Instant Detection of Cerebral Blood Flow Changes in Infants with Congenital Heart Disease during Transcatheter Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
2.2. The Transfontanellar Cerebral Doppler Monitoring System
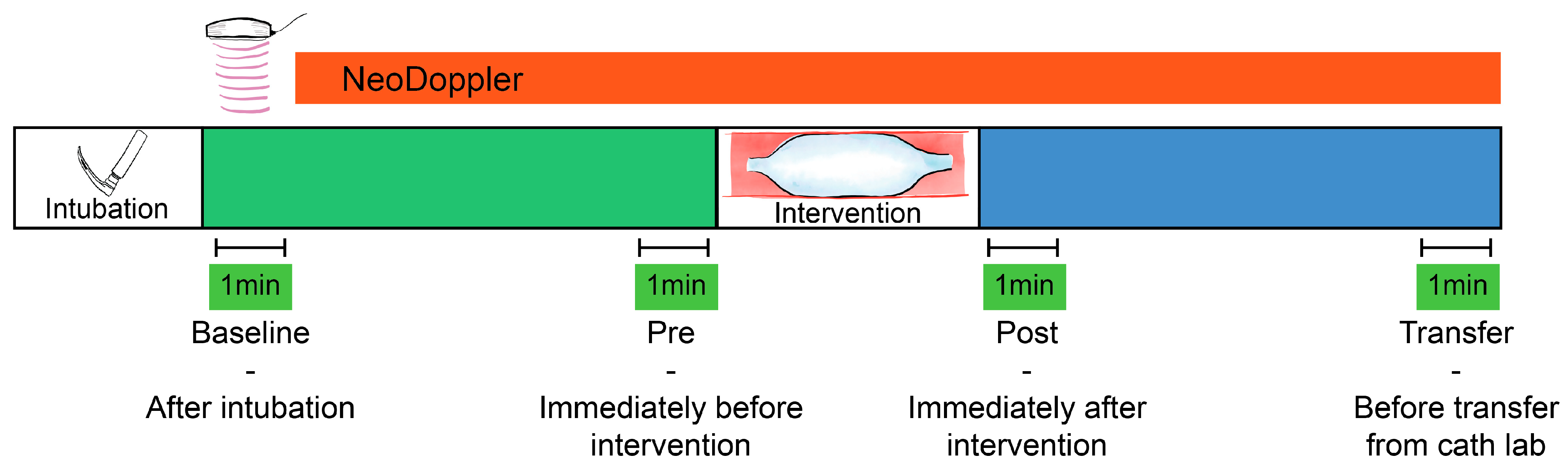
2.3. Monitoring Protocol
2.4. Feasibility and Quality Evaluation
2.5. Analysis of Doppler Measurements and Trends
2.6. Interventions and Events/Complications
2.7. Statistical Analysis
2.8. Safety
3. Results
3.1. Participants, Feasibility and Quality Evaluation
3.2. Trends
3.3. Interventions and Events
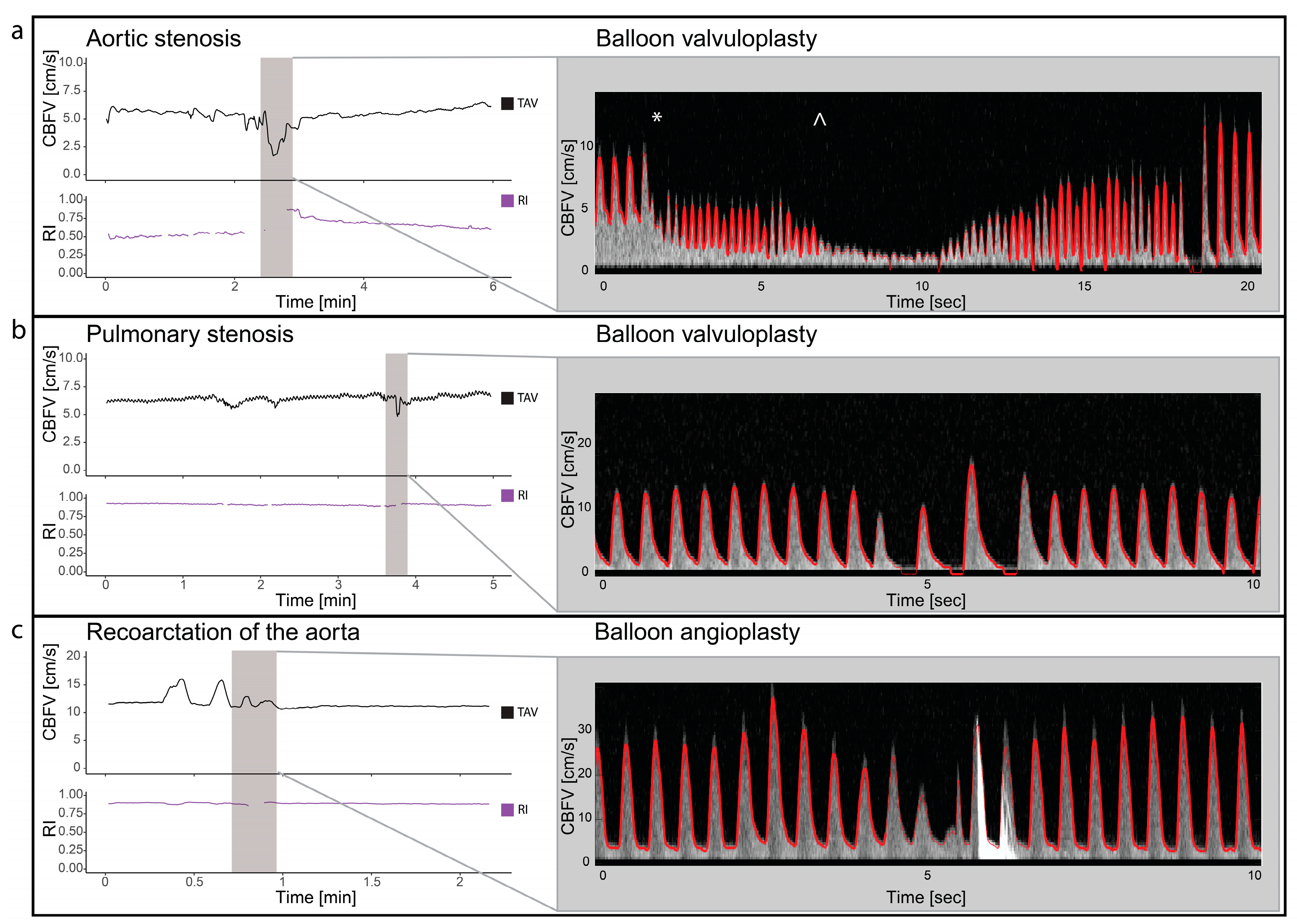
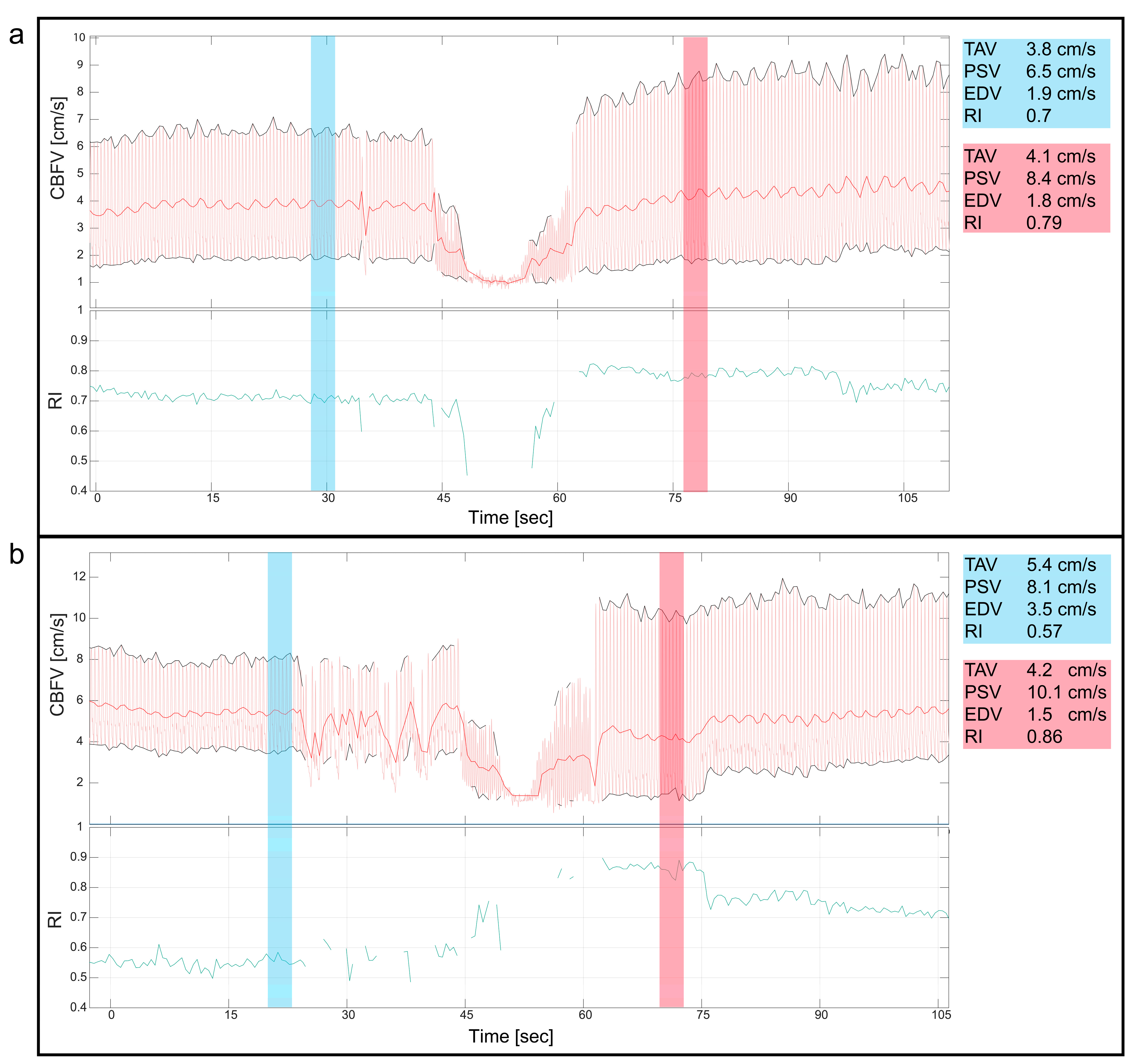
3.4. Balloon Valvuloplasty/Angioplasty/Procedures
3.5. Patent Ductus Arteriosus
3.6. Pulmonary Atresia
4. Discussion
4.1. Monitoring Trends and Events
4.2. Monitoring to Detect Complications
4.3. Future Research
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kenny, D.P.; Hijazi, Z.M. Current Status and Future Potential of Transcatheter Interventions in Congenital Heart Disease. Circ. Res. 2017, 120, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Devanagondi, R.; Peck, D.; Sagi, J.; Donohue, J.; Yu, S.; Pasquali, S.K.; Armstrong, A.K. Long-Term Outcomes of Balloon Valvuloplasty for Isolated Pulmonary Valve Stenosis. Pediatr. Cardiol. 2017, 38, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Sathanandam, S.K.; Gutfinger, D.; O’Brien, L.; Forbes, T.J.; Gillespie, M.J.; Berman, D.P.; Armstrong, A.K.; Shahanavaz, S.; Jones, T.K.; Morray, B.H.; et al. Amplatzer Piccolo Occluder clinical trial for percutaneous closure of the patent ductus arteriosus in patients ≥700 grams. Catheter. Cardiovasc. Interv. 2020, 96, 1266–1276. [Google Scholar] [CrossRef] [PubMed]
- El-Said, H.G.; Bratincsak, A.; Foerster, S.R.; Murphy, J.J.; Vincent, J.; Holzer, R.; Porras, D.; Moore, J.; Bergersen, L. Safety of Percutaneous Patent Ductus Arteriosus Closure: An Unselected Multicenter Population Experience. J. Am. Heart Assoc. 2013, 2, e000424. [Google Scholar] [CrossRef] [PubMed]
