The Fate of Mitral Valve Surgery in the Pediatric Age: A 25-Year Single-Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Surgical Strategy
2.3. Mitral Valve Assessment and Data Collection
2.4. Statistical Analysis
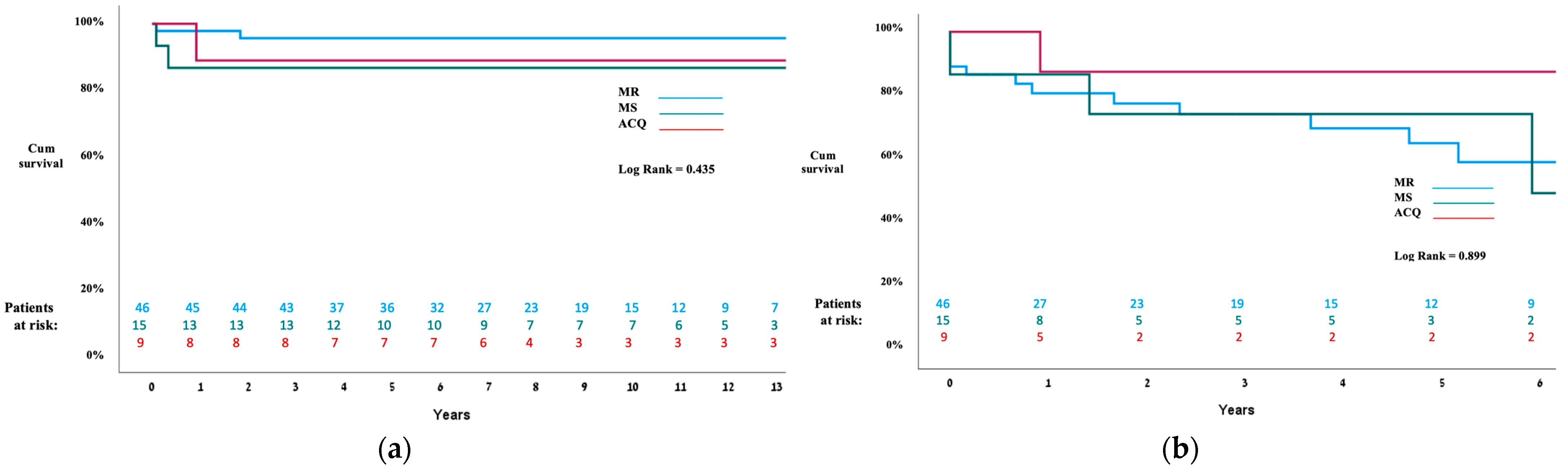
3. Results
3.1. Patients with Congenital MV Disease
3.1.1. Overall
3.1.2. Mitral Regurgitation Group
3.1.3. Mitral Stenosis Group
3.2. Patients with Acquired MV Disease
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carpentier, A. Cardiac valve surgery—The “French correction”. J. Thorac. Cardiovasc. Surg. 1983, 86, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Baird, C.W.; Myers, P.O. Mitral valve operations at a high-volume pediatric heart center: Evolving techniques and improved survival with mitral valve repair versus replacement. Ann. Pediatr. Cardiol. 2012, 5, 13–20. [Google Scholar] [CrossRef]
- Mccarthy, J.; Neligan, M.; Wood, A. Ten years’ experience of an aggressive reparative approach to congenital mitral valve anomalies. Eur. J. Cardiothorac. Surg. 1996, 10, 534–539. [Google Scholar] [CrossRef]
- Caldarone, C.; Raghuveer, G. Long-term survival after mitral valve replacement in children aged < 5 years: A multi- institutional study. Circulation 2001, 104 (Suppl. 1), I143–I147. [Google Scholar]
- Wunderlich, N.C.; Beigel, R. Management of mitral stenosis using 2D and 3D echo-Doppler imaging. JACC Cardiovasc. Imaging 2013, 6, 1191–1205. [Google Scholar] [CrossRef]
- Yakub, M.A.; Krishna Moorthy, P.S. Contemporary long-term outcomes of an aggressive approach to mitral valve repair in children: Is it effective and durable for both congenital and acquired mitral valve lesions? Eur. J. Cardiothorac. Surg. 2016, 49, 553–560. [Google Scholar] [CrossRef] [PubMed]
- David, T.E.; Armstrong, S. Left ventricular function after mitral valve surgery. J. Heart Valve Dis. 1995, 4 (Suppl. 2), S175–S180. [Google Scholar] [PubMed]
- Geoffrion, T.; Pirolli, T. Mitral Valve Surgery in the First Year of Life. Pediatr. Cardiol. 2020, 41, 334–340. [Google Scholar] [CrossRef]
- Günther, T.; Mazzitelli, D. Mitral-valve replacement in children under 6 years of age. Eur. J. Cardio-Thorac. Surg. 2000, 17, 426–430. [Google Scholar] [CrossRef]
- Wood, A.; Healy, D. Mitral valve reconstruction in a pediatric population: Late clinical results and predictors of long-term outcome. J. Thorac. Cardiovasc. Surg. 2005, 130, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Carpentier, A.; Chauvaud, S. Classification of congenital malformations of the mitral valve and their surgical management. In Perspectives in Pediatric Cardiology. Part 3: Pediatric Cardiac Surgery; Crupi, G., Parenzan, L., Anderson, R.G., Eds.; Futura Publishing Company: Mt Kisco, NY, USA, 1990; pp. 97–102. [Google Scholar]
- Zoghbi, W.A.; Enriquez-Sarano, M. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J. Am. Soc. Echocardiogr. 2003, 16, 777–802. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Kohl, T. Echocardiographic evaluation of congenital mitral valve anomalies in children. Am. J. Cardiol. 1995, 76, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Vida, V.L.; Carrozzini, M. Surgical treatment of congenital mitral valve dysplasia. J. Card. Surg. 2016, 31, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Mayr, B.; Vitanova, K. Mitral Valve Repair in Children Below Age 10 Years: Trouble or Success? Ann. Thorac. Surg. 2020, 110, 2082–2087. [Google Scholar] [CrossRef] [PubMed]
- Stellin, G.; Padalino, M.A. Surgical repair of congenital mitral valve malformations in infancy and childhood: A single-center 36-year experience. J. Thorac. Cardiovasc. Surg. 2010, 140, 1238–1244. [Google Scholar] [CrossRef]
- Chauvaud, S.; Fuzellier, J.F. Reconstructive surgery in congenital mitral valve insufficiency (Carpentier’s techniques): Long-term results. J. Thorac. Cardiovasc. Surg. 1998, 115, 84–93. [Google Scholar] [CrossRef]
- Brancaccio, G.; Trezzi, M. Predictors of survival in paediatric mitral valve replacement. Eur. J. Cardio-Thorac. Surg. 2021, 60, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Iddawela, S.; Joseph, P.J.S. Paediatric mitral valve disease—From presentation to management. Eur. J. Pediatr. 2022, 181, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Remenyi, B.; Webb, R. Improved long-term survival for rheumatic mitral valve repair compared to replacement in the young. World J. Pediatr. Congenit. Heart Surg. 2013, 4, 155–164. [Google Scholar] [CrossRef]
- Talwar, S.; Rajesh, M.R. Mitral valve repair in children with rheumatic heart disease. J. Thorac. Cardiovasc. Surg. 2005, 129, 875–879. [Google Scholar] [CrossRef] [PubMed]

| MR (n = 46) | MS (n = 14) | RHD/SBE (n = 9) | |
|---|---|---|---|
| Median age, y (range, days–years) | 2 (20–10.5) | 2 (11–6) | 7.2 (2.1 y–16 y) |
| Median weight, kg (range) | 11.4 (2.6–34.5) | 9.7 (3.1–20) | 22.8 (10.3–60) |
| Median gestational age, weeks (range) | 40 (30–41) | 39 (33–42) | - |
| Median birth weight, gr (range) | 3200 (843–4000) | 3100 (1800–3600) | - |
| Male sex (%) | 17 (36.9%) | 9 (60.0%) | 5 (55.5%) |
| Concomitant Cardiac Anomaly: | |||
| VSD | 12 (26.6%) | 3 (20.0%) | - |
| ASD | 5 (10.8%) | 1 (6.6%) | - |
| Shone’s complex | 2 (4.3%) | 4 (26.6%) | - |
| ALCAPA | 4 (8.6%) | - | - |
| ToF | 1 (2.1%) | - | - |
| TGA | 1 (2.1%) | 1 (6.6%) | - |
| TAPVD | - | 1 (6.6%) | - |
| PAPVD | 1 (2.1%) | - | - |
| Ebstein’s Anomaly | 1 (2.1%) | - | - |
| PLSVC | 1 (2.1%) | - | - |
| Aortic Coarctation | - | 2 (13.3%) | - |
| Aortic valve stenosis | - | 1 (6.6%) | 1 (11.1%) |
| >mod. LV Dysfunction | 7 (15.2%) | 1 (6.6%) | 0% |
| Operative data *: | |||
| Re-sternotomy | 4 (8.8%) | 5 (33.3%) | - |
| CPB time, min | 81 (27–203) | 89 (43–306) | 88 (43–154) |
| XCP time, min | 64 (22–177) | 62 (32–179) | 67 (35–123) |
| Temperature, °C | 34 °C (27–36) | 34 °C (20–36) | 32 °C (30–36) |
| Concomitant Procedure | 6 (13.0%) | 6 (40.0%) | 1 (11.1%) |
| Procedural ECMO | 2 (4.3%) | 0% | 0% |
| Mitral Valve Insufficiency | 46 | ||
|---|---|---|---|
