Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations
Abstract
1. Introduction
2. Materials and Methods
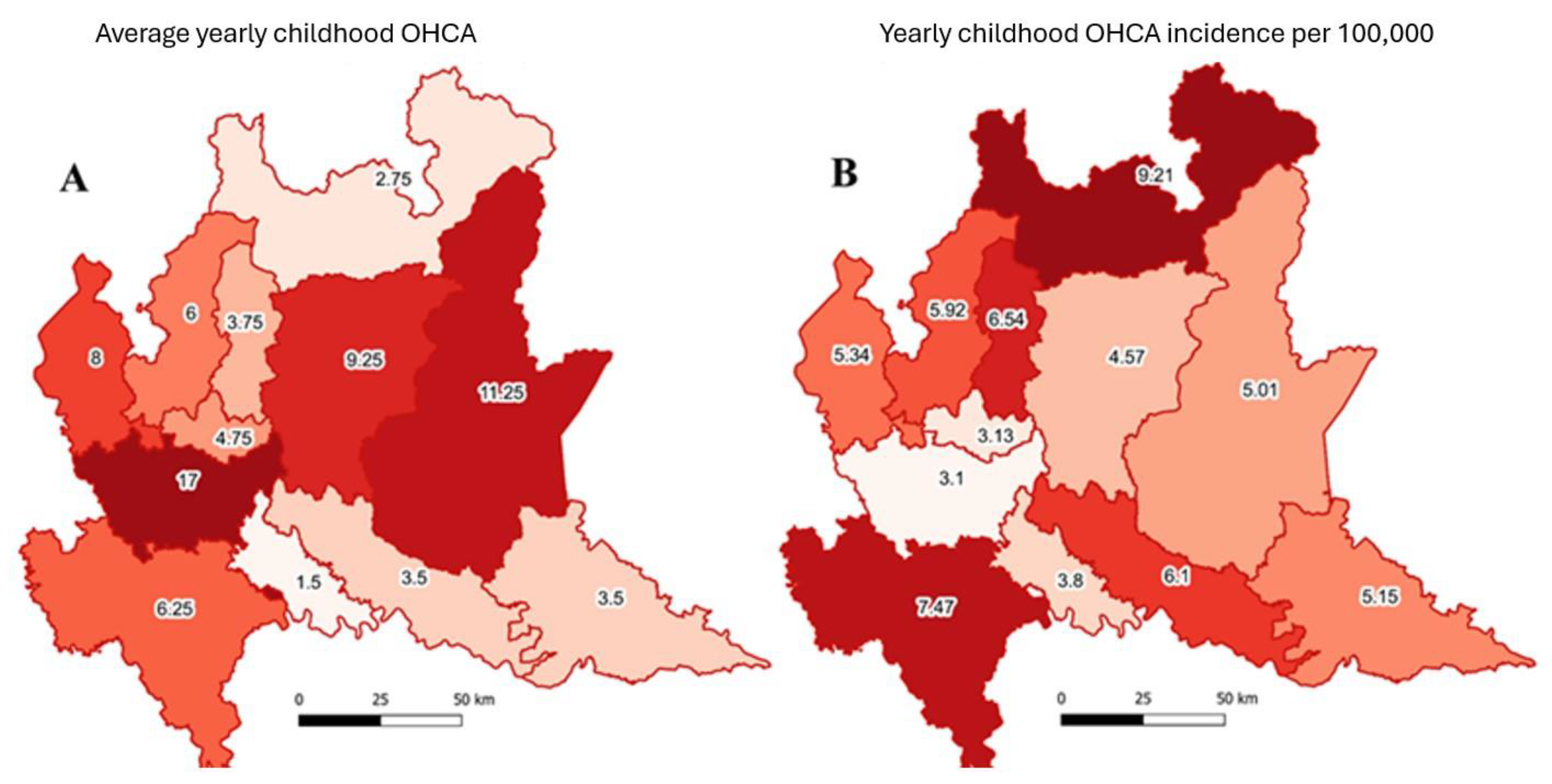
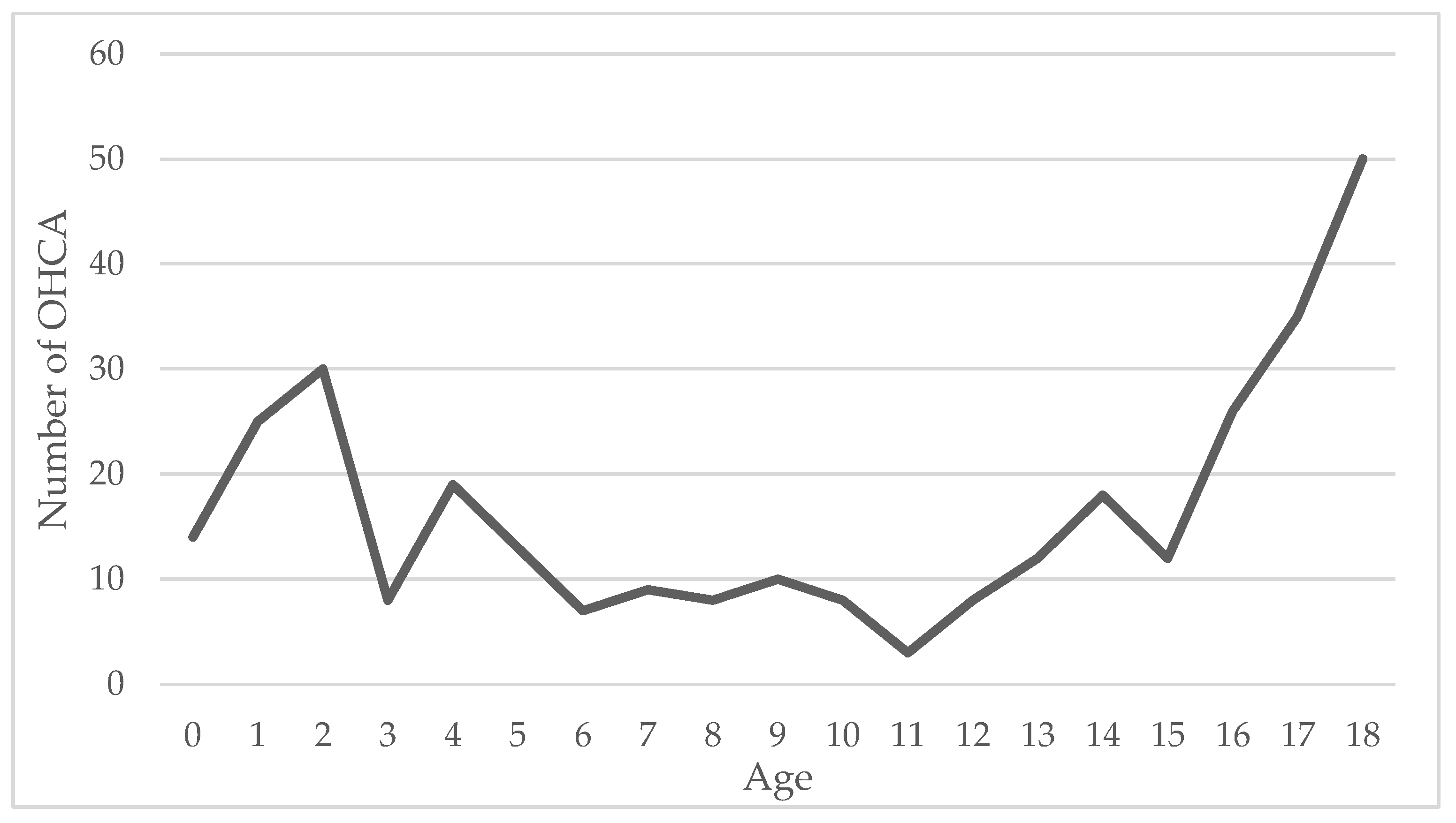
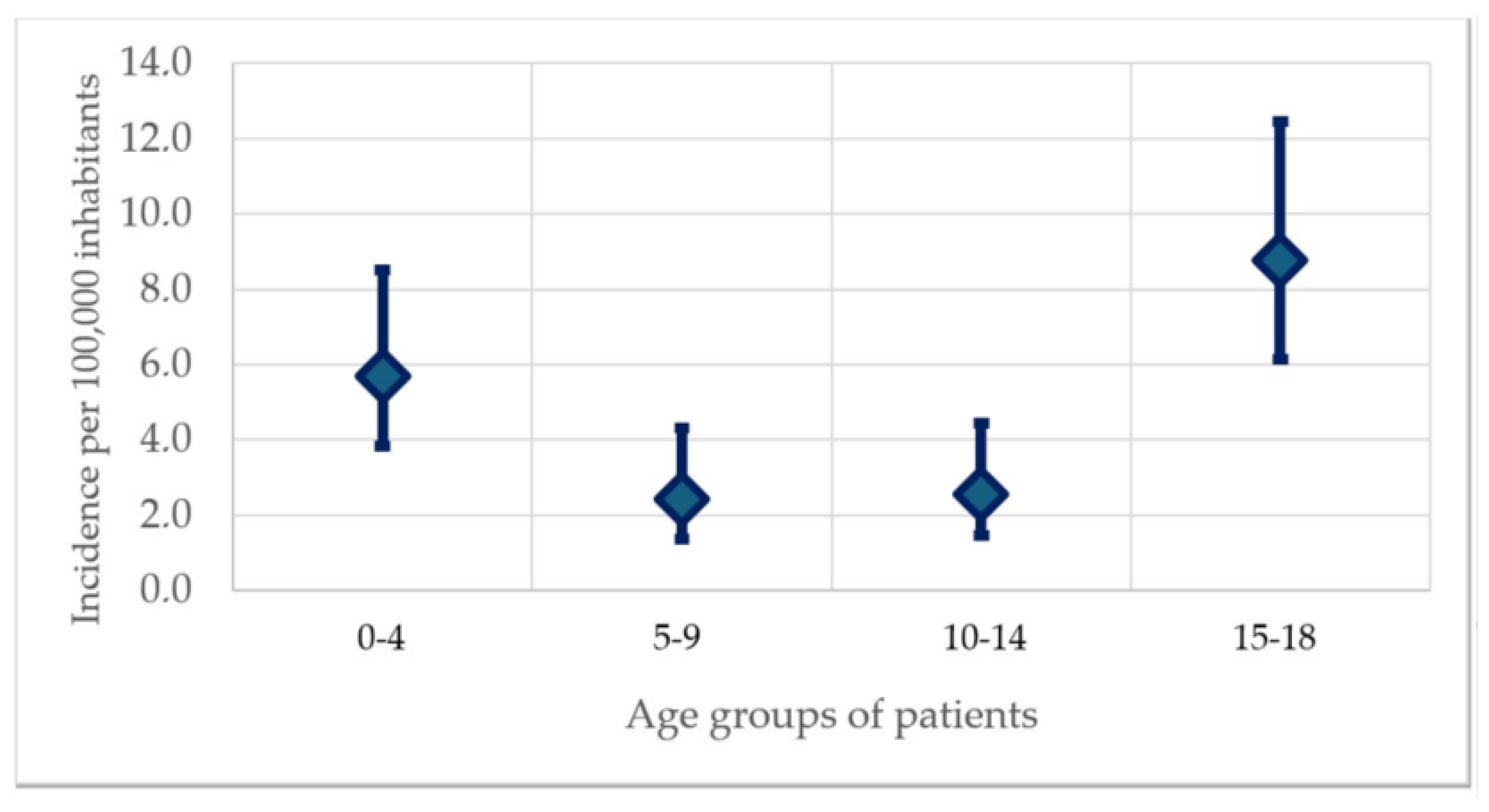
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Myat, A.; Song, K.J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Callaway, C.W.; Guyette, F.X.; Rittenberger, J.C.; Doshi, A.A.; Dezfulian, C.; Elmer, J. Pittsburgh Post-Cardiac Arrest Service. Arrest etiology among patients resuscitated from cardiac arrest. Resuscitation 2018, 130, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.L.; Berger, S.; Duff, J.P.; Gonzales, J.C.; Hunt, E.A.; Joyner, B.L.; Meaney, P.A.; Niles, D.E.; Samson, R.A.; Schexnayder, S.M. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132 (Suppl. S2), S519–S525. [Google Scholar] [CrossRef] [PubMed]
- Važanić, D.; Prkačin, I.; Nesek-Adam, V.; Kurtović, B.; Rotim, C. Out-Of-Hospital Cardiac Arrest Outcomes—Bystander Cardiopulmonary Resuscitation Rate Improvement. Acta Clin. Croat. 2022, 61, 265–272. [Google Scholar] [CrossRef] [PubMed]
- LEGGE 4 Agosto 2021, n. 116. Disposizioni in Materia di Utilizzo dei Defibrillatori Semiautomatici e Automatici. (21G00126) (GU Serie Generale n.193 del 13-08-2021). Available online: https://www.gazzettaufficiale.it/eli/id/2021/08/13/21G00126/sg (accessed on 2 January 2023).