- Takaya, Y.; Akagi, T.; Kijima, Y.; Nakagawa, K.; Sano, S.; Ito, H. Long-Term Outcome After Transcatheter Closure of Atrial Septal Defect in Older Patients: Impact of Age at Procedure. JACC Cardiovasc. Interv. 2015, 8, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Meliota, G.; Vairo, U. Transcatheter Interventions for Neonates with Congenital Heart Disease: A Review. Diagnostics 2023, 13, 2673. [Google Scholar] [CrossRef] [PubMed]
- Barry, O.M.; Bouhout, I.; Turner, M.E.; Petit, C.J.; Kalfa, D.M. Transcatheter Cardiac Interventions in the Newborn: JACC Focus Seminar. J. Am. Coll. Cardiol. 2022, 79, 2270–2283. [Google Scholar] [CrossRef]
- Rodriguez, R.A.; Hosking, M.C.; Duncan, W.J.; Sinclair, B.; Teixeira, O.H.; Cornel, G. Cerebral blood flow velocities monitored by transcranial Doppler during cardiac catheterizations in children. Cathet. Cardiovasc. Diagn. 1998, 43, 282–290. [Google Scholar] [CrossRef]
- de Vries, J.W.; Hoorntje, T.M.; Sreeram, N. Neurophysiological Effects of Pediatric Balloon Dilatation Procedures. Pediatr. Cardiol. 2000, 21, 461–464. [Google Scholar] [CrossRef]
- Bissonnette, B.; Benson, L.N. Closure of persistently patent arterial duct and its impact on cerebral circulatory haemodynamics in children. Can. J. Anaesth. 1998, 45, 199–205. [Google Scholar] [CrossRef]
- Rodriguez, R.A.; Cornel, G.; Hosking, M.C.; Weerasena, N.; Splinter, W.M.; Murto, K. Cerebral blood flow velocity during occlusive manipulation of patent ductus arteriosus in children. J. Neuroimaging 1999, 9, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Vik, S.D.; Torp, H.; Jarmund, A.H.; Kiss, G.; Follestad, T.; Støen, R.; Nyrnes, S.A. Continuous monitoring of cerebral blood flow during general anaesthesia in infants. BJA Open 2023, 6, 100144. [Google Scholar] [CrossRef] [PubMed]