| Type I (normal leaflet motion) | 26 | ||
| Cleft anterior leaflet | 18 | ||
| Annular dilatation | 7 | ||
| Leaflet defect | 1 | ||
| Type II (leaflet prolapse) | 9 | ||
| Type III (restricted leaflet motion) | 11 | ||
| Type A (normal papillary muscle) | 7 | ||
| Type B (abnormal papillary muscle) | 4 | ||
| Mitral Valve Stenosis | 15 | ||
| Type A (normal papillary muscle) | 8 | ||
| Supravalvular ring | 6 | ||
| Leaflet fusion | 2 | ||
| Type B (abnormal papillary muscle) | 7 | ||
| Parachute | 2 | ||
| Papillary muscle abnormality | 5 |
| Mitral Valve Insufficiency | |||
|---|---|---|---|
| Cleft suture | 21 | 45.6% | |
| Posterior commissuroplasty | 23 | 50.0% | |
| Wooler–Kay annuloplasty | 2 | 4.3% | |
| De Vega annuloplasty | 4 | 8.6% | |
| Papillary muscle split | 8 | 17.3% | |
| Annuloplasty ring | 8 | 17.3% | |
| Open ring | 6 | ||
| Closed ring | 2 | ||
| Chords repair | 8 | 17.3% | |
| Mitral Valve Stenosis | |||
| Papillary muscle split | 6 | 54.5% | |
| Repair of chordae | 2 | 18.1% | |
| Resection of supravalvular ring | 6 | 54.5% | |
| Commissurotomy | 4 | 36.3% | |
| Annuloplasty ring | 1 | 9.0% | |
| Open ring | 1 | ||
| Leaflet augmentation | 3 | 27.2% |
| MR (n = 46) | MS (n = 15) | RHD/SBE (n = 9) | |
|---|---|---|---|
| Minor postoperative complications (PNX/AKI1-2/pneumonia/arrhythmia) | 14 (30.4)% | 3 (20.0%) | 0% |
| Major postoperative complications (Revision/ECMO/AKI3/CVA/PPM) | 2 (4.3)% | 6 (40.0%) | 0% |
| Ventilation days (range) | 1 (0–37) | 2 (0–45) | 1 (0–4) |
| PCICU days (range) | 3 (1–40) | 4 (1–445 | 2 (1–6) |
| Hospitalization days (range) | 8 (4–53) | 12 (6–45) | 8 (5–21) |
| In-hospital mortality | 1 (2.1%) | 2 (13.3%) | 0% |
| 1-year mortality | 1(2.1%) | 0% | 1 (11.1%) |
| Long-term mortality | 0% | 0% | 0% |
| Mitral reintervention | 13 (28.8%) | 4 (40%) | 2 (22.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keizman, E.; Tejman-Yarden, S.; Hubara, E.; Illouz, S.; Katz, U.; Mishaly, D.; Serraf, A.E.; Pollak, U. The Fate of Mitral Valve Surgery in the Pediatric Age: A 25-Year Single-Center Experience. J. Clin. Med. 2024, 13, 3761. https://doi.org/10.3390/jcm13133761
Keizman E, Tejman-Yarden S, Hubara E, Illouz S, Katz U, Mishaly D, Serraf AE, Pollak U. The Fate of Mitral Valve Surgery in the Pediatric Age: A 25-Year Single-Center Experience. Journal of Clinical Medicine. 2024; 13(13):3761. https://doi.org/10.3390/jcm13133761
Chicago/Turabian StyleKeizman, Eitan, Shai Tejman-Yarden, Evyatar Hubara, Shay Illouz, Uriel Katz, David Mishaly, Alain E. Serraf, and Uri Pollak. 2024. "The Fate of Mitral Valve Surgery in the Pediatric Age: A 25-Year Single-Center Experience" Journal of Clinical Medicine 13, no. 13: 3761. https://doi.org/10.3390/jcm13133761
APA StyleKeizman, E., Tejman-Yarden, S., Hubara, E., Illouz, S., Katz, U., Mishaly, D., Serraf, A. E., & Pollak, U. (2024). The Fate of Mitral Valve Surgery in the Pediatric Age: A 25-Year Single-Center Experience. Journal of Clinical Medicine, 13(13), 3761. https://doi.org/10.3390/jcm13133761






