A Functional and Immunologic Point of View on Corneal Endothelial Transplantation: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Material and Methods
2.1. Selection Criteria and Search Methods
2.2. Study Selection
2.3. Data Synthesis and Analysis
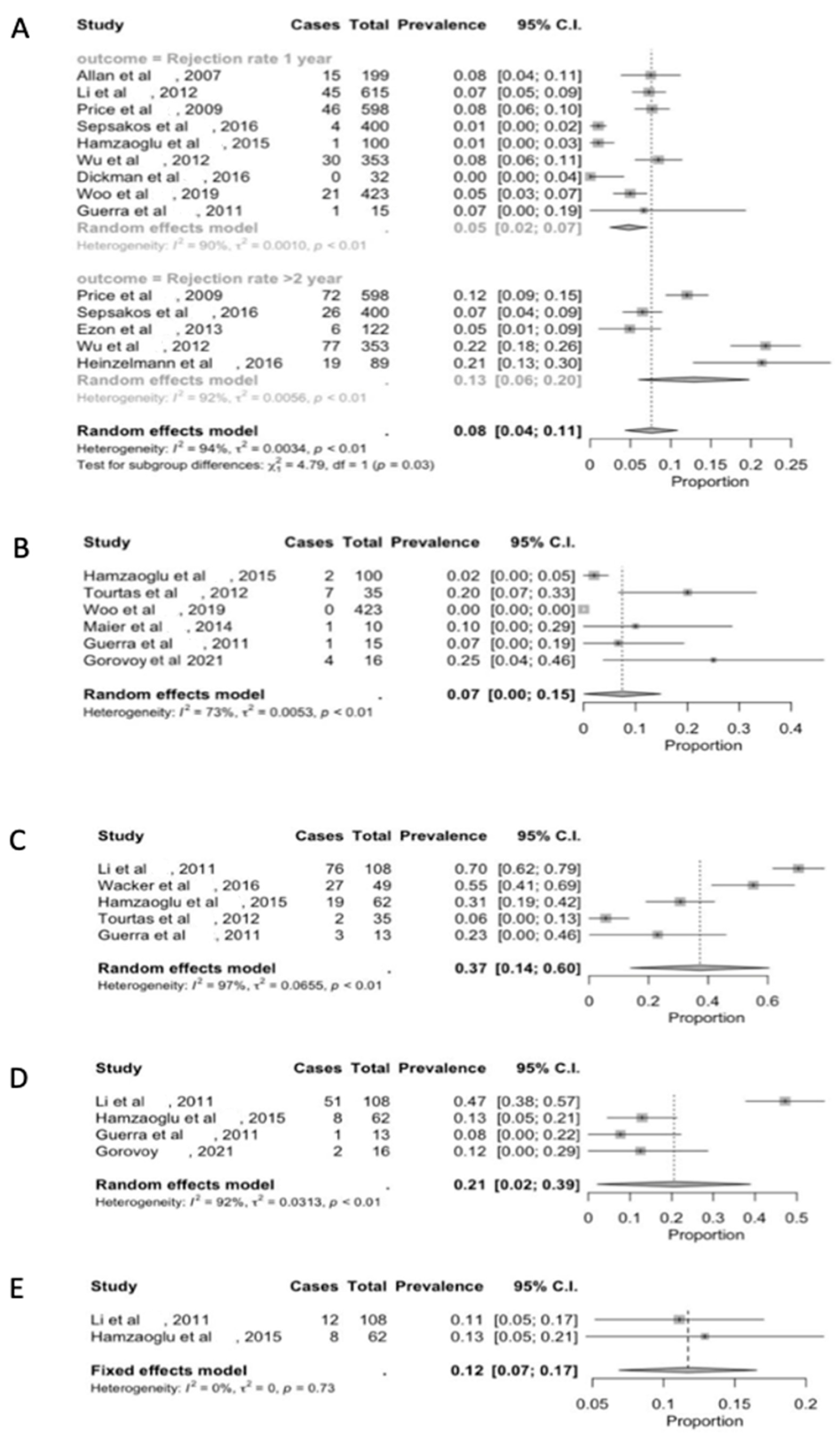
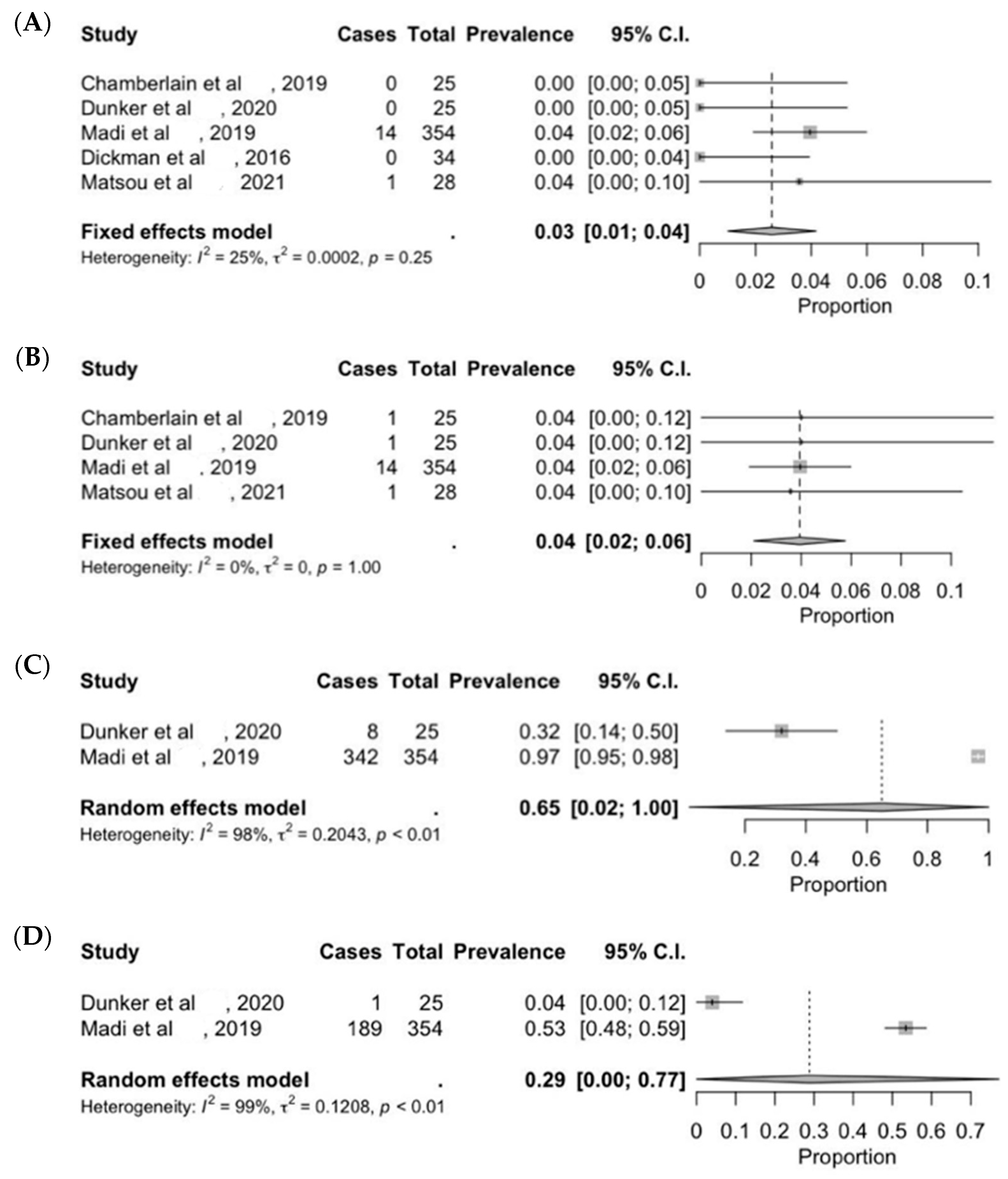
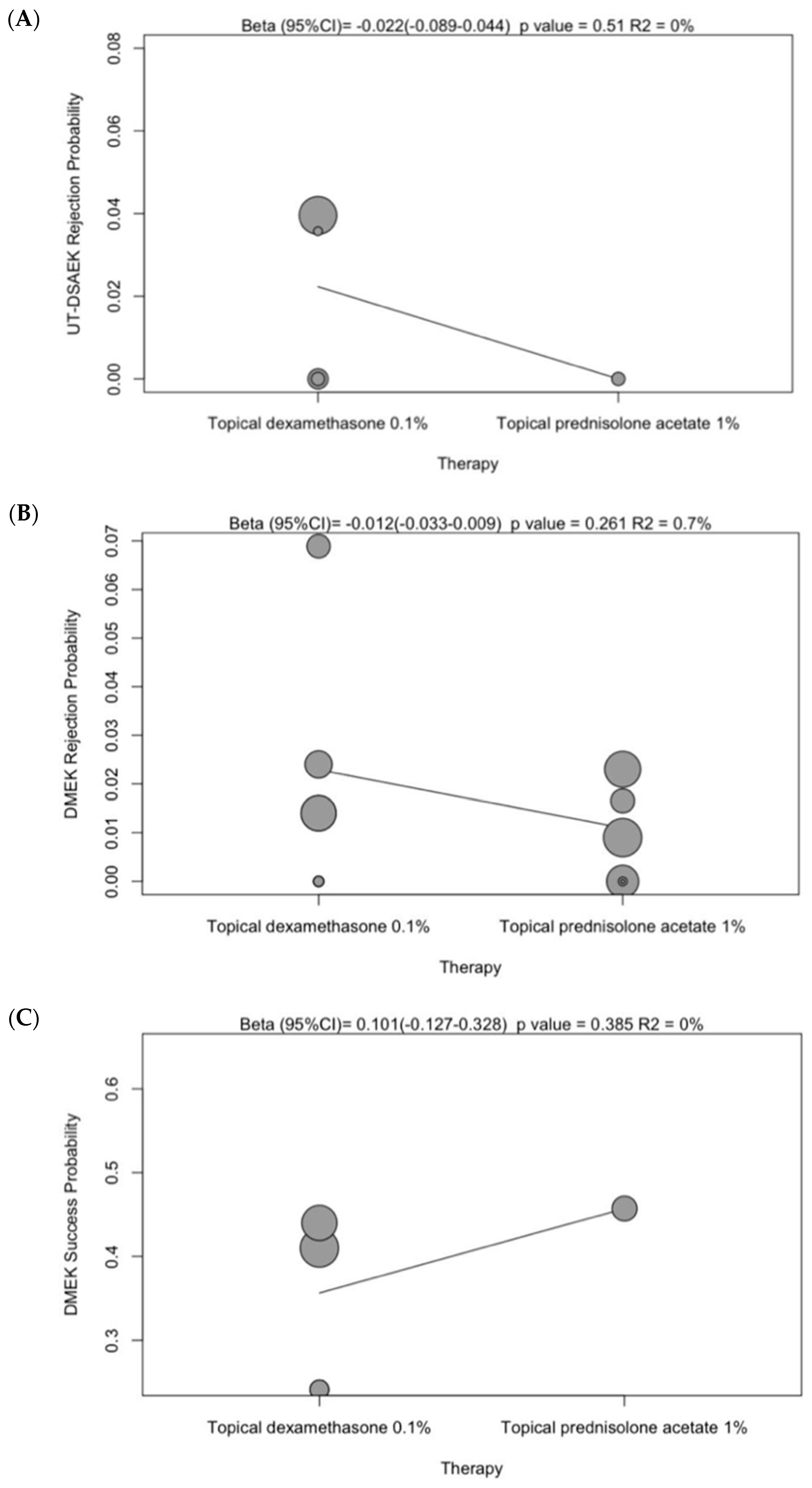
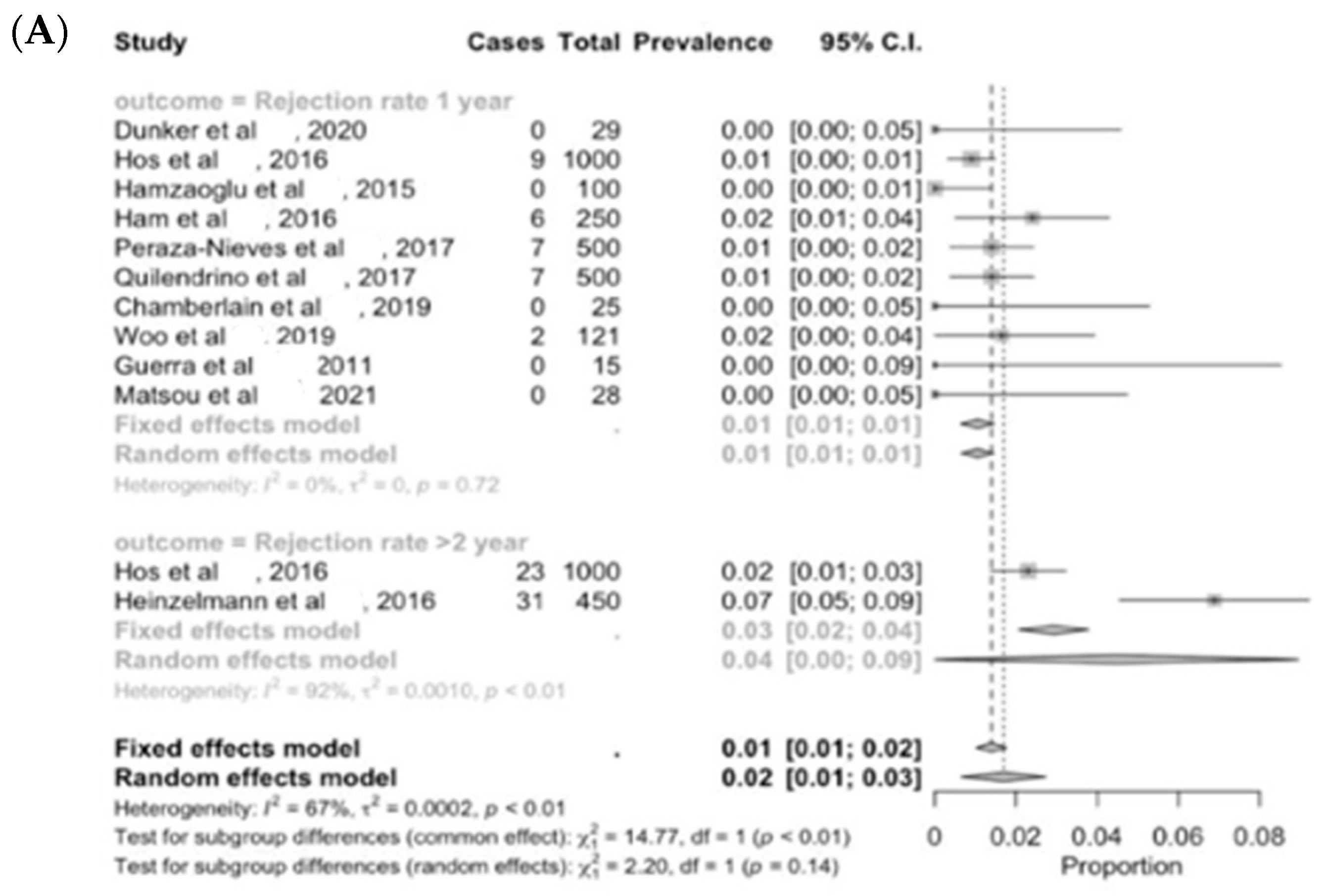
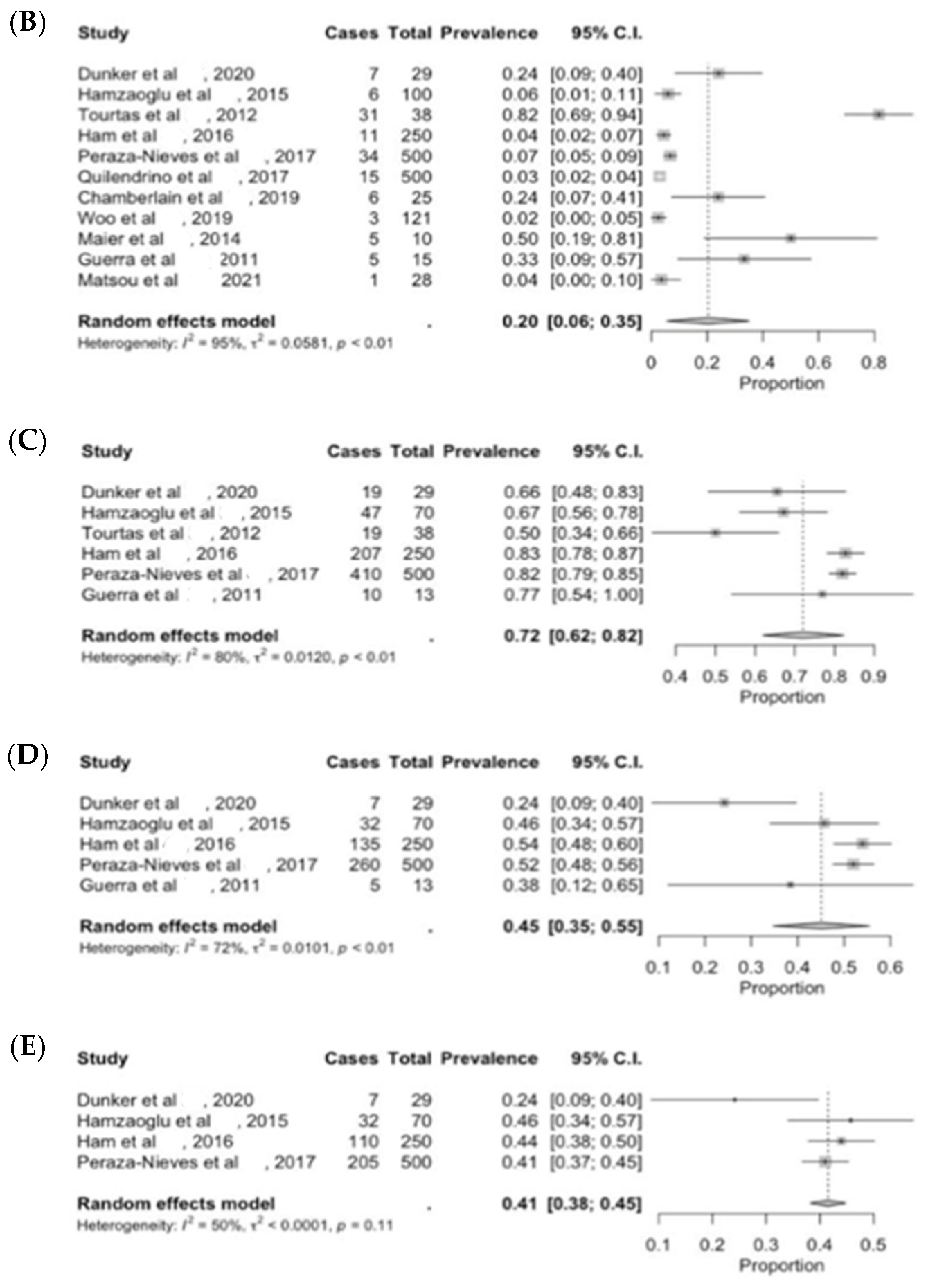
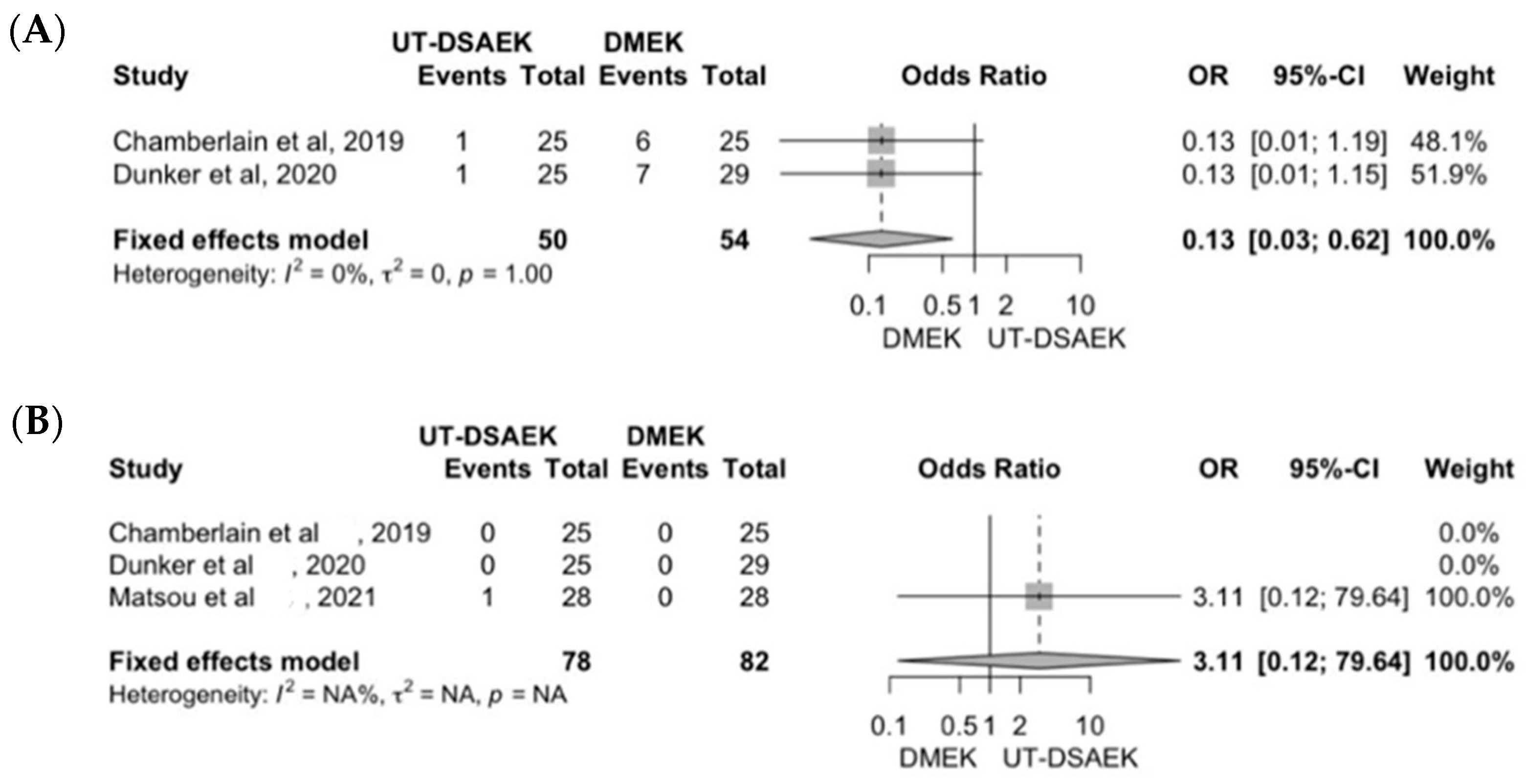
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Niederkorn, J.Y. See no evil, hear no evil, do no evil: The lessons of immune privilege. Nat. Immunol. 2006, 7, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Streilein, J.W. Ocular immune privilege: Therapeutic opportunities from an experiment of nature. Nat. Rev. Immunol. 2003, 3, 879–889. [Google Scholar] [CrossRef]
- Hos, D.; Matthaei, M.; Bock, F.; Maruyama, K.; Notara, M.; Clahsen, T.; Hou, Y.; Le, V.N.H.; Salabarria, A.-C.; Horstmann, J.; et al. Immune reactions after modern lamellar (DALK, DSAEK, DMEK) versus conventional penetrating corneal transplantation. Prog. Retin. Eye Res. 2019, 73, 100768. [Google Scholar] [CrossRef]
- Hori, J.; Yamaguchi, T.; Keino, H.; Hamrah, P.; Maruyama, K. Immune privilege in corneal transplantation. Prog. Retin. Eye Res. 2019, 72, 100758. [Google Scholar] [CrossRef]
- Niederkorn, J.Y.; Kaplan, H.J. Rationale for immune response and the eye. Chem. Immunol. Allergy 2007, 92, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Stein-Streilein, J.; Streilein, J.W. Anterior chamber associated immune deviation (ACAID): Regulation, biological relevance, and implications for therapy. Int. Rev. Immunol. 2002, 21, 123–152. [Google Scholar] [CrossRef] [PubMed]
- Streilein, J.W.; Masli, S.; Takeuchi, M.; Kezuka, T. The eye’s view of antigen presentation. Hum. Immunol. 2002, 63, 435–443. [Google Scholar] [CrossRef]
- Kaplan, H.J.; Streilein, J.W. Immune response to immunization via the anterior chamber of the eye. II. An analysis of F1 lymphocyte-induced immune deviation. J. Immunol. 1978, 120, 689–693. [Google Scholar] [CrossRef]
- Ksander, B.R.; Streilein, J.W. Analysis of cytotoxic T cell responses to intracameral allogeneic tumors. Investig. Ophthalmol. Vis. Sci. 1989, 30, 323–329. [Google Scholar]
- Wilbanks, G.A.; Streilein, J.W. Distinctive humoral immune responses following anterior chamber and intravenous administration of soluble antigen. Evidence for active suppression of IgG2-secreting B lymphocytes. Immunology 1990, 71, 566. [Google Scholar]