- Vik, S.D.; Torp, H.; Follestad, T.; Støen, R.; Nyrnes, S.A. NeoDoppler: New ultrasound technology for continous cerebral circulation monitoring in neonates. Pediatr. Res. 2020, 87, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Leth-Olsen, M.; Døhlen, G.; Torp, H.; Nyrnes, S.A. Detection of Cerebral High-Intensity Transient Signals by NeoDoppler during Cardiac Catheterization and Cardiac Surgery in Infants. Ultrasound Med. Biol. 2022, 48, 1256–1267. [Google Scholar] [CrossRef] [PubMed]
- Saliba, E.M.; Chantepie, A.; Gold, F.; Marchand, M.; Pourcelot, L.; Laugier, J. Intraoperative measurements of cerebral haemodynamics during ductus arteriosus ligation in preterm infants. Eur. J. Pediatr. 1991, 150, 362–365. [Google Scholar] [CrossRef] [PubMed]
- Hoodbhoy, S.A.; Cutting, H.A.; Seddon, J.A.; Campbell, M.E. Cerebral and splanchnic hemodynamics after duct ligation in very low birth weight infants. J. Pediatr. 2009, 154, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Keusters, L.; Purna, J.; Deshpande, P.; Mertens, L.; Shah, P.; McNamara, P.J.; Weisz, D.E.; Jain, A. Clinical validity of systemic arterial steal among extremely preterm infants with persistent patent ductus arteriosus. J. Perinatol. 2021, 41, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Camfferman, F.A.; de Goederen, R.; Govaert, P.; Dudink, J.; van Bel, F.; Pellicer, A.; Cools, F.; Agut, T.; Alarcon, A.; Arena, R.; et al. Diagnostic and predictive value of Doppler ultrasound for evaluation of the brain circulation in preterm infants: A systematic review. Pediatr. Res. 2020, 87, 50–58. [Google Scholar] [CrossRef]
- Mitra, S.; de Boode, W.P.; Weisz, D.E.; Shah, P.S. Interventions for patent ductus arteriosus (PDA) in preterm infants: An overview of Cochrane Systematic Reviews. Cochrane Database Syst. Rev. 2023, 4, CD013588. [Google Scholar] [CrossRef]
- Zaleski, K.L.; Kussman, B.D. Near-Infrared Spectroscopy in Pediatric Congenital Heart Disease. J. Cardiothorac. Vasc. Anesth. 2020, 34, 489–500. [Google Scholar] [CrossRef]
- Moerman, A.; Meert, F.; De Hert, S. Cerebral near-infrared spectroscopy in the care of patients during cardiological procedures: A summary of the clinical evidence. J. Clin. Monit. Comput. 2016, 30, 901–909. [Google Scholar] [CrossRef] [PubMed]
