Modified Implant Fixation Technique Is an Alternative for Patients with an Anterior Cruciate Ligament Tear in Limited Resource Settings: A Comparison Functional Outcome Study with Polyether Ether Ketone and Bioabsorbable Screws
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting and Population
2.3. Inclusion and Exclusion Criteria
2.4. Data Collection
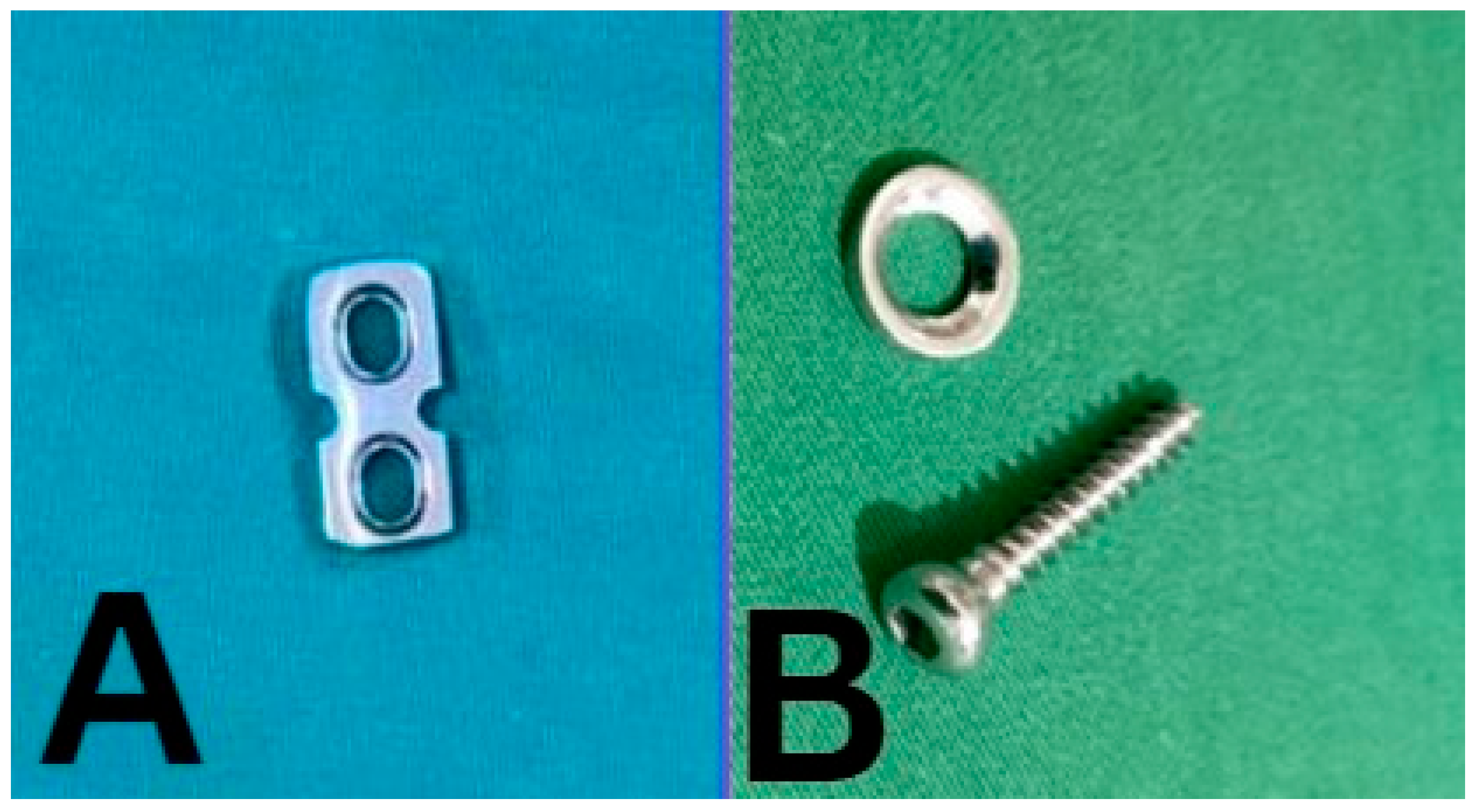
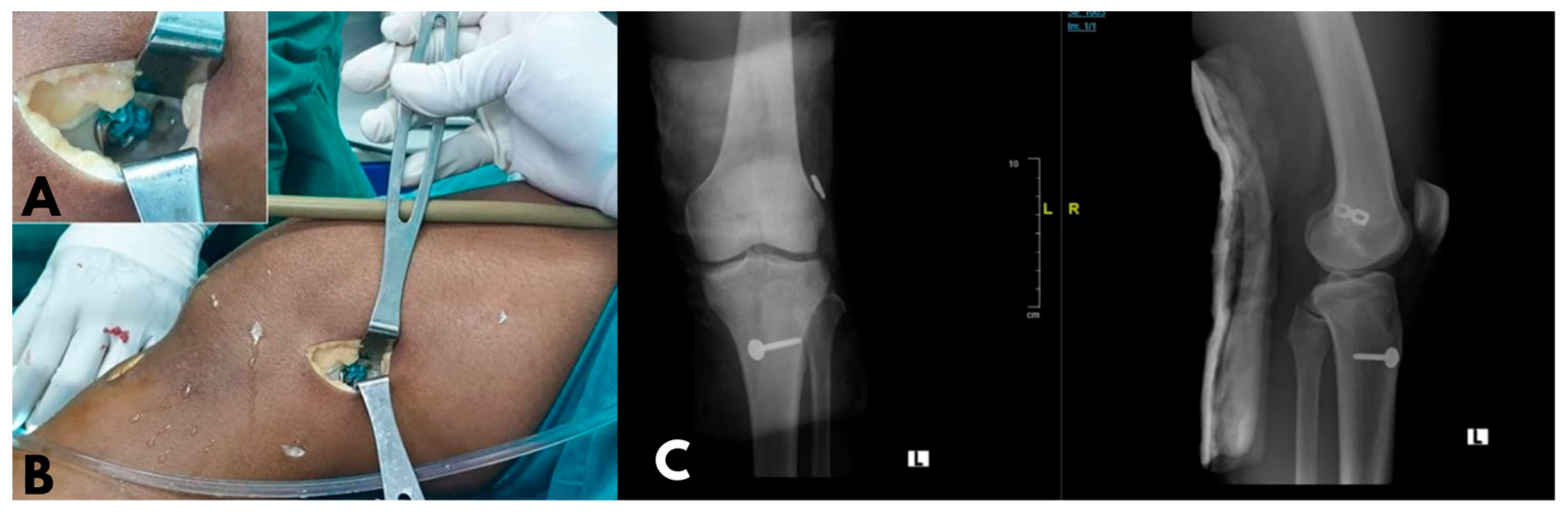
2.5. Operative Technique
2.6. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Lysholm Score
3.3. IKDC Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gans, I.; Retzky, J.S.; Jones, L.C.; Tanaka, M.J. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association sports: The Injury Surveillance Program, 2004–2014. Orthop J. Sports Med. 2018, 6, 2325967118777823. [Google Scholar] [CrossRef] [PubMed]
- Chia, L.; Silva, D.D.O.; Whalan, M.; McKay, M.J.; Sullivan, J.; Fuller, C.W.; Pappas, E. Non-contact anterior cruciate ligament injury epidemiology in team-ball sports: A systematic review with meta-analysis by sex, age, sport, participation level, and exposure type. Sports Med. 2022, 52, 2447–2467. [Google Scholar] [CrossRef]
- McDermott, E.; DeFoor, M.T.; Blaber, O.K.; Aman, Z.S.; DePhillipo, N.N.; Dekker, T.J. Biomechanical comparison of anterior cruciate ligament reconstruction fixation methods and implications on clinical outcomes. Ann. Joint. 2023, 8, 15. [Google Scholar] [CrossRef]
- Zeng, C.; Lei, G.; Gao, S.; Luo, W. Methods and devices for graft fixation in anterior cruciate ligament reconstruction. Cochrane Database Syst. Rev. 2018, 2018, CD010730. [Google Scholar] [CrossRef]
- Abulhasan, J.F.; Grey, M.J. Anatomy and physiology of knee stability. J. Funct. Morphol. Kinesiol. 2017, 2, 34. [Google Scholar] [CrossRef]
- Deviandri, R.; van der Veen, H.C.; Lubis, A.M.T.; Utoyo, G.A.; van den Akker-Scheek, I.; Postma, M.J. Burden and cost of anterior cruciate ligament reconstruction and reimbursement of its treatment in a developing country: An observational study in Indonesia. Clin. Outcomes Res. 2022, 14, 479–486. [Google Scholar] [CrossRef]