- Stirparo, G.; Gambolò, L.; Bellini, L.; Medioli, F.; Bertuol, M.; Guasconi, M.; Sulla, F.; Artioli, G.; Sarli, L. Satisfaction evaluation for ACLS training. Acta Biomed. 2022, 93, e2022260. [Google Scholar] [CrossRef] [PubMed]
- Giuseppe, S.; Bellini, L.; Fagoni, N.; Compatti, S.; Botteri, M.; Villa, G.F.; Sironi, S.; Signorelli, C.; Sechi, G.M.; Zoli, A. Missed training, collateral damage from COVID-19? Disaster Med. Public Health Prep. 2022, 16, 2403–2405. [Google Scholar] [CrossRef]
- Stirparo, G.; Pireddu, R.; Kacerik, E.; Scognamiglio, T.; Andreassi, A.; Sechi, G.M.; Zoli, A.; Signorelli, C. Stroke and the need for immediate assistance at the place of onset: The future of mandatory training for lay people in Italy. Ann. Ig. 2023, 35, 480–485. [Google Scholar] [CrossRef]
- Oliveira, K.M.G.; Carmona, M.J.C.; Mansur, A.P.; Takada, J.Y.; Fijačko, N.; Semeraro, F.; Lockey, A.; Böttiger, B.W.; Nakagawa, N.K. CPR Quality Assessment in Schoolchildren Training. J. Cardiovasc. Dev. Dis. 2022, 9, 398. [Google Scholar] [CrossRef]
- Winkle, R.A. The effectiveness and cost effectiveness of public-access defibrillation. Clin. Cardiol. 2010, 33, 396–399. [Google Scholar] [CrossRef]
- Scapigliati, A.; Zace, D.; Matsuyama, T.; Pisapia, L.; Saviani, M.; Semeraro, F.; Ristagno, G.; Laurenti, P.; Bray, J.E.; Greif, R.; et al. Community Initiatives to Promote Basic Life Support Implementation-A Scoping Review. J. Clin. Med. 2021, 10, 5719. [Google Scholar] [CrossRef]
- Lorenzo, G.; Maria Antonia, B.; Piero Maria, B.; Andrea, P.; Guido Francesco, V.; Enrico Gianluca, C. Development of a Novel Framework to Propose New Strategies for Automated External Defibrillators Deployment Targeting Residential Out-Of-Hospital Cardiac Arrests: Application to the City of Milan. ISPRS Int. J. Geo-Inf. 2020, 9, 491. [Google Scholar] [CrossRef]
- Birkun, A.; Baldi, E.; Böttiger, B.W. Public interest in cardiac arrest and cardiopulmonary resuscitation: A Google Trends analysis of global online search traffic. Eur. J. Emerg. Med. 2022, 29, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Michelson, K.A.; Hudgins, J.D.; Monuteaux, M.C.; Bachur, R.G.; Finkelstein, J.A. Cardiac Arrest Survival in Pediatric and General Emergency Departments. Pediatrics 2018, 141, e20172741. [Google Scholar] [CrossRef] [PubMed]
- Ng, Z.H.C.; Ho, S.J.; Caleb, T.; Yaow, C.Y.L.; Teoh, S.E.; Tham, L.P.; Ong, M.E.H.; Chong, S.L.; Ho, A.F.W. Long-Term Outcomes after Non-Traumatic Out-of-Hospital Cardiac Arrest in Pediatric Patients: A Systematic Review. J. Clin. Med. 2022, 11, 5003. [Google Scholar] [CrossRef] [PubMed]
- Irvine, R.; Doan, T.; Bosley, E.; Colbeck, M.; Bowles, K.A. Pediatric Out-of-Hospital Cardiac Arrests: An Epidemiological Study. Prehosp. Emerg. Care 2022, 27, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.H.; Juan, I.C.; Hsu, H.Y.; Chen, W.L.; Huang, C.C.; Yang, M.C.; Lei, W.Y.; Lin, C.M.; Chou, C.C.; Chang, C.F.; et al. Demographics of Pediatric OHCA Survivors with Postdischarge Diseases: A National Population-Based Follow-Up Study. Front. Pediatr. 2020, 7, 537. [Google Scholar] [CrossRef] [PubMed]
