1. Introduction
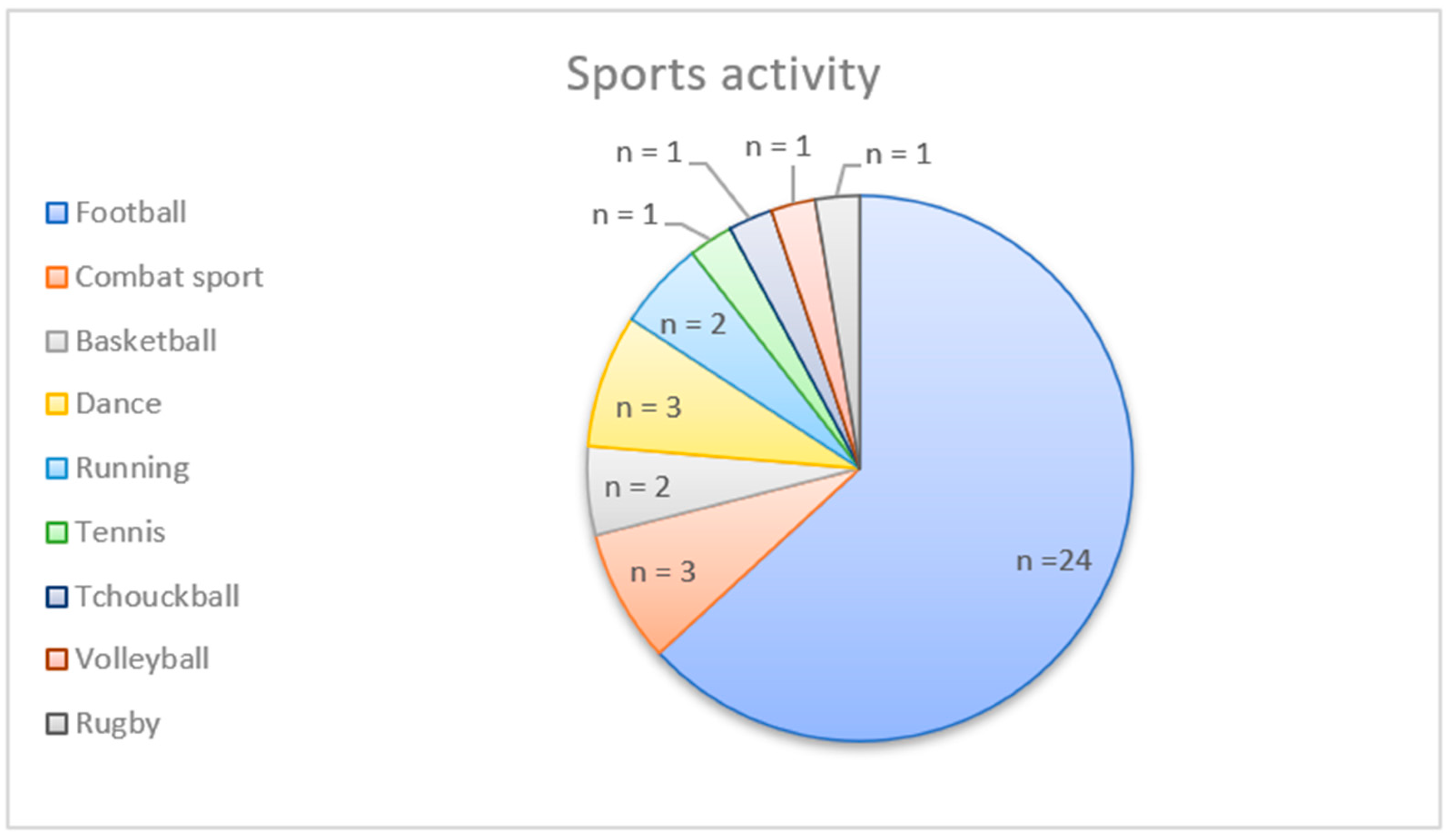
ACL injuries are among the most common and significant knee injuries in sports. These injuries are particularly common in young and active individuals participating in sports that involve jumping, pivoting, and changing direction, such as football and basketball [
1]. Approximately 3% of amateur athletes sustain an ACL injury each year [
2]. Return to sport (RTS) is the primary goal following anterior cruciate ligament reconstruction (ACLR) [
3]. In amateur athletes, only 65% of the patients return to their pre-injury level of sport two years after ACLR [
4]. The risk of a second ACL injury in athletes is high, up to 20–23% [
5]. RTS decision-making after ACLR is challenging, as current evidence shows a conflicting relationship between RTS criteria and the potential risk of a second ACL injury [
6,
7,
8]. For example, Webster and Hewett (2019) found no significant association between passing the return to sport (RTS) criteria and a reduced rate of subsequent ACL injury [
7]. However, Capin et al. (2019) re-analyzed the data, excluding two inappropriate studies, and found that athletes who met the RTS criteria had a 75% lower risk of ACL injury than those who did not meet the criteria [
6]. A criterion-based approach has also become mandatory [
9,
10,
11]. In order to assess readiness for RTS, important functional parameters should be measured, such as functional capacity through lower limb strength, psychological readiness, hop testing, and measurement of movement quality [
10,
12]. Indeed, greater quadriceps strength is associated with effective RTS and a reduction in subsequent knee injuries, and psychological readiness is known to be a reason for not returning to play in 65% of cases [
13,
14,
15,
16]. Meeting qualitative movement criteria is associated with a lower rate of second ACL injury when returning to pivoting sports [
17]. With regard to hop tests, the available evidence suggests a lack of consistency in their ability to predict safe RTS [
18].
The side hop test (SHT) consists of jumping on one leg from side to side for 30 s between two parallel bands 40 cm apart [
19]. The maximum number of hops is recorded and usually compared to the non-operated (NOP) limb and described by the limb symmetry index (LSI). Several relevant aspects are tested during the SHT, such as plyometric and side cutting movements with an endurance component, both of which are known to be highly associated with ACL injury risk due to transient poor knee control in a relatively straight, abducted, and rotated knee position [
20]. As described for other hop tests, the use of the number of hops alone does not provide complete information, as it does not guarantee unaltered or symmetrical jump biomechanics and does not consider variables related to the test execution strategy, such as spatiotemporal parameters that are not obvious to the clinician’s visual perception [