- Mathew, G.; Agha, R.; Albrecht, J.; Goel, P.; Mukherjee, I.; Pai, P.; D’cruz, A.K.; Nixon, I.J.; Roberto, K.; Enam, S.A.; et al. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. 2021, 96, 106165. [Google Scholar] [CrossRef] [PubMed]
- Deviandri, R.; der Veen, H.C.V.; Lubis, A.M.; Postma, M.J.; Van den Akker-Scheek, I. Translation and Psychometric Analysis of the Indonesian Versions of the Lysholm and Tegner Scores for Patients with Anterior Cruciate Ligament Injuries. Orthop. J. Sports Med. 2022, 10, 23259671211066506. [Google Scholar] [CrossRef] [PubMed]
- Deviandri, R.; van der Veen, H.C.; Lubis, A.M.T.; Postma, M.J.; van den Akker-Scheek, I. Translation, Cross-Cultural Adaptation, Validity, and Reliability of the Indonesian Version of the IKDC Subjective Knee Form. Orthop. J. Sports Med. 2021, 9, 23259671211038372. [Google Scholar] [CrossRef]
- Briggs, K.K.; Steadman, J.R.; Hay, C.J.; Hines, S.L. Lysholm score and Tegner activity level in individuals with normal knees. Am. J. Sports Med. 2009, 37, 898–901. [Google Scholar] [CrossRef]
- Irrgang, J.J.; Ho, H.; Harner, C.D.; Fu, F.H. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 1998, 6, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Mouarbes, D.; Menetrey, J.; Marot, V.; Courtot, L.; Berard, E.; Cavaignac, E. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring-tendon autografts. Am. J. Sports Med. 2019, 47, 3531–3540. [Google Scholar] [CrossRef] [PubMed]
- Higgins, L.D.; Taylor, M.K.; Park, D.; Ghodadra, N.; Marchant, M.; Pietrobon, R.; Cook, C. International Knee Documentation Committee. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt. Bone Spine 2007, 74, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Shumborski, S.; Heath, E.; Salmon, L.J.; Roe, J.P.; Linklater, J.P.; Facek, M.; Pinczewski, L.A. A randomized controlled trial of PEEK versus titanium interference screws for anterior cruciate ligament reconstruction with 2-year follow-up. Am. J. Sports Med. 2019, 47, 2386–2393. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Jiang, S.D.; Jiang, L.S.; Dai, L.Y. Bioabsorbable versus metallic interference screw fixation in anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials. Arthroscopy 2010, 26, 705–713. [Google Scholar] [CrossRef]
