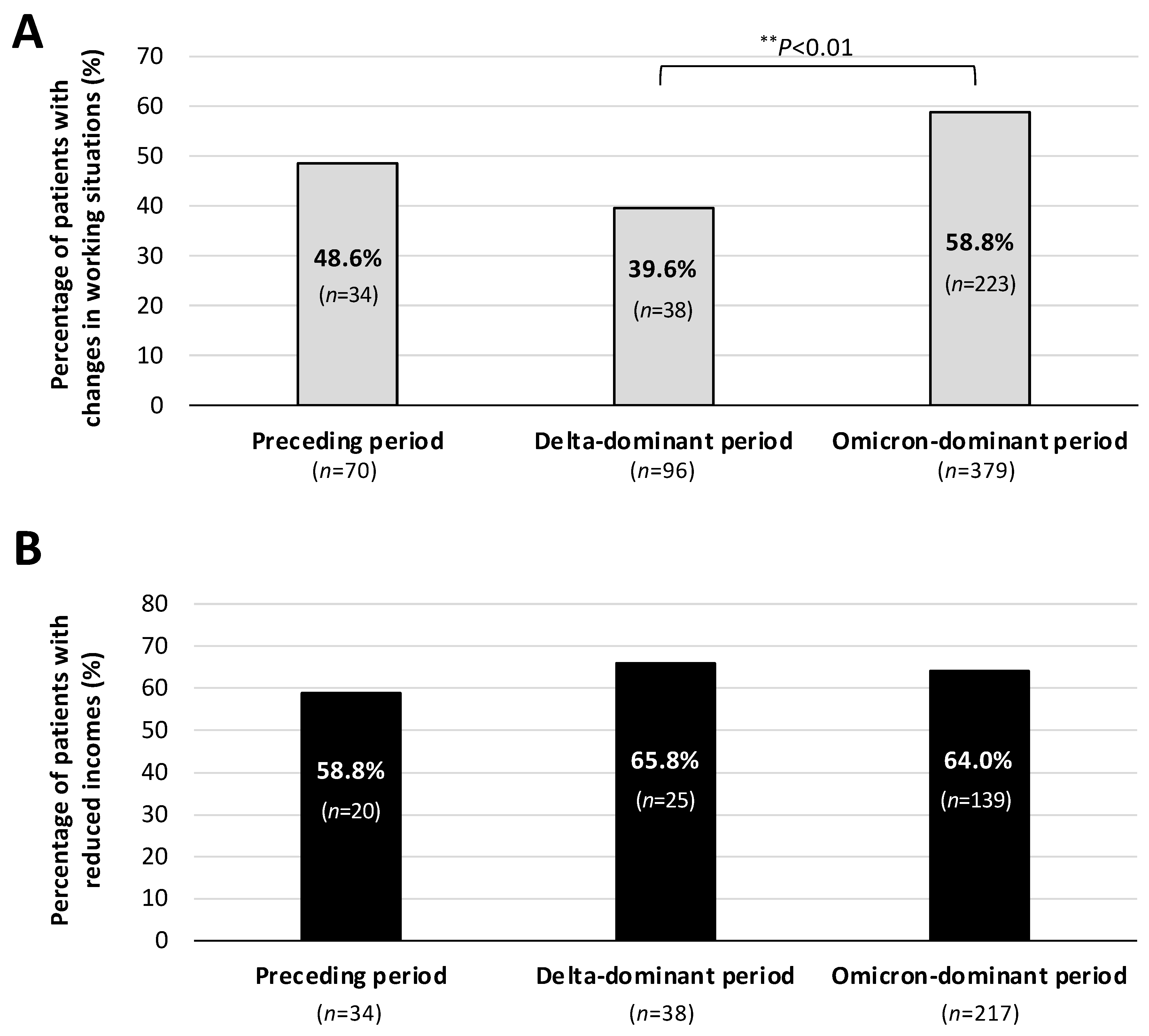
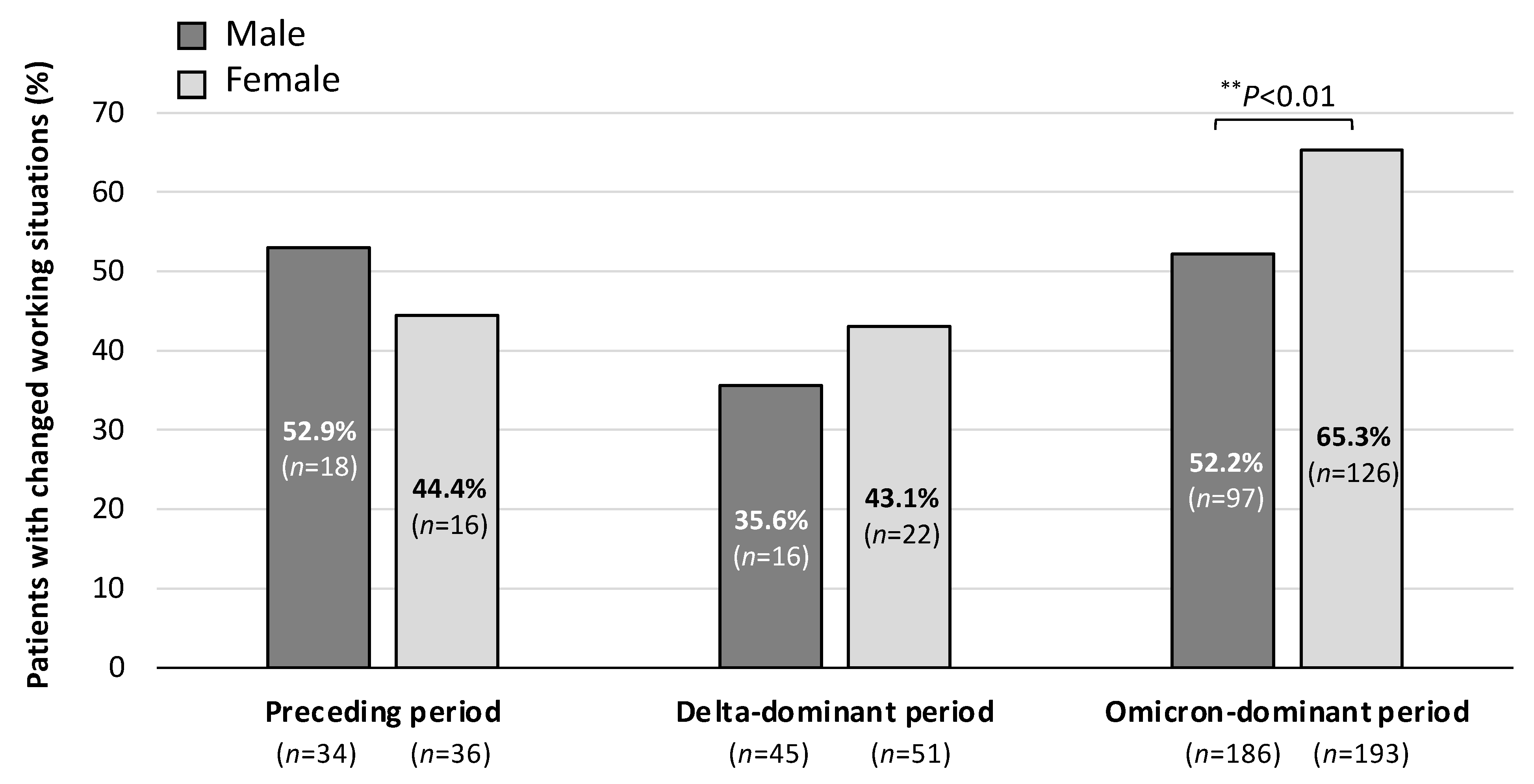
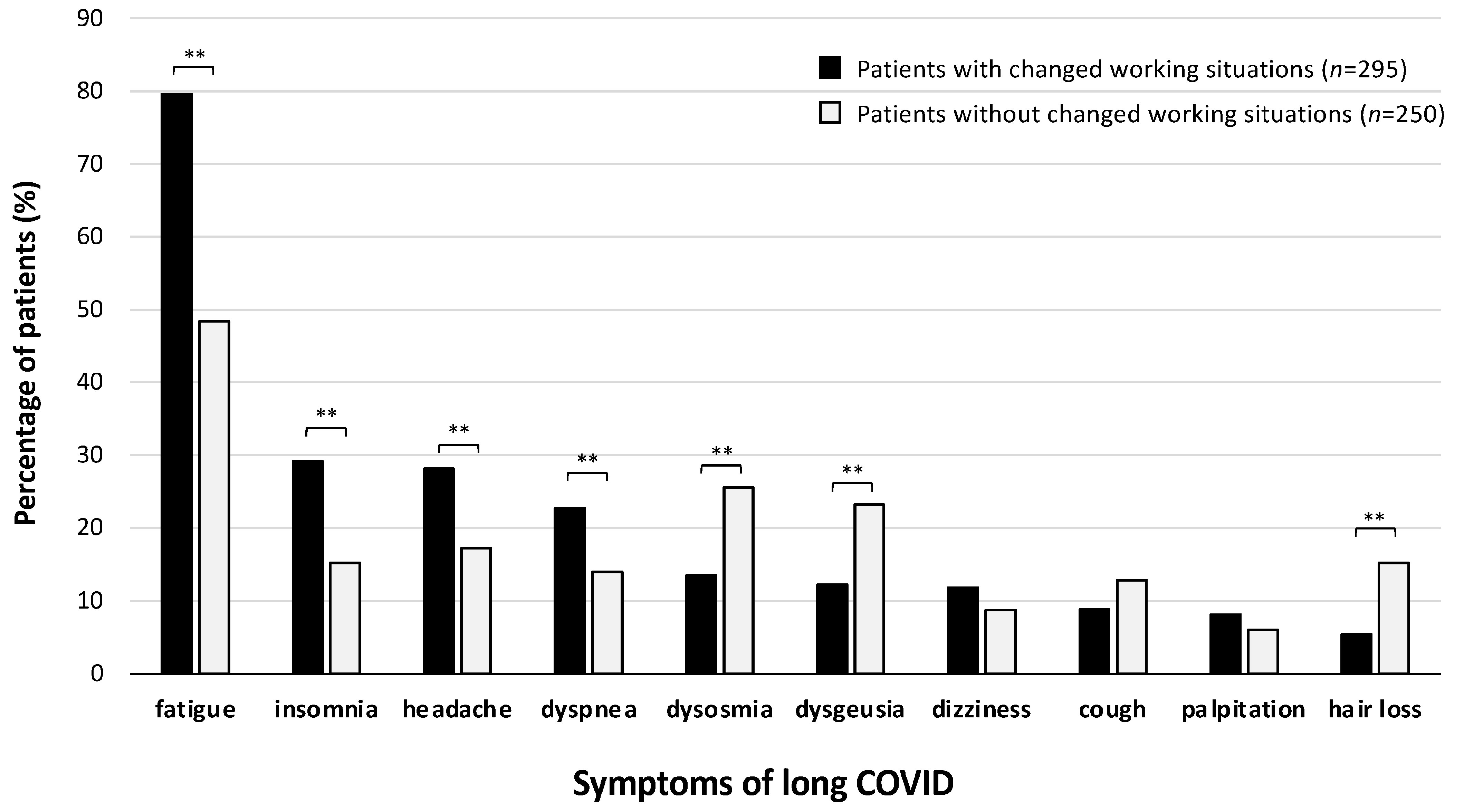
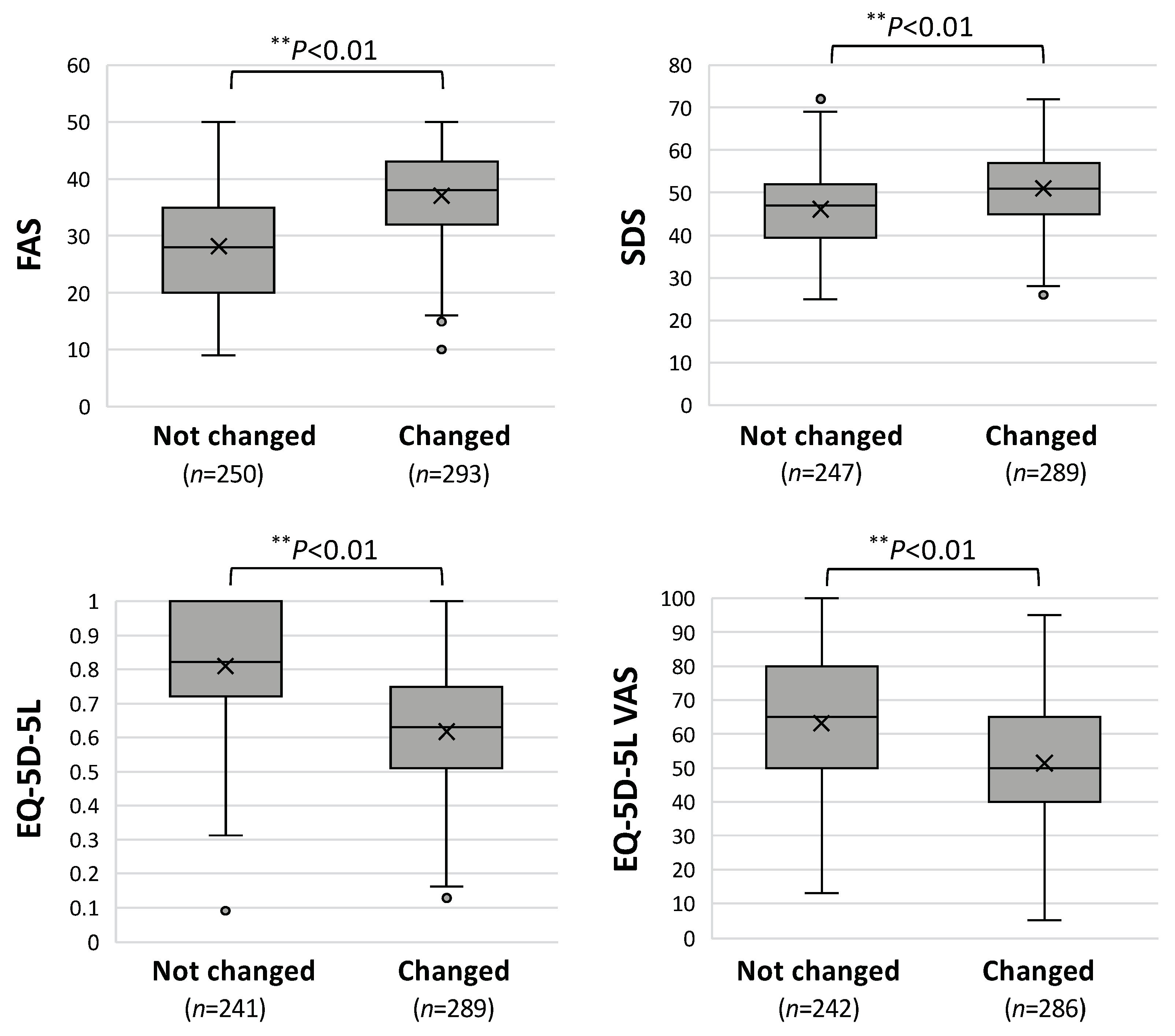
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Shrestha, L.B.; Foster, C.; Rawlinson, W.; Tedla, N.; Bull, R.A. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission. Rev. Med. Virol. 2022, 32, e2381. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Raveendran, A.V.; Jayadevan, R.; Sashidharan, S. Long COVID: An overview. Diabetes Metab. Syndr. 2021, 15, 869–875. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Klein, J.; Wood, J.; Jaycox, J.; Dhodapkar, R.M.; Lu, P.; Gehlhausen, J.R.; Tabachnikova, A.; Greene, K.; Tabacof, L.; Malik, A.A.; et al. Distinguishing features of Long COVID identified through immune profiling. Nature 2023, 623, 139–148. [Google Scholar] [CrossRef]
- Monje, M.; Iwasaki, A. The neurobiology of long COVID. Neuron 2022, 110, 3484–3496. [Google Scholar] [CrossRef] [PubMed]
- Sunada, N.; Nakano, Y.; Otsuka, Y.; Tokumasu, K.; Honda, H.; Sakurada, Y.; Matsuda, Y.; Hasegawa, T.; Omura, D.; Ochi, K.; et al. Characteristics of Sleep Disturbance in Patients with Long COVID: A Retrospective Observational Study in Japan. J. Clin. Med. 2022, 11, 7332. [Google Scholar] [CrossRef] [PubMed]
- Fujita, K.; Otsuka, Y.; Sunada, N.; Honda, H.; Tokumasu, K.; Nakano, Y.; Sakurada, Y.; Obika, M.; Hagiya, H.; Otsuka, F. Manifestation of Headache Affecting Quality of Life in Long COVID Patients. J. Clin. Med. 2023, 12, 3533. [Google Scholar] [CrossRef]