21,
22]. Currently, there are very few studies evaluating spatiotemporal parameters during hop tests [
23,
24,
25]. Mani et al. (2017) showed significant discriminant validity (between the involved and uninvolved sides) for both mean contact time and hop distance for a hop test consisting of four consecutive forward hops [
23]. Ahmadian et al. (2020) showed no significant difference in spatiotemporal parameters during a triple hop test (consisting of three consecutive forward hops), although they demonstrated differences in hop biomechanics between healthy and injured participants [
24]. To our knowledge, there are no studies on the psychometric properties of these parameters for clinical use.
The aim of this study is to investigate the reliability and validity of temporal parameters of the SHT using a video analysis system in ACLR patients. We hypothesized that the operated (OP) leg would have a longer mean contact time and greater variability in temporal parameters compared to the NOP leg and would not be associated with LSI values of the number of valid hops. Patients with a longer mean contact time or higher variability will show a moderate correlation with the strength and the ACL–RSI scale.
4. Discussion
This study is the first to analyze temporal parameters of the SHT, such as variability, and compare them with other important clinical parameters, such as leg strength, using an affordable and clinician-friendly 2D video analysis system.
The aim of this study was to investigate the reliability and validity of temporal parameters of the SHT in ACLR patients. Measures of temporal parameters of the 30 s SHT showed good to excellent intra-tester reliability. As discriminate factors, mean and SD contact times were significantly longer in the OP leg compared to the NOP leg. These results should be interpreted with caution, as the mean difference did not exceed the MDC and SEM values. This means that the observed change may be partially explained by measurement error or random variation. However, the number of valid hops and CV contact time had no discriminative value. Quadriceps and hamstring strength showed a strong to moderate negative correlation with mean and SD contact time for both legs, whereas psychological readiness was not correlated with any contact time parameter.
The results of this study revealed differences in performance between the OP and NOP in terms of strategies for performing the SHT. Temporal parameters have better psychometric properties than the number of valid jumps. The number of jumps had no discriminating value, whereas the temporal parameters seem to be more discriminating and sensitive to changes.
The average number of valid jumps (35–56 hops) and LSI score (93–99%) reported in the literature are similar to this study [
36,
37,
38,
39,
40,
41,
42]. However, performance is not in line with healthy normative values (55–57 jumps with an average LSI value of 100%) [
42].
