An Umbrella Review and Updated Meta-Analysis of Imaging Modalities in Occult Scaphoid and Hip and Femoral Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Eligibility Criteria
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction and Quality Assessment
2.5. Stratification of Evidence
2.6. Data Synthesis
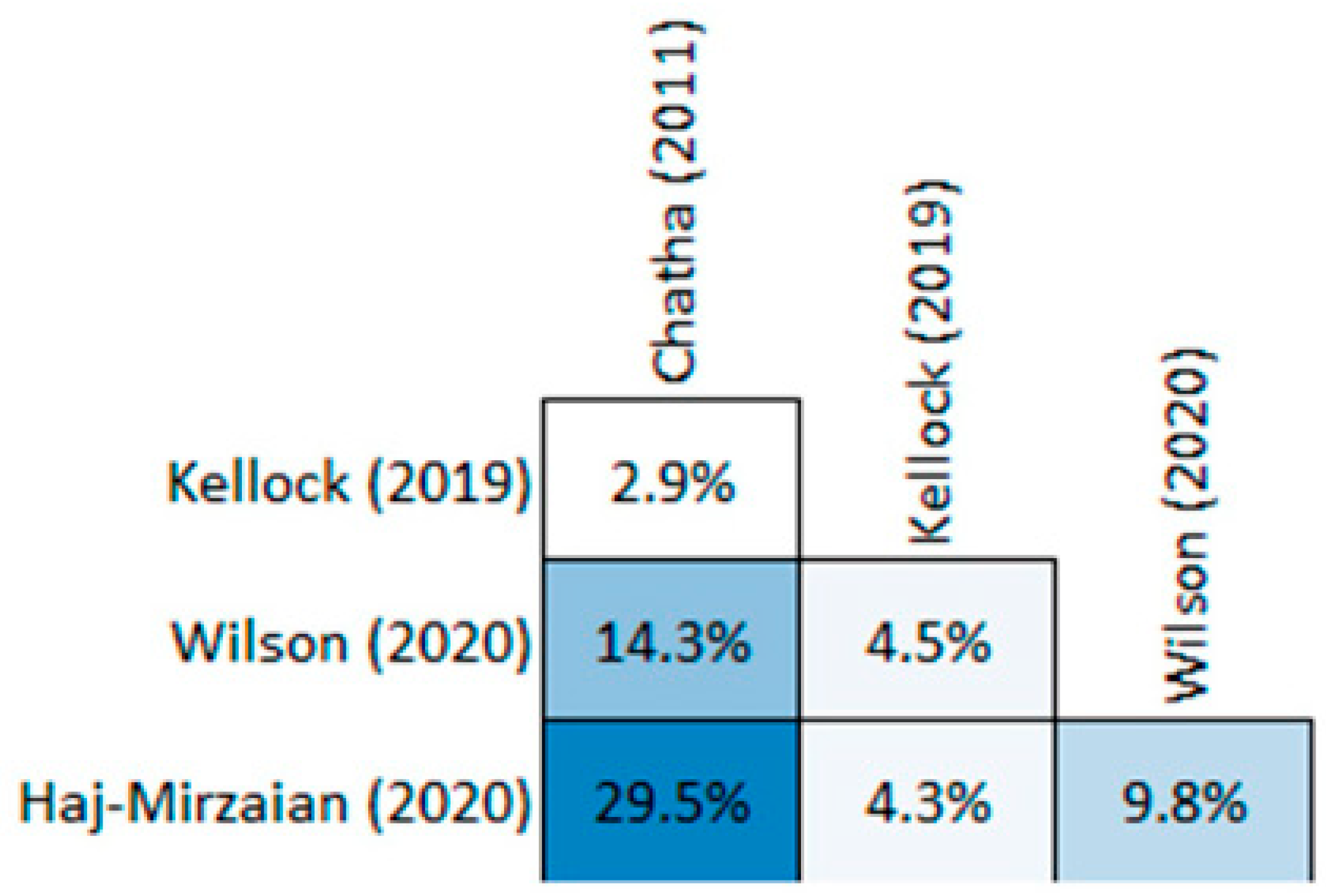
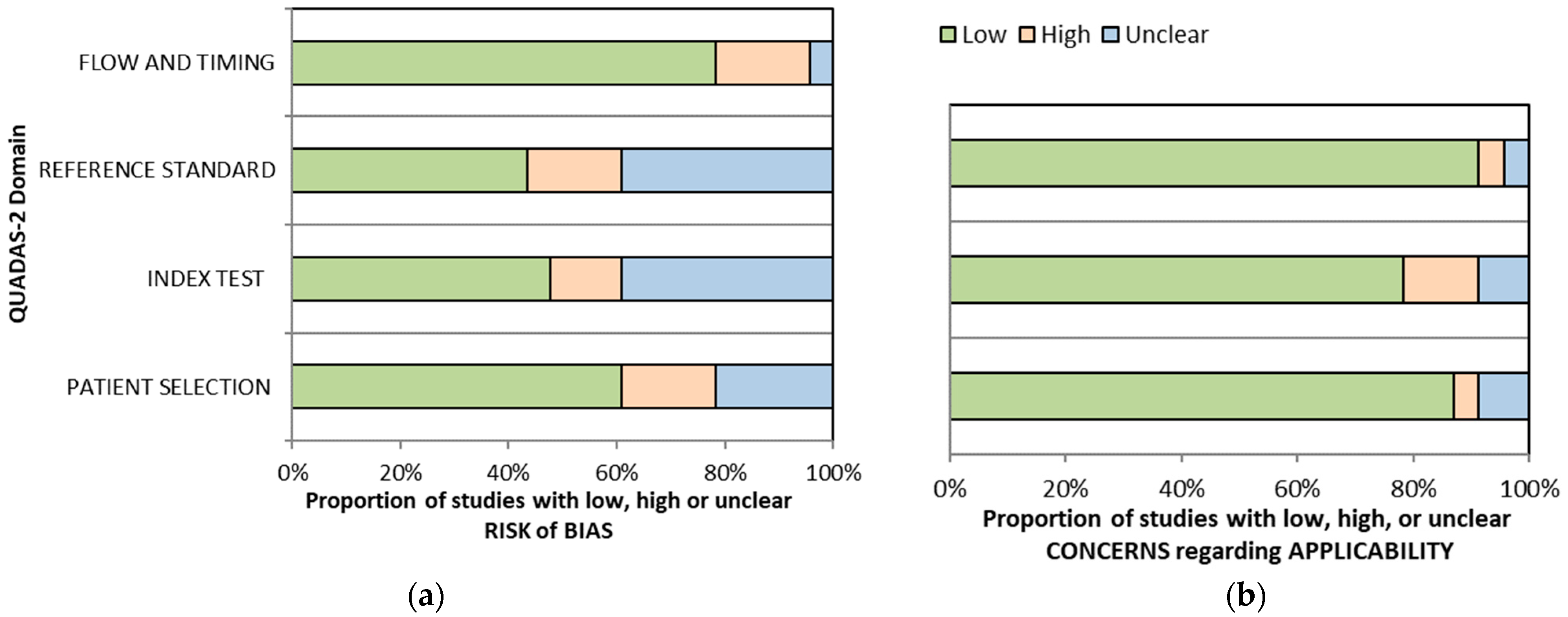
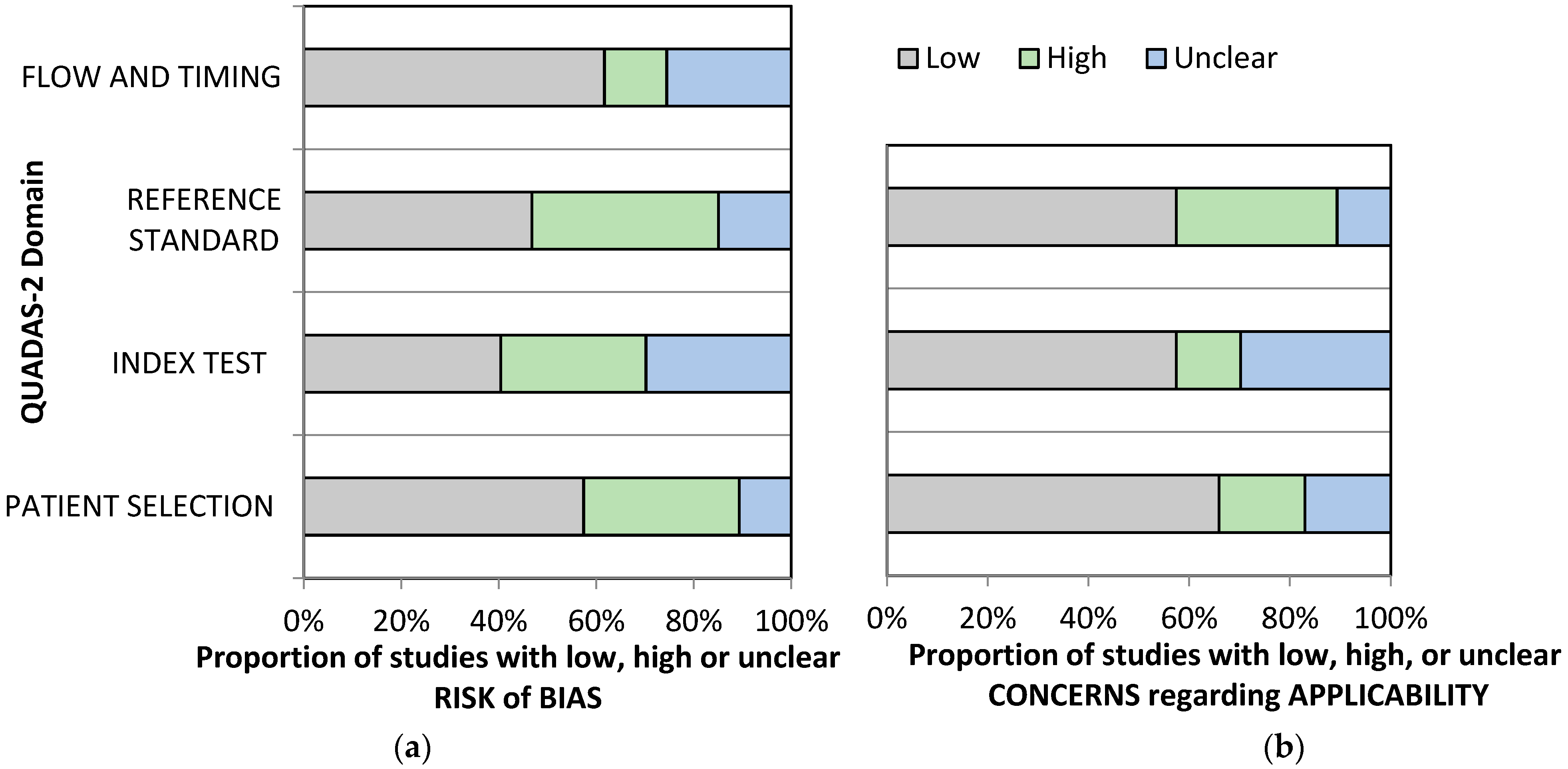
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Study | Risk of Bias | Applicability Concerns | Conclusions | |||||
|---|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Index Test | Reference Standard | ||
| Yildirim (2013) [46] | ☺ | ☺ | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Platon (2011) [47] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Fusetti (2005) [48] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Senall (2004) [49] | ☺ | ☺ | ☹ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Hauger (2002) [50] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Herneth (2001) [51] | ☺ | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Xie (2020) [41] | ☹ | ? | ☺ | ☺ | ? | ? | ☺ | At risk of bias |
| Kitsis (1989) [42] | ☹ | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Thorpe (1996) [43] | ☺ | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Fowler (1998) [44] | ☺ | ? | ☺ | ☺ | ☺ | ? | ☺ | At risk of bias |
| Borel (2017) [63] | ☺ | ? | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Edlund (2016) [64] | ☺ | ☺ | ☺ | ☹ | ☺ | ☺ | ☺ | At risk of bias |
| De Zwart (2012) [52] | ? | ☹ | ☹ | ☺ | ☺ | ☹ | ☺ | At risk of bias |
| Beeres (2008) [56] | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | ☺ | At risk of bias |
| Ilica (2011) [53] | ☹ | ☺ | ☺ | ☹ | ☺ | ☺ | ☺ | At risk of bias |
| Mallee (2011) [54] | ☺ | ? | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Memasadeghi (2006) [55] | ? | ☺ | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Breitenseher (1997) [57] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Tiel-van Buul (1996) [58] | ? | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Nielsen (1983) [62] | ? | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| O’Carroll (1982) [61] | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | At risk of bias |
| Stordahl (1984) [60] | ? | ☺ | ? | ? | ? | ☺ | ? | At risk of bias |
| Tiel-van Buul (1993) [59] | ☺ | ☺ | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Study | Risk of Bias | Applicability Concerns | Conclusions | |||||
|---|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Index Test | Reference Standard | ||
| Deutsch (1989) [89] | ☹ | ☹ | ? | ☺ | ? | ? | ? | At risk of bias |
| Rizzo (1993) [76] | ☹ | ☹ | ? | ☺ | ? | ? | ? | At risk of bias |
| Quinn and McCarthy (1993) [90] | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | ☺ | At risk of bias |
| Evans (1994) [75] | ☺ | ☹ | ? | ☺ | ? | ? | ? | At risk of bias |
| Haramati (1994) [91] | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | At risk of bias |
| Bogost (1995) [92] | ? | ☹ | ☹ | ☺ | ? | ☺ | ☺ | At risk of bias |
| Stiris and Lilleas (1997) [93] | ? | ☹ | ☹ | ☺ | ? | ☺ | ☺ | At risk of bias |
| Rubin (1998) [74] | ? | ? | ? | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Pandey (1998) [94] | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | ☹ | At risk of bias |
| Lim (2002) [95] | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | ☹ | At risk of bias |