- Nakano, Y.; Otsuka, Y.; Honda, H.; Sunada, N.; Tokumasu, K.; Sakurada, Y.; Matsuda, Y.; Hasegawa, T.; Ochi, K.; Hagiya, H.; et al. Transitional Changes in Fatigue-Related Symptoms Due to Long COVID: A Single-Center Retrospective Observational Study in Japan. Medicina 2022, 58, 1393. [Google Scholar] [CrossRef]
- Nakano, Y.; Sunada, N.; Tokumasu, K.; Honda, H.; Otsuka, Y.; Sakurada, Y.; Matsuda, Y.; Hasegawa, T.; Omura, D.; Ochi, K.; et al. Occult endocrine disorders newly diagnosed in patients with post-COVID-19 symptoms. Sci. Rep. 2024, 14, 5446. [Google Scholar] [CrossRef]
- Ladds, E.; Rushforth, A.; Wieringa, S.; Taylor, S.; Rayner, C.; Husain, L.; Greenhalgh, T. Persistent symptoms after COVID-19: Qualitative study of 114 “long COVID” patients and draft quality principles for services. BMC Health Serv. Res. 2020, 20, 1144. [Google Scholar] [CrossRef]
- Kohn, L.; Dauvrin, M.; Detollenaere, J.; Primus-de Jong, C.; Maertens de Noordhout, C.; Castanares-Zapatero, D.; Cleemput, I.; Van den Heede, K. Long COVID and return to work: A qualitative study. Occup. Med. 2024, 74, 29–36. [Google Scholar] [CrossRef]
- Suran, M. Long COVID Linked With Unemployment in New Analysis. JAMA 2023, 329, 701–702. [Google Scholar] [CrossRef]