Participants in this study had difficulty maintaining a consistent rhythm during the SHT on their OP, as the overall SD and corresponding LSI difference were able to discriminate limb differences. These results show that the stabilization time on the OP leg can vary from jump to jump; although some jumps were fast, others required a longer stabilization time. A longer stabilization time can be explained by an adjustment jump or a loss of balance. This means that participants had more difficulty maintaining a consistent rhythm on their OP leg during the SHT. However, the patient’s strategy can significantly influence the results. If the pace is slowed down or more invalid hops are made to reduce the difficulty, the results in this study may be less variable than expected.
When comparing the endurance components of the SHT, a similar decrease in temporal parameters was recorded for both legs, with no leg difference when comparing the performance of the first and last ten seconds. It is possible that the duration of the test is not long enough to cause fatigue and discriminate between the two legs in terms of endurance components.
In this study, the inter-individual differences between valid hops and temporal parameters were very high. Several patients performed some adjustment jumps (several small hops on one side), which significantly increased the value of the contact time parameters. This indicates a poor stabilization strategy and, therefore, poor motor control or fatigue.
In terms of convergent validity, low scores on the number of valid hops and higher mean and SD contact times were associated with low quadriceps or hamstring strength. The correlation was slightly stronger for the quadriceps, probably because most of the patients received a quadricipital or patellar graft on the OP leg, and therefore, the strength for this muscle was lowest. These findings are consistent with those of Thomas et al. (2015), who found that maximum force production during isometric mid-thigh pull correlated with change of direction (COD) ability in athletes [
43].
However, the temporal parameters of the SHT were not correlated with subjective psychological readiness. As the questionnaire is not specific to the SHT task but to return to a sport defined by the patient, it would be interesting to be more specific and directly measure anxiety during the SHT and the level of anxiety related to specific tasks such as cutting maneuvers.
In terms of confounders, it is interesting to note that the participant’s height was weakly correlated with CV contact time in both legs, suggesting that reduced height increases variability in contact time due to increased difficulty in performing the test. Higher variability may be the result of greater difficulty in performing the test. It would, therefore, be interesting to propose a SHT with a width between the bands that is proportional to the size of the participants’ lower limbs.
If we compare these results with the study by Urhausen et al. (2022), they found no significant differences in the number of jumps or temporal parameters [
