Autophagy in Osteoarthritis: A Double-Edged Sword in Cartilage Aging and Mechanical Stress Response: A Systematic Review
Abstract
1. Introduction
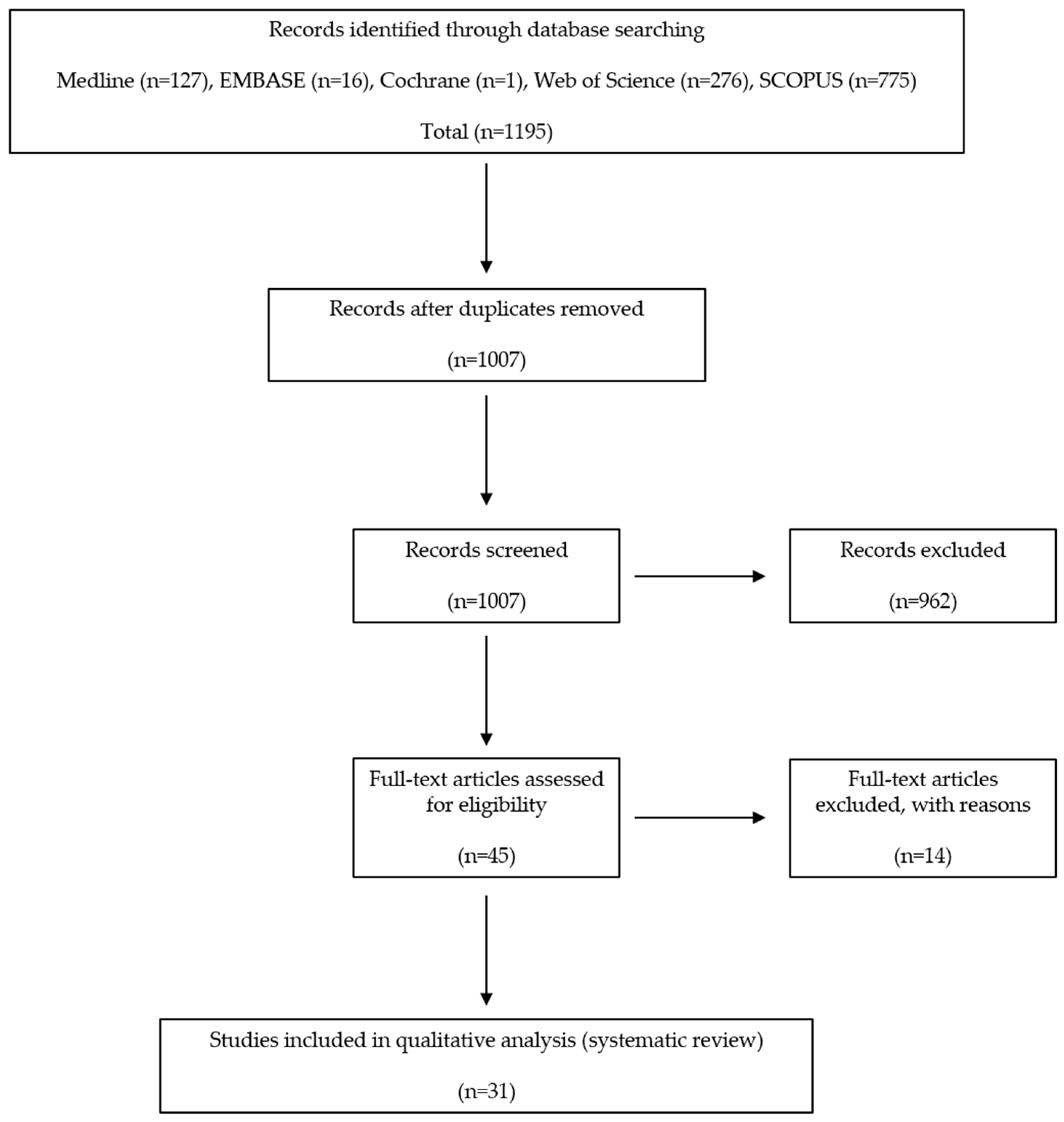
2. Materials and Methods
2.1. Study Selection
2.2. Eligibility Criteria
2.3. Extraction of Data
2.4. Characteristics of the Included Studies
3. Results
3.1. Study Selection
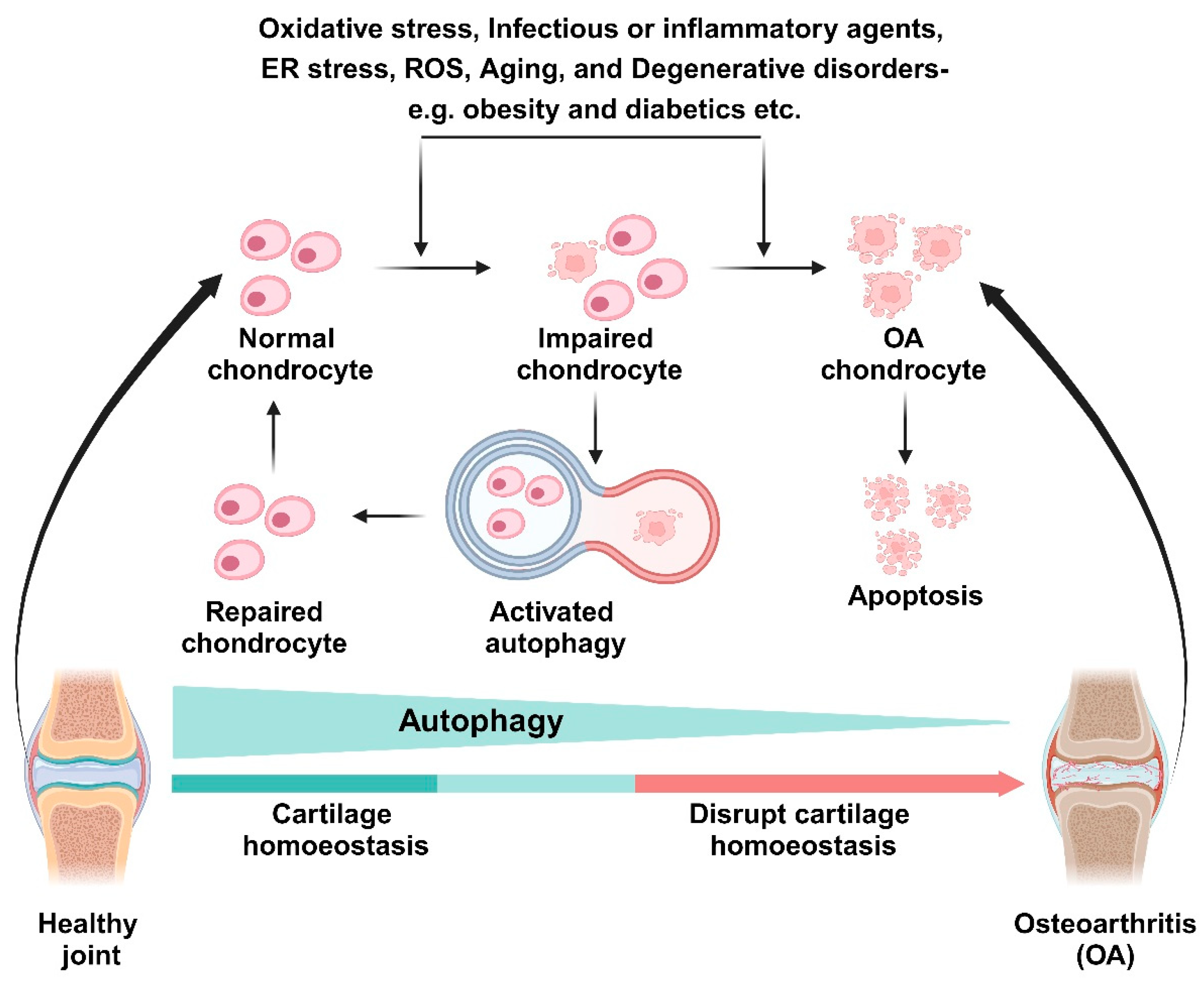
3.2. The Role of Autophagy in Aging and OA Chondrocytes
3.3. The Role of Autophagy in Normal Human Chondrocytes
3.4. The Role of Mechanical Stress-Induced Autophagy in Normal Human Chondrocytes
4. Discussion
5. Future Perspectives
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Martin, J.A.; Buckwalter, J.A. Aging, articular cartilage chondrocyte senescence and osteoarthritis. Biogerontology 2002, 3, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Qing, Y.; Xiaohao, W.; Chu, T.; Weiyuan, G.; Mingjue, C.; Minghao, Q.; Yiming, Z.; Tailin, H.; Sheng, C.; Guozhi, X. Osteoarthritis: Pathogenic signaling pathways and therapeutic targets. Signal Transduct. Target. Ther. 2023, 8, 56. [Google Scholar]
- Kevin, R.; Bryan, P.; Benjamin, J.; Heather, K. The pathophysiology of osteoarthritis: A mechanical perspective on the knee joint. PM&R. 2012, 4, S3–S9. [Google Scholar]
- Vilim, M.; Vid, M.; Ivan, K.; Roko, B.; Zeljko, J.; Damir, H.; Eduard, R.; Fabijan, C.; Trpimir, V.; Dinko, V.; et al. Cytokines and Chemokines Involved in Osteoarthritis Pathogenesis. Int. J. Mol. Sci. 2021, 22, 9208. [Google Scholar]
- Warmink, K.; Vinod, P.; Korthagen, N.M.; Weinans, H.; Rios, J.L. Macrophage-Driven Inflammation in Metabolic Osteoarthritis: Implications for Biomarker and Therapy Development. Int. J. Mol. Sci. 2023, 24, 6112. [Google Scholar] [CrossRef] [PubMed]
- Mercedes, F.; Ignacio, R.; Vanessa, C.; Francisco, J. Genetics in osteoarthritis. Curr. Genomics 2008, 9, 542–547. [Google Scholar]
- Hemanth, A.; Anja, N. Role of Chondrocytes in Cartilage Formation, Progression of Osteoarthritis and Cartilage Regeneration. J. Dev. Biol. 2015, 3, 177–192. [Google Scholar]
- David, J.; Jason, J.; Francis, J. The symptoms of osteoarthritis and the genesis of pain. Rheum. Dis. Clin. N. Am. 2008, 34, 623–643. [Google Scholar]
- Lv, X.; Zhao, T.; Dai, Y.; Shi, M.; Huang, W.; Wei, Y.; Sehn, J.; Zhang, X.; Xie, Z.; Wang, Q.; et al. New insight into the interplay between autophagy and cartilage degeneration in osteoarthritis. Front. Cell Dev. Biol. 2022, 10, 1089668. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Park, Y.-J.; Song, M.-G.; Kim, D.-R.; Zada, S.; Kim, D.-H. Cytoprotective Effects of Delphinidin for Human Chondrocytes against Oxidative Stress through Activation of Autophagy. Antioxidants 2020, 9, 83. [Google Scholar] [CrossRef]
- Mizushima, N. Physiological functions of autophagy. Curr. Top. Microbiol. Immunol. 2009, 335, 71–84. [Google Scholar] [PubMed]
- Maiuri, M.C.; Zalckvar, E.; Kimchi, A.; Kroemer, G. Self-eating and self-killing: Crosstalk between autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2007, 8, 741–752. [Google Scholar] [CrossRef] [PubMed]
- Levine, B.; Yuan, J. Autophagy in cell death: An innocent convict? J. Clin. Investig. 2005, 115, 2679–2688. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.C.; Juhasz, G.; Neufeld, T.P. Direct induction of autophagy by Atg1 inhibits cell growth and induces apoptotic cell death. Curr. Biol. 2007, 17, 1–11. [Google Scholar] [CrossRef]
- Chang, J.; Wang, W.; Zhang, H.; Hu, Y.; Wang, M.; Yin, Z. The dual role of autophagy in chondrocyte responses in the pathogenesis of articular cartilage degeneration in osteoarthritis. Int. J. Mol. Med. 2013, 32, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Carames, B.; Taniguchi, N.; Otsuki, S.; Blanco, F.J.; Lotz, M. Autophagy is a protective mechanism in normal cartilage, and its aging-related loss is linked with cell death and osteoarthritis. Arthritis Rheum. 2010, 62, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Almonte-Becerril, M.; Navarro-Garcia, F.; Gonzalez-Robles, A.; Vega-Lopez, M.A.; Lavalle, C.; Kouri, J.B. Cell death of chondrocytes is a combination between apoptosis and autophagy during the pathogenesis of Osteoarthritis within an experimental model. Apoptosis 2010, 15, 631–638. [Google Scholar] [CrossRef]
- Kroemer, G.; Marino, G.; Levine, B. Autophagy and the integrated stress response. Mol. Cell 2010, 40, 280–293. [Google Scholar] [CrossRef] [PubMed]
- Laura, G.; Maria, D.; Diego, S.; Jazmin, G.; Gustavo, L.; Arminda, M.; Ana, E.; Jose, L.; Francisco, M.; Luis, O.; et al. Autophagy: A Key Regulator of Homeostasis and Disease: An Overview of Molecular Mechanisms and Modulators. Cells 2022, 11, 2262. [Google Scholar]
- Wang, Z.J.; Zhang, H.B.; Chen, C.; Huang, H.; Liang, J.X. Effect of PPARG on AGEs-induced AKT/MTOR signaling-associated human chondrocytes autophagy. Cell Biol. Int. 2018, 42, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Takayama, K.; Matsushita, T.; Ishida, K.; Kubo, S.; Matsumoto, T.; Fujita, N.; Oka, S.; Kurosaka, M.; Kuroda, R. Autophagy modulates osteoarthritis-related gene expression in human chondrocytes. Arthritis Rheum. 2012, 64, 1920–1928. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.; Lopez de Figueroa, P.; Blanco, F.J.; Mendes, A.F.; Carames, B. Insulin decreases autophagy and leads to cartilage degradation. Osteoarthr. Cartil. 2016, 24, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Yang, C.M.; Park, S.J.; Kim, H.A. Monosodium Urate Crystal-Induced Chondrocyte Death via Autophagic Process. Int. J. Mol. Sci. 2015, 16, 29265–29277. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.; Zhu, Y.; Zhu, L.; Weng, F.; Li, X.; Xu, Y. Oxidized low density lipoprotein facilitates tumor necrosis factor-α mediated chondrocyte death via autophagy pathway. Mol. Med. Rep. 2017, 16, 9449–9456. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, X.; Yang, X.; Maimaitijuma, T.; Cao, X.Y.; Jiao, Y.; Wu, H.; Meng, Z.C.; Liu, H.; Guan, Z.P.; Cao, Y.P. Plant homeodomain finger protein 23 inhibits autophagy and promotes apoptosis of chondrocytes in osteoarthritis. Chin. Med. J. 2019, 132, 2581–2587. [Google Scholar] [CrossRef] [PubMed]
- Wangyang, Y.; Zheng, X.; Liu, G.W.; Li, D.Y.; Feng, Y.B.; Guo, T.Y.; Ma, C.; Wang, T. Upregulation of P63 inhibits chondrocyte autophagy thereby enhancing the malignant progression of osteoarthritis. Pharmazie 2017, 72, 361–364. [Google Scholar] [PubMed]
- Sekar, S.; Wu, X.; Friis, T.; Crawford, R.; Prasadam, I.; Xiao, Y. Saturated fatty acids promote chondrocyte matrix remodeling through reprogramming of autophagy pathways. Nutrition 2018, 54, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Duan, Z.X.; Tu, C.; Liu, Q.; Li, S.Q.; Li, Y.H.; Xie, P.; Li, Z.H. Adiponectin receptor agonist AdipoRon attenuates calcification of osteoarthritis chondrocytes by promoting autophagy. J. Cell Biochem. 2020, 121, 3333–3344. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Wang, J.; Chen, S.; Feng, Y. Autophagy promotion enhances the protective effect of Morroniside on human OA chondrocyte. Biosci. Biotechnol. Biochem. 2020, 84, 989–996. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.M.; Ansari, M.Y.; Haqqi, T.M. Sucrose, But Not Glucose, Blocks IL1-beta-Induced Inflammatory Response in Human Chondrocytes by Inducing Autophagy via AKT/mTOR Pathway. J. Cell Biochem. 2017, 118, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Carames, B.; Kiosses, W.B.; Akasaki, Y.; Brinson, D.C.; Eap, W.; Koziol, J.; Lotz, M.K. Glucosamine activates autophagy in vitro and in vivo. Arthritis Rheum. 2013, 65, 1843–1852. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.Y.; Ahmad, N.; Haqqi, T.M. Butein Activates Autophagy Through AMPK/TSC2/ULK1/mTOR Pathway to Inhibit IL-6 Expression in IL-1beta Stimulated Human Chondrocytes. Cell Physiol. Biochem. 2018, 49, 932–946. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Meng, Q.; Jing, H.; Zhou, S. Astragaloside IV protects against apoptosis in human degenerative chondrocytes through autophagy activation. Mol. Med. Rep. 2017, 16, 3269–3275. [Google Scholar] [CrossRef] [PubMed]
- Moussa, M.; Lajeunesse, D.; Hilal, G.; El Atat, O.; Haykal, G.; Serhal, R.; Chalhoub, A.; Khalil, C.; Alaaeddine, N. Platelet rich plasma (PRP) induces chondroprotection via increasing autophagy, anti-inflammatory markers, and decreasing apoptosis in human osteoarthritic cartilage. Exp. Cell Res. 2017, 352, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Nogueira-Recalde, U.; Lorenzo-Gomez, I.; Blanco, F.J.; Loza, M.I.; Grassi, D.; Shirinsky, V.; Shirinsky, I.; Lotz, M.; Robbins, P.D.; Dominguez, E.; et al. Fibrates as drugs with senolytic and autophagic activity for osteoarthritis therapy. EBioMedicine 2019, 45, 588–605. [Google Scholar] [CrossRef] [PubMed]
- Cetrullo, S.; D’Adamo, S.; Guidotti, S.; Borzi, R.M.; Flamigni, F. Hydroxytyrosol prevents chondrocyte death under oxidative stress by inducing autophagy through sirtuin 1-dependent and –independent mechanisms. Biochim. Biophys. Acta 2016, 1860, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.Y.; Khan, N.M.; Haqqi, T.M. A standardized extract of Butea monosperma (Lam.) flowers suppresses the IL-1β-induced expression of IL-6 and matrix-metalloproteases by activating autophagy in human osteoarthritis chondrocytes. Biomed. Pharmacother. 2017, 96, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.F.; Lin, X.L.; Wang, X.; Ping, Z.G.; Guo, X. Comparison of Apoptosis and Autophagy in Human Chondrocytes Induced by the T-2 and HT-2 Toxins. Toxins 2019, 11, 260. [Google Scholar] [CrossRef] [PubMed]
- Liao, F.X.; Huang, F.; Ma, W.G.; Qin, K.P.; Xu, P.F.; Wu, Y.F.; Wang, H.; Chang, J.; Yin, Z.S. The New Role of Sirtuin1 in Human Osteoarthritis Chondrocytes by Regulating Autophagy. Cartilage 2019, 13, 1237S–1248S. [Google Scholar] [CrossRef] [PubMed]
- Zhong, G.; Long, H.; Ma, S.; Shunhan, Y.; Li, J.; Yao, J. miRNA-335-5p relieves chondrocyte inflammation by activating autophagy in osteoarthritis. Life Sci. 2019, 226, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hu, J.; Pan, Y.; Shan, Y.; Jiang, L.; Qi, X.; Jia, L. miR-140-5p/miR-149 Affects Chondrocyte Proliferation, Apoptosis, and Autophagy by Targeting FUT1 in Osteoarthritis. Inflammation 2018, 41, 959–971. [Google Scholar] [CrossRef] [PubMed]
- D’Adamo, S.; Alvarez-Garcia, O.; Muramatsu, Y.; Flamigni, F.; Lotz, M.K. MicroRNA-155 suppresses autophagy in chondrocytes by modulating expression of autophagy proteins. Osteoarthr. Cartil. 2016, 24, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Huang, R.; Ma, H.; Zhao, X.; Wang, G. miRNA-411 Regulates Chondrocyte Autophagy in Osteoarthritis by Targeting Hypoxia-Inducible Factor 1 alpha (HIF-1α). Med. Sci. Monit. 2020, 26, e921155. [Google Scholar] [CrossRef]
- Tian, F.; Wang, J.; Zhang, Z.; Yang, J. LncRNA SNHG7/miR-34a-5p/SYVN1 axis plays a vital role in proliferation, apoptosis and autophagy in osteoarthritis. Biol. Res. 2020, 53, 9. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Tang, Y.; Lu, H.; Shi, B.; Ye, Y.; Xu, G.; Zhao, Q. Long non-coding RNA reprogramming (lncRNA-ROR) regulates cell apoptosis and autophagy in chondrocytes. J. Cell Biochem. 2018, 119, 8432–8440. [Google Scholar] [CrossRef] [PubMed]
- Akasaki, Y.; Alvarez-Garcia, O.; Saito, M.; Carames, B.; Iwamoto, Y.; Lotz, M.K. FoxO transcription factors support oxidative stress resistance in human chondrocytes. Arthritis Rheumatol. 2014, 66, 3349–3358. [Google Scholar] [CrossRef]
- Huang, W.; Cheng, C.; Shan, W.S.; Ding, Z.F.; Liu, F.E.; Lu, W.; He, W.; Xu, J.G.; Yin, Z.S. Knockdown of SGK1 alleviates the IL-1beta-induced chondrocyte anabolic and catabolic imbalance by activating FoxO1-mediated autophagy in human chondrocytes. FEBS J. 2020, 287, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Choi, M.H.; Kim, H.A. 29-kDa FN-f inhibited autophagy through modulating localization of HMGB1 in human articular chondrocytes. BMB Rep. 2018, 51, 508–513. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Jiang, D. HOTAIR-induced apoptosis is mediated by sponging miR-130a-3p to repress chondrocyte autophagy in knee osteoarthritis. Cell Biol. Int. 2020, 44, 524–535. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Y.; Song, W.; Ma, T.; Wang, K. microRNA-590-5p targets transforming growth factor beta1 to promote chondrocyte apoptosis and autophagy in response to mechanical pressure injury. J. Cell Biochem. 2018, 119, 9931–9940. [Google Scholar] [CrossRef]
- Liao, J.; Yu, X.; Chen, J.; Wu, Z.; He, Q.; Zhang, Y.; Song, W.; Lou, J.; Tao, Q. Knowledge mapping of autophagy in osteoarthritis from 2004 to 2022: A bibliometric analysis. Front. Immunol. 2023, 14, 1063018. [Google Scholar] [CrossRef] [PubMed]
- Kao, W.C.; Chen, J.C.; Liu, P.C.; Lu, C.C.; Lin, S.Y.; Chuang, S.C.; Wu, S.C.; Chang, L.H.; Lee, M.J.; Yang, C.D.; et al. The Role of Autophagy in Osteoarthritic Cartilage. Biomolecules 2022, 12, 1357. [Google Scholar] [CrossRef] [PubMed]
- Jun, Q.; Jin, Z.; Jian, J.; Xiao, R.; Qiu, L.; Jin, M.; Ni, H. Identification of autophagy-related gene in osteoarthritis articular cartilage and their roles in immune infiltration. Front. Immunol. 2023, 14, 1263988. [Google Scholar]
- Ziwei, O.; Lei, D.; Feng, Y.; Ke, W.; Yong, C.; Shufang, L.; Renpeng, Z.; Yingjie, Z.; Wei, H. Cartilage-Related Collagens in Osteoarthritis and Rheumatoid Arthritis: From Pathogenesis to Therapeutics. Int. J. Mol. Sci. 2023, 24, 9841. [Google Scholar]
- Pan, L.; Fuqiang, G.; Dongsheng, N.; Xichun, S.; Qiang, S.; Chongjun, G.; Yuqi, L.; Wei, S. The Role of Autophagy in Chondrocyte Metabolism and Osteoarthritis: A Comprehensive Research Review. Biomed. Res. Int. 2019, 2019, 5171602. [Google Scholar]
- Salucci, S.; Falcieri, E.; Battistelli, M. Chondrocyte death involvement in osteoarthritis. Cell Tissue Res. 2022, 389, 159–170. [Google Scholar] [CrossRef]
- Vellai, T. Autophagy genes and ageing. Cell Death Differ. 2009, 16, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Cecconi, F.; Levine, B. The role of autophagy in mammalian development: Cell makeover rather than cell death. Dev. Cell 2008, 15, 344–357. [Google Scholar] [CrossRef] [PubMed]
- Klionsky, D.J.; Emr, S.D. Autophagy as a regulated pathway of cellular degradation. Science 2000, 290, 1717–1721. [Google Scholar] [CrossRef] [PubMed]
- Levine, B.; Kroemer, G. Autophagy in the pathogenesis of disease. Cell 2008, 132, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Codogno, P.; Meijer, A.J. Autophagy and signaling: Their role in cell survival and cell death. Cell Death Differ. 2005, 12 (Suppl. S2), 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Wan, F.; Dutta, S.; Welsh, S.; Liu, Z.; Freundt, E.; Baehrecke, E.H.; Lenardo, M. Autophagic programmed cell death by selective catalase degradation. Proc. Natl. Acad. Sci. USA 2006, 103, 4952–4957. [Google Scholar] [CrossRef] [PubMed]
- Mizushima, N.; Levine, B.; Cuervo, A.M.; Klionsky, D.J. Autophagy fights disease through cellular self-digestion. Nature 2008, 451, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
- Outerbridge, R.E. The etiology of chondromalacia patellae. Clin. Orthop. Relat. Res. 2001, 389, 5–8. [Google Scholar] [CrossRef] [PubMed]
- van den Borne, M.P.; Raijmakers, N.J.; Vanlauwe, J.; Victor, J.; de Jong, S.N.; Bellemans, J.; Saris, D.B.; International Cartilage Repair, S. International Cartilage Repair Society (ICRS) and Oswestry macroscopic cartilage evaluation scores validated for use in Autologous Chondrocyte Implantation (ACI) and microfracture. Osteoarthr. Cartil. 2007, 15, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Goutas, A.; Syrrou, C.; Papathanasiou, I.; Tsezou, A.; Trachana, V. The autophagic response to oxidative stress in osteoarthritic chondrocytes is deregulated. Free Radic. Biol. Med. 2018, 126, 122–132. [Google Scholar] [CrossRef] [PubMed]
- King, J.S.; Veltman, D.M.; Insall, R.H. The induction of autophagy by mechanical stress. Autophagy 2011, 7, 1490–1499. [Google Scholar] [CrossRef] [PubMed]
- Caramés, B.; Taniguchi, N.; Seino, D.; Blanco, F.J.; D’Lima, D.; Lotz, M. Mechanical injury suppresses autophagy regulators and pharmacologic activation of autophagy results in chondroprotection. Arthritis Rheum. 2012, 64, 1182–1192. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, Q.; Yang, W.; Chen, J.; Wang, Y. Metabolic syndrome meets osteoarthritis. Nat. Rev. Rheumatol. 2012, 8, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Cheng, Y.; Shao, D.; Chen, J.; Sang, Y.; Gui, T.; Luo, S.; Li, J.; Chen, C.; Ye, Y.; et al. Metabolic Syndrome Increases the Risk for Knee Osteoarthritis: A Meta-Analysis. Evid. Based Complement. Altern. Med. 2016, 2016, 7242478. [Google Scholar] [CrossRef] [PubMed]
- Le Clanche, S.; Bonnefont-Rousselot, D.; Sari-Ali, E.; Rannou, F.; Borderie, D. Inter-relations between osteoarthritis and metabolic syndrome: A common link? Biochimie 2016, 121, 238–252. [Google Scholar] [CrossRef] [PubMed]
- Courties, A.; Gualillo, O.; Berenbaum, F.; Sellam, J. Metabolic stress-induced joint inflammation and osteoarthritis. Osteoarthr. Cartil. 2015, 23, 1955–1965. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hunter, D.; Xu, J.; Ding, C. Metabolic triggered inflammation in osteoarthritis. Osteoarthr. Cartil. 2015, 23, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Chao, P.; Cheng, C.; Xin, C.; Hui, L.; Li, X.; Ping, X.; Tao, X. The role of AGEs in pathogenesis of cartilage destruction in osteoarthritis. Bone Joint Res. 2022, 11, 292–300. [Google Scholar]
- Siri-Tarino, P.W.; Sun, Q.; Hu, F.B.; Krauss, R.M. Saturated fatty acids and risk of coronary heart disease: Modulation by replacement nutrients. Curr. Atheroscler. Rep. 2010, 12, 384–390. [Google Scholar] [CrossRef]
- Puenpatom, R.A.; Victor, T.W. Increased prevalence of metabolic syndrome in individuals with osteoarthritis: An analysis of NHANES III data. Postgrad. Med. 2009, 121, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Engstrom, G.; Gerhardsson de Verdier, M.; Rollof, J.; Nilsson, P.M.; Lohmander, L.S. C-reactive protein, metabolic syndrome and incidence of severe hip and knee osteoarthritis. A population-based cohort study. Osteoarthr. Cartil. 2009, 17, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Marks, R.; Allegrante, J.P. Comorbid disease profiles of adults with end-stage hip osteoarthritis. Med. Sci. Monit. 2002, 8, CR305–CR309. [Google Scholar] [PubMed]
- Lopez de Figueroa, P.; Lotz, M.K.; Blanco, F.J.; Carames, B. Autophagy activation and protection from mitochondrial dysfunction in human chondrocytes. Arthritis Rheumatol. 2015, 67, 966–976. [Google Scholar] [CrossRef] [PubMed]
- Blanco, F.J.; Rego, I.; Ruiz-Romero, C. The role of mitochondria in osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 161–169. [Google Scholar] [CrossRef]
- Green, D.R.; Galluzzi, L.; Kroemer, G. Mitochondria and the autophagy-inflammation-cell death axis in organismal aging. Science 2011, 333, 1109–1112. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| Study | Reagents | Condition of Subject’s Cartilage | Act of Reagents in Autophagy | Role of Reagents in Osteoarthritis | Related Mechanisms |
|---|---|---|---|---|---|
| Ribeiro et al. [22] | Insulin | OA human chondrocyte | Inhibition | Induction | Autophagy via Akt/mTOR signaling pathway. Activation of inflammation (loss of proteoglycans, increased MMP-13 and IL-1β). |
| Hwang et al. [23] | Monosodium urate (MSU) | OA human chondrocyte | Activation | Induction | Autophagy via Akt/mTOR signaling pathway. Independent of other cell death mechanisms, including apoptosis, ER stress-induced death, necroptosis, and pyroptosis. |
| Shen et al. [24] | Oxidized low density lipoprotein (Ox-LDL) | OA human chondrocyte | Activation | Induction | Increased ox-LDL and lectin-like ox-LDL receptor-1 (LOX-1) expression level was found in OA patients. Tumor necrosis factor-α mediated chondrocyte death. |
| Li et al. [25] | Plant homeodomain finger protein 23 (PHF 23) | OA human chondrocyte | Inhibition | Induction | Expression of PHF 23 increased in OA and was induced by IL-1β through inflammatory stress. PHF 23 suppressed autophagy of chondrocytes and accelerated apoptosis. |
| Wangyang et al. [26] | P63 | OA human chondrocyte | Inhibition | Induction | P63 was overexpressed in OA patients. P63 upregulation correlated with suppressed autophagy and cell viability. |
| Sekar et al. [27] | Saturated fatty acid (palmitic acid (PA), stearic acid (SA), lauric acid (LA), myristic acid (MA)) | OA human chondrocyte | PA, SA, MA: Autophagy activation LA: Similar to control | PA, SA, MA: OA inductionLA: Similar to control | Autophagy via NF-κB signaling pathway. PA, SA, MA treatment significantly decreased early chondrogenic markers such as ACAN, COL2, and SOX9 and significantly increased degenerative markers such as MMP13, ADAMTS4, and ADAMTS5. LA showed similar expressions in comparison with the controls. |
| Lee et al. [10] | Delphinidin | Normal human chondrocytes cell line (C28/I2), | Activation | Prevention | Delphinidin inhibited oxidative stress-induced apoptosis while it activated autophagy via NF-κB and Nrf2 pathways. |
| Duan et al. [28] | AdipoRon | OA human chondrocyte | Activation | Prevention | AdipoRon significantly alleviates the calcification of OA chondrocytes via activating AMPK/mTOR signaling to promote autophagy. |
| Xiao et al. [29] | Morroniside | OA human chondrocyte | Inhibition | Prevention | Morroniside inhibited chondrocyte autophagy through PI3K/AKT/mTOR signaling, thus it prevented cell death. Overexpression of autophagy enhanced the protection of Morroniside on chondrocytes. |
| Khan et al. [30] | Sucrose | OA human chondrocyte | Activation | Prevention | Sucrose induced autophagy in vitro dependent on the activation of AKT/mTOR/P70S6K signaling pathway and independent of ROS. Sucrose activated autophagy blocked IL-1β induced apoptosis and mRNA expression of MMP-13, COX-2, PGE-2, and IL-6. |
| Wang et al. [20] | Advanced glycation end products (AGEs) | Normal human chondrocyte | Biphasic effects | Biphasic effects | Low doses of AGEs over a short amount of time stimulated chondrocyte proliferation and autophagy by limiting phosphorylation of Akt/mTOR signaling. High dose and long exposure to AGEs inhibited cell viability and autophagy by increasing phosphorylation of Akt/mTOR signaling. AGEs can downregulate PPARG and that PPARG maintains cell viability by activating the Akt/mTOR signaling pathway as well as inducing autophagy. |
| Carames et al. [31] | Glucosamine | Normal human chondrocyte | Activation | Prevention | Glucosamine is an effective autophagy activator, and the enhancement of autophagy was mainly dependent on the Akt/FOXO and mTOR pathway. |
| Ansari et al. [32] | Butein | OA human chondrocyte | Activation | Prevention | Butein increased the phosphorylation of AMPKαThr-172, TSCSer-1387, and ULK1Ser-317 and inhibited the phosphorylation of mTORSer-2448. Increased autophagy flux that correlated with the suppression of the IL-1β mediated expression of IL-6. |
| Liu et al. [33] | Astragaloside Ⅳ (AST) | OA human chondrocyte | Activation | Prevention | AST-mediated autophagy protected against chondrocyte apoptosis induced by IL-1β. |
| Moussa et al. [34] | Platelet rich plasma (PRP) | OA human chondrocyte | Activation | Prevention | PRP increased significantly the proliferation of chondrocytes, decreased apoptosis and increased autophagy via FOXO1, FOXO3, HIF-1. PRP caused a significant decrease in MMP3, MMP13, ADAMTS-5, IL-6, and COX-2 while increasing TGF-β, aggrecan, collagen type 2, TIMPs and intracellular IL-4, IL-10, IL-13. |
| Nogueira-Recalde et al. [35] | Fenofibrate (FN) | OA and ageing human chondrocyte | Activation | Prevention | FN (PPARα agonist) reduced proteoglycan loss and protected against cartilage degradation. PPARα was mainly expressed in the superficial zone in non-OA cartilage with decreased expression in OA patients. FN reduced both senescence and inflammation and increased autophagy in both aging human and OA chondrocytes. |
| Cetrullo et al. [36] | Hydroxytyrosol (HT) | Normal human chondrocytes cell line (C28/I2), OA human chondrocyte | Activation | Prevention | The protective effect requires the deacetylase sirtuin 1 (SIRT-1) and silencing of this enzyme prevented HT from promoting the autophagic process and cell survival. HT supports autophagy even in a SIRT-1-independent manner, by increasing p62 transcription, required for autophagic degradation of polyubiquitin-containing bodies. HT exerts its cell protective action in C28/I2 line and human OA chondrocytes by the same modalities. |
| Ansari et al. [37] | Butea monosperma (Butein, BME) | OA human chondrocyte | Activation | Prevention | BME activated autophagy via inhibition of mTOR pathway. BME suppressed the IL-1β induced expression of IL-6, MMP-3, MMP-9, and MMP-13. |
| Yu et al. [38] | T-2, HT-2 toxin | Normal human chondrocytes cell line (C28/I2) | Activation | Prevention | T-2 and HT-2 toxins induce apoptosis and autophagy, and the level of oxidative stress plays an important role in autophagy activation. The expression levels of apoptosis and autophagy induced by T-2 toxin were significantly higher when compared with those levels induced by the HT-2 toxin. The activation of autophagy can reduce oxidative damage and apoptosis. |
| Liao et al. [39] | Resveratrol (Sirt I inducer) | OA human chondrocyte | High levels of Sirt I inhibited autophagy in OA | Prevention | Sirt I regulates autophagy by interacting with Atg7. The expression of Sirt I might be age-related: it is high in young people and decreased in elderly and OA patients. Of note, the high levels of Sirt I reduced autophagy in OA. Through increasing the activity of Sirt I the autophagic cell death of OA chondrocyte could be inhibited. |
| Zhong et al. [40] | miRNA-335-5p | OA human chondrocyte | Activation | Prevention | The expression of miRNA-355-5p was significantly lower in OA chondrocytes. miRNA-355-5p can significantly alleviate inflammation in human OA chondrocytes by activating autophagy. |
| Wang et al. [41] | miR-140-5p/miR-149 | OA human chondrocyte | Activation | Prevention | The overexpression of miR-140-5p/miR-149 inhibited apoptosis and promoted proliferation and autophagy of primary human chondrocytes via downregulating FUT1. |
| D’Adamo et al. [42] | miRNA-155 | Normal human chondrocyte and cell line (T/C28a2) | Inhibition | Induction | miRNA-155 regulates autophagy by suppressing MAP1LC3, GABARAPL1, Atg3, Atg5, Atg, 14, ULK1, and FOXO3.miRNA-155 inhibited autophagy by activating mTOR pathway. |
| Yang et al. [43] | miRNA-411 | OA induced C28/I2 chondrocyte cell line by IL-1β | Mimic: inhibition, Inhibitor: activation | Mimic: prevention, Inhibitor: induction | miRNA-411 regulates autophagy by targeting HIF-1α. miRNA-411 mimic inhibited autophagy by reducing HIF-1α while miRNA-411 inhibitor activated autophagy by increasing HIF-1α in chondrocytes. miRNA-411 was downregulated in OA chondrocyte, so this causes activation of autophagy by increasing HIF-1α. Thus, downregulated miRNA-411 is closely associated with the development of OA. |
| Tian et al. [44] | upregulated small nuclear RNA host gene 7 (SNHG7), downregulated miR-34a-5p | OA human chondrocyte | Inhibition | Prevention | SNHG7 and SYVN1 were downregulated, but miR-34a-5p was upregulated in OA. Upregulated SNHG7 promoted cell proliferation as well as inhibited cell apoptosis and autophagy by sponging miR-34a-5p through regulating SYNV1 in OA cells. |
| Yang et al. [45] | Long non-coding RNA reprogramming (lncRNA-ROR) | OA human chondrocyte | Activation | Prevention | Level of lncRNA-ROR was decreased in OA. Overexpression of lncRNA-ROR dramatically promoted cell viability of OA chondrocytes. Knockdown lncRNA-ROR inhibited apoptosis and promoted autophagy by regulating HIF-1α and p53. |
| Akasaki et al. [46] | Downregulated FOXO transcription factors | OA human chondrocyte | Inhibition | Induction | Reduced expression of FOXO transcription factors in chondrocytes increased susceptibility to cell death induced by oxidative stress. This was associated with reduced antioxidant proteins and autophagy-related proteins. FOXO downregulation: ADAMTS-4↑ and Chemerin↑ in OA chondrocytes. |
| Huang et al. [47] | Knockdown of serum- and glucocorticoid-regulated kinase 1 (SGK1) | OA human chondrocyte | Activation | Prevention | SGK1 was upregulated in OA cartilage. SGK1 knockdown leads to increased autophagy, subsequently inhibiting OA by regulating FOXO1. SGK1 knockdown: collagen II↑, aggrecan↑, ADAMTS-5↓, MMP-13↓, disintegrin↓ |
| Hwang et al. [48] | 29 kDa fibronectin fragment (29 kDa FN-f) | OA human chondrocyte | Inhibition | Induction | HMGB1 level was significantly lower in human OA cartilage. 29-kDa FN-f inhibits chondrocyte autophagy by modulating the mTOR pathway and HMGB1 signaling pathway. |
| He et al. [49] | Hox transcript antisense intergenic RNA (HOTAIR) | OA human chondrocyte | Inhibition | Induction | Upregulation of HOTAIR and downregulation of miR130a-3p were found in OA. Expression of HOTAIR resulted in apoptosis events caused by the sponging of miR-130a-3p to suppress autophagy, subsequently induced OA. |
| Wang et al. [50] | Upregulated microRNA-590-5p (miR-590-5p) | Normal human chondrocyte | Activation | Induction | Mechanical pressure injury resulted in a significantly increased expression of miR-590-5p and decreased expression of TGFβ1. The miR-590-5p targets TGFβ1 to regulate chondrocyte apoptosis and autophagy in response to mechanical pressure injury. Decreased miR-590-5p leads to increased cell viability and decreased autophagy. And, decreased TGFβ1 leads to increased autophagy and apoptosis. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-Y.; Bahar, M.E.; Kim, C.-W.; Seo, M.-S.; Song, M.-G.; Song, S.-Y.; Kim, S.-Y.; Kim, D.-R.; Kim, D.-H. Autophagy in Osteoarthritis: A Double-Edged Sword in Cartilage Aging and Mechanical Stress Response: A Systematic Review. J. Clin. Med. 2024, 13, 3005. https://doi.org/10.3390/jcm13103005
Lee D-Y, Bahar ME, Kim C-W, Seo M-S, Song M-G, Song S-Y, Kim S-Y, Kim D-R, Kim D-H. Autophagy in Osteoarthritis: A Double-Edged Sword in Cartilage Aging and Mechanical Stress Response: A Systematic Review. Journal of Clinical Medicine. 2024; 13(10):3005. https://doi.org/10.3390/jcm13103005
Chicago/Turabian StyleLee, Dong-Yeong, Md Entaz Bahar, Chang-Won Kim, Min-Seok Seo, Myung-Geun Song, Sang-Youn Song, Soung-Yon Kim, Deok-Ryong Kim, and Dong-Hee Kim. 2024. "Autophagy in Osteoarthritis: A Double-Edged Sword in Cartilage Aging and Mechanical Stress Response: A Systematic Review" Journal of Clinical Medicine 13, no. 10: 3005. https://doi.org/10.3390/jcm13103005
APA StyleLee, D.-Y., Bahar, M. E., Kim, C.-W., Seo, M.-S., Song, M.-G., Song, S.-Y., Kim, S.-Y., Kim, D.-R., & Kim, D.-H. (2024). Autophagy in Osteoarthritis: A Double-Edged Sword in Cartilage Aging and Mechanical Stress Response: A Systematic Review. Journal of Clinical Medicine, 13(10), 3005. https://doi.org/10.3390/jcm13103005