- Cruickshank, M.; Brazzelli, M.; Manson, P.; Torrance, N.; Grant, A. What is the impact of long-term COVID-19 on workers in healthcare settings? A rapid systematic review of current evidence. PLoS ONE 2024, 19, e0299743. [Google Scholar] [CrossRef]
- Otsuka, Y.; Tokumasu, K.; Nakano, Y.; Honda, H.; Sakurada, Y.; Sunada, N.; Omura, D.; Hasegawa, K.; Hagiya, H.; Obika, M.; et al. Clinical Characteristics of Japanese Patients Who Visited a COVID-19 Aftercare Clinic for Post-Acute Sequelae of COVID-19/Long COVID. Cureus 2021, 13, e18568. [Google Scholar] [CrossRef]
- Sakurada, Y.; Sunada, N.; Honda, H.; Tokumasu, K.; Otsuka, Y.; Nakano, Y.; Hanayama, Y.; Furukawa, M.; Hagiya, H.; Otsuka, F. Serial Changes of Long COVID Symptoms and Clinical Utility of Serum Antibody Titers for Evaluation of Long COVID. J. Clin. Med. 2022, 11, 1309. [Google Scholar] [CrossRef]
- Siso-Almirall, A.; Brito-Zeron, P.; Conangla Ferrin, L.; Kostov, B.; Moragas Moreno, A.; Mestres, J.; Sellares, J.; Galindo, G.; Morera, R.; Basora, J.; et al. Long COVID-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management. Int. J. Environ. Res. Public Health 2021, 18, 4350. [Google Scholar] [CrossRef]
- Kato, Y. Case Management of COVID-19 (Secondary Version). JMA J. 2021, 4, 191–197. [Google Scholar] [CrossRef]
- De Vries, J.; Michielsen, H.; Van Heck, G.L.; Drent, M. Measuring fatigue in sarcoidosis: The Fatigue Assessment Scale (FAS). Br. J. Health Psychol. 2004, 9, 279–291. [Google Scholar] [CrossRef]
