Clostridioides difficile Infection in the Elderly: Trend Analysis from 2000 to 2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. The Measurement of Burdens Attributable to Clostridioides difficile in GBD 2019
2.3. Data and Statistical Analysis
3. Results
3.1. Global Mortality and Disability Attributable to Clostridioides difficile in the Elderly
3.2. Mortality and Disability Attributable to Clostridioides difficile in the Elderly, by Sex
3.3. Mortality and Disability Attributable to Clostridioides difficile in the Elderly, by the WHO Region
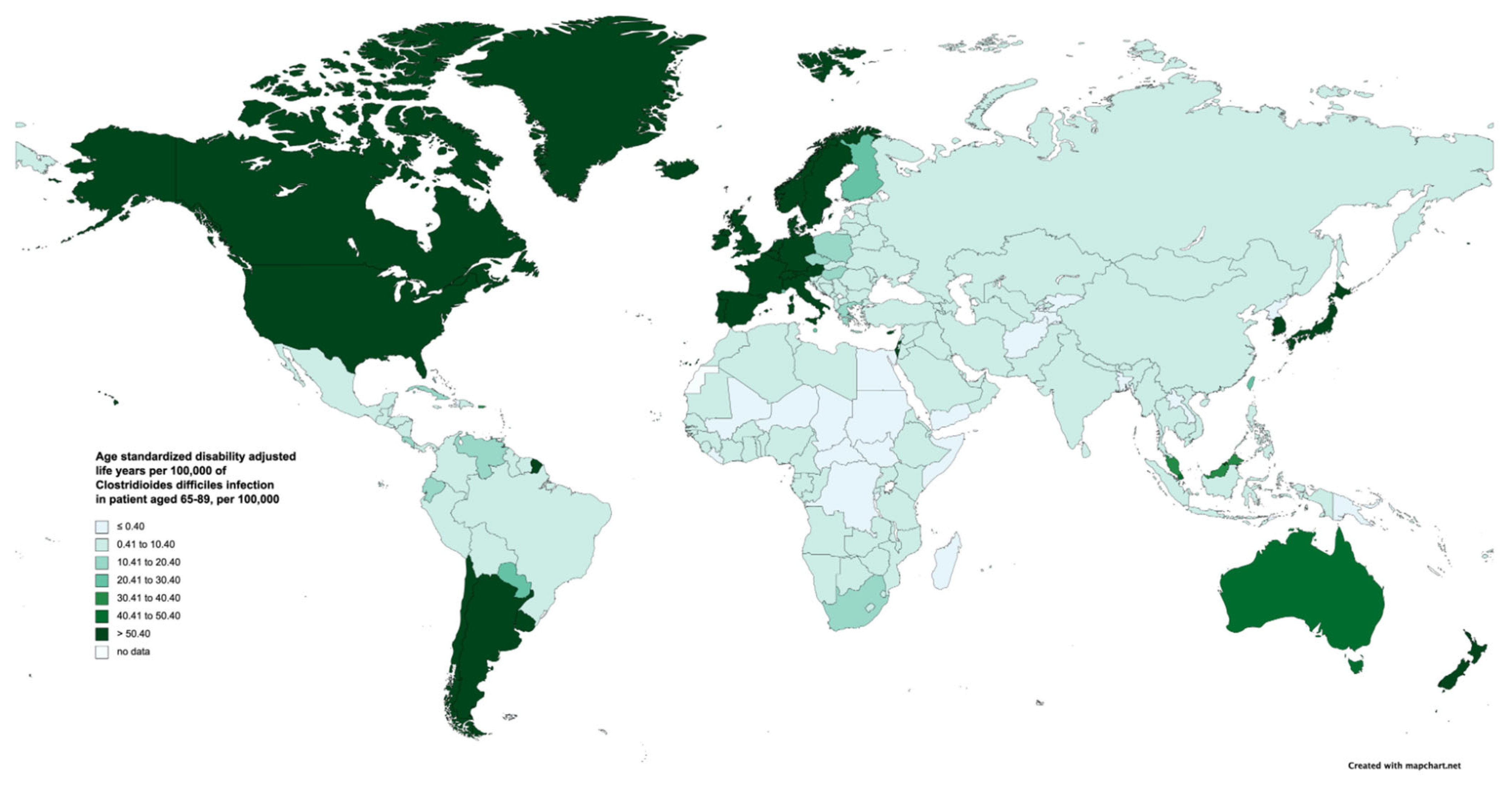
3.4. The Burden of Clostridioides difficile in the Elderly, by Country
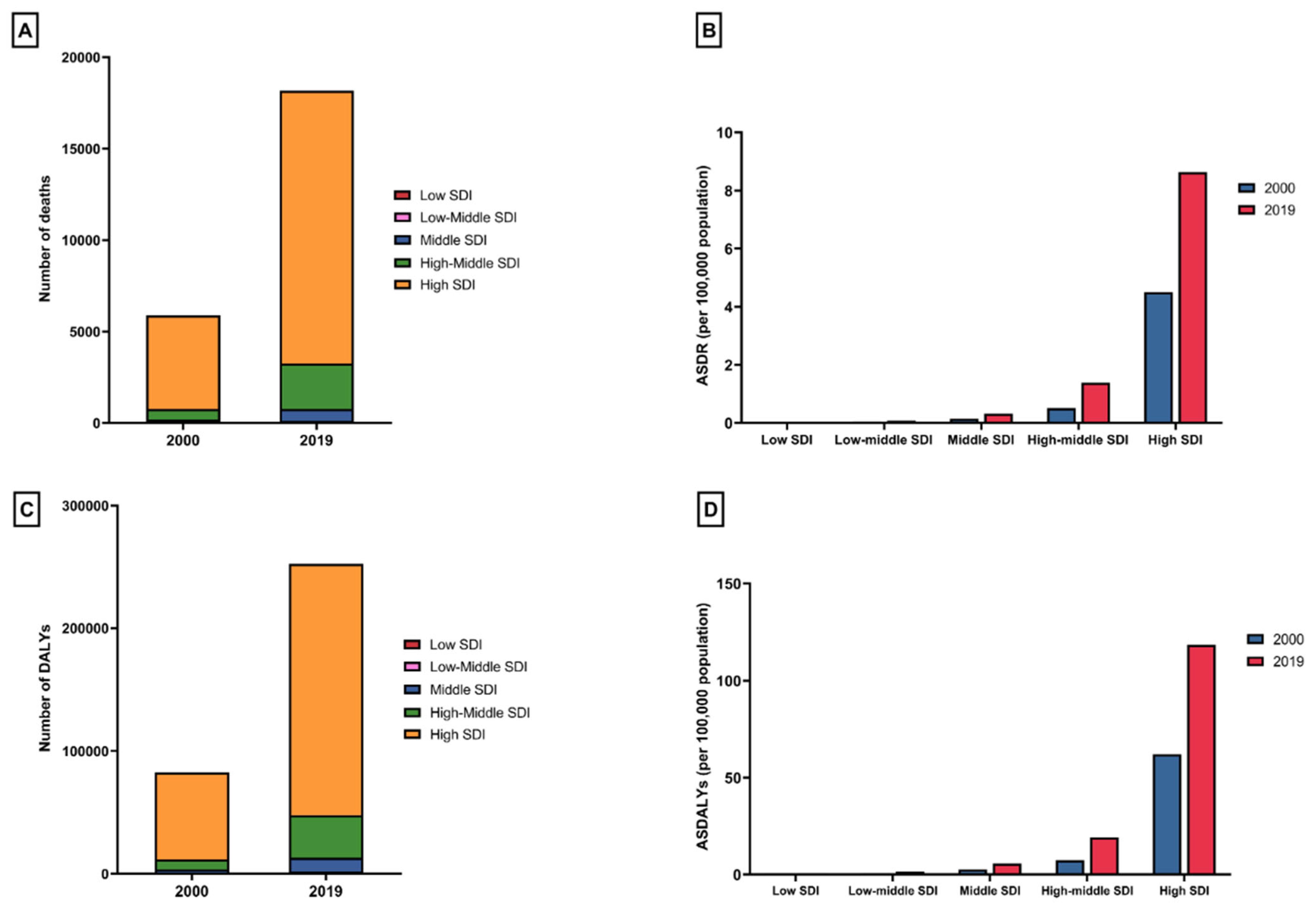
3.5. The Burden of Clostridioides difficile in the Elderly, by Sociodemographic Index
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nanwa, N.; Kendzerska, T.; Krahn, M.; Kwong, J.C.; Daneman, N.; Witteman, W.; Mittmann, N.; Cadarette, S.M.; Rosella, L.; Sander, B. The economic impact of Clostridium difficile infection: A systematic review. Am. J. Gastroenterol. 2015, 110, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Louh, I.K.; Greendyke, W.G.; Hermann, E.A.; Davidson, K.W.; Falzon, L.; Vawdrey, D.K.; Shaffer, J.A.; Calfee, D.P.; Furuya, E.Y.; Ting, H.H. Clostridium difficile Infection in Acute Care Hospitals: Systematic Review and Best Practices for Prevention. Infect. Control Hosp. Epidemiol. 2017, 38, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Voth, E.; Khanna, S. Rise to the Challenge: Master the Management of Clostridioides difficile Infection. Mayo Clin. Proc. 2024, 99, 971–979. [Google Scholar] [CrossRef] [PubMed]
- McGlone, S.M.; Bailey, R.R.; Zimmer, S.M.; Popovich, M.J.; Tian, Y.; Ufberg, P.; Muder, R.R.; Lee, B.Y. The economic burden of Clostridium difficile. Clin. Microbiol. Infect. 2012, 18, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Bignardi, G.E. Risk factors for Clostridium difficile infection. J. Hosp. Infect. 1998, 40, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Loo, V.G.; Bourgault, A.M.; Poirier, L.; Lamothe, F.; Michaud, S.; Turgeon, N.; Toye, B.; Beaudoin, A.; Frost, E.H.; Gilca, R.; et al. Host and pathogen factors for Clostridium difficile infection and colonization. N. Engl. J. Med. 2011, 365, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Jump, R.L. Clostridium difficile infection in older adults. Aging Health 2013, 9, 403–414. [Google Scholar] [CrossRef]
- Asempa, T.E.; Nicolau, D.P. Clostridium difficile infection in the elderly: An update on management. Clin. Interv. Aging 2017, 12, 1799–1809. [Google Scholar] [CrossRef]
- Shin, J.H.; High, K.P.; Warren, C.A. Older Is Not Wiser, Immunologically Speaking: Effect of Aging on Host Response to Clostridium difficile Infections. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 916–922. [Google Scholar] [CrossRef]
- Ofori, E.; Ramai, D.; Dhawan, M.; Mustafa, F.; Gasperino, J.; Reddy, M. Community-acquired Clostridium difficile: Epidemiology, ribotype, risk factors, hospital and intensive care unit outcomes, and current and emerging therapies. J. Hosp. Infect. 2018, 99, 436–442. [Google Scholar] [CrossRef]
- Jump, R.L.; Donskey, C.J. Clostridium difficile in the Long-Term Care Facility: Prevention and Management. Curr. Geriatr. Rep. 2015, 4, 60–69. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Antimicrobial Resistance Collaborators. Global mortality associated with 33 bacterial pathogens in 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022, 400, 2221–2248. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Non-Typhoidal Salmonella Invasive Disease Collaborators. The global burden of non-typhoidal salmonella invasive disease: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect. Dis. 2019, 19, 1312–1324. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Zhong, Y.; Chen, L.; Ge, M.; Yu, M.; Sun, Y.; Shen, L. Global burden and trends of the Entamoeba infection-associated diseases from 1990 to 2019: An observational trend study. Acta Trop. 2023, 240, 106866. [Google Scholar] [CrossRef]
- Inghammar, M.; Svanstrom, H.; Voldstedlund, M.; Melbye, M.; Hviid, A.; Molbak, K.; Pasternak, B. Proton-Pump Inhibitor Use and the Risk of Community-Associated Clostridium difficile Infection. Clin. Infect. Dis. 2021, 72, e1084–e1089. [Google Scholar] [CrossRef]
- D’Silva, K.M.; Mehta, R.; Mitchell, M.; Lee, T.C.; Singhal, V.; Wilson, M.G.; McDonald, E.G. Proton pump inhibitor use and risk for recurrent Clostridioides difficile infection: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 697–703. [Google Scholar] [CrossRef]
- Daniels, B.; Pearson, S.A.; Buckley, N.A.; Bruno, C.; Zoega, H. Long-term use of proton-pump inhibitors: Whole-of-population patterns in Australia 2013–2016. Therap. Adv. Gastroenterol. 2020, 13, 1756284820913743. [Google Scholar] [CrossRef]
- Finn, E.; Andersson, F.L.; Madin-Warburton, M. Burden of Clostridioides difficile infection (CDI)—A systematic review of the epidemiology of primary and recurrent CDI. BMC Infect. Dis. 2021, 21, 456. [Google Scholar] [CrossRef]
- Asensio, A.; Vaque-Rafart, J.; Calbo-Torrecillas, F.; Gestal-Otero, J.J.; Lopez-Fernandez, F.; Trilla-Garcia, A.; Canton, R.; EPINE Working Group. Increasing rates in Clostridium difficile infection (CDI) among hospitalised patients, Spain 1999–2007. Eurosurveillance 2008, 13, 18943. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Vasallo, M.D.; Naval Pellicer, S.; Dominguez-Berjon, M.F.; Cantero Caballero, M.; Asensio, A.; Saravia, G.; Astray-Mochales, J. Age and gender differences in Clostridium difficile-related hospitalization trends in Madrid (Spain) over a 12-year period. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Collins, D.A.; Marcella, S.; Campbell, M.; Riley, T.V. Linkage study of surveillance and hospital admission data to investigate Clostridium difficile infection in hospital patients in Perth, Western Australia. Anaerobe 2022, 74, 102528. [Google Scholar] [CrossRef] [PubMed]
- Schroder, W.; Sommer, H.; Gladstone, B.P.; Foschi, F.; Hellman, J.; Evengard, B.; Tacconelli, E. Gender differences in antibiotic prescribing in the community: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2016, 71, 1800–1806. [Google Scholar] [CrossRef] [PubMed]
- Pham-Duc, P.; Sriparamananthan, K. Exploring gender differences in knowledge and practices related to antibiotic use in Southeast Asia: A scoping review. PLoS ONE 2021, 16, e0259069. [Google Scholar] [CrossRef] [PubMed]
- Dias, S.P.; Brouwer, M.C.; van de Beek, D. Sex and Gender Differences in Bacterial Infections. Infect. Immun. 2022, 90, e0028322. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L. The Global Burden of Disease Study at 30 years. Nat. Med. 2022, 28, 2019–2026. [Google Scholar] [CrossRef]
- Zay Ya, K.; Win, P.T.N.; Bielicki, J.; Lambiris, M.; Fink, G. Association between Antimicrobial Stewardship Programs and Antibiotic Use Globally: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2023, 6, e2253806. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Langford, B.J.; Bonaconsa, C.; Nampoothiri, V.; Charani, E.; Goff, D.A. Global collaborations in antimicrobial stewardship: All hands on deck. Antimicrob. Steward. Healthc. Epidemiol. 2023, 3, e66. [Google Scholar] [CrossRef]
- Kenyon, C.; Manoharan-Basil, S.S. Cultural Drivers of Antibiotic Consumption in High-Income Countries: A Global Ecological Analysis. Microb. Drug Resist. 2020, 26, 1063–1070. [Google Scholar] [CrossRef]
- Vargas Bustamante, A.; Shimoga, V.S. Comparing the Income Elasticity of Health Spending in Middle-Income and High-Income Countries: The Role of Financial Protection. Int. J. Health Policy Manag. 2018, 7, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Danpanichkul, P.; Suparan, K.; Arayakarnkul, S.; Jaroenlapnopparat, A.; Polpichai, N.; Fangsaard, P.; Kongarin, S.; Srisurapanont, K.; Sukphutanan, B.; Wanchaitanawong, W.; et al. Global Epidemiology and Burden of Elderly-Onset Inflammatory Bowel Disease: A Decade in Review. J. Clin. Med. 2023, 12, 5142. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.; Click, B.; Ramos-Rivers, C.; Cheng, D.; Babichenko, D.; Koutroubakis, I.E.; Hashash, J.G.; Schwartz, M.; Swoger, J.; Barrie, A.M., 3rd; et al. Lasting Impact of Clostridium difficile Infection in Inflammatory Bowel Disease: A Propensity Score Matched Analysis. Inflamm. Bowel Dis. 2017, 23, 2180–2188. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, K.; Yadav, D.; Khanna, S. The interplay of Clostridioides difficile infection and inflammatory bowel disease. Therap. Adv. Gastroenterol. 2021, 14, 17562848211020285. [Google Scholar] [CrossRef] [PubMed]
- Roldan, G.A.; Cui, A.X.; Pollock, N.R. Assessing the Burden of Clostridium difficile Infection in Low- and Middle-Income Countries. J. Clin. Microbiol. 2018, 56, e01747-17. [Google Scholar] [CrossRef] [PubMed]
- Forrester, J.D.; Cai, L.Z.; Mbanje, C.; Rinderknecht, T.N.; Wren, S.M. Clostridium difficile infection in low- and middle-human development index countries: A systematic review. Trop. Med. Int. Health 2017, 22, 1223–1232. [Google Scholar] [CrossRef]
- Simango, C.; Uladi, S. Detection of Clostridium difficile diarrhoea in Harare, Zimbabwe. Trans. R. Soc. Trop. Med. Hyg. 2014, 108, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.R.; Fischer, M.; Allegretti, J.R.; LaPlante, K.; Stewart, D.B.; Limketkai, B.N.; Stollman, N.H. ACG Clinical Guidelines: Prevention, Diagnosis, and Treatment of Clostridioides difficile Infections. Am. J. Gastroenterol. 2021, 116, 1124–1147. [Google Scholar] [CrossRef]
- Mejia-Chew, C.; Dubberke, E.R. Clostridium difficile control measures: Current and future methods for prevention. Expert Rev. Anti-Infect. Ther. 2018, 16, 121–131. [Google Scholar] [CrossRef]
- Wang, Y.; Hunt, A.; Danziger, L.; Drwiega, E.N. A Comparison of Currently Available and Investigational Fecal Microbiota Transplant Products for Recurrent Clostridioides difficile Infection. Antibiotics 2024, 13, 436. [Google Scholar] [CrossRef] [PubMed]
- Al Naser, Y.; AlGashami, M.; Aljashaami, L. Clostridioides difficile infection: A changing treatment paradigm. Prz. Gastroenterol. 2024, 19, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Del Prete, R.; Ronga, L.; Addati, G.; Magrone, R.; Abbasciano, A.; Decimo, M.; Miragliotta, G. Clostridium difficile. A review on an emerging infection. Clin. Ther. 2019, 170, e41–e47. [Google Scholar] [CrossRef]
- Sheitoyan-Pesant, C.; Abou Chakra, C.N.; Pepin, J.; Marcil-Heguy, A.; Nault, V.; Valiquette, L. Clinical and Healthcare Burden of Multiple Recurrences of Clostridium difficile Infection. Clin. Infect. Dis. 2016, 62, 574–580. [Google Scholar] [CrossRef]
- Escudero-Sanchez, R.; Valencia-Alijo, A.; Cuellar Tovar, S.; Merino-de Lucas, E.; Garcia Fernandez, S.; Gutierrez-Rojas, A.; Ramos-Martinez, A.; Salavert Lleti, M.; Castro Hernandez, I.; Giner, L.; et al. Real-life experience with fidaxomicin in Clostridioides difficile infection: A multicentre cohort study on 244 episodes. Infection 2021, 49, 475–482. [Google Scholar] [CrossRef]
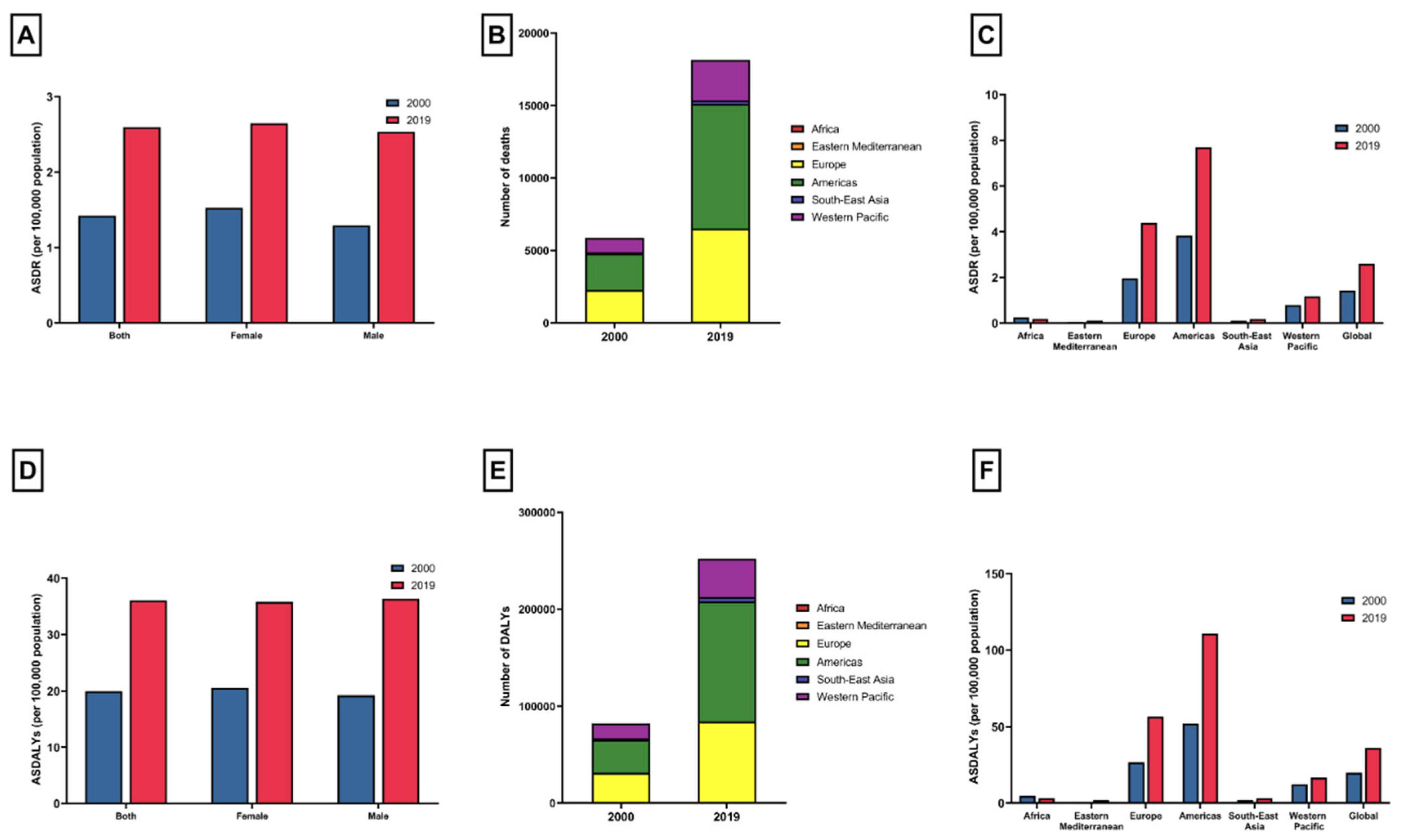
| 2000 Deaths (95% UI) | 2000 ASDR, per 100,000 People (95% UI) | 2019 Deaths (95% UI) | 2019 ASDR, per 100,000 People (95% UI) | Annual Percentage Change (95% CI) | p | |
|---|---|---|---|---|---|---|
| Overall | 5891.39 (5108.27 to 6652.06) | 1.42 (1.23 to 1.61) | 18,180.85 (15,420.75 to 20,742.48) | 2.59 (2.2 to 2.96) | 3.25 (2.88 to 3.62) | <0.001 |
| Sex | ||||||
| Female | 3507.55 (3033.48 to 3947.63) | 1.53 (1.32 to 1.72) | 10,060.78 (8443.83 to 11,546.96) | 2.65 (2.22 to 3.04) | 2.96 (2.59 to 3.33) | <0.001 |
| Male | 2383.84 (2074.77 to 2709.68) | 1.29 (1.12 to 1.47) | 8120.07 (6911.8 to 9307.49) | 2.53 (2.16 to 2.9) | 3.66 (3.28 to 4.05) | <0.001 |
| Region | ||||||
| Africa | 51.71 (33.65 to 79.19) | 0.25 (0.16 to 0.38) | 62.06 (38.58 to 95.81) | 0.18 (0.11 to 0.28) | −1.59 (−1.77 to −1.41) | <0.001 |
| Eastern Mediterranean | 8.39 (4.12 to 15.73) | 0.05 (0.02 to 0.09) | 32.09 (17.58 to 54.93) | 0.11 (0.06 to 0.19) | 4.44 (4.13 to 4.75) | <0.001 |
| Europe | 2211.44 (1856.81 to 2542.51) | 1.95 (1.64 to 2.25) | 6420.59 (5289.96 to 7462.52) | 4.38 (3.61 to 5.09) | 4.37 (4.05 to 4.7) | <0.001 |
| Americas | 2520.24 (2312.7 to 2665.25) | 3.83 (3.52 to 4.05) | 8598.58 (7597.19 to 9493.99) | 7.7 (6.8 to 8.5) | 3.81 (3.42 to 4.2) | <0.001 |
| Southeast Asia | 72.12 (41.36 to 120.81) | 0.11 (0.06 to 0.18) | 234.27 (130.82 to 380.38) | 0.17 (0.1 to 0.28) | 2.58 (2.41 to 2.74) | <0.001 |
| Western Pacific | 1012.59 (735.22 to 1297.86) | 0.79 (0.57 to 1.01) | 2802.49 (2061.73 to 3563.12) | 1.17 (0.86 to 1.48) | 2.07 (1.82 to 2.33) | <0.001 |
| Sociodemographic Index | ||||||
| Low SDI | 8.19 (4.35 to 15.29) | 0.04 (0.02 to 0.07) | 16.26 (9.06 to 29.85) | 0.04 (0.02 to 0.08) | 0.66 (0.21 to 1.1) | 0.004 |
| Low Middle SDI | 27.18 (14.45 to 50.01) | 0.05 (0.02 to 0.09) | 92.52 (48 to 163.57) | 0.09 (0.04 to 0.15) | 3.24 (2.89 to 3.6) | <0.001 |
| Middle SDI | 150.88 (88.15 to 247.36) | 0.14 (0.08 to 0.23) | 651.04 (369.85 to 1061.71) | 0.32 (0.18 to 0.53) | 4.41 (4.04 to 4.79) | <0.001 |
| Middle High SDI | 578.78 (465.29 to 717.31) | 0.51 (0.41 to 0.63) | 2495.86 (1980.53 to 3054.86) | 1.39 (1.1 to 1.7) | 5.42 (4.91 to 5.92) | <0.001 |
| High SDI | 5124.06 (4510.76 to 5698.47) | 4.5 (3.96 to 5.01) | 14,918.3 (12,903.63 to 16,784.59) | 8.63 (7.47 to 9.71) | 3.58 (3.18 to 3.98) | <0.001 |
| 2000 DALYs (95% UI) | 2000 ASDALYs, per 100,000 People (95% UI) | 2019 DALYs (95% UI) | 2019 ASDALYs, per 100,000 People (95% UI) | Annual Percentage Change (95% CI) | p | |
|---|---|---|---|---|---|---|
| Overall | 82,795.67 (72,513.27 to 93,090.47) | 19.98 (17.5 to 22.46) | 252,708.6 (219,561.1 to 285,092.27) | 36.07 (31.34 to 40.69) | 3.14 (2.84 to 3.44) | <0.001 |
| Sex | ||||||
| Female | 47,260.2 (41,445.26 to 52,788.1) | 20.56 (18.03 to 22.96) | 136,162.99 (116,981.15 to 154,642.68) | 35.82 (30.77 to 40.68) | 2.93 (2.62 to 3.24) | <0.001 |
| Male | 35,535.47 (30,812.78 to 40,303.54) | 19.26 (16.7 to 21.84) | 116,545.61 (101,137.72 to 132,318.84) | 36.37 (31.56 to 41.29) | 3.45 (3.1 to 3.8) | <0.001 |
| Region | ||||||
| Africa | 960.13 (634.31 to 1423.19) | 4.62 (3.05 to 6.85) | 1142.78 (724.44 to 1731.5) | 3.37 (2.13 to 5.1) | −1.63 (−1.81 to −1.46) | <0.001 |
| Eastern Mediterranean | 152.63 (74.48 to 283.74) | 0.88 (0.43 to 1.64) | 547.14 (300.03 to 937.02) | 1.86 (1.02 to 3.19) | 4.13 (3.84 to 4.42) | <0.001 |
| Europe | 30,311.15 (25,936.21 to 34,360.54) | 26.78 (22.91 to 30.35) | 82,743.26 (69,974.17 to 94,324.98) | 56.48 (47.77 to 64.39) | 4 (3.51 to 4.5) | <0.001 |
| Americas | 34,196.51 (31,716.82 to 35,949.11) | 52 (48.23 to 54.67) | 123,586.49 (111,590.06 to 134,186.45) | 110.69 (99.94 to 120.18) | 4.07 (3.57 to 4.57) | <0.001 |
| Southeast Asia | 1357.82 (787.34 to 2225.35) | 2 (1.16 to 3.28) | 4194.45 (2335.79 to 6824.43) | 3.08 (1.71 to 5.01) | 2.32 (2.1 to 2.53) | <0.001 |
| Western Pacific | 15,568.35 (11,471.66 to 19,746.6) | 12.16 (8.96 to 15.42) | 40,010.73 (29,982.4 to 50,849.22) | 16.64 (12.47 to 21.15) | 1.66 (1.37 to 1.94) | <0.001 |
| Sociodemographic Index | ||||||
| Low SDI | 150.52 (77.75 to 273.91) | 0.7 (0.36 to 1.28) | 290.23 (155.77 to 536.32) | 0.78 (0.42 to 1.44) | 0.51 (0.19 to 0.84) | 0.002 |
| Low Middle SDI | 498.94 (263.68 to 909.2) | 0.85 (0.45 to 1.56) | 1630.46 (843.11 to 2862.67) | 1.5 (0.78 to 2.64) | 3.02 (2.68 to 3.36) | <0.001 |
| Middle SDI | 2779.74 (1647.31 to 4471.72) | 2.62 (1.55 to 4.22) | 11,369.99 (6494.79 to 18,363.91) | 5.63 (3.22 to 9.09) | 4.11 (3.74 to 4.48) | <0.001 |
| Middle High SDI | 8592.09 (6880.79 to 10,745.73) | 7.5 (6.01 to 9.38) | 34,559.29 (27,686 to 42,248.11) | 19.22 (15.4 to 23.49) | 5.01 (4.56 to 5.46) | <0.001 |
| High SDI | 70,741.48 (63,046.81 to 77,544.13) | 62.17 (55.41 to 68.15) | 204,764.75 (181,755.23 to 224,788.6) | 118.48 (105.17 to 130.07) | 3.52 (3.18 to 3.87) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danpanichkul, P.; Duangsonk, K.; Uawithya, E.; Kongarin, S.; Simadibrata, D.M.; Polpichai, N.; Suenghataiphorn, T.; Wattanachayakul, P.; Pang, Y.; Sukphutanan, B.; et al. Clostridioides difficile Infection in the Elderly: Trend Analysis from 2000 to 2019. J. Clin. Med. 2024, 13, 3740. https://doi.org/10.3390/jcm13133740
Danpanichkul P, Duangsonk K, Uawithya E, Kongarin S, Simadibrata DM, Polpichai N, Suenghataiphorn T, Wattanachayakul P, Pang Y, Sukphutanan B, et al. Clostridioides difficile Infection in the Elderly: Trend Analysis from 2000 to 2019. Journal of Clinical Medicine. 2024; 13(13):3740. https://doi.org/10.3390/jcm13133740
Chicago/Turabian StyleDanpanichkul, Pojsakorn, Kwanjit Duangsonk, Ekdanai Uawithya, Siwanart Kongarin, Daniel M. Simadibrata, Natchaya Polpichai, Thanathip Suenghataiphorn, Phuuwadith Wattanachayakul, Yanfang Pang, Banthoon Sukphutanan, and et al. 2024. "Clostridioides difficile Infection in the Elderly: Trend Analysis from 2000 to 2019" Journal of Clinical Medicine 13, no. 13: 3740. https://doi.org/10.3390/jcm13133740
APA StyleDanpanichkul, P., Duangsonk, K., Uawithya, E., Kongarin, S., Simadibrata, D. M., Polpichai, N., Suenghataiphorn, T., Wattanachayakul, P., Pang, Y., Sukphutanan, B., Kaewdech, A., Panpradist, N., Chaiyakunapruk, N., Pupaibool, J., & Wijarnpreecha, K. (2024). Clostridioides difficile Infection in the Elderly: Trend Analysis from 2000 to 2019. Journal of Clinical Medicine, 13(13), 3740. https://doi.org/10.3390/jcm13133740