- Okubo, M.; Matsuyama, T.; Gibo, K.; Komukai, S.; Izawa, J.; Kiyohara, K.; Nishiyama, C.; Kiguchi, T.; Callaway, C.W.; Iwami, T.; et al. Sex Differences in Receiving Layperson Cardiopulmonary Resuscitation in Pediatric Out-of-Hospital Cardiac Arrest: A Nationwide Cohort Study in Japan. J. Am. Heart Assoc. 2019, 8, e010324. [Google Scholar] [CrossRef]
- Fukuda, T.; Ohashi-Fukuda, N.; Sekiguchi, H.; Inokuchi, R.; Kukita, I. Survival from Pediatric Out-of-Hospital Cardiac Arrest During Nights and Weekends: An Updated Japanese Registry-Based Study. JACC Asia 2022, 2, 433–443. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga, M.; Ishikawa, S.; Otsubo, Y.; Shida, M.; Hoshiko, K.; Yatsunami, K.; Kanaya, Y.; Takagi, J.; Takamura, K.; Ganaha, H.; et al. Sudden out-of-hospital cardiac arrest in pediatric patients in Kyushu area in Japan. Pediatr. Int. 2021, 63, 1441–1450. [Google Scholar] [CrossRef]
- Di Marco, S.; Tucci, R.; Tonelli, G.; Frione, G.; Semeraro, F.; Ristagno, G.; Scapigliati, A. Preparedness for telephone dispatch-assisted cardiopulmonary resuscitation in Italy. A National survey. Resuscitation 2020, 149, 87–88. [Google Scholar] [CrossRef]
- Di Marco, S.; Petacco, M.; Semeraro, F.; Scapigliati, A.; Boccuzzi, A.; De Luca, M.; Panzarino, B.; Cataldi, W.; Scelsi, S.; Ristagno, G. Telephone dispatcher-assisted cardiopulmonary resuscitation in Italy. A picture from a nationwide survey. Resuscitation 2017, 111, e9–e10. [Google Scholar] [CrossRef]
- Babini, G.; Ristagno, G. COVID-19 and reduced bystander cardiopulmonary resuscitation: A thanatophobic attitude leading to increased deaths from cardiac arrest? Acta Anaesthesiol. Scand. 2023, 67, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Stirparo, G.; Bellini, L.; Ristagno, G.; Bonora, R.; Pagliosa, A.; Migliari, M.; Andreassi, A.; Signorelli, C.; Sechi, G.M.; Fagoni, N. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network-A Three-Year Study. J. Clin. Med. 2022, 11, 5718. [Google Scholar] [CrossRef]
- Novelli, V.; Cutti, S.; Muzzi, A.; Marena, C.; Grugnetti, G.; Triarico, A.; Nicora, C.; Venturi, A.; Licari, A.; Marseglia, G.L.; et al. Timely adaptation of a Pediatric Unit to COVID-19 emergency in Northern Italy: The experience of Fondazione IRCCS Policlinico San Matteo in Pavia. Acta Biomed. 2020, 91, e2020004. [Google Scholar] [CrossRef]
- Stirparo, G.; Oradini-Alacreu, A.; Signorelli, C.; Sechi, G.M.; Zoli, A.; Fagoni, N. Smart-working policies during COVID-19 pandemic: A way to reduce work-related traumas? Intern. Emerg. Med. 2022, 17, 2427–2430. [Google Scholar] [CrossRef]
- Caminiti, C.; Maglietta, G.; Meschi, T.; Ticinesi, A.; Silva, M.; Sverzellati, N. Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. J. Clin. Med. 2021, 10, 880. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Ahn, C.; Park, Y.; Won, M. Comparison of out-of-hospital cardiac arrests during the COVID-19 pandemic with those before the pandemic: An updated systematic review and meta-analysis. Front. Public Health. 2023, 11, 1180511. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.J.; Reddy, M.P.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef]