- van der Laan, M.E.; Verhagen, E.A.; Bos, A.F.; Berger, R.M.F.; Kooi, E.M.W. Effect of balloon atrial septostomy on cerebral oxygenation in neonates with transposition of the great arteries. Pediatr. Res. 2013, 73, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Tanidir, I.C.; Ozturk, E.; Ozyilmaz, I.; Saygi, M.; Kiplapinar, N.; Haydin, S.; Guzeltas, A.; Odemis, E. Near Infrared Spectroscopy Monitoring in the Pediatric Cardiac Catheterization Laboratory. Artif. Organs 2014, 38, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Leth-Olsen, M.; Døhlen, G.; Torp, H.; Nyrnes, S.A. Cerebral blood flow dynamics during cardiac surgery in infants. Pediatr. Res. 2024. [Google Scholar] [CrossRef] [PubMed]
- Mir, M.; Moore, S.S.; Wutthigate, P.; Simoneau, J.; Villegas Martinez, D.; Shemie, S.D.; Brossard-Racine, M.; Dancea, A.; Bertolizio, G.; Altit, G. Newborns with a Congenital Heart Defect and Diastolic Steal Have an Altered Cerebral Arterial Doppler Profile. J. Pediatr. 2023, 257, 113369. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Lee, J.H.; Song, I.K.; Kim, H.S.; Jang, Y.E.; Kim, W.H.; Kwak, J.G.; Kim, J.T. Potential Role of Transfontanelle Ultrasound for Infants Undergoing Modified Blalock-Taussig Shunt. J. Cardiothorac. Vasc. Anesth. 2018, 32, 1648–1654. [Google Scholar] [CrossRef]
- Ing, R.J.; Twite, M.D. Toward Improved Neurodevelopmental Outcomes: The Role of Transfontanel Ultrasound Assessment of Cerebral Blood Flow in Infants Undergoing Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2018, 32, 1655–1656. [Google Scholar] [CrossRef]



| Basic Clinical Data (Units) | |
|---|---|
| Age (months) | 3.5 ± 2.8 |
| Weight (g) | 5187 ± 1977 |
| BSA (m2) | 0.29 ± 0.08 |
| Female (n) | 6 (37.5%) |
| Blood pressure systolic (mmHg) | 85 ± 13 |
| Blood pressure diastolic (mmHg) | 49 ± 9 |
| Mean blood pressure (mmHg) | 63 ± 9 |
| HR (bpm) | 134 ± 24 |
| Cerebral Doppler monitoring time (min) | 72.8 ± 38.2 |