- Shiroiwa, T.; Ikeda, S.; Noto, S.; Igarashi, A.; Fukuda, T.; Saito, S.; Shimozuma, K. Comparison of Value Set Based on DCE and/or TTO Data: Scoring for EQ-5D-5L Health States in Japan. Value Health 2016, 19, 648–654. [Google Scholar] [CrossRef]
- Tokumasu, K.; Matsuki, N.; Fujikawa, H.; Sakamoto, Y.; Otsuka, F. Reliability and Validity of the Japanese Version of the Fatigue Assessment Scale. Intern. Med. 2024; in press. [Google Scholar]
- Zung, W.W. A Self-Rating Depression Scale. Arch. Gen. Psychiatry 1965, 12, 63–70. [Google Scholar] [CrossRef]
- Sakurada, Y.; Matsuda, Y.; Motohashi, K.; Hasegawa, T.; Otsuka, Y.; Nakano, Y.; Tokumasu, K.; Yamamoto, K.; Sunada, N.; Honda, H.; et al. Clinical characteristics of female long COVID patients with menstrual symptoms: A retrospective study from a Japanese outpatient clinic. J. Psychosom. Obstet. Gynaecol. 2024, 45, 2305899. [Google Scholar] [CrossRef]
- Jacob, L.; Koyanagi, A.; Smith, L.; Tanislav, C.; Konrad, M.; van der Beck, S.; Kostev, K. Prevalence of, and factors associated with, long-term COVID-19 sick leave in working-age patients followed in general practices in Germany. Int. J. Infect. Dis. 2021, 109, 203–208. [Google Scholar] [CrossRef]
- Carvalho-Schneider, C.; Laurent, E.; Lemaignen, A.; Beaufils, E.; Bourbao-Tournois, C.; Laribi, S.; Flament, T.; Ferreira-Maldent, N.; Bruyere, F.; Stefic, K.; et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021, 27, 258–263. [Google Scholar] [CrossRef]