| Oka and Monu (2004) [96] | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | ☹ | At risk of bias |
| Galloway (2004) [97] | ☹ | ? | ☺ | ? | ☺ | ☺ | ☺ | At risk of bias |
| Lee (2004) [98] | ☹ | ? | ☺ | ? | ☺ | ☺ | ☺ | At risk of bias |
| Alam (2005) [99] | ☺ | ? | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Frihagen (2005) [100] | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | ☹ | At risk of bias |
| Verbeeten (2005) [101] | ☺ | ? | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Lubovsky (2005) [88] | ☹ | ? | ☺ | ☹ | ☹ | ? | ☺ | At risk of bias |
| Dominguez (2005) [102] | ☹ | ? | ☺ | ☺ | ? | ☺ | ☺ | At risk of bias |
| Chana (2006) [103] | ? | ☹ | ☺ | ? | ☺ | ☺ | ? | At risk of bias |
| Hossain (2007) [104] | ? | ? | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Sankey (2009) [105] | ☺ | ☹ | ☺ | ☺ | ☺ | ☺ | ☺ | At risk of bias |
| Safran (2009) [73] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Szewczyk (2012) [106] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Iwata (2012) [107] | ☺ | ? | ☺ | ☺ | ☺ | ? | ☺ | At risk of bias |
| Dunker (2012) [80] | ☺ | ☺ | ☹ | ☺ | ☺ | ☺ | ☹ | At risk of bias |
| Ohishi (2012) [108] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Geijer (2012) [79] | ☺ | ☺ | ☹ | ? | ☺ | ☺ | ☹ | At risk of bias |
| Gill (2013) [77] | ☹ | ☺ | ☹ | ? | ☹ | ? | ☹ | At risk of bias |
| Heikal (2014) [81] | ☺ | ☺ | ☹ | ☹ | ☺ | ☺ | ☹ | At risk of bias |
| Haubro (2015) [82] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Deleanu (2015) [83] | ☺ | ? | ☹ | ☹ | ☹ | ? | ☹ | At risk of bias |
| Collin (2016) [72] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Rehman (2016) [78] | ☺ | ? | ☹ | ? | ☺ | ? | ☹ | At risk of bias |
| Sadozai (2016) [84] | ☺ | ☺ | ☹ | ? | ☺ | ☺ | ☹ | At risk of bias |
| Thomas (2016) [85] | ☹ | ☺ | ☹ | ? | ☺ | ☺ | ☹ | At risk of bias |
| Lakshmanan (2017) [109] | ☺ | ? | ☺ | ☺ | ☺ | ? | ☺ | At risk of bias |
| Lord (2017) [110] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Mandell (2018) [86] | ☺ | ☺ | ☹ | ☺ | ☺ | ☺ | ☹ | At risk of bias |
| Ross (2019) [111] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Heynen (2019) [87] | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ | Low risk of bias |
| Haims (2020) [66] | ☹ | ? | ? | ☺ | ☹ | ? | ☺ | At risk of bias |
| Lanotte (2019) [65] | ☹ | ☺ | ? | ☹ | ☹ | ☺ | ☺ | At risk of bias |
| Kutaiba (2020) [68] | ☹ | ☺ | ☺ | ? | ? | ? | ☺ | At risk of bias |
| Tsukamoto (2023) [67] | ☹ | ☹ | ? | ? | ? | ? | ? | At risk of bias |
| Reddy (2015) [69] | ☹ | ☺ | ☹ | ? | ☹ | ? | ☹ | At risk of bias |
References
- Ahn, J.M.; El-Khoury, G.Y. Occult Fractures of Extremities. Radiol. Clin. North Am. 2007, 45, 561–579. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.G.; Zhang, J.B.; Kan, S.L.; Wang, X.G. Diagnostic accuracy of imaging modalities for suspected scaphoid fractures: Meta-analysis combined with latent class analysis. J Bone Jt. Surg Br. 2012, 94, 1077–1085. [Google Scholar] [CrossRef]
- Busardò, F.P.; Frati, P.; Santurro, A.; Zaami, S.; Fineschi, V. Errors and malpractice lawsuits in radiology: What the radiologist needs to know. Radiol. Med. 2015, 120, 779–784. [Google Scholar] [CrossRef]
- Beloosesky, Y.; Hershkovitz, A.; Guz, A.; Golan, H.; Salai, M.; Weiss, A. Clinical characteristics and long-term mortality of occult hip fracture elderly patients. Injury 2010, 41, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Yun, B.J.; Hunink, M.G.M.; Prabhakar, A.M.; Heng, M.; Liu, S.W.; Qudsi, R.; Raja, A.S. Diagnostic Imaging Strategies for Occult Hip Fractures: A Decision and Cost-Effectiveness Analysis. Acad. Emerg. Med. 2016, 23, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Bulstra, A.E.J.; van Boxel, M.F.; Crijns, T.J.; Kelly, J.; Obdeijn, M.C.; Kerkhoffs, G.M.M.J.; Doornberg, J.N.; Ring, D.; Jaarsma, R.L. Routine MRI Among Patients with a Suspected Scaphoid Fracture Risks Overdiagnosis. Clin. Orthop. Relat. Res. 2023, 481, 2309–2315. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J. Letter to the Editor: Routine MRI Among Patients with a Suspected Scaphoid Fracture Risks Overdiagnosis. Clin. Orthop. Relat. Res. 2024. [Google Scholar] [CrossRef] [PubMed]
- Torabi, M.; Lenchik, L.; Beaman, F.D.; Wessell, D.E.; Bussell, J.K.; Cassidy, R.C.; Czuczman, G.J.; Demertzis, J.L.; Khurana, B.; Klitzke, A.; et al. ACR Appropriateness Criteria® Acute Hand and Wrist Trauma. J. Am. Coll. Radiol. 2019, 16, S7–S17. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.B.; Lee, K.S.; Chang, E.Y.; Amini, B.; Bussell, J.K.; Gorbachova, T.; Ha, A.S.; Khurana, B.; Klitzke, A.; Mooar, P.A.; et al. ACR Appropriateness Criteria® Acute Hip Pain-Suspected Fracture. J. Am. Coll. Radiol. 2019, 16, S18–S25. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Salameh, J.P.; Bossuyt, P.M.; McGrath, T.A.; Thombs, B.D.; Hyde, C.J.; Macaskill, P.; Takwoingi, Y. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): Explanation, elaboration, and checklist. BMJ 2020, 370, m2632. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Radua, J. Ten simple rules for conducting umbrella reviews. Evid. Based Ment. Health 2018, 21, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Choi, G.J.; Kang, H. Introduction to Umbrella Reviews as a Useful Evidence-Based Practice. J. Lipid Atheroscler. 2023, 12, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Bracchiglione, J.; Meza, N.; Bangdiwala, S.I.; de Guzmán, E.N.; Urrútia, G.; Bonfill, X.; Madrid, E. Graphical Representation of Overlap for OVErviews: GROOVE tool. Res. Synth. Methods 2022, 13, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Nyaga, V.N.; Arbyn, M.; Aerts, M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health 2014, 72, 39. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M. Research Note: In a meta-analysis, the I(2) index does not tell us how much the effect size varies across studies. J. Physiother. 2020, 66, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Yang, L.; Zhao, J.; Wang, L.; Zou, J.; Wang, C.; Fan, X. Comparison of problem-based learning and traditional teaching methods in medical psychology education in China: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0243897. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; Higgins, J.; Sterne, J. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons: Chichester, UK, 2019; pp. 349–374. [Google Scholar]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane handbook for Systematic Reviews of Interventions, 2nd ed.; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons: Chichester, UK, 2019; pp. 241–284. [Google Scholar]
- MedCalc Software Ltd. Diagnostic Test Evaluation Calculator (Version 22.016). 2023. Available online: https://www.medcalc.org/calc/diagnostic_test.php (accessed on 29 December 2023).
- Reitsma, J.B.; Glas, A.S.; Rutjes, A.W.; Scholten, R.J.; Bossuyt, P.M.; Zwinderman, A.H. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J. Clin. Epidemiol. 2005, 58, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Rutter, C.M.; Gatsonis, C.A. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat. Med. 2001, 20, 2865–2884. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H. Overview of the Process of Conducting Meta-analyses of the Diagnostic Test Accuracy. J. Rheum. Dis. 2018, 25, 3–10. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Stengel, D.; Bauwens, K.; Sehouli, J.; Ekkernkamp, A.; Porzsolt, F. A likelihood ratio approach to meta-analysis of diagnostic studies. J. Med. Screen. 2003, 10, 47–51. [Google Scholar] [CrossRef]
- Li, J.; Fine, J.P.; Safdar, N. Prevalence-dependent diagnostic accuracy measures. Stat. Med. 2007, 26, 3258–3273. [Google Scholar] [CrossRef] [PubMed]
- Dwamena, B.; Sylvester, R.; Carlos, R.C. MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. Stata J. 2007, 12, 605–622. [Google Scholar]
- Chatha, H.; Ullah, S.; Cheema, Z. Review article: Magnetic resonance imaging and computed tomography in the diagnosis of occult proximal femur fractures. J. Orthop. Surg. 2011, 19, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Kellock, T.T.; Khurana, B.; Mandell, J.C. Diagnostic Performance of CT for Occult Proximal Femoral Fractures: A Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2019, 213, 1324–1330. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.P.; Nobbee, D.; Murad, M.H.; Dhillon, S.; McInnes, M.D.F.; Katlariwala, P.; Low, G. Diagnostic Accuracy of Limited MRI Protocols for Detecting Radiographically Occult Hip Fractures: A Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2020, 215, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Haj-Mirzaian, A.; Eng, J.; Khorasani, R.; Raja, A.S.; Levin, A.S.; Smith, S.E.; Johnson, P.T.; Demehri, S. Use of Advanced Imaging for Radiographically Occult Hip Fracture in Elderly Patients: A Systematic Review and Meta-Analysis. Radiology 2020, 296, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Mallee, W.H.; Wang, J.; Poolman, R.W.; Kloen, P.; Maas, M.; de Vet, H.C.; Doornberg, J.N. Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspected scaphoid fractures in patients with negative plain radiographs. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Kwee, R.M.; Kwee, T.C. Ultrasound for diagnosing radiographically occult scaphoid fracture. Skelet. Radiol. 2018, 47, 1205–1212. [Google Scholar] [CrossRef]
- Xie, C.; Ather, S.; Mansour, R.; Gleeson, F.; Chowdhury, R. Dual-energy CT in the diagnosis of occult acute scaphoid injury: A direct comparison with MRI. Eur. Radiol. 2021, 31, 3610–3615. [Google Scholar] [CrossRef] [PubMed]
- Kitsis, C.; Taylor, M.; Chandey, J.; Smith, R.; Latham, J.; Turner, S.; Wade, P. Imaging the problem scaphoid. Injury 1998, 29, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, A.P.; Murray, A.D.; Smith, F.W.; Ferguson, J. Clinically suspected scaphoid fracture: A comparison of magnetic resonance imaging and bone scintigraphy. Br. J. Radiol. 1996, 69, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Fowler, C.; Sullivan, B.; Williams, L.A.; McCarthy, G.; Savage, R.; Palmer, A. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skelet. Radiol. 1998, 27, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Hodgkinson, D.W.; Nicholson, D.A.; Stewart, G.; Sheridan, M.; Hughes, P. Scaphoid fracture: A new method of assessment. Clin. Radiol. 1993, 48, 398–401. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, A.; Unlüer, E.E.; Vandenberk, N.; Karagöz, A. The role of bedside ultrasonography for occult scaphoid fractures in the emergency department. Ulus. Travma Acil. Cerrahi. Derg. 2013, 19, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Platon, A.; Poletti, P.-A.; Van Aaken, J.; Fusetti, C.; Della Santa, D.; Beaulieu, J.-Y.; Becker, C.D. Occult fractures of the scaphoid: The role of ultrasonography in the emergency department. Skelet. Radiol. 2011, 40, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Fusetti, C.; A Poletti, P.; Pradel, P.H.; Garavaglia, G.; Platon, A.; Della Santa, D.R.; Bianchi, S. Diagnosis of occult scaphoid fracture with high-spatial-resolution sonography: A prospective blind study. J. Trauma 2005, 59, 677–681. [Google Scholar] [PubMed]
- Senall, J.A.; Failla, J.M.; Bouffard, J.A.; van Holsbeeck, M. Ultrasound for the early diagnosis of clinically suspected scaphoid fracture. J. Hand Surg. Am. 2004, 29, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Hauger, O.; Bonnefoy, O.; Moinard, M.; Bersani, D.; Diard, F. Occult fractures of the waist of the scaphoid: Early diagnosis by high-spatial-resolution sonography. AJR Am. J. Roentgenol. 2002, 178, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Herneth, A.M.; Siegmeth, A.; Bader, T.R.; Ba-Ssalamah, A.; Lechner, G.; Metz, V.M.; Grabenwoeger, F. Scaphoid fractures: Evaluation with high-spatial-resolution US initial results. Radiology 2001, 220, 231–235. [Google Scholar] [CrossRef] [PubMed]
- de Zwart, A.; Rhemrev, S.J.; Kingma, L.M.; Meylaerts, S.A.; Arndt, J.-W.; Schipper, I.B.; Beeres, F.J. Early CT compared with bone scintigraphy in suspected schapoid fractures. Clin. Nucl. Med. 2012, 37, 981. [Google Scholar] [CrossRef]
- Ilica, A.T.; Ozyurek, S.; Kose, O.; Durusu, M. Diagnostic accuracy of multidetector computed tomography for patients with suspected scaphoid fractures and negative radiographic examinations. Jpn. J. Radiol. 2011, 29, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Mallee, W.; Doornberg, J.N.; Ring, D.; van Dijk, C.N.; Maas, M.; Goslings, J.C. Comparison of CT and MRI for diagnosis of suspected scaphoid fractures. J. Bone Jt. Surg. Am. 2011, 93, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Memarsadeghi, M.; Breitenseher, M.J.; Schaefer-Prokop, C.; Weber, M.; Aldrian, S.; Gäbler, C.; Prokop, M. Occult scaphoid fractures: Comparison of multidetector CT and MR imaging--initial experience. Radiology 2006, 240, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Beeres, F.J.; Rhemrev, S.J.; den Hollander, P.; Kingma, L.M.; Meylaerts, S.A.; le Cessie, S.; Bartlema, K.A.; Hamming, J.F.; Hogervorst, M. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J. Bone Jt. Surg. Br. 2008, 90, 1205–1209. [Google Scholar] [CrossRef] [PubMed]