- Di Zazzo, A.; Lee, S.-M.; Sung, J.; Niutta, M.; Coassin, M.; Mashaghi, A.; Inomata, T. Variable Responses to Corneal Grafts: Insights from Immunology and Systems Biology. J. Clin. Med. 2020, 9, 586. [Google Scholar] [CrossRef] [PubMed]
- Di Zazzo, A.; Kheirkhah, A.; Abud, T.B.; Goyal, S.; Dana, R. Management of high-risk corneal transplantation. Surv. Ophthalmol. 2017, 62, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Akanda, Z.Z.; Naeem, A.; Russell, E.; Belrose, J.; Si, F.F.; Hodge, W.G. Graft rejection rate and graft failure rate of penetrating keratoplasty (PKP) vs lamellar procedures: A systematic review. PLoS ONE 2015, 10, e0119934. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hori, J.; Joyce, N.; Streilein, J.W. Epithelium-deficient corneal allografts display immune privilege beneath the kidney capsule. Investig. Ophthalmol. Vis. Sci. 2000, 41, 443–452. [Google Scholar]
- Busin, M.; Albé, E. Does thickness matter: Ultrathin Descemet stripping automated endothelial keratoplasty. Curr. Opin. Ophthalmol. 2014, 25, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Galvis, V.; Berrospi, R.D.; Arias, J.D.; Tello, A.; Bernal, J.C. Heads up Descemet membrane endothelial keratoplasty performed using a 3D visualization system. J Surg Case Rep. 2017, 2017, rjx231. [Google Scholar] [CrossRef] [PubMed]
- Mosca, L.; Scartozzi, L.; De Filippis, A.; Guccione, L.; Fasciani, R.; Rizzo, S. 3D Heads-up digital filters for cataract surgery and corneal transplantation. Eur J Ophthalmol. 2024, 6, 11206721241253633. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.S.; Goshe, J.M.; Srivastava, S.K.; Ehlers, J.P. Intraoperative Optical Coherence Tomography-Assisted Descemet Membrane Endothelial Keratoplasty in the DISCOVER Study: First 100 Cases. Am. J. Ophthalmol. 2020, 210, 167–173. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cursiefen, C.; Kruse, F.E. DMEK: Descemet membrane endothelial keratoplasty. Ophthalmol. Z. Dtsch. Ophthalmol. Ges. 2010, 107, 370–376. [Google Scholar] [CrossRef]
- Matthaei, M.; Bachmann, B.; Siebelmann, S.; Cursiefen, C. Technique of Descemet membrane endothelial keratoplasty (DMEK): Video article. Der Ophthalmol. Z. Dtsch. Ophthalmol. Ges. 2018, 115, 778–784. [Google Scholar] [CrossRef]
- Allan, B.D.S.; Terry, M.A.; Price, F.W.; Price, M.O.; Griffin, N.B.; Claesson, M. Corneal transplant rejection rate and severity after endothelial keratoplasty. Cornea 2007, 26, 1039–1042. [Google Scholar] [CrossRef] [PubMed]