- O’Regan, E.; Svalgaard, I.B.; Sorensen, A.I.V.; Spiliopoulos, L.; Bager, P.; Nielsen, N.M.; Hansen, J.V.; Koch, A.; Ethelberg, S.; Hviid, A. A hybrid register and questionnaire study of COVID-19 and post-acute sick leave in Denmark. Nat. Commun. 2023, 14, 6266. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef]
- Morioka, S.; Tsuzuki, S.; Maruki, T.; Terada, M.; Miyazato, Y.; Kutsuna, S.; Saito, S.; Shimanishi, Y.; Takahashi, K.; Sanada, M.; et al. Epidemiology of post-COVID conditions beyond 1 year: A cross-sectional study. Public Health 2023, 216, 39–44. [Google Scholar] [CrossRef]
- Ayoubkhani, D.; Zaccardi, F.; Pouwels, K.B.; Walker, A.S.; Houston, D.; Alwan, N.A.; Martin, J.; Khunti, K.; Nafilyan, V. Employment outcomes of people with Long COVID symptoms: Community-based cohort study. Eur. J. Public Health 2024, 34, 489–496. [Google Scholar] [CrossRef]
- Van Herck, M.; Goertz, Y.M.J.; Houben-Wilke, S.; Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Vaes, A.W.; Burtin, C.; Posthuma, R.; Franssen, F.M.E.; et al. Severe Fatigue in Long COVID: Web-Based Quantitative Follow-up Study in Members of Online Long COVID Support Groups. J. Med. Internet Res. 2021, 23, e30274. [Google Scholar] [CrossRef]
- Hosozawa, M.; Hori, M.; Hayama-Terada, M.; Arisa, I.; Muto, Y.; Kitamura, A.; Takayama, Y.; Iso, H. Prevalence and risk factors of post-coronavirus disease 2019 condition among children and adolescents in Japan: A matched case-control study in the general population. Int. J. Infect. Dis. 2024, 143, 107008. [Google Scholar] [CrossRef]