- Breitenseher, M.J.; Metz, V.M.; A Gilula, L.; Gaebler, C.; Kukla, C.; Fleischmann, D.; Imhof, H.; Trattnig, S. Radiographically occult scaphoid fractures: Value of MR imaging in detection. Radiology 1997, 203, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Tiel-van Buul, M.M.; Roolker, W.; Verbeeten, B.W.; Broekhuizen, A.H. Magnetic resonance imaging versus bone scintigraphy in suspected scaphoid fracture. Eur. J. Nucl. Med. 1996, 23, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Tiel-van Buul, M.M.; van Beek, E.J.; Broekhuizen, A.H.; Bakker, A.J.; Bos, K.E.; van Royen, E.A. Radiography and scintigraphy of suspected scaphoid fracture. A long-term study in 160 patients. J. Bone Jt. Surg. Br. 1993, 75, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Stordahl, A.; Schjøth, A.; Woxholt, G.; Fjermeros, H. Bone scanning of fractures of the scaphoid. J. Hand Surg. Br. 1984, 9, 189–190. [Google Scholar] [CrossRef] [PubMed]
- O’Carroll, P.F.; Doyle, J.; Duffy, G. Radiography and scintigraphy in the diagnosis of carpal scaphoid fractures. Ir. J. Med. Sci. 1982, 151, 211–213. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.T.; Hedeboe, J.; Thommesen, P. Bone scintigraphy in the evaluation of fracture of the carpal scaphoid bone. Acta Orthop. Scand. 1983, 54, 303–306. [Google Scholar] [CrossRef]
- Borel, C.; Larbi, A.; Delclaux, S.; Lapegue, F.; Chiavassa-Gandois, H.; Sans, N.; Faruch-Bilfeld, M. Diagnostic value of cone beam computed tomography (CBCT) in occult scaphoid and wrist fractures. Eur. J. Radiol. 2017, 97, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Edlund, R.; Skorpil, M.; Lapidus, G.; Bäcklund, J. Cone-Beam CT in diagnosis of scaphoid fractures. Skelet. Radiol. 2016, 45, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Lanotte, S.J.; Larbi, A.; Michoux, N.; Baron, M.-P.; Hamard, A.; Mourad, C.; Malghem, J.; Cyteval, C.; Berg, B.C.V. Value of CT to detect radiographically occult injuries of the proximal femur in elderly patients after low-energy trauma: Determination of non-inferiority margins of CT in comparison with MRI. Eur. Radiol. 2020, 30, 1113–1126. [Google Scholar] [CrossRef] [PubMed]
- Haims, A.H.; Wang, A.; Yoo, B.J.; Porrino, J. Negative predictive value of CT for occult fractures of the hip and pelvis with imaging follow-up. Emerg Radiol. 2021, 28, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, H.; Kijima, H.; Saito, K.; Saito, H.; Miyakoshi, N. Diagnostic accuracy of ultrasonography for occult femoral neck fracture. J. Clin. Orthop. Trauma 2023, 36, 102087. [Google Scholar] [CrossRef] [PubMed]
- Kutaiba, N.; Lamanna, A.; Malara, F.; Yap, L.P. Use of computed tomography and magnetic resonance imaging for occult neck of femur fractures: A single-centre study. Emerg. Med. Australas. 2020, 32, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Reddy, T.; McLaughlin, P.D.; Mallinson, P.I.; Reagan, A.C.; Munk, P.L.; Nicolaou, S.; Ouellette, H.A. Detection of occult, undisplaced hip fractures with a dual-energy CT algorithm targeted to detection of bone marrow edema. Emerg. Radiol. 2015, 22, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Collin, D.; Geijer, M.; Göthlin, J.H. Computed tomography compared to magnetic resonance imaging in occult or suspect hip fractures. A retrospective study in 44 patients. Eur. Radiol. 2016, 26, 3932–3938. [Google Scholar] [CrossRef]
- Collin, D.; Göthlin, J.H.; Nilsson, M.; Hellström, M.; Geijer, M. Added value of interpreter experience in occult and suspect hip fractures: A retrospective analysis of 254 patients. Emerg. Radiol. 2016, 23, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Collin, D.; Geijer, M.; Göthlin, J.H. Prevalence of exclusively and concomitant pelvic fractures at magnetic resonance imaging of suspect and occult hip fractures. Emerg. Radiol. 2016, 23, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Safran, O.; Goldman, V.; Applbaum, Y.; Milgrom, C.; Bloom, R.; Peyser, A.; Kisselgoff, D. Posttraumatic painful hip: Sonography as a screening test for occult hip fractures. J. Ultrasound Med. 2009, 28, 1447–1452. [Google Scholar] [CrossRef] [PubMed]
- Rubin, S.J.; Marquardt, J.D.; Gottlieb, R.H.; Meyers, S.P.; Totterman, S.M.; O’Mara, R.E. Magnetic resonance imaging: A cost-effective alternative to bone scintigraphy in the evaluation of patients with suspected hip fractures. Skelet. Radiol. 1998, 27, 199–204. [Google Scholar] [CrossRef]
- Evans, P.D.; Wilson, C.; Lyons, K. Comparison of MRI with bone scanning for suspected hip fracture in elderly patients. J. Bone Jt. Surg Br. 1994, 76, 158–159. [Google Scholar] [CrossRef]
- Rizzo, P.F.; Gould, E.S.; Lyden, J.P.; Asnis, S.E. Diagnosis of occult fractures about the hip. Magnetic resonance imaging compared with bone-scanning. JBJS 1993, 75, 395–401. [Google Scholar] [CrossRef]
- Gill, S.K.; Smith, J.; Fox, R.; Chesser, T.J. Investigation of occult hip fractures: The use of CT and MRI. Sci. World J. 2013, 2013, 830319. [Google Scholar] [CrossRef]
- Rehman, H.; Clement, R.G.; Perks, F.; White, T.O. Imaging of occult hip fractures: CT or MRI? Injury 2016, 47, 1297–1301. [Google Scholar] [CrossRef]
- Geijer, M.; Dunker, D.; Collin, D.; Göthlin, J.H. Bone bruise, lipohemarthrosis, and joint effusion in CT of non-displaced hip fracture. Acta Radiol. 2012, 53, 197–202. [Google Scholar] [CrossRef]
- Dunker, D.; Collin, D.; Göthlin, J.H.; Geijer, M. High clinical utility of computed tomography compared to radiography in elderly patients with occult hip fracture after low-energy trauma. Emerg. Radiol. 2012, 19, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Heikal, S.; Riou, P.; Jones, L. The use of computed tomography in identifying radiologically occult hip fractures in the elderly. Ann. R Coll. Surg. Engl. 2014, 96, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Haubro, M.; Stougaard, C.; Torfing, T.; Overgaard, S. Sensitivity and specificity of CT- and MRI-scanning in evaluation of occult fracture of the proximal femur. Injury 2015, 46, 1557–1561. [Google Scholar] [CrossRef]
- Deleanu, B.; Prejbeanu, R.; Tsiridis, E.; Vermesan, D.; Crisan, D.; Haragus, H.; Predescu, V.; Birsasteanu, F. Occult fractures of the proximal femur: Imaging diagnosis and management of 82 cases in a regional trauma center. World J. Emerg. Surg. 2015, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Sadozai, Z.; Davies, R.; Warner, J. The sensitivity of ct scans in diagnosing occult femoral neck fractures. Injury 2016, 47, 2769–2771. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.W.; Williams, H.L.; Carpenter, E.C.; Lyons, K. The validity of investigating occult hip fractures using multidetector CT. Br. J. Radiol. 2016, 89, 20150250. [Google Scholar] [CrossRef] [PubMed]