- Li, J.Y.; Terry, M.A.; Goshe, J.; Shamie, N.; Davis-Boozer, D. Graft rejection after Descemet’s stripping automated endothelial keratoplasty: Graft survival and endothelial cell loss. Ophthalmology 2012, 119, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Price, M.O.; Jordan, C.S.; Moore, G.; Price, F.W. Graft rejection episodes after Descemet stripping with endothelial keratoplasty: Part two: The statistical analysis of probability and risk factors. Br. J. Ophthalmol. 2009, 93, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Sepsakos, L.; Shah, K.; Lindquist, T.P.; Lee, W.B.; Holland, E. Rate of Rejection After Descemet Stripping Automated Endothelial Keratoplasty in Fuchs Dystrophy: Three-Year Follow-up. Cornea 2016, 35, 1537–1541. [Google Scholar] [CrossRef]
- Li, J.Y.; Terry, M.A.; Goshe, J.; Davis-Boozer, D.; Shamie, N. Three-year visual acuity outcomes after Descemet’s stripping automated endothelial keratoplasty. Ophthalmology 2012, 119, 1126–1129. [Google Scholar] [CrossRef]
- Wacker, K.; Baratz, K.H.; Maguire, L.J.; McLaren, J.W.; Patel, S.V. Descemet Stripping Endothelial Keratoplasty for Fuchs’ Endothelial Corneal Dystrophy: Five-Year Results of a Prospective Study. Ophthalmology 2016, 123, 154–160. [Google Scholar] [CrossRef]
- Ezon, I.; Shih, C.Y.; Rosen, L.M.; Suthar, T.; Udell, I.J. Immunologic graft rejection in descemet’s stripping endothelial keratoplasty and penetrating keratoplasty for endothelial disease. Ophthalmology 2013, 120, 1360–1365. [Google Scholar] [CrossRef] [PubMed]
- Hamzaoglu, E.C.; Straiko, M.D.; Mayko, Z.M.; Sáles, C.S.; Terry, M.A. The First 100 Eyes of Standardized Descemet Stripping Automated Endothelial Keratoplasty versus Standardized Descemet Membrane Endothelial Keratoplasty. Ophthalmology 2015, 122, 2193–2199. [Google Scholar] [CrossRef]
- Wu, E.I.; Ritterband, D.C.; Yu, G.; Shields, R.A.; Seedor, J.A. Graft rejection following descemet stripping automated endothelial keratoplasty: Features, risk factors, and outcomes. Am. J. Ophthalmol. 2012, 153, 949–957. [Google Scholar] [CrossRef]
- Tourtas, T.; Laaser, K.; Bachmann, B.O.; Cursiefen, C.; Kruse, F.E. Descemet membrane endothelial keratoplasty versus descemet stripping automated endothelial keratoplasty. Am. J. Ophthalmol. 2012, 153, 1082–1090.e2. [Google Scholar] [CrossRef]
- Dickman, M.M.; Kruit, P.J.; Remeijer, L.; van Rooij, J.; Van der Lelij, A.; Wijdh, R.H.; Biggelaar, F.J.v.D.; Berendschot, T.T.; Nuijts, R.M. A Randomized Multicenter Clinical Trial of Ultrathin Descemet Stripping Automated Endothelial Keratoplasty (DSAEK) versus DSAEK. Ophthalmology 2016, 123, 2276–2284. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.H.; Ang, M.; Htoon, H.M.; Tan, D. Descemet Membrane Endothelial Keratoplasty Versus Descemet Stripping Automated Endothelial Keratoplasty and Penetrating Keratoplasty. Am. J. Ophthalmol. 2019, 207, 288–303. [Google Scholar] [CrossRef] [PubMed]