- Molnar, T.; Varnai, R.; Schranz, D.; Zavori, L.; Peterfi, Z.; Sipos, D.; Tokes-Fuzesi, M.; Illes, Z.; Buki, A.; Csecsei, P. Severe Fatigue and Memory Impairment Are Associated with Lower Serum Level of Anti-SARS-CoV-2 Antibodies in Patients with Post-COVID Symptoms. J. Clin. Med. 2021, 10, 4337. [Google Scholar] [CrossRef]

| Changes in Working Situations | Not Changed (n = 250) | Changed (n = 295) | p-Value |
|---|---|---|---|
| Age, median years (IQR) | |||
| 43 (33–49) | 43 (32–51) | 0.938 (a) | |
| Gender, n (%) | |||
| Male | 134 (53.6) | 131 (44.4) | * 0.032 (b) |
| Female | 116 (46.4) | 164 (55.6) | |
| BMI, median (IQR) | |||
| 22.9 (20.6–25.8) | 23 (20.5–27.2) | 0.297 (a) | |
| Smoking habit, n (%) | |||
| Yes | 92 (36.95) | 104 (35.62) | 0.748 (b) |
| No | 157 (63.05) | 188 (64.38) | |
| Unknown | 1 | 3 | |
| Severity in the acute phase, n (%) | |||
| Mild | 215 (86) | 275 (93.2) | ** p < 0.01 (b) |
| Moderate/Severe | 35 (14) | 20 (6.8) | |
| Duration between infection and first visit to the CAC, n (%) | |||
| ≦90 days | 105 (42) | 160 (54.2) | ** p < 0.01 (b) |
| >90 days | 145 (58) | 135 (45.8) | |
| Vaccination history, n (%) | |||
| 0 to 1 time | 93 (38.0) | 100 (34.1) | 0.356 (b) |
| 2 to 5 times | 152 (62.0) | 193 (65.9) | |
| Unknown | 5 | 2 | |
| Changes in income, n (%) | |||
| Not decreased | 162 (66.4) | 105 (36.3) | ** p < 0.01 (b) |
| Decreased | 82 (33.6) | 184 (63.7) | |