- Mandell, J.C.; Weaver, M.J.; Khurana, B. Computed tomography for occult fractures of the proximal femur, pelvis, and sacrum in clinical practice: Single institution, dual-site experience. Emerg. Radiol. 2018, 25, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Heynen, B.; Tamigneaux, C.; Pasoglou, V.; Malghem, J.; Vande Berg, B.; Kirchgesner, T. MRI detection of radiographically occult fractures of the hip and pelvis in the elderly: Comparison of T2-weighted Dixon sequence with T1-weighted and STIR sequences. Diagn. Interv. Imaging 2019, 100, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Lubovsky, O.; Liebergall, M.; Mattan, Y.; Weil, Y.; Mosheiff, R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury 2005, 36, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, A.L.; Mink, J.H.; Waxman, A.D. Occult fractures of the proximal femur: MR imaging. Radiology 1989, 170, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.F.; McCarthy, J.L. Prospective evaluation of patients with suspected hip fracture and indeterminate radiographs: Use of T1-weighted MR images. Radiology 1993, 187, 469–471. [Google Scholar] [CrossRef] [PubMed]
- Haramati, N.; Staron, R.B.; Barax, C.; Feldman, F. Magnetic resonance imaging of occult fractures of the proximal femur. Skelet. Radiol. 1994, 23, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Bogost, G.A.; Lizerbram, E.K.; Crues, J.V., III. MR imaging in evaluation of suspected hip fracture: Frequency of unsuspected bone and soft-tissue injury. Radiology 1995, 197, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Stiris, M.G.; Lilleås, F.G. MR findings in cases of suspected impacted fracture of the femoral neck. Acta. Radiol. 1997, 38, 863–866. [Google Scholar] [CrossRef] [PubMed]
- Pandey, R.; McNally, E.; Ali, A.; Bulstrode, C. The role of MRI in the diagnosis of occult hip fractures. Injury 1998, 29, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.B.; Eng, A.K.; Chng, S.M.; Tan, A.G.; Thoo, F.L.; Low, C.O. Limited magnetic resonance imaging (MRI) and the occult hip fracture. Ann. Acad. Med. Singap. 2002, 31, 607–610. [Google Scholar] [PubMed]
- Oka, M.; Monu, J.U. Prevalence and patterns of occult hip fractures and mimics revealed by MRI. AJR Am. J. Roentgenol. 2004, 182, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Galloway, H.R.; Meikle, G.R.; Despois, M. Patterns of injury in patients with radiographic occult fracture of neck of femur as determined by magnetic resonance imaging. Australas. Radiol. 2004, 48, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.P.; Griffith, J.F.; Antonio, G.E.; Tang, N.; Leung, K.S. Early magnetic resonance imaging of radiographically occult osteoporotic fractures of the femoral neck. Hong Kong Med. J. 2004, 10, 271–275. [Google Scholar]
- Alam, A.; Willett, K.; Ostlere, S. The MRI diagnosis and management of incomplete intertrochanteric fractures of the femur. J. Bone Jt. Surg. Br. 2005, 87, 1253–1255. [Google Scholar] [CrossRef] [PubMed]
- Frihagen, F.; Nordsletten, L.; Tariq, R.; Madsen, J.E. MRI diagnosis of occult hip fractures. Acta Orthop. 2005, 76, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Verbeeten, K.M.; Hermann, K.L.; Hasselqvist, M.; Lausten, G.S.; Joergensen, P.; Jensen, C.M.; Thomsen, H.S. The advantages of MRI in the detection of occult hip fractures. Eur. Radiol. 2005, 15, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, S.; Liu, P.; Roberts, C.; Mandell, M.; Richman, P.B. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs--a study of emergency department patients. Acad. Emerg. Med. 2005, 12, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Chana, R.; Noorani, A.; Ashwood, N.; Chatterji, U.; Healy, J.; Baird, P. The role of MRI in the diagnosis of proximal femoral fractures in the elderly. Injury 2006, 37, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.; Barwick, C.; Sinha, A.K.; Andrew, J.G. Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury 2007, 38, 1204–1208. [Google Scholar] [CrossRef] [PubMed]
- Sankey, R.A.; Turner, J.; Lee, J.; Healy, J.; Gibbons, C.E. The use of MRI to detect occult fractures of the proximal femur: A study of 102 consecutive cases over a ten-year period. J. Bone Jt. Surg. Br. 2009, 91, 1064–1068. [Google Scholar] [CrossRef] [PubMed]
- Szewczyk-Bieda, M.; Thomas, N.; Oliver, T.B. Radiographically occult femoral and pelvic fractures are not mutually exclusive: A review of fractures detected by MRI following low-energy trauma. Skelet. Radiol. 2012, 41, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- Iwata, T.; Nozawa, S.; Dohjima, T.; Yamamoto, T.; Ishimaru, D.; Tsugita, M.; Maeda, M.; Shimizu, K. The value of T1-weighted coronal MRI scans in diagnosing occult fracture of the hip. J. Bone Jt. Surg. Br. 2012, 94, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Ohishi, T.; Ito, T.; Suzuki, D.; Banno, T.; Honda, Y. Occult hip and pelvic fractures and accompanying muscle injuries around the hip. Arch. Orthop. Trauma Surg. 2012, 132, 105–112. [Google Scholar] [CrossRef]
- Lakshmanan, P.; Sharma, A.; Lyons, K.; Peehal, J.P. Are occult fractures of the hip and pelvic ring mutually exclusive? J. Bone Jt. Surg. Br. 2007, 89, 1344–1346. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.; Leach, S.; Skiadas, V.T. (Eds.) MRI for suspected hip fracture: How many sequences are enough? ESSR 2017, 2017. [Google Scholar] [CrossRef]
- Ross, A.B.; Chan, B.Y.; Yi, P.H.; Repplinger, M.D.; Vanness, D.J.; Lee, K.S. Diagnostic accuracy of an abbreviated MRI protocol for detecting radiographically occult hip and pelvis fractures in the elderly. Skelet. Radiol. 2019, 48, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Turan, A.; Kose, O.; Aktan, C.; Unal, M.; Acar, B.; Sindel, M. Radiographic analysis of anatomic risk factors for scaphoid fractures; A case-control study. Clin. Imaging 2018, 51, 341–346. [Google Scholar] [CrossRef]
- Wiklund, R.; Toots, A.; Conradsson, M.; Olofsson, B.; Holmberg, H.; Rosendahl, E.; Gustafson, Y.; Littbrand, H. Risk factors for hip fracture in very old people: A population-based study. Osteoporos. Int. 2016, 27, 923–931. [Google Scholar] [CrossRef]
- Oztürk, A.; Ozkan, Y.; Akgöz, S.; Yalçýn, N.; Ozdemir, R.M.; Aykut, S. The risk factors for mortality in elderly patients with hip fractures: Postoperative one-year results. Singap. Med. J. 2010, 51, 137–143. [Google Scholar]
- Wells, M.E.; Nicholson, T.C.; Macias, R.A.; Nesti, L.J.; Dunn, J.C. Incidence of Scaphoid Fractures and Associated Injuries at US Trauma Centers. J. Wrist Surg. 2021, 10, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Trevethan, R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Health 2017, 5, 308890. [Google Scholar] [CrossRef] [PubMed]
- Trikalinos, T.A.; Balion, C.M.; Coleman, C.I.; Griffith, L.; Santaguida, P.L.; Vandermeer, B.; Fu, R. Chapter 8: Meta-analysis of test performance when there is a “gold standard”. J. Gen. Intern. Med. 2012, 27 (Suppl. 1), S56–S66. [Google Scholar] [CrossRef] [PubMed]
- Leeflang, M.M.; Bossuyt, P.M.; Irwig, L. Diagnostic test accuracy may vary with prevalence: Implications for evidence-based diagnosis. J. Clin. Epidemiol. 2009, 62, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Moons, K.G.; Biesheuvel, C.J.; Grobbee, D.E. Test research versus diagnostic research. Clin. Chem. 2004, 50, 473–476. [Google Scholar] [CrossRef]
- Snaith, B.; Walker, A.; Robertshaw, S.; Spencer, N.J.B.; Smith, A.; Harris, M.A. Has NICE guidance changed the management of the suspected scaphoid fracture: A survey of UK practice. Radiography 2021, 27, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Dorsay, T.A.; Major, N.M.; Helms, C.A. Cost-effectiveness of immediate MR imaging versus traditional follow-up for revealing radiographically occult scaphoid fractures. AJR Am. J. Roentgenol. 2001, 177, 1257–1263. [Google Scholar] [CrossRef] [PubMed]
- Rua, T.; Malhotra, B.; Vijayanathan, S.; Hunter, L.; Peacock, J.; Shearer, J.; Goh, V.; McCrone, P.; Gidwani, S. Clinical and cost implications of using immediate MRI in the management of patients with a suspected scaphoid fracture and negative radiographs results from the SMaRT trial. Bone Jt. J. 2019, 101, 984–994. [Google Scholar] [CrossRef]
- Rua, T.; Gidwani, S.; Malhotra, B.; Vijayanathan, S.; Hunter, L.; Peacock, J.; Turville, J.; Razavi, R.; Goh, V.; McCrone, P.; et al. Cost-Effectiveness of Immediate Magnetic Resonance Imaging In the Management of Patients With Suspected Scaphoid Fracture: Results From a Randomized Clinical Trial. Value Health. 2020, 23, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Groves, A.M.; Kayani, I.; Syed, R.; Hutton, B.F.; Bearcroft, P.P.; Dixon, A.K.; Ell, P.J. An international survey of hospital practice in the imaging of acute scaphoid trauma. AJR Am. J. Roentgenol. 2006, 187, 1453–1456. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, A.F.H.; Guevara, S.Z.; Ramírez, S.M.; Rojas, J.C.; Malo, R.G.; Beaujon, L.F.; Ochoa, M.M.; Zarate, J.F.; Niño, M.F.; Aguilar, M.O. What is the role of ultrasonography in the early diagnosis of scaphoid fractures? Eur. J. Radiol. Open. 2021, 8, 100358. [Google Scholar] [CrossRef] [PubMed]
- Muljadi, R.; Koesbandono Octavius, G.S. A systematic review and meta-analysis of diagnostic test accuracy of chest ultrasound in diagnosing pediatric pulmonary tuberculosis. Pediatr. Pulmonol. 2024. [Google Scholar] [CrossRef]
- Bailey, J.; Solan, M.; Moore, E. Cone-beam computed tomography in orthopaedics. Orthop. Trauma 2022, 36, 194–201. [Google Scholar] [CrossRef]
- Compton, N.; Murphy, L.; Lyons, F.; Jones, J.; MacMahon, P.; Cashman, J. Tomosynthesis: A new radiologic technique for rapid diagnosis of scaphoid fractures. Surgeon 2018, 16, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Jacques, T.; Morel, V.; Dartus, J.; Badr, S.; Demondion, X.; Cotten, A. Impact of introducing extremity cone-beam CT in an emergency radiology department: A population-based study. Orthop. Traumatol. Surg. Res. 2021, 107, 102834. [Google Scholar] [CrossRef]
- Hughes, J.; Harris, M.; Snaith, B.; Benn, H. Comparison of scattered entrance skin dose burden in MSCT, CBCT, and X-ray for suspected scaphoid injury: Regional dose measurements in a phantom model. Radiography 2022, 28, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Najaf-Zadeh, A.; Nectoux, E.; Dubos, F.; Happiette, L.; Demondion, X.; Gnansounou, M.; Herbaux, B.; Martinot, A. Prevalence and clinical significance of occult fractures in children with radiograph-negative acute ankle injury. A meta-analysis. Acta Orthop. 2014, 85, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Leopold, S.S. Editor’s Spotlight/Take 5: Routine MRI Among Patients With a Suspected Scaphoid Fracture Risks Overdiagnosis. Clin. Orthop. Relat. Res. 2023, 481, 2303–2308. [Google Scholar] [CrossRef]
- Jarraya, M.; Hayashi, D.; Roemer, F.W.; Crema, M.D.; Diaz, L.; Conlin, J.; Marra, M.D.; Jomaah, N.; Guermazi, A. Radiographically occult and subtle fractures: A pictorial review. Radiol. Res. Pract. 2013, 2013, 370169. [Google Scholar] [CrossRef] [PubMed]
- Ravenel, J.G.; Gordon, L.L.; Pope, T.L.; Reed, C.E. FDG-PET uptake in occult acute pelvic fracture. Skelet. Radiol. 2004, 33, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Gholamrezanezhad, A.; Basques, K.; Batouli, A.; Matcuk, G.; Alavi, A.; Jadvar, H. Clinical Nononcologic Applications of PET/CT and PET/MRI in Musculoskeletal, Orthopedic, and Rheumatologic Imaging. AJR Am. J. Roentgenol. 2018, 210, W245–W263. [Google Scholar] [CrossRef] [PubMed]
- Allainmat, L.; Aubault, M.; Noël, V.; Baulieu, F.; Laulan, J.; Eder, V. Use of hybrid SPECT/CT for diagnosis of radiographic occult fractures of the wrist. Clin. Nucl. Med. 2013, 38, e246–e251. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Objectives | Anatomy | Setting and Context | Number of Databases Sourced and Searched | Date Range of Database Searching | Publication Date Range of Studies Included in the Review that Inform Each Outcome of Interest | Number of Studies | Types of Studies | Total Number of Patients | Country of Origin of Studies | Instruments Used to Appraise the Primary Studies | AMSTAR | Relevant Outcomes Reported | Methods of Synthesis | Publication Bias | Heterogeneity | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chatha (2011) [35] | To determine the role of CT and MRI in diagnosing occult fracture | Femur | N/A | 5 (MEDLINE, EMBASE, CINAHL, Google Scholar, and the Cochrane Library) | 31 October 2009 | 1989 to 2009 | 22 | 15 prospective and 7 retrospective | 996 | N/A | None | Critically low | MRI was an investigation of choice for occult proximal femoral fractures. | Qualitative | N/A | N/A | N/A |
| Kellock (2019) [36] | The diagnostic performance of CT for the detection of occult proximal femoral fracture | Femur | N/A | 3 (Pubmed, Embase, and Web of Science) | 1 December 2018 | 2005 to 2018 | 13 | 1 prospective, the rest are retrospective | 1248 | 5 UK, 1 USA, 1 Israel, 3 Sweden, 1 Romania, 1 Denmark, 1 Canada | QUADAS-2 | High Quality | The estimated summary sensitivity of CT for the detection of nondisplaced hip fracture was 94% (95% credible interval, 83–99%), and the specificity was 100% (95% credible interval, 99–100%) with an AUC of 0.981. | Meta-analysis | Present | Present | High risk of bias in the reference standard, with no single study achieving a good quality |
| Wilson (2019) [37] | Evaluate the diagnostic accuracy of limited MRI protocols for detecting radiographically occult proximal femoral fractures | Femur | All single-centre, academic hospitals | 4 (MEDLINE, Embase, Cochrane Library and Scopus) | 15 November 2019 | 1993–2019 (2012 to 2019 for meta-analysis; 1993 to 2016 for systematic review) | 11 (only five for meta-analysis) | 5 Prospective, 6 Retrospective (1 prospective and 4 retrospective for meta-analysis; 4 prospective and 2 retrospective for systematic review) | 938 | N/A | QUADAS-2 | High Quality | The pooled and weighted summary sensitivity and specificity and the area under the summary ROC curve for limited MRI protocols in detecting radiographically occult hip fractures were 99% (95% CI, 91–100%), 99% (95% CI, 97–100%), and 100% (95% CI, 0.99–1), respectively. | Qualitative and Meta-Analysis | N/A | N/A | All studies included in the meta-analysis were low-risk |
| Haj-Mirzaian (2020) [38] | Determine the diagnostic performance of CT and bone scanning in the detection of occult fractures using MRI as the reference standard | Femoral head, femoral neck, intertrochanteric, or subtrochanteric fractures | N/A | 3 (Pubmed, EMBASE, and Cochrane Library) | 27 September 2018 | 1993 to 2018 | 35 | N/A | 2992 | N/A | ROB | High Quality | CT and bone scanning yielded comparable diagnostic performance in the detection of radiographically occult hip fracture (p = 0.67) with a sensitivity of 79% and 87%, respectively. | Meta-analysis | Present | Present | Low ROB = 27, Moderate ROB = 6, High ROB = 2 |
| Mallee (2015) [39] | identify the most suitable diagnostic imaging strategy for identifying clinically suspected fractures of the scaphoid bone in patients with normal radiographs | Scaphoid | People of all ages who presented at the hospital or clinics within one week of trauma with a clinically suspected scaphoid fracture and negative post-trauma radiographs | 10 (Cochrane Register of Diagnostic Test Accuracy Studies, MEDLINE, EMBASE, the Database of Abstracts of Reviews of EHects, the Cochrane Central Register of Controlled Trials, the NHS Economic Evaluation Database, MEDION, ARIF, Current Controlled Trials, the World Health Organization (WHO) International Clinical Trials Registry Platform) | July 2012 | 1983–2011 | 11 | 9 Prospective, 3 Not Reported | 1041 | 5 Netherlands, 2 Austria, 1 Turkey, 1 Denmark, 1 Ireland, 1 Norway | Not Specified | High Quality | Summary sensitivity and specificity of CT were 0.72 (95% confidence interval (CI) 0.36 to 0.92) and 0.99 (95% CI 0.71 to 1.00); for MRI, these were 0.88 (95% CI 0.64 to 0.97) and 1.00 (95% CI 0.38 to 1.00); for BS, these were 0.99 (95% CI 0.69 to 1.00) and 0.86 (95% CI 0.73 to 0.94). Indirect comparisons suggest that the diagnostic accuracy of BS was significantly higher than CT and MRI, and CT and MRI have comparable diagnostic accuracy. | Meta-analysis | Present | Could not be investigated formally | Five studies were considered “good quality”, and six studies had “moderate quality”. |
| Kwee (2018) [40] | To systematically review the literature on the performance of ultrasound in diagnosing radiographically occult scaphoid fracture. | Scaphoid | N/A | 2 (MEDLINE and Embase databases) | No Limit–8 January 2018 | 2001–2013 | 7 | Not Specified | 314 | 1 Turkey, 2 Switzerland, 1 USA, 1 France, 1 Austria, 1 UK | QUADAS-2 | Critically low | The sensitivity and specificity of ultrasound in diagnosing radiographically occult scaphoid fracture ranged from 77.8% to 100% and from 71.4% to 100% respectively, with pooled estimates of 85.6% (95% CI: 73.9%, 92.6%) and 83.3% (95% CI: 72.0%, 90.6%), respectively. | Meta-analysis | Not Assessed | Cannot be explored | Index Test: Low ROB: 6, High ROB: 1; Reference Standard: High ROB: 2, Unclear: 2; Low ROB: 3; Patient Selection and Flow and Timing: Low ROB 7. |
| Parameter | Scaphoid | Hip and Femur | ||||
|---|---|---|---|---|---|---|
| Ultrasound | CT Scan | MRI | Bone Scan | CT Scan | MRI | |
| No. of studies | 6 | 5 | 8 | 7 | 15 | 29 |
| No. of patients | 270 | 297 | 345 | 586 | 1329 | 1905 |
| Sensitivity (%) | 96 (66–100) | 81 (64–91) | 86 (68–94) | 98 (90–100) | 94 (80–99) | 98 (97–99) |
| Specificity (%) | 94 (66–99) | 98 (86–100) | 98 (28–100) | 80 (44–95) | 99 (96–100) | 99 (98–99) |
| Positive likelihood ratio | 16 (2.2–114.4) | 41.7 (5.5–316.6) | 48.7 (0.4–6437.6) | 4.9 (1.3–17.9) | 82.1 (22.6–298.5) | 69 (41–116.1) |
| Posterior probability (%) assuming a 25% prior probability | 84 | 93 | 95 | 62 | 96 | 96 |
| Negative likelihood ratio | 0.04 (0–0.47) | 0.2 (0.1–0.39) | 0.15 (0.06–0.35) | 0.02 (0–0.16) | 0.06 (0.01–0.22) | 0.02 (0.01–0.03) |
| Posterior probability (%) assuming a 25% prior probability | 1 | 6 | 0.15 | 1 | 2 | 1 |
| Positive predictive value | 0.95 (0.9–1) | 0.82 (0.8–0.84) | 0.86 (0.84–0.88) | 0.97 (0.85–1) | 82.1 (22.6–298.5) | 69 (41–116.1) |
| Negative predictive value | 0.93 (0.88–0.99) | 0.97 (0.95–1) | 0.98 (0.95–1) | 0.81 (0.7–0.92) | 0.06 (0.01–0.22) | 0.02 (0.01–0.03) |
| Diagnostic odds ratio | 387 (17–8879) | 210 (31–1449) | 334 (2–49,601) | 213 (12–3743) | 1425 (171–11851) | 4185 (2009–8720) |
| Area under the curve | 0.99 (0.2–1) | 0.91 (0.17–1) | 0.91 (0.89–0.94) | 0.99 (0.97–0.99) | 1 (0.99–1) | 1 (0.99–1) |
| I2 (%) and p-value | 81 (59–100) and 0.003 | 85 (70–100) and 0.001 | 96 (93–99) and <0.0001 | 1 (0–100) and 0.182 | 92 (83–100) and <0.0001 | 100 (0–100) and 0.5 |
| Publication bias | 0.56 | 0.03 | 0.07 | 0.13 | <0.001 | <0.001 |
| Likelihood ratio scattergram | LUQ; Exclusion and confirmation | RUQ; Confirmation only | RUQ; Confirmation only | RLQ; No exclusion or confirmation | LUQ; Exclusion and confirmation | LUQ; Exclusion and confirmation |
| Stratification of evidence | Weak | Weak | Weak | Weak | Suggestive | Suggestive |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jorisal, P.; Sulay, C.B.H.; Octavius, G.S. An Umbrella Review and Updated Meta-Analysis of Imaging Modalities in Occult Scaphoid and Hip and Femoral Fractures. J. Clin. Med. 2024, 13, 3769. https://doi.org/10.3390/jcm13133769
Jorisal P, Sulay CBH, Octavius GS. An Umbrella Review and Updated Meta-Analysis of Imaging Modalities in Occult Scaphoid and Hip and Femoral Fractures. Journal of Clinical Medicine. 2024; 13(13):3769. https://doi.org/10.3390/jcm13133769
Chicago/Turabian StyleJorisal, Patricia, Callistus Bruce Henfry Sulay, and Gilbert Sterling Octavius. 2024. "An Umbrella Review and Updated Meta-Analysis of Imaging Modalities in Occult Scaphoid and Hip and Femoral Fractures" Journal of Clinical Medicine 13, no. 13: 3769. https://doi.org/10.3390/jcm13133769
APA StyleJorisal, P., Sulay, C. B. H., & Octavius, G. S. (2024). An Umbrella Review and Updated Meta-Analysis of Imaging Modalities in Occult Scaphoid and Hip and Femoral Fractures. Journal of Clinical Medicine, 13(13), 3769. https://doi.org/10.3390/jcm13133769