- Maier, A.-K.; Gundlach, E.; Gonnermann, J.; Klamann, M.K.J.; Bertelmann, E.; Rieck, P.W.; Joussen, A.M.; Torun, N. Retrospective contralateral study comparing Descemet membrane endothelial keratoplasty with Descemet stripping automated endothelial keratoplasty. Eye 2015, 29, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Heinzelmann, S.; Böhringer, D.; Eberwein, P.; Reinhard, T.; Maier, P. Outcomes of Descemet membrane endothelial keratoplasty, Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty from a single centre study. Graefe’s Arch. Clin. Exp. Ophthalmol. Albrecht Von Graefes Arch. Fur Klin. Exp. Ophthalmol. 2016, 254, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Guerra, F.P.; Anshu, A.; Price, M.O.; Price, F.W. Endothelial keratoplasty: Fellow eyes comparison of descemet stripping automated endothelial keratoplasty and descemet membrane endothelial keratoplasty. Cornea 2011, 30, 1382–1386. [Google Scholar] [CrossRef] [PubMed]
- Gorovoy, M.S. Descemet-Stripping Automated Endothelial Keratoplasty. Cornea 2021, 40, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, W.; Lin, C.C.; Austin, A.; Schubach, N.; Clover, J.; McLeod, S.D.; Porco, T.C.; Lietman, T.M.; Rose-Nussbaumer, J. Descemet Endothelial Thickness Comparison Trial: A Randomized Trial Comparing Ultrathin Descemet Stripping Automated Endothelial Keratoplasty with Descemet Membrane Endothelial Keratoplasty. Ophthalmology 2019, 126, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Dunker, S.L.; Dickman, M.M.; Wisse, R.P.; Nobacht, S.; Wijdh, R.H.; Bartels, M.C.; Tang, M.L.; Biggelaar, F.J.v.D.; Kruit, P.J.; Nuijts, R.M. Descemet Membrane Endothelial Keratoplasty versus Ultrathin Descemet Stripping Automated Endothelial Keratoplasty: A Multicenter Randomized Controlled Clinical Trial. Ophthalmology 2020, 127, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Madi, S.; Leon, P.; Nahum, Y.; D‘Angelo, S.; Giannaccare, G.; Beltz, J.; Busin, M. Five-Year Outcomes of Ultrathin Descemet Stripping Automated Endothelial Keratoplasty. Cornea 2019, 38, 1192–1197. [Google Scholar] [CrossRef]
- Matsou, A.M.; Pujari, R.M.; Sarwar, H.F.; Rana, M.M.; Myerscough, J.M.; Thomson, S.M.B.; Nandakumar, G.B.; Zhang, J.; Rajan, M.S.M. Microthin Descemet Stripping Automated Endothelial Keratoplasty Versus Descemet Membrane Endothelial Keratoplasty: A Randomized Clinical Trial. Cornea 2021, 40, 1117–1125. [Google Scholar] [CrossRef]