| Unknown | 6 | 6 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuda, Y.; Sakurada, Y.; Otsuka, Y.; Tokumasu, K.; Nakano, Y.; Sunada, N.; Honda, H.; Hasegawa, T.; Takase, R.; Omura, D.; et al. Changes in Working Situations of Employed Long COVID Patients: Retrospective Study in Japanese Outpatient Clinic. J. Clin. Med. 2024, 13, 3809. https://doi.org/10.3390/jcm13133809
Matsuda Y, Sakurada Y, Otsuka Y, Tokumasu K, Nakano Y, Sunada N, Honda H, Hasegawa T, Takase R, Omura D, et al. Changes in Working Situations of Employed Long COVID Patients: Retrospective Study in Japanese Outpatient Clinic. Journal of Clinical Medicine. 2024; 13(13):3809. https://doi.org/10.3390/jcm13133809
Chicago/Turabian StyleMatsuda, Yui, Yasue Sakurada, Yuki Otsuka, Kazuki Tokumasu, Yasuhiro Nakano, Naruhiko Sunada, Hiroyuki Honda, Toru Hasegawa, Ryosuke Takase, Daisuke Omura, and et al. 2024. "Changes in Working Situations of Employed Long COVID Patients: Retrospective Study in Japanese Outpatient Clinic" Journal of Clinical Medicine 13, no. 13: 3809. https://doi.org/10.3390/jcm13133809
APA StyleMatsuda, Y., Sakurada, Y., Otsuka, Y., Tokumasu, K., Nakano, Y., Sunada, N., Honda, H., Hasegawa, T., Takase, R., Omura, D., Ueda, K., & Otsuka, F. (2024). Changes in Working Situations of Employed Long COVID Patients: Retrospective Study in Japanese Outpatient Clinic. Journal of Clinical Medicine, 13(13), 3809. https://doi.org/10.3390/jcm13133809