- Singh, S.; Fong, H.K.; Mercedes, B.R.; Serwat, A.; Malik, F.A.; Desai, R. COVID-19 and out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation 2020, 156, 164–166. [Google Scholar] [CrossRef]
- Mobinizadeh, M.; Berenjian, F.; Mohamadi, E.; Habibi, F.; Olyaeemanesh, A.; Zendedel, K.; Sharif-Alhoseini, M. Trauma Registry Data as a Policy-Making Tool: A Systematic Review on the Research Dimensions. Bull. Emerg. Trauma 2022, 10, 49–58. [Google Scholar] [CrossRef]
- Munot, S.; Bray, J.; Bauman, A.; Rugel, E.J.; Giordan, L.B.; Marschner, S.; Chow, C.K.; Redfern, J. Development of an intervention to facilitate dissemination of community-based training to respond to out-of-hospital cardiac arrest: FirstCPR. PLoS ONE 2022, 17, e0273028. [Google Scholar] [CrossRef] [PubMed]
- Paglino, M.; Contri, E.; Baggiani, M.; Tonani, M.; Costantini, G.; Bonomo, M.C.; Baldi, E. A video-based training to effectively teach CPR with long-term retention: The ScuolaSalvaVita.it (“SchoolSavesLives.it”) project. Intern. Emerg. Med. 2019, 14, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Rubbi, I.; Lapucci, G.; Bondi, B.; Monti, A.; Cortini, C.; Cremonini, V.; Nanni, E.; Pasquinelli, G.; Ferri, P. Effectiveness of a video lesson for the correct use in an emergency of the automated external defibrillator (AED). Acta Biomed. 2020, 91, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Caviglia, M.; Putoto, G.; Conti, A.; Tognon, F.; Jambai, A.; Vandy, M.J.; Youkee, D.; Buson, R.; Pini, S.; Rosi, P.; et al. Association between ambulance prehospital time and maternal and perinatal outcomes in Sierra Leone: A countrywide study. BMJ Glob. Health 2021, 6, e007315. [Google Scholar] [CrossRef] [PubMed]
- Conti, A.; Sacchetto, D.; Putoto, G.; Mazzotta, M.; de Meneghi, G.; de Vivo, E.; Ronco, L.L.; Hubloue, I.; Della Corte, F.; Barone-Adesi, F.; et al. Implementation of the South African Triage Scale (SATS) in a New Ambulance System in Beira, Mozambique: A Retrospective Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 10298. [Google Scholar] [CrossRef] [PubMed]
- Vassallo, J.; Webster, M.; Barnard, E.B.G.; Lyttle, M.D.; Smith, J.E.; PERUKI (Paediatric Emergency Research in the UK and Ireland). Epidemiology and aetiology of paediatric traumatic cardiac arrest in England and Wales. Arch. Dis. Child. 2019, 104, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.; Carballo, C.; Colosimo, C.; Gratton, A.; Mentzer, C.; Yon, J. Traumatic Cardiac Arrest in Pediatric Patients: An Analysis of the National Trauma Database 2007–2016. Am Surg. 2022, 88, 2252–2254. [Google Scholar] [CrossRef] [PubMed]
- Kiyohara, K.; Sado, J.; Kitamura, T.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Sato, Y.; Kojimahara, N.; Yamaguchi, N.; et al. Epidemiology of Pediatric Out-of-Hospital Cardiac Arrest at School—An Investigation of a Nationwide Registry in Japan. Circ. J. 2018, 82, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Lockey, A.S.; Brown, T.P.; Carlyon, J.D.; Hawkes, C.A. Impact of community initiatives on non-EMS bystander CPR rates in West Yorkshire between 2014 and 2018. Resusc. Plus 2021, 6, 100115. [Google Scholar] [CrossRef]