- Hos, D.; Tuac, O.; Schaub, F.; Stanzel, T.P.; Schrittenlocher, S.; Hellmich, M.; Bachmann, B.O.; Cursiefen, C. Incidence and Clinical Course of Immune Reactions after Descemet Membrane Endothelial Keratoplasty: Retrospective Analysis of 1000 Consecutive Eyes. Ophthalmology 2017, 124, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Ham, L.; Dapena, I.; Liarakos, V.S.; Baydoun, L.; van Dijk, K.; Ilyas, A.; Oellerich, S.; Melles, G.R. Midterm Results of Descemet Membrane Endothelial Keratoplasty: 4 to 7 Years Clinical Outcome. Am. J. Ophthalmol. 2016, 171, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Peraza-Nieves, J.; Baydoun, L.; Dapena, I.; Ilyas, A.; Frank, L.E.; Luceri, S.; Ham, L.; Oellerich, S.; Melles, G.R.J. Two-Year Clinical Outcome of 500 Consecutive Cases Undergoing Descemet Membrane Endothelial Keratoplasty. Cornea 2017, 36, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Quilendrino, R.; de Mora, M.R.-C.; Baydoun, L.; Ham, L.; van Dijk, K.; Dapena, I.; Oellerich, S.; Melles, G.R.J. Prevention and Management of Descemet Membrane Endothelial Keratoplasty Complications. Cornea 2017, 36, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.X.; Seitz, B.; Martus, P.; Langenbucher, A.; Cursiefen, C. Long-term topical steroid treatment improves graft survival following normal-risk penetrating keratoplasty. Am. J. Ophthalmol. 2007, 144, 318–319. [Google Scholar] [CrossRef] [PubMed]
- Fiorentzis, M.; Viestenz, A.; Seitz, B. [Immunological graft rejection with Khodadoust line after “Descemet stripping automated endothelial keratoplasty” (DSAEK)]. Ophthalmol. Z. Dtsch. Ophthalmol. Ges. 2015, 112, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Jordan, C.S.; Price, M.O.; Trespalacios, R.; Price, F.W. Graft rejection episodes after Descemet stripping with endothelial keratoplasty: Part one: Clinical signs and symptoms. Br. J. Ophthalmol. 2009, 93, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Saelens, I.E.Y.; Bleyen, I.; Bartels, M.C.; Van Rij, G. A posterior khodadoust line in a graft rejection episode after descemet stripping automated endothelial keratoplasty. Cornea 2011, 30, 245–246. [Google Scholar] [CrossRef] [PubMed]
- Price, M.O.; Gupta, P.; Lass, J.; Price, F.W. EK (DLEK, DSEK, DMEK): New Frontier in Cornea Surgery. Annu. Rev. Vis. Sci. 2017, 3, 69–90. [Google Scholar] [CrossRef]
- Koenig, S.B.; Covert, D.J.; Dupps, W.J.; Meisler, D.M. Visual acuity, refractive error, and endothelial cell density six months after Descemet stripping and automated endothelial keratoplasty (DSAEK). Cornea 2007, 26, 670–674. [Google Scholar] [CrossRef]
- Busin, M.; Yu, A.C. The Ongoing Debate: Descemet Membrane Endothelial Keratoplasty Versus Ultrathin Descemet Stripping Automated Endothelial Keratoplasty. Ophthalmology 2020, 127, 1160–1161. [Google Scholar] [CrossRef] [PubMed]
- Stuart, A.J.; Romano, V.; Virgili, G.; Shortt, A.J. Descemet’s membrane endothelial keratoplasty (DMEK) versus Descemet’s stripping automated endothelial keratoplasty (DSAEK) for corneal endothelial failure. Cochrane Database Syst. Rev. 2018, 6, CD012097. [Google Scholar] [CrossRef]
- Koechel, D.; Hofmann, N.; Unterlauft, J.D.; Wiedemann, P.; Girbardt, C. Descemet membrane endothelial keratoplasty (DMEK): Clinical results of precut versus surgeon-cut grafts. Graefe’s Arch. Clin. Exp. Ophthalmol. Albrecht Von Graefes Arch. Fur Klin. Exp. Ophthalmol. 2021, 259, 113–119. [Google Scholar] [CrossRef]
- Dapena, I.; Ham, L.; Melles, G.R.J. Endothelial keratoplasty: DSEK/DSAEK or DMEK--the thinner the better? Curr. Opin. Ophthalmol. 2009, 20, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Bucher, F.; Hos, D.; Müller-Schwefe, S.; Steven, P.; Cursiefen, C.; Heindl, L.M. Spontaneous long-term course of persistent peripheral graft detachments after Descemet’s membrane endothelial keratoplasty. Br. J. Ophthalmol. 2015, 99, 768–772. [Google Scholar] [CrossRef]
- Fritz, M.; Grewing, V.; Böhringer, D.; Lapp, T.; Maier, P.; Reinhard, T.; Wacker, K. Avoiding Hyperopic Surprises After Descemet Membrane Endothelial Keratoplasty in Fuchs Dystrophy Eyes by Assessing Corneal Shape. Am. J. Ophthalmol. 2019, 197, 1–6. [Google Scholar] [CrossRef]
- Deng, S.X.; Lee, W.B.; Hammersmith, K.M.; Kuo, A.N.; Li, J.Y.; Shen, J.F.; Weikert, M.P.; Shtein, R.M. Descemet Membrane Endothelial Keratoplasty: Safety and Outcomes: A Report by the American Academy of Ophthalmology. Ophthalmology 2018, 125, 295–310. [Google Scholar] [CrossRef]
- Droutsas, K.; Lazaridis, A.; Papaconstantinou, D.; Brouzas, D.; Moschos, M.M.; Schulze, S.; Sekundo, W. Visual Outcomes After Descemet Membrane Endothelial Keratoplasty Versus Descemet Stripping Automated Endothelial Keratoplasty-Comparison of Specific Matched Pairs. Cornea 2016, 35, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, B.O.; Pogorelov, P.; Kruse, F.E.; Cursiefen, C. [Patient satisfaction after posterior lamellar keratoplasty (DSAEK)]. Klin. Monatsblatter Augenheilkd. 2008, 225, 577–581. [Google Scholar] [CrossRef]
- Baydoun, L.; Dapena, I.; Melles, G. Evolution of Posterior Lamellar Keratoplasty: PK–DLEK–DSEK/DSAEK–DMEK–DMET. In Current Treatment Options for Fuchs Endothelial Dystrophy; Springer: Cham, Switzerland, 2017; pp. 73–85. [Google Scholar] [CrossRef]
- Jamali, A.; Kenyon, B.; Ortiz, G.; Abou-Slaybi, A.; Sendra, V.G.; Harris, D.L.; Hamrah, P. Plasmacytoid dendritic cells in the eye. Prog. Retin. Eye Res. 2021, 80, 100877. [Google Scholar] [CrossRef]
- Anshu, A.; Price, M.O.; Price, F.W. Risk of corneal transplant rejection significantly reduced with Descemet’s membrane endothelial keratoplasty. Ophthalmology 2012, 119, 536–540. [Google Scholar] [CrossRef] [PubMed]
| Study | Year | Eyes | Design | Evidence Level |
|---|---|---|---|---|
| DSAEK | ||||
| Allan et al. [21] | 2007 | 199 | Retrospective case series | 4 |
| Li et al. [22] | 2012 | 615 | Retrospective case series | 4 |
| Price et al. [23] | 2009 | 598 | Retrospective study | 4 |
| Sepsakos et al. [24] | 2016 | 400 | Retrospective study | 4 |
| Li et al. [25] | 2011 | 108 | Retrospective case series | 4 |
| Wacker et al. [26] | 2016 | 49 | Prospective clinical trial | 1c |
| Ezon et al. [27] | 2013 | 122 | Retrospective study | 4 |
| Hamzaoglu et al. [28] | 2015 | 100 | Retrospective case series | 4 |
| Wu et al. [29] | 2012 | 353 | Retrospective case series | 4 |
| Tourtas et al. [30] | 2012 | 35 | Retrospective case series | 4 |
| Dickman et al. [31] | 2016 | 32 | Randomized controlled clinical trial | 1b |
| Woo et al. [32] | 2019 | 423 | Retrospective study | 4 |
| Maier et al. [33] | 2015 | 10 | Retrospective study | 4 |
| Heinzelmann et al. [34] | 2016 | 89 | Retrospective study | 4 |
| Guerra et al. [35] | 2011 | 15 | Retrospective case series | 4 |
| Gorovoy et al. [36] | 2021 | 16 | Retrospective study | 4 |
| UT-DSAEK | ||||
| Chamberlain et al. [37] | 2019 | 25 | Randomized controlled clinical trial | 1b |
| Dunker et al. [38] | 2020 | 25 | Randomized controlled clinical trial | 1b |
| Madi et al. [39] | 2019 | 354 | Retrospective case series | 4 |
| Dickman et al. [31] | 2016 | 34 | Randomized controlled clinical trial | 1b |
| Matsou et al. [40] | 2021 | 28 | Randomized controlled clinical trial | 1b |
| DMEK | ||||
| Dunker et al. [38] | 2020 | 29 | Randomized controlled clinical trial | 1b |
| Hos et al. [41] | 2017 | 1000 | Retrospective case series | 4 |
| Hamzaoglu et al. [28] | 2015 | 100 | Retrospective case series | 4 |
| Tourtas et al. [30] | 2012 | 38 | Retrospective case series | 4 |