- Xu, B.; Yin, Y.; Zhu, Y.; Yin, Y.; Fu, W. Comparison of bioabsorbable and metallic interference screws for graft fixation during ACL reconstruction: A meta-analysis of randomized controlled trials. Orthop. J. Sports Med. 2021, 9, 23259671211021576. [Google Scholar] [CrossRef]
- Emond, C.E.; Woelber, E.B.; Kurd, S.K.; Ciccotti, M.G.; Cohen, S.B. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: A meta-analysis. J. Bone Jt. Surg. Am. 2011, 93, 572–580. [Google Scholar] [CrossRef]
- Nie, S.; Zhou, S.; Huang, W. Femoral fixation methods for hamstring graft in anterior cruciate ligament reconstruction: A network meta-analysis of controlled clinical trials. PLoS ONE 2022, 17, e0275097. [Google Scholar] [CrossRef] [PubMed]
- Ekdahl, M.; Wang, J.; Ronga, M.; Fu, F. Graft healing in anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 935–947. [Google Scholar] [CrossRef] [PubMed]
- Janssen, R.P.A.; Scheffler, S.U. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2102–2108. [Google Scholar] [CrossRef]
- Eggerding, V.; Reijman, M.; Meuffels, D.E.; van Es, E.; van Arkel, E.; Brand, I.v.D.; van Linge, J.; Zijl, J.; Bierma-Zeinstra, S.M.; Koopmanschap, M. ACL reconstruction for all is not cost-effective after acute ACL rupture. Br. J. Sports Med. 2022, 56, 24–28. [Google Scholar] [CrossRef]
- Kiadaliri, A.A.; Englund, M.; Lohmander, L.S.; Carlsson, K.S.; Frobell, R.B. No economic benefit of early knee reconstruction over optional delayed reconstruction for ACL tears: Registry enriched randomised controlled trial data. Br. J. Sports Med. 2016, 50, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Farshad, M.; Gerber, C.; Meyer, D.C.; Schwab, A.; Blank, P.R.; Szucs, T. Reconstruction versus conservative treatment after rupture of the anterior cruciate ligament: Cost effectiveness analysis. BMC Health Serv. Res. 2011, 11, 317. [Google Scholar] [CrossRef] [PubMed]
| Indicator | N | Mean ± SD | |
|---|---|---|---|
| Age (year) | 26.50 ± 6.50 | ||
| Gender | Male | 29 (87.9%) | |
| Female | 4 (12.1%) | ||
| Implant | Modified implant group | 10 (30.3%) | |
| PEEK group | 10 (30.3%) | ||
| Bioabsorbable group | 13 (39.4%) | ||
| Affected Knