Oral Health Status and Treatment Needs Based on Artificial Intelligence (AI) Dental Panoramic Radiograph (DPR) Analysis: A Cross-Sectional Study
Abstract
1. Introduction
Background
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Variables
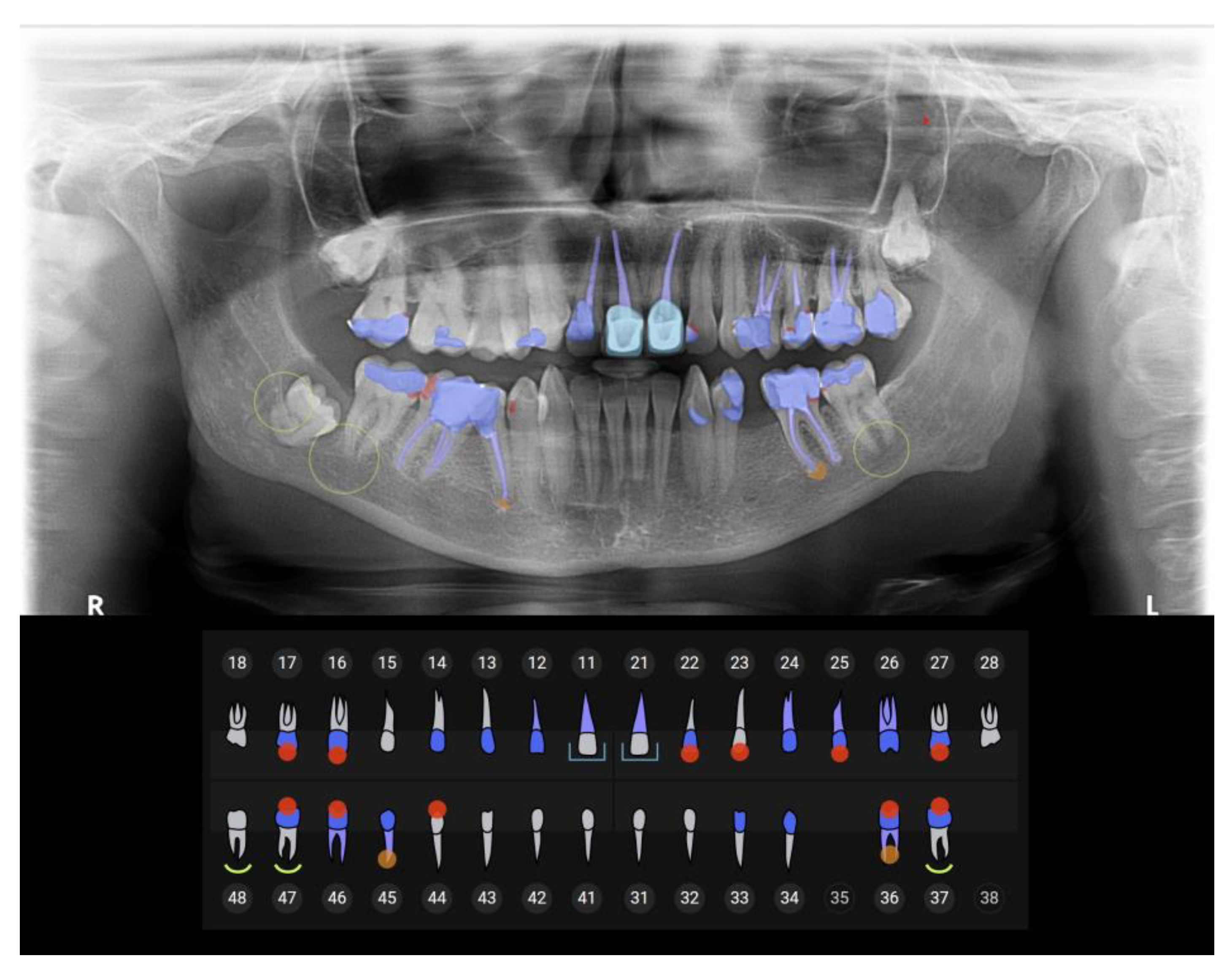
2.5. Data Sources/Measurement
2.6. Bias
2.7. Study Size
2.8. Quantitative Variables
2.9. Statistical Methods
3. Results
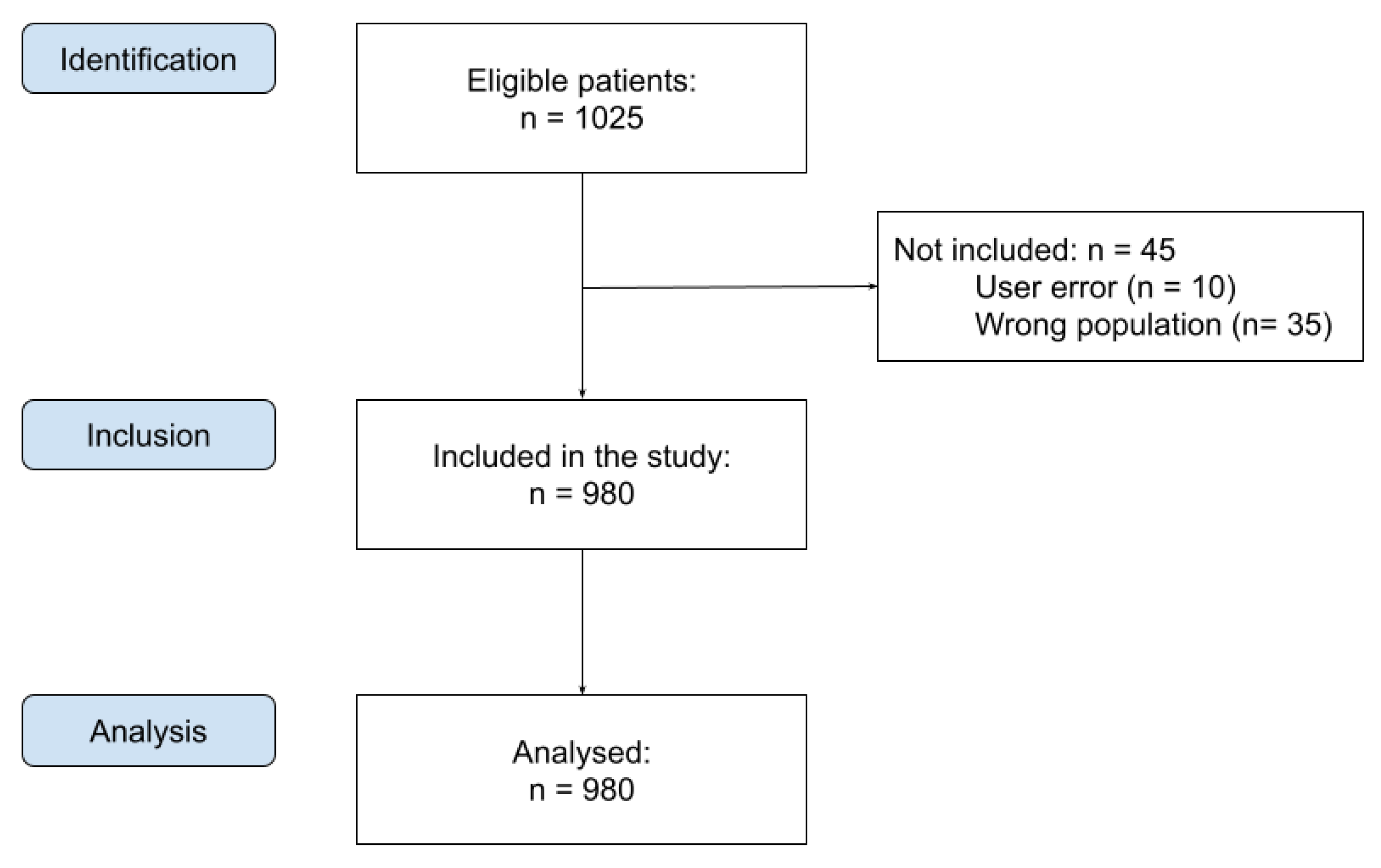
3.1. Participants
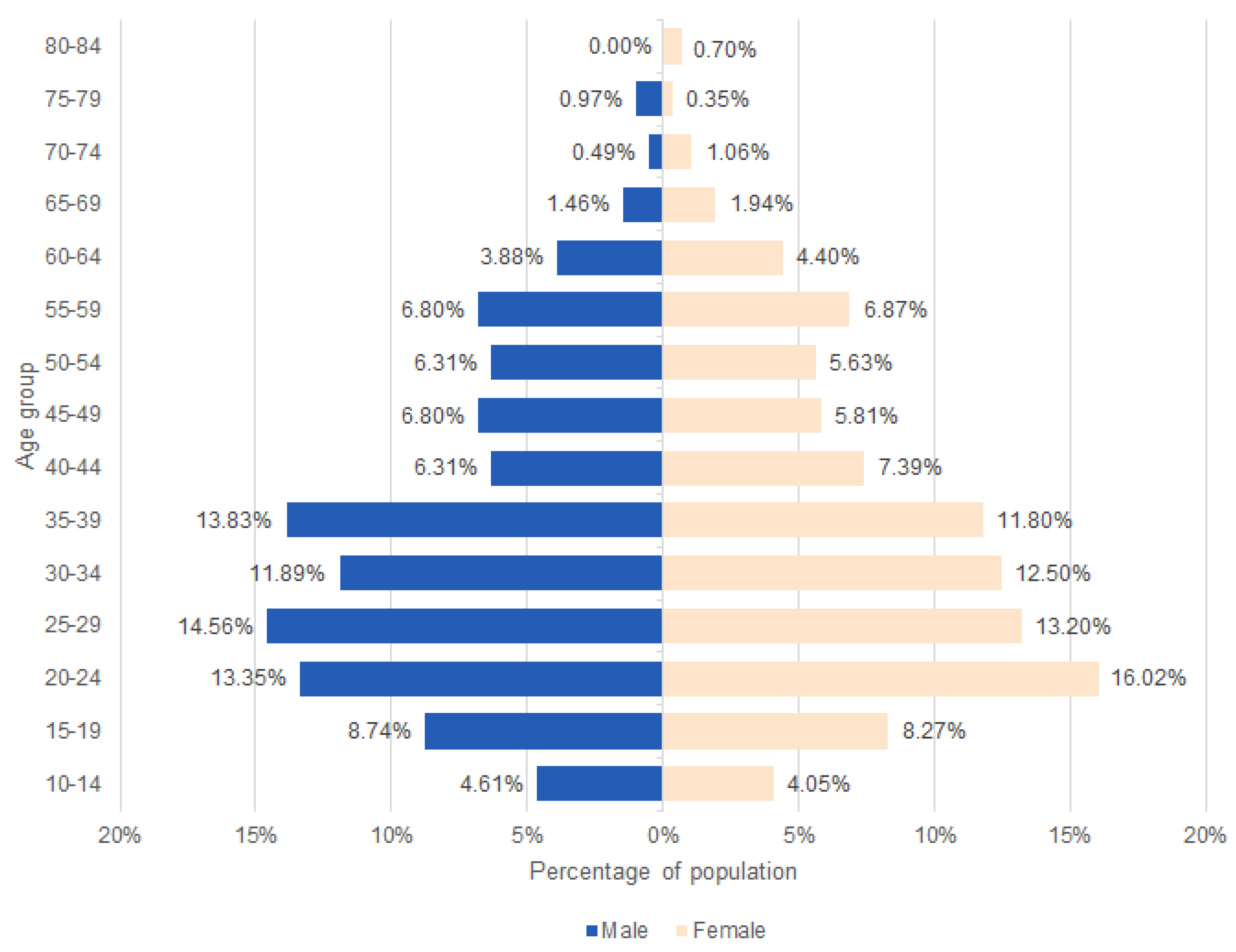
3.2. Descriptive Data
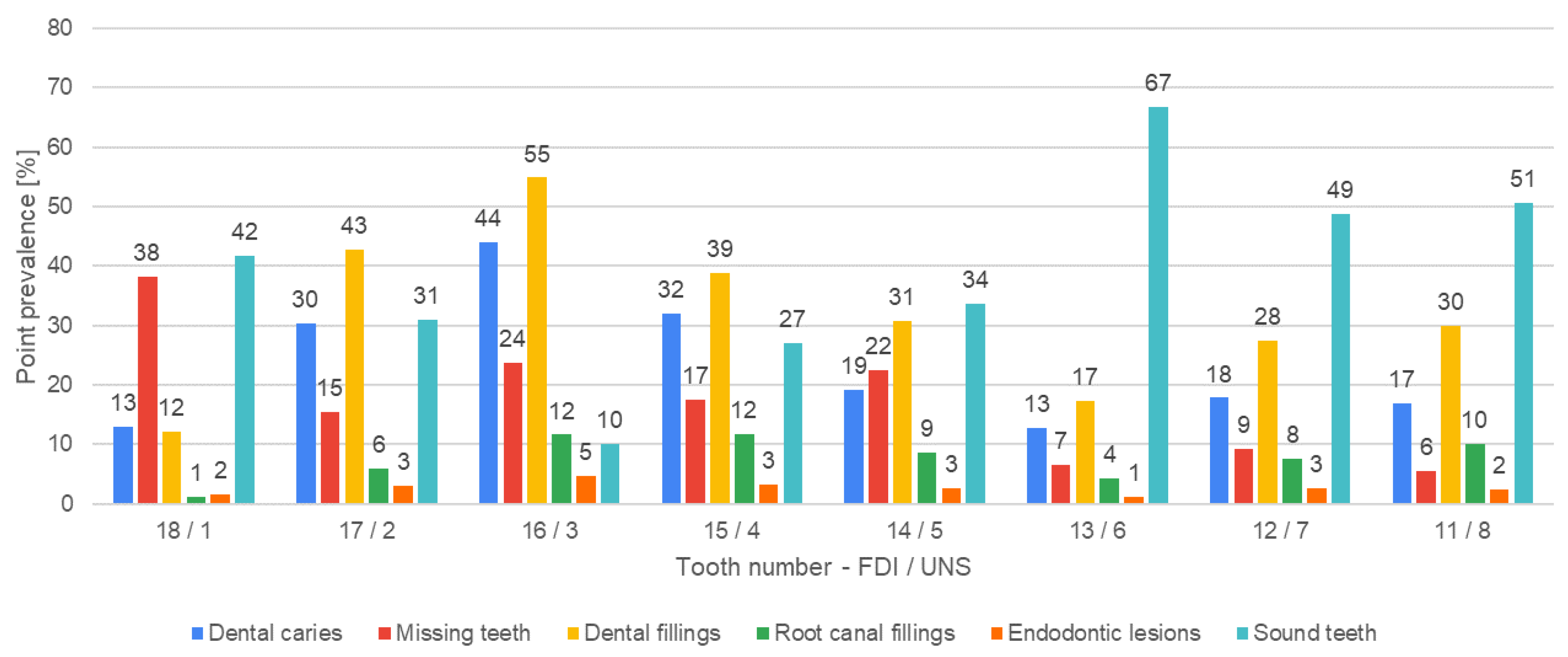
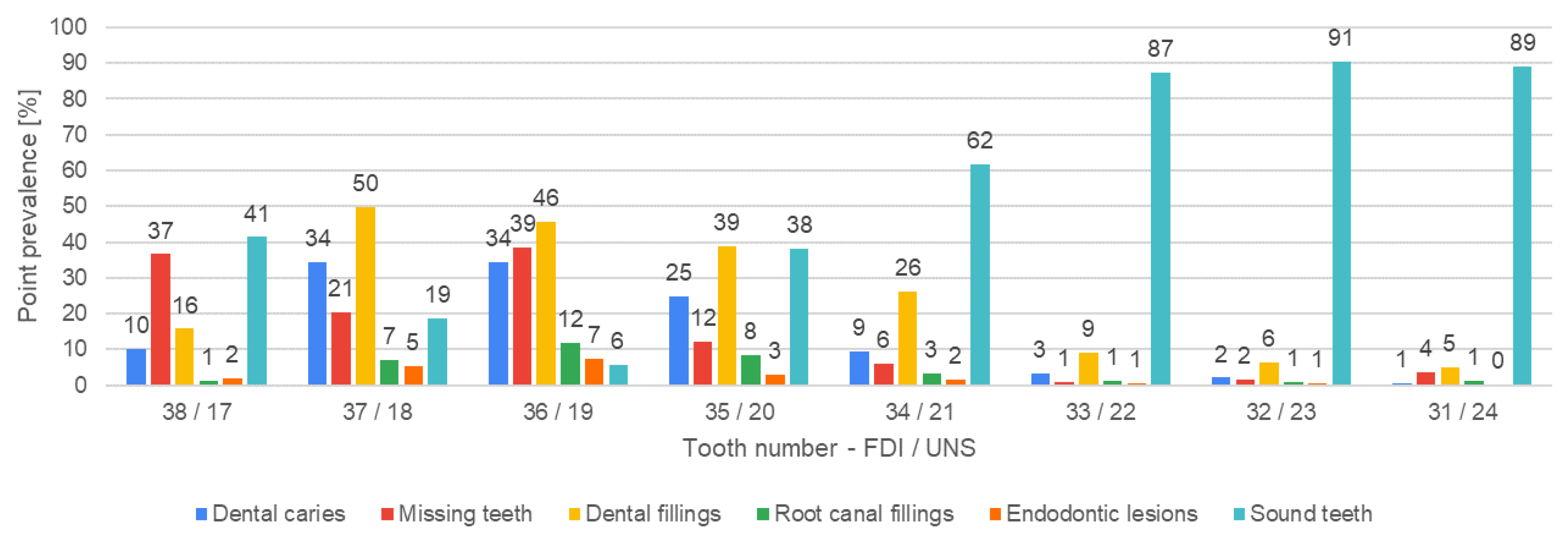
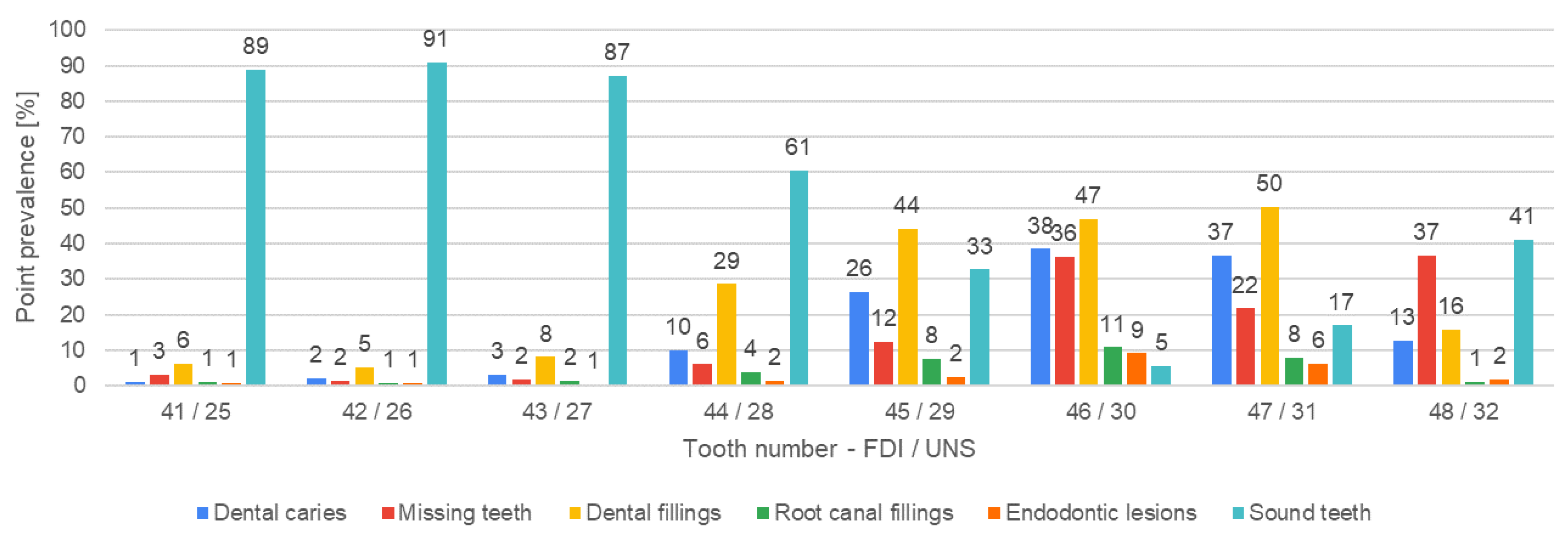
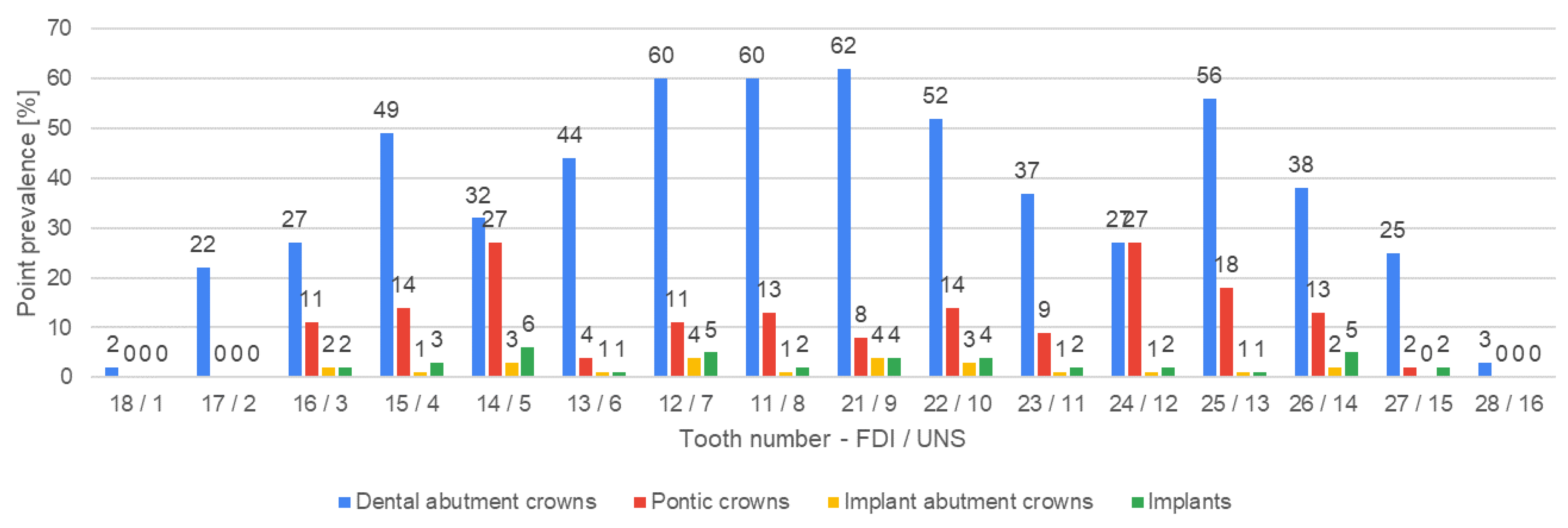
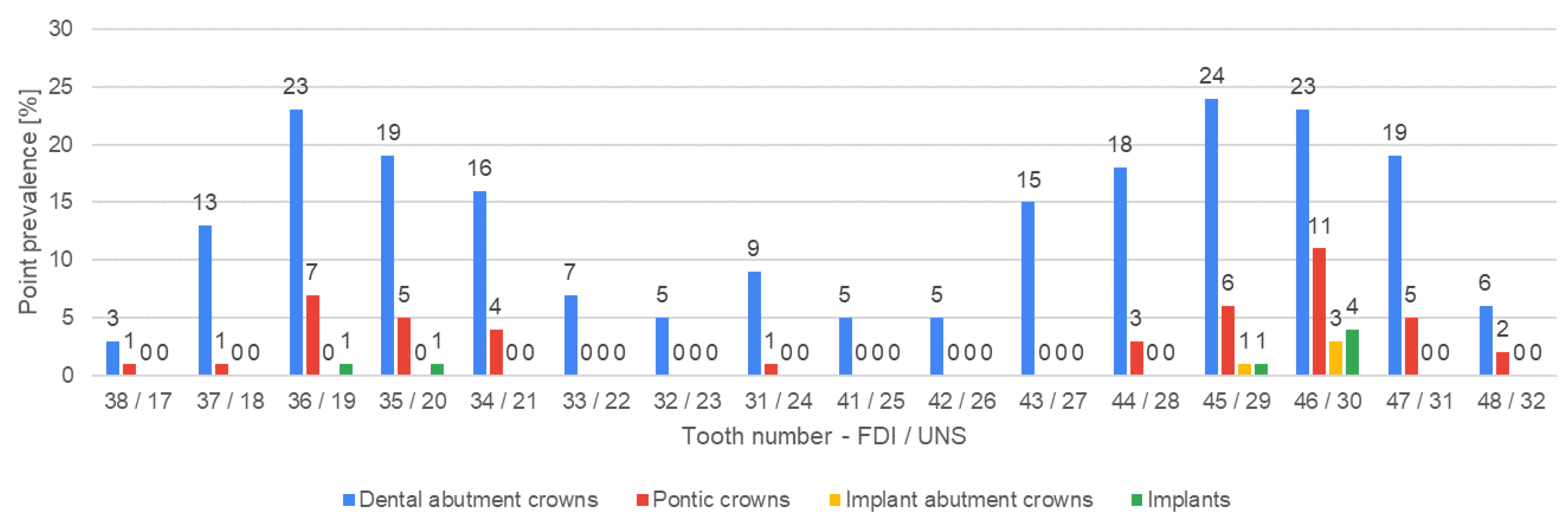
3.3. Outcome Data
3.4. Main Results
3.5. Subgroup Analyses
3.6. Other Analyses
4. Discussion
4.1. AI Software
4.2. Dental Caries
4.3. Missing Teeth
4.4. Endodontic Lesions and Treatment
4.5. Restoring Missing Teeth with Dental Implants and Bridges
4.6. Dental Crowns
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Różyło-Kalinowska, I. Panoramic Radiography in Dentistry. Clin. Dent. Rev. 2021, 5, 26. [Google Scholar] [CrossRef]
- Iannucci, J.; Howerton, L.J. Dental Radiography—Principles and Techniques, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Lee, J.-H.; Han, S.-S.; Kim, Y.H.; Lee, C.; Kim, I. Application of a Fully Deep Convolutional Neural Network to the Automation of Tooth Segmentation on Panoramic Radiographs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Delamare, E.; Fu, X.; Huang, Z.; Kim, J. Panoramic Imaging Errors in Machine Learning Model Development: A Systematic Review. Dentomaxillofacial Radiol. 2024, 53, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Leite, A.F.; Gerven, A.V.; Willems, H.; Beznik, T.; Lahoud, P.; Gaêta-Araujo, H.; Vranckx, M.; Jacobs, R. Artificial Intelligence-Driven Novel Tool for Tooth Detection and Segmentation on Panoramic Radiographs. Clin. Oral Investig. 2021, 25, 2257–2267. [Google Scholar] [CrossRef] [PubMed]
- Turosz, N.; Chęcińska, K.; Chęciński, M.; Brzozowska, A.; Nowak, Z.; Sikora, M. Applications of Artificial Intelligence in the Analysis of Dental Panoramic Radiographs: An Overview of Systematic Reviews. Dentomaxillofacial Radiol. 2023, 52, 20230284. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Albogami, S.; Hosmani, J.; Mujoo, S.; Kamil, M.A.; Mansour, M.A.; Abdul, H.N.; Bhandi, S.; Ahmed, S.S.S.J. Artificial Intelligence in the Diagnosis of Oral Diseases: Applications and Pitfalls. Diagnostics 2022, 12, 1029. [Google Scholar] [CrossRef] [PubMed]
- Zadrożny, Ł.; Regulski, P.; Brus-Sawczuk, K.; Czajkowska, M.; Parkanyi, L.; Ganz, S.; Mijiritsky, E. Artificial Intelligence Application in Assessment of Panoramic Radiographs. Diagnostics 2022, 12, 224. [Google Scholar] [CrossRef] [PubMed]
- The Digital Landscape of Dentistry: Dental AI Software—Diagnocat. Available online: https://diagnocat.com/eu/blog/the-digital-landscape-of-dentistry-dental-ai-software/ (accessed on 10 April 2024).
- PRESS RELEASE: Artificial Intelligence Takes Root—AI Insights Delivers Automatic Panoramic Image Analysis and Reporting in Seconds. Available online: https://www.carestreamdental.com/en-emea/training-resources/emea-newsroom/english/posts/2022/press-release-artificial-intelligence-takes-root--ai-insights-delivers-automatic-panoramic-image-analysis-and-reporting-in-seconds/ (accessed on 30 May 2024).
- Bonfanti-Gris, M.; Garcia-Cañas, A.; Alonso-Calvo, R.; Salido Rodriguez-Manzaneque, M.P.; Pradies Ramiro, G. Evaluation of an Artificial Intelligence Web-Based Software to Detect and Classify Dental Structures and Treatments in Panoramic Radiographs. J. Dent. 2022, 126, 104301. [Google Scholar] [CrossRef] [PubMed]
- Putra, R.H.; Doi, C.; Yoda, N.; Astuti, E.R.; Sasaki, K. Current Applications and Development of Artificial Intelligence for Digital Dental Radiography. Dento Maxillo Facial Radiol. 2022, 51, 20210197. [Google Scholar] [CrossRef]
- Pesapane, F.; Codari, M.; Sardanelli, F. Artificial Intelligence in Medical Imaging: Threat or Opportunity? Radiologists Again at the Forefront of Innovation in Medicine. Eur. Radiol. Exp. 2018, 2, 35. [Google Scholar] [CrossRef]
- Shafi, I.; Fatima, A.; Afzal, H.; Díez, I.d.l.T.; Lipari, V.; Breñosa, J.; Ashraf, I. A Comprehensive Review of Recent Advances in Artificial Intelligence for Dentistry E-Health. Diagnostics 2023, 13, 2196. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Lo, E.C.M.; Leung, K.C.M.; Chu, C.H. A Systematic Review on Caries Status of Older Adults. Int. J. Environ. Res. Public. Health 2021, 18, 10662. [Google Scholar] [CrossRef] [PubMed]
- Olczak-Kowalczyk, D. Monitorowanie Stanu Zdrowia Populacji Polskiej w Latach 2016–2020. Choroba Próchnicowa i Stan Tkanek Przyzębia Populacji Polskiej. Podsumowanie Wyników Badań z Lat 2016–2019. Sekcja Druków Uczelnianych Warszawskiego Uniwersytetu Medycznego Warszawa, Poland, 2021. Available online: https://www.gov.pl/attachment/e837445b-41ef-4b49-b261-d21d869e0018/ (accessed on 30 March 2024).
- Yang, B.; Olsen, M.; Vali, Y.; Langendam, M.W.; Takwoingi, Y.; Hyde, C.J.; Bossuyt, P.M.M.; Leeflang, M.M.G. Study Designs for Comparative Diagnostic Test Accuracy: A Methodological Review and Classification Scheme. J. Clin. Epidemiol. 2021, 138, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, J.E.; Chaurasia, A.; Feldberg, B.; Krois, J.; Schwendicke, F. Classification of Dental Radiographs Using Deep Learning. J. Clin. Med. 2021, 10, 1496. [Google Scholar] [CrossRef]
- Ekert, T.; Krois, J.; Meinhold, L.; Elhennawy, K.; Emara, R.; Golla, T.; Schwendicke, F. Deep Learning for the Radiographic Detection of Apical Lesions. J. Endod. 2019, 45, 917–922.e5. [Google Scholar] [CrossRef] [PubMed]
- Dziennik Urzędowy Ministra Zdrowia Obwieszczenie Ministra Zdrowia z Dnia 10 Listopada 2015 r. w Sprawie Ogłoszenia Wykazu Wzorcowych Procedur Radiologicznych z Zakresu Radiologii—Diagnostyki Obrazowej i Radiologii Zabiegowej. 2015; p. 43. Available online: https://dziennikmz.mz.gov.pl/DUM_MZ/2015/78/akt.pdf (accessed on 18 March 2024).
- González-Ramírez, A.R.; Rivas-Ruiz, F. Measures of Frequency, Magnitude of Association and Impact in Epidemiology. Allergol. Immunopathol. 2010, 38, 147–152. [Google Scholar] [CrossRef] [PubMed]
- What Is Prevalence?—National Institute of Mental Health (NIMH). Available online: https://www.nimh.nih.gov/health/statistics/what-is-prevalence (accessed on 7 February 2024).
- Correlation Coefficient—An Overview|ScienceDirect Topics. Available online: https://www.sciencedirect.com/topics/earth-and-planetary-sciences/correlation-coefficient (accessed on 7 February 2024).
- Carestream Dental|AI Insights. Available online: https://www.carestreamdental.com/en-gb/csd-products/software/imaging-software/ai-insights/ (accessed on 18 June 2024).
- Demirci, M.; Tuncer, S.; Yuceokur, A.A. Prevalence of Caries on Individual Tooth Surfaces and Its Distribution by Age and Gender in University Clinic Patients. Eur. J. Dent. 2010, 4, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Luan, W.; Baelum, V.; Fejerskov, O.; Chen, X. Ten-Year Incidence of Dental Caries in Adult and Elderly Chinese. Caries Res. 2000, 34, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.; Khan, J.A.; Ali, S.A. Caries Susceptibility of Proximal Surfaces in Permanent First Molars: A Cross Sectional Survey. J. Islam. Int. Med. Coll. JIIMC 2019, 14, 38–42. [Google Scholar]
- Dosumu, O.O.; Ogunrinde, J.T.; Bamigboye, S.A. Knowledge of Consequences of Missing Teeth in Patients Attending Prosthetic Clinic in U.C.H. Ibadan. Ann. Ib. Postgrad. Med. 2014, 12, 42–48. [Google Scholar]
- Scheiwiller, M.; Oeschger, E.S.; Gkantidis, N. Third Molar Agenesis in Modern Humans with and without Agenesis of Other Teeth. PeerJ 2020, 8, e10367. [Google Scholar] [CrossRef] [PubMed]
- Lindauer, S.J.; Laskin, D.M.; Tüfekçi, E.; Taylor, R.S.; Cushing, B.J.; Best, A.M. Orthodontists’ and Surgeons’ Opinions on the Role of Third Molars as a Cause of DENTAL crowding. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Lyros, I.; Vasoglou, G.; Lykogeorgos, T.; Tsolakis, I.A.; Maroulakos, M.P.; Fora, E.; Tsolakis, A.I. The Effect of Third Molars on the Mandibular Anterior Crowding Relapse—A Systematic Review. Dent. J. 2023, 11, 131. [Google Scholar] [CrossRef] [PubMed]
- Assali, A.; Oualalou, Y.; Zaoui, F. The Evolution of Third Molars in Orthodontics: What about Anterior Dental Crowding?—A Systematic Review. Integr. J. Med. Sci. 2022, 9, 1–4. [Google Scholar] [CrossRef]
- León-López, M.; Cabanillas-Balsera, D.; Martín-González, J.; Montero-Miralles, P.; Saúco-Márquez, J.J.; Segura-Egea, J.J. Prevalence of Root Canal Treatment Worldwide: A Systematic Review and Meta-Analysis. Int. Endod. J. 2022, 55, 1105–1127. [Google Scholar] [CrossRef] [PubMed]
- American Association of Endodontists. Glossary of Endodontic Terms; American Association of Endodontists: Chicago, IL, USA, 2020; p. 33. [Google Scholar]
- Özbaş, H.; Aşcı, S.; Aydın, Y. Examination of the Prevalence of Periapical Lesions and Technical Quality of Endodontic Treatment in a Turkish Subpopulation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Alnowailaty, Y.; Alghamdi, F. Prevalence of Endodontically Treated Premolars and Molars With Untreated Canals and Their Association With Apical Periodontitis Using Cone-Beam Computed Tomography. Cureus 2022, 14, e25619. [Google Scholar] [CrossRef]
- Orstavik, D. Time-Course and Risk Analyses of the Development and Healing of Chronic Apical Periodontitis in Man. Int. Endod. J. 1996, 29, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Mosquera-Barreiro, C.; Ruíz-Piñón, M.; Sans, F.A.; Nagendrababu, V.; Vinothkumar, T.S.; Martín-González, J.; Martín-Biedma, B.; Castelo-Baz, P. Predictors of Periapical Bone Healing Associated with Teeth Having Large Periapical Lesions Following Nonsurgical Root Canal Treatment or Retreatment: A Cone Beam Computed Tomography-Based Retrospective Study. Int. Endod. J. 2024, 57, 23–36. [Google Scholar] [CrossRef]
- Daviet-Noual, V.; Ejeil, A.-L.; Gossiome, C.; Moreau, N.; Salmon, B. Differentiating Early Stage Florid Osseous Dysplasia from Periapical Endodontic Lesions: A Radiological-Based Diagnostic Algorithm. BMC Oral Health 2017, 17, 161. [Google Scholar] [CrossRef]
- Mupparapu, M.; Shi, K.J.; Ko, E. Differential Diagnosis of Periapical Radiopacities and Radiolucencies. Dent. Clin. N. Am. 2020, 64, 163–189. [Google Scholar] [CrossRef] [PubMed]
- Ghafoor, R. Conservative Management of Progressive External Inflammatory Root Resorption after Traumatic Tooth Intrusion. J. Conserv. Dent. 2013, 16, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Krupińska, A.M.; Bogucki, Z. Evaluation of Patients’ Awareness and Knowledge Regarding Dental Implants among Patients of the Department of Prosthetic Dentistry at Wroclaw Medical University in Poland. Adv. Clin. Exp. Med. 2023, 32, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Buser, D.; Sculean, A.; Belser, U.C. Complications and Treatment Errors in Implant Positioning in the Aesthetic Zone: Diagnosis and Possible Solutions. Periodontology 2000 2023, 92, 220–234. [Google Scholar] [CrossRef] [PubMed]
- Tikku, A.P.; Chandra, A.; Bharti, R. Are Full Cast Crowns Mandatory after Endodontic Treatment in Posterior Teeth? J. Conserv. Dent. 2010, 13, 246–248. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Pharoah, M.J. Oral Radiology—Principles and Interpretation, 6th ed.; MOSBY Elsevier: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Kamburoğlu, K.; Kolsuz, E.; Murat, S.; Yüksel, S.; Özen, T. Proximal Caries Detection Accuracy Using Intraoral Bitewing Radiography, Extraoral Bitewing Radiography and PANORAMIC radiography. Dentomaxillofacial Radiol. 2012, 41, 450–459. [Google Scholar] [CrossRef]
- Kweon, H.H.-I.; Lee, J.-H.; Youk, T.; Lee, B.-A.; Kim, Y.-T. Panoramic Radiography Can Be an Effective Diagnostic Tool Adjunctive to Oral Examinations in the National Health Checkup Program. J. Periodontal Implant. Sci. 2018, 48, 317. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Pakbaznejad Esmaeili, E.; Robinson, S. Dentomaxillofacial Imaging with Panoramic Views and Cone Beam CT. Insights Imaging 2015, 6, 1–16. [Google Scholar] [CrossRef]
- Peretz, B.; Gotler, M.; Kaffe, I. Common Errors in Digital Panoramic Radiographs of Patients with Mixed Dentition and Patients with Permanent Dentition. Int. J. Dent. 2012, 2012, 584138. [Google Scholar] [CrossRef]
- Dziennik Ustaw Rzeczpospolitej Polskiej, Rozporządzenie Ministra Zdrowia z Dnia 8 Grudnia 2017 r. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20170002397/O/D20172397.pdf (accessed on 19 May 2024).
- Krois, J.; Ekert, T.; Meinhold, L.; Golla, T.; Kharbot, B.; Wittemeier, A.; Dörfer, C.; Schwendicke, F. Deep Learning for the Radiographic Detection of Periodontal Bone Loss. Sci. Rep. 2019, 9, 8495. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Barmak, A.B.; Inam, W.; Kan, J.Y.K.; Kois, J.C.; Akal, O. Artificial Intelligence Models for Diagnosing Gingivitis and Periodontal Disease: A Systematic Review. J. Prosthet. Dent. 2022, 130, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, B.A.; Galluci, G.O.; Att, W.; Krishnamurthy, V.R. Artificial Intelligence Applications in Implant Dentistry: A Systematic Review. J. Prosthet. Dent. 2023, 129, 293–300. [Google Scholar] [CrossRef] [PubMed]


| Study Design Feature | Applied Study Design |
|---|---|
| Direction of data collection | Retrospective |
| Number of gates (sets of eligibility criteria) | Double gate (AI, human) |
| Participant sampling method | Consecutive |
| Method of allocating participants to index tests | Each participant received all index tests |
| Number of reference standards | Single test standard |
| Limited verification | Full verification (not limited) |
| Domain | Criteria for Inclusion | Criteria for Exclusion |
|---|---|---|
| Indications | Typical indications for DPR imaging confirmed by a written referral from the dentist or physician (both screening tests and tests performed for treatment purposes were allowed) | Not applicable |
| Dentition | Not applicable | Patients with mixed or primary dentition |
| Age | Patients of any age | No age restrictions applied due to the limitation in the dentition category |
| Sex | All genders | No gender restrictions |
| Quality of DPRs | Correctly performed DPR in accordance with the criteria of the Polish Ministry of Health [20] | AI error resulting in no results or partial results |
| Abbreviation | Name of the Variable | Description |
|---|---|---|
| D | Dental caries | Presence of at least one cavity (carious or non-carious) in a given tooth |
| M | Missing tooth | Absence of any tooth remnants in a given location |
| F | Dental filling | Presence of at least one filling in a given tooth |
| R | Root canal filling | Presence of at least one filled root canal (completely or partially) |
| E | Endodontic lesion | Periapical radiological radiolucency primarily suggesting periapical inflammation |
| I | Implant | Radiological shading in the shape of an intraosseous dental implant |
| A | Implant abutment crown | Prosthetic crown based on an implant |
| P | Pontic crown | Prosthetic bridge span (prosthetic crown without direct support) |
| C | Dental abutment crown | A prosthetic crown supported on a tooth |
| S | Sound tooth | A tooth without signs of the above-mentioned pathologies or signs of the above-mentioned treatment methods |
| Finding | Total Number | Average per Patient | Standard Deviation | Upper Arch | Lower Arch |
|---|---|---|---|---|---|
| Sound tooth | 14,533 | 14.83 | 6.99 | 6141 | 8392 |
| Dental filling | 8882 | 9.06 | 4.80 | 4942 | 3940 |
| Dental caries | 5975 | 6.10 | 3.11 | 3526 | 2449 |
| Missing tooth | 5066 | 5.17 | 5.68 | 2714 | 2352 |
| Root canal filling | 1918 | 1.96 | 2.18 | 1227 | 691 |
| Endodontic lesion | 882 | 0.90 | 1.19 | 447 | 435 |
| Dental abutment crown | 806 | 0.82 | 1.76 | 596 | 210 |
| Pontic crown | 217 | 0.22 | 0.89 | 171 | 46 |
| Implant | 46 | 0.05 | 0.38 | 39 | 7 |
| Implant abutment crown | 28 | 0.03 | 0.32 | 24 | 4 |
| The Most Common Tooth (Frequency) FDI/UNS | The Least Common Tooth (Frequency) FDI/UNS | |
|---|---|---|
| Dental caries | 16/3 (432 times) | 31/24 (7 times) |
| Missing teeth | 28/16 (385 times) | 33/22 (8 times) |
| Dental filling | 16/3 (538 times) | 31/24 (51 times) |
| Root canal filling | 26/14 (141 times) | 28/16, 42/26 (8 times) |
| Endodontic lesion | 46/30 (89 times) | 31/24 (3 times) |
| Dental abutment crown | 21/9 (62 times) | 18/1 (2 times) |
| Pontic abutment crown | 14/5, 24/12 (27 times) | 18/1, 17/2, 28/16, 33/22, 32/2, 41/25–44/27 (0 times) |
| Implant abutment crown | 12/7, 21/9 (4 times) | 18/1, 17/2, 27/15–44/28, 47/31, 48/32 (0 times) |
| Implant | 14/5 (6 times) | 18/1, 17/2, 28/16–37/18, 34/21–44/28, 47/31, 48/32 (0 times) |
| Sound tooth | 42/26 (892 times) | 46/30 (53 times) |
| The Most Common Tooth (Frequency) FDI/UNS | The Least Common Tooth (Frequency) FDI/UNS | Average per Patient | |
|---|---|---|---|
| Dental caries | 36/19 (57 times) | 13/6, 38/17, 33/22–43/27, 48/32 (0 times) | 4.01 |
| Missing teeth | 18/1, 28/16, 48/32 (11 times) | 15/4, 13/6, 11/8–22/10, 37/18, 33/22–43/27 (0 times) | 0.79 |
| Dental filling | 16/3, 36/19 (60 times) | 18/1, 28/16, 38/17 (0 times) | 4.5 |
| Root canal filling | 46/30 (6 times) | 18/1, 17/2, 14/5, 13/6, 11/8, 22/10, 23/11, 25/13, 28/16, 38/17, 35/20–44/28, 47/31, 48/32 (0 times) | 0.27 |
| Endodontic lesion | 46/30 (7 times) | 18/1, 17/2, 13/6, 24/12, 27/15, 28/16, 33/22–43/27, 48/32 (0 times) | 0.44 |
| Dental abutment crown | 16/3, 26/14 (2 times) | 18/1, 17/2, 14/5, 13/6, 11/8, 22/10, 23/11, 25/13, 27/15–37/18, 35/20–45/29, 47/31, 48/32 (0 times) | 0.09 |
| Pontic abutment crown | 1 (1 time) | 18/1–12/7, 21/9–48/32 (0 times) | 0.01 |
| Implant abutment crown | 0 | 0 | 0 |
| Implant | 0 | 0 | 0 |
| Sound tooth | 13/6, 42/26 (110 times) | 36/19 (27 times) | 24.5 |
| The Most Common Tooth (Frequency) FDI/UNS | The Least Common Tooth (Frequency) FDI/UNS | Average per Patient | |
|---|---|---|---|
| Dental caries | 16/3 (270 times) | 41/25 (2 times) | 6.6 |
| Missing teeth | 28/16, 36/19 (157 times) | 42/26 (1 time) | 3.2 |
| Dental filling | 16/3 (352 times) | 32/23, 42/26 (19 times) | 9.9 |
| Root canal filling | 36/19 (83 times) | 33/22 (0 times) | 1.8 |
| Endodontic lesion | 46/30 (58 times) | 43/27 (0 times) | 0.9 |
| Dental abutment crown | 25/13 (26 times) | 38/17, 33/22, 41/25, 42/26, 48/32 (0 times) | 0.4 |
| Pontic abutment crown | 24/12 (9 times) | 18/1, 17/2, 13/6, 27/15–35/20, 33/22–48/32 (0 times) | 0.1 |
| Implant abutment crown | 21/9 (2 times) | 18/1–15/4, 13/6, 11/8, 22/10–44/28, 47/31, 48/32 (0 times) | 0 |
| Implant | 14/5 (3 times) | 18/1–15/4, 13/6, 11/8, 22/10, 23/11, 25/13, 27/15–37,18, 35/20–44/28, 47/31, 48/32 (0 times) | 0 |
| Sound tooth | 42/26 (525 times) | 46/30 (24 times) | 16 |
| The Most Common Tooth (Frequency) FDI/UNS | The Least Common Tooth (Frequency) | Average per Patient | |
|---|---|---|---|
| Dental caries | 17/2, 16/3 (91 times) | 31/24 (2 times) | 6.2 |
| Missing teeth | 36/19 (163 times) | 33/22 (3 times) | 8.9 |
| Dental filling | 17/2 (131 times) | 31/24 (15 times) | 9.9 |
| Root canal filling | 26/14 (44 times) | 32/23, 41/25, 48/32 (3 times) | 2.9 |
| Endodontic lesion | 46/30 (23 times) | 31/24, 48/32 (2 times) | 1 |
| Dental abutment crown | 12/7 (31 times) | 18/1, 28/16 (1 time) | 1.7 |
| Pontic abutment crown | 14/5 (17 times) | 18/1, 17/2, 28/16, 33/22, 32/23, 41/25–43/27 (0 times) | 0.5 |
| Implant abutment crown | 14/5, 12/7, 21/9, 22/10, 46/30 (2 times) | 18/1, 17/2, 13/6, 23/11, 27/15–45/29, 47/31, 48/32 (0 times) | 0.1 |
| Implant | 15/4, 14/5, 12/7, 22/10, 26/14, 46/30 (3 times) | 18/1, 17/2, 13/6, 28/16–36/19, 34/21–45/29, 47/31, 48/32 (0 times) | 0.1 |
| Sound tooth | 42/26 (216 times) | 46/30 (0 times) | 9.6 |
| The Most Common Tooth (Frequency) FDI/UNS | The Least Common Tooth (Frequency) | Average per Patient | |
|---|---|---|---|
| Dental caries | 13/6 (21 times) | 38/17 (0 times) | 4.9 |
| Missing teeth | 38/17 (58 times) | 33/22 (2 times) | 15 |
| Dental filling | 45/29 (26 times) | 38/17 (3 times) | 6.5 |
| Root canal filling | 35/20 (14 times) | 28/16, 38/17 (0 times) | 2.4 |
| Endodontic lesion | 25/13, 37/18, 47/31(5 times) | 13/6, 11/8, 38/17, 32/23, 31/24 (0 times) | 0.8 |
| Dental abutment crown | 15/4, 12/7 (13 times) | 18/1, 28/16, 38/17, 32/23, 41/25, 42/26 (0 times) | 2.4 |
| Pontic abutment crown | 24/12 (6 times) | 18/1, 17/2, 28/16–37/18, 35/20, 33/22–43/27, 48/32 (0 times) | 0.7 |
| Implant abutment crown | 16/3, 13/6, 12/7, 22/10, 23/11, 26/14 (1 time) | 18/1, 17/2, 15/4, 14/5, 11/8, 21/9, 24/12, 25/13, 27/15–48/32 (0 times) | 0.1 |
| Implant | 16/3, 13/6, 12/7, 22/10, 23/11, 26/14 (1 time) | 18/1, 17/2, 15/4, 14/5, 11/8, 21/9, 24/12, 25/13, 27/15–48/32 (0 times) | 0.1 |
| Sound tooth | 32/23, 43/27 (42 times) | 37/18, 36/19 (0 times) | 6.6 |
| Age | D | M | F | R | E | I | A | P | C | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | ||||||||||
| D | 0.01 | |||||||||
| M | 0.71 * | −0.12 | ||||||||
| F | 0.09 | 0.38 | −0.21 | |||||||
| R | 0.35 | 0.27 | 0.15 | 0.39 | ||||||
| E | 0.12 | 0.37 | 0.08 | 0.01 | 0.23 | |||||
| I | 0.12 | −0.06 | 0.06 | −0.06 | 0.12 | −0.06 | ||||
| A | 0.10 | −0.08 | 0.05 | −0.06 | 0.10 | −0.05 | 0.88 * | |||
| P | 0.29 | −0.04 | 0.10 | −0.10 | 0.19 | 0.01 | 0.27 | 0.32 | ||
| C | 0.44 | 0.02 | 0.23 | −0.04 | 0.44 | 0.08 | 0.28 | 0.26 | 0.63 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turosz, N.; Chęcińska, K.; Chęciński, M.; Rutański, I.; Sielski, M.; Sikora, M. Oral Health Status and Treatment Needs Based on Artificial Intelligence (AI) Dental Panoramic Radiograph (DPR) Analysis: A Cross-Sectional Study. J. Clin. Med. 2024, 13, 3686. https://doi.org/10.3390/jcm13133686
Turosz N, Chęcińska K, Chęciński M, Rutański I, Sielski M, Sikora M. Oral Health Status and Treatment Needs Based on Artificial Intelligence (AI) Dental Panoramic Radiograph (DPR) Analysis: A Cross-Sectional Study. Journal of Clinical Medicine. 2024; 13(13):3686. https://doi.org/10.3390/jcm13133686
Chicago/Turabian StyleTurosz, Natalia, Kamila Chęcińska, Maciej Chęciński, Iwo Rutański, Marcin Sielski, and Maciej Sikora. 2024. "Oral Health Status and Treatment Needs Based on Artificial Intelligence (AI) Dental Panoramic Radiograph (DPR) Analysis: A Cross-Sectional Study" Journal of Clinical Medicine 13, no. 13: 3686. https://doi.org/10.3390/jcm13133686
APA StyleTurosz, N., Chęcińska, K., Chęciński, M., Rutański, I., Sielski, M., & Sikora, M. (2024). Oral Health Status and Treatment Needs Based on Artificial Intelligence (AI) Dental Panoramic Radiograph (DPR) Analysis: A Cross-Sectional Study. Journal of Clinical Medicine, 13(13), 3686. https://doi.org/10.3390/jcm13133686