25]. However, the characteristics of their participants are different from those in this study. The SHT in our study was performed, on average, 1.4 months earlier, and our participants had a majority of quadriceps tendon grafts (instead of semi-tendinous grafts in their study). In addition, their reported rate of invalid hops (0.2%) was lower than in this study (8–9%). Probably due to the early testing, our participants perceived more difficulty in performing the test and may have a different execution strategy. On the one hand, an invalid hop may lead to a shorter contact time because the effort was less difficult than required. On the other hand, it is also possible that the effort was too difficult, and therefore, a longer stabilization time followed due to a lack of balance.
Strength and Limitations
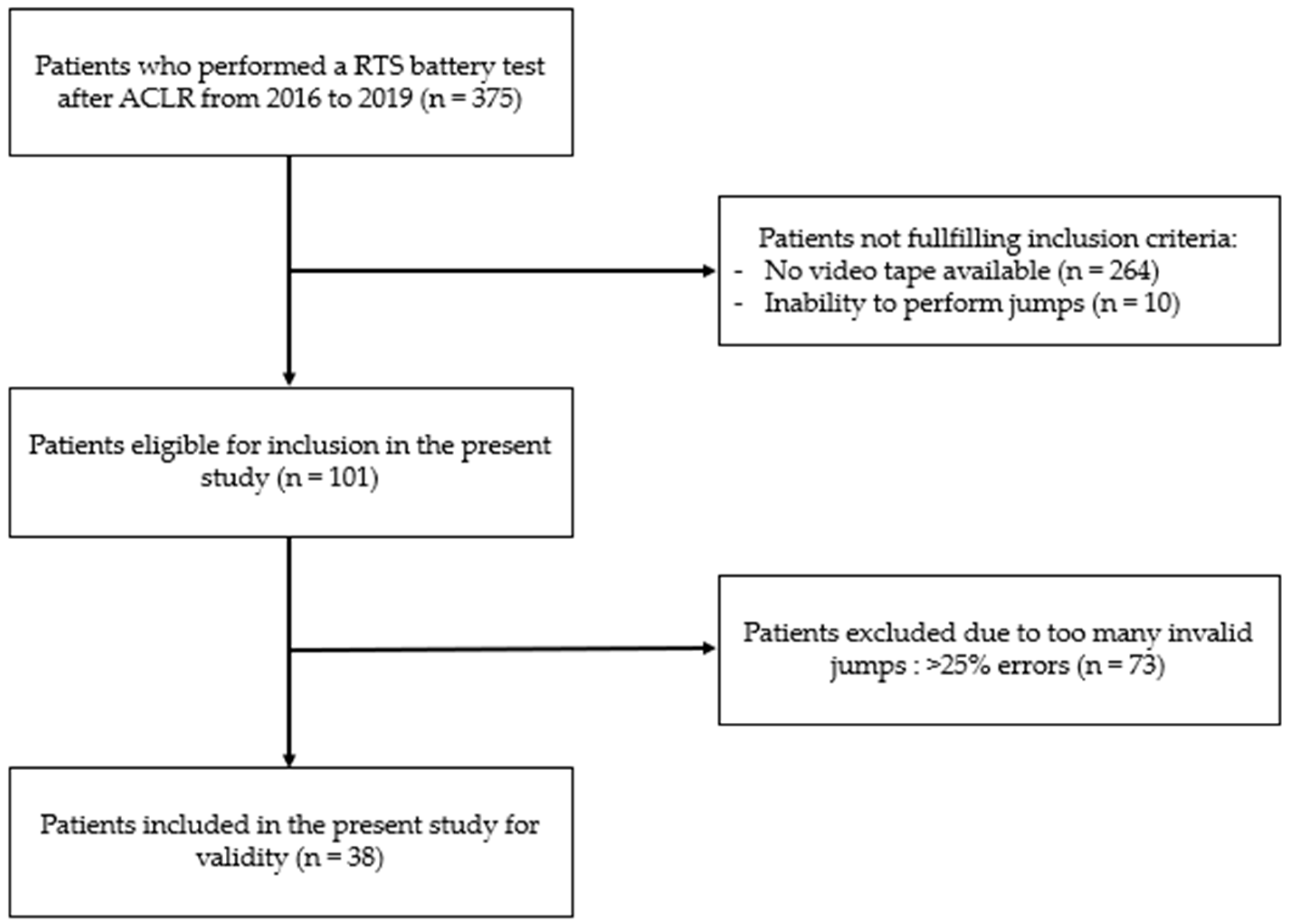
The first major limitation is the large standard deviation of all contact time results, which reflects the heterogeneity of SHT performance in the population of this study, although patients with too many invalid jumps were excluded from the analysis.
The second main limitation of this study was that the criterion validity of the video measurement was not measured. It is possible that the accuracy of the measurement device does not allow enough difference in the temporal parameters between the legs to determine adequate variability. The mean would probably not change much, and the SD would remain high, but the coefficient of variation is very sensitive to variations in numbers. Temporal parameters are probably more important than the number of valid jumps performed. However, a standard 50Hz camera may be inadequate, as the potential error is 8% due to the large time frame. The 8% is explained by the difference in measurement when the evaluator hesitates between 2 frames to determine the 1st ground contact. Therefore, better cameras with 200 frames/second could improve the measurement accuracy.
In addition, the average time taken to obtain time parameter data from an individual in this study was around 10 min. The use of other tools, such as inertial measurement units, force plates, or even artificial intelligence, would significantly reduce the measurement time, which would be of great benefit to clinicians. An in-depth analysis of the measurement properties of this tool should be carried out.
Another potential bias in this study was the use of a paired statistical test. As the results compared data of both legs of each individual, the data were considered as paired. However, the assumption of symmetry between the legs is questionable. Differences such as the presence of a dominant leg or medical history can influence asymmetry.
Finally, as the participants had no pre-operative values, this study assessed the limb asymmetry of participants having undergone unilateral ACLR regarding the number of valid jumps and temporal parameters. However, deficit after ACLR is also common in the NOP leg, and the limb symmetry index may overestimate the hop performance [
44]. This makes it difficult to assess the responsiveness of the test. Further studies are needed to assess these parameters in healthy control subjects or compare the results with pre-operative values.