| TAV cm/s (%) | RI (%) | EtCO2 kPa (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Procedure | Baseline | Pre | Post | Transfer | Baseline | Pre | Post | Transfer | Baseline | Pre | Post | Transfer |
| vPS | Balloon valvulopasty | 7.28 (100%) | 6.65 (91%) | 6.45 (89%) | 6.67 (92%) | 0.78 (100%) | 0.9 (115%) | 0.91 (117%) | 0.9 (115%) | 4.2 (100%) | 3.2 (76%) | 3 (71%) | 3.3 (79%) |
| reCoA | Balloon angiopasty | 13.61 (100%) | 13.97 (103%) | 13.59 (100%) | 13.84 (102%) | 0.79 (100%) | 0.76 (96%) | 0.76 (96%) | 0.75 (95%) | 5.1 (100%) | 5.2 (102%) | 5.1 (100%) | 5.5 (108%) |
| vPS | Balloon valvulopasty | 6.95 (100%) | 4.79 (69%) | 5.06 (73%) | 4.81 (69%) | 0.82 (100%) | 0.81 (99%) | 0.8 (98%) | 0.76 (93%) | 5.85 (100%) | 4.7 (80%) | 4.5 (77%) | |
| HLHS | Sano shunt test occlusion | 8.68 (100%) | 9.15 (105%) | 8.98 (103%) | 9.12 (105%) | 0.78 (100%) | 0.76 (97%) | 0.72 (92%) | 0.78 (100%) | ||||
| vPS | Balloon valvulopasty | 8.42 (100%) | 8.39 (100%) | 7.32 (87%) | 7.92 (94%) | 0.66 (100%) | 0.73 (111%) | 0.74 (112%) | 0.74 (112%) | 5.35 (100%) | 5.7 (107%) | 5.6 (105%) | 5.4 (101%) |
| svPS | Balloon valvulopasty | 10.75 (100%) | 10.93 (102%) | 11.86 (110%) | 11.89 (111%) | 0.72 (100%) | 0.76 (106%) | 0.73 (101%) | 0.74 (103%) | 4.9 (100%) | 4.6 (94%) | 4.9 (100%) | 5.2 (106%) |
| reCoA | Balloon angiopasty | 14.91 (100%) | 12.03 (81%) | 11.15 (75%) | 11.79 (79%) | 0.81 (100%) | 0.89 (110%) | 0.89 (110%) | 0.87 (107%) | 6.7 (100%) | 6.2 (93%) | 6.1 (91%) | 6.15 (92%) |
| Ebstein anomaly | PDA stent | 3.84 (100%) | 5.79 (151%) | 5.26 (137%) | 5.01 (130%) | 0.99 (100%) | 0.95 (96%) | 1 (101%) | 0.99 (100%) | 5.03 (100%) | 5.3 (105%) | 5.3 (105%) | 5.15 (102%) |
| PDA | Occlusion | 9.41 (100%) | 8.45 (90%) | 10.34 (110%) | 10.68 (113%) | 0.82 (100%) | 0.82 (100%) | 0.55 (67%) | 0.56 (68%) | 6.43 (100%) | 5 (78%) | 5 (78%) | 6.45 (100%) |
| vAS | Balloon valvulopasty | 4.34 (100%) | 3.58 (82%) | 4.29 (99%) | 4.28 (99%) | 0.56 (100%) | 0.73 (130%) | 0.77 (138%) | 0.7 (125%) | 4.4 (100%) | 4.3 (98%) | 4.3 (98%) | 4.5 (102%) |