- Villalobos, F.; Del Pozo, A.; Rey-Reñones, C.; Granado-Font, E.; Sabaté-Lissner, D.; Poblet-Calaf, C.; Basora, J.; Castro, A.; Flores-Mateo, G. Lay People Training in CPR and in the Use of an Automated External Defibrillator, and Its Social Impact: A Community Health Study. Int. J. Environ. Res. Public Health 2019, 16, 2870. [Google Scholar] [CrossRef]
- Auricchio, A.; Gianquintieri, L.; Burkart, R.; Benvenuti, C.; Muschietti, S.; Peluso, S.; Mira, A.; Moccetti, T.; Caputo, M.L. Real-life time and distance covered by lay first responders alerted by means of smartphone-application: Implications for early initiation of cardiopulmonary resuscitation and access to automatic external defibrillators. Resuscitation 2019, 141, 182–187. [Google Scholar] [CrossRef] [PubMed]
| Number | Percentage | |
|---|---|---|
| Acute medical event | 174 | 55.2% |
| Traffic accident | 50 | 15.9% |
| Violent event | 26 | 8.3% |
| Accident/injury | 19 | 6.0% |
| Fall from a height | 13 | 4.1% |
| Drowning | 5 | 1.6% |
| Railroad accident | 5 | 1.6% |
| Mass event | 4 | 1.3% |
| Intoxication | 1 | 0.3% |
| Animal assault | 1 | 0.3% |
| Unknown | 17 | 5.4% |
| Total | 315 | 100% |
| Number | Percentage | |
|---|---|---|
| Home | 185 | 58.7% |
| Road | 73 | 23.2% |
| Sports facility | 14 | 4.4% |
| Lake/water | 9 | 2.9% |
| Rail/metro | 8 | 2.5% |
| Public office | 7 | 2.2% |
| Health facility | 6 | 1.9% |
| School | 6 | 1.9% |
| Skiing facility | 2 | 0.6% |
| Mountain/impervious site | 1 | 0.3% |
| Unknown—not reported | 4 | 1.3% |
| Total | 315 | 100% |
| OHCA Response | Number | Percentage |
|---|---|---|
| Witnessed | 124 | 39.4% |
| Not witnessed | 88 | 27.9% |
| Witnessed EMS | 19 | 6.0% |
| Missing data | 84 | 26.7% |
| Rescue Time | Mean (minute) | Standard Deviation |
| Time to first emergency vehicle on scene | 11.08 | 5.3 |
| Time of overall mission duration | 65.03 | 22.7 |
| Resuscitation outcome | Number | Percentage |
| ROSC | 64 | 20.3% |
| Dead on site | 111 | 35.2% |
| Sent to the Emergency Department | 131 | 41.6% |
| Missing data | 9 | 2.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pireddu, R.; Ristagno, G.; Gianquintieri, L.; Bonora, R.; Pagliosa, A.; Andreassi, A.; Sechi, G.M.; Signorelli, C.; Stirparo, G. Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations. J. Clin. Med. 2024, 13, 3133. https://doi.org/10.3390/jcm13113133
Pireddu R, Ristagno G, Gianquintieri L, Bonora R, Pagliosa A, Andreassi A, Sechi GM, Signorelli C, Stirparo G. Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations. Journal of Clinical Medicine. 2024; 13(11):3133. https://doi.org/10.3390/jcm13113133
Chicago/Turabian StylePireddu, Roberta, Giuseppe Ristagno, Lorenzo Gianquintieri, Rodolfo Bonora, Andrea Pagliosa, Aida Andreassi, Giuseppe Maria Sechi, Carlo Signorelli, and Giuseppe Stirparo. 2024. "Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations" Journal of Clinical Medicine 13, no. 11: 3133. https://doi.org/10.3390/jcm13113133
APA StylePireddu, R., Ristagno, G., Gianquintieri, L., Bonora, R., Pagliosa, A., Andreassi, A., Sechi, G. M., Signorelli, C., & Stirparo, G. (2024). Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations. Journal of Clinical Medicine, 13(11), 3133. https://doi.org/10.3390/jcm13113133