| Ham et al. [42] | 2016 | 250 | Retrospective case series | 4 |
| Peraza-Nieves et al. [43] | 2017 | 500 | Retrospective case series | 4 |
| Quilendrino et al. [44] | 2017 | 500 | Retrospective study | 4 |
| Chamberlain et al. [37] | 2019 | 25 | Randomized controlled clinical trial | 1b |
| Woo et al. [32] | 2019 | 121 | Retrospective cohort study | 2b |
| Maier et al. [33] | 2015 | 10 | Retrospective study | 4 |
| Heinzelmann et al. [34] | 2016 | 450 | Retrospective study | 4 |
| Guerra et al. [35] | 2011 | 15 | Retrospective case series | 4 |
| Matsou et al. [40] | 2021 | 28 | Randomized controlled clinical trial | 1b |
| Treatment | Rejection Rate 1 Year | Rejection Rate > 2 Year | Re-Bubbling Rate | BSCVA > 20/30 | BSCVA 20/20 | Success Rate 6 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % (C.I) | n/eyes | % (C.I) | n/eyes | % (C.I) | n/eyes | % (C.I) | n/eyes | % (C.I) | n/eyes | % (C.I) | n/eyes | |
| DSAEK | 5 (2–7) | 163/2735 | 13 (6–20) | 200/1562 | 7 (0–15) | 15/599 | 37 (14–60) | 127/267 | 21 (2–39) | 62/199 | 12 (7–17) | 20/170 |
| UT-DSAEK | 3 (1–4) | 15/466 | 4 (2–6) | 17/432 | 65 (2–100) | 350/379 | 29 (0–77) | 190/379 | ||||
| DMEK | 1 (1–1) | 31/2568 | 4 (0–9) | 54/1450 | 20 (6–35) | 124/1616 | 72 (62–82) | 712/900 | 45 (35–55) | 439/862 | 41 (38–45) | 354/849 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spelta, S.; Micera, A.; Gaudenzi, D.; Niutta, M.; Surico, P.L.; De Vincentis, A.; Coassin, M.; Di Zazzo, A. A Functional and Immunologic Point of View on Corneal Endothelial Transplantation: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 3431. https://doi.org/10.3390/jcm13123431
Spelta S, Micera A, Gaudenzi D, Niutta M, Surico PL, De Vincentis A, Coassin M, Di Zazzo A. A Functional and Immunologic Point of View on Corneal Endothelial Transplantation: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(12):3431. https://doi.org/10.3390/jcm13123431
Chicago/Turabian StyleSpelta, Sara, Alessandra Micera, Daniele Gaudenzi, Matteo Niutta, Pier Luigi Surico, Antonio De Vincentis, Marco Coassin, and Antonio Di Zazzo. 2024. "A Functional and Immunologic Point of View on Corneal Endothelial Transplantation: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 12: 3431. https://doi.org/10.3390/jcm13123431
APA StyleSpelta, S., Micera, A., Gaudenzi, D., Niutta, M., Surico, P. L., De Vincentis, A., Coassin, M., & Di Zazzo, A. (2024). A Functional and Immunologic Point of View on Corneal Endothelial Transplantation: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(12), 3431. https://doi.org/10.3390/jcm13123431