| vAS | Balloon valvulopasty | 5.58 (100%) | 5.21 (93%) | 5.04 (90%) | 5.52 (99%) | 0.53 (100%) | 0.55 (104%) | 0.76 (143%) | 0.59 (111%) | 5.35 (100%) | 5.4 (101%) | 5.2 (97%) | 4.75 (89%) |
| PA-IVS | Radio frequency ablation | 5.95 (100%) | 6.99 (117%) | 4.35 (73%) | 5.61 (94%) | 0.71 (100%) | 0.65 (92%) | 0.61 (86%) | 0.53 (75%) | 5.4 (100%) | 5.4 (100%) | 6.4 (119%) | |
| LPA stenosis | Balloon valvulopasty | 13.56 (100%) | 12.87 (95%) | 13.64 (101%) | 13.56 (100%) | 0.76 (100%) | 0.78 (103%) | 0.78 (103%) | 0.79 (104%) | 4.85 (100%) | 5.05 (104%) | 4.8 (99%) | 4.9 (101%) |
| ASD secundum | Occlusion | 9.62 (100%) | 9.25 (96%) | 9.54 (99%) | 8.76 (91%) | 0.85 (100%) | 0.88 (104%) | 0.86 (101%) | 0.87 (102%) | ||||
| PDA | Occlusion | 23.27 (100%) | 21.49 (92%) | 22.7 (98%) | 23.44 (101%) | 0.7 (100%) | 0.77 (110%) | 0.71 (101%) | 0.58 (83%) | 6.6 (100%) | 5.9 (89%) | 6 (91%) | 6.5 (98%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leth-Olsen, M.; Døhlen, G.; Torp, H.; Nyrnes, S.A. Instant Detection of Cerebral Blood Flow Changes in Infants with Congenital Heart Disease during Transcatheter Interventions. J. Clin. Med. 2024, 13, 3115. https://doi.org/10.3390/jcm13113115
Leth-Olsen M, Døhlen G, Torp H, Nyrnes SA. Instant Detection of Cerebral Blood Flow Changes in Infants with Congenital Heart Disease during Transcatheter Interventions. Journal of Clinical Medicine. 2024; 13(11):3115. https://doi.org/10.3390/jcm13113115
Chicago/Turabian StyleLeth-Olsen, Martin, Gaute Døhlen, Hans Torp, and Siri Ann Nyrnes. 2024. "Instant Detection of Cerebral Blood Flow Changes in Infants with Congenital Heart Disease during Transcatheter Interventions" Journal of Clinical Medicine 13, no. 11: 3115. https://doi.org/10.3390/jcm13113115
APA StyleLeth-Olsen, M., Døhlen, G., Torp, H., & Nyrnes, S. A. (2024). Instant Detection of Cerebral Blood Flow Changes in Infants with Congenital Heart Disease during Transcatheter Interventions. Journal of Clinical Medicine, 13(11), 3115. https://doi.org/10.3390/jcm13113115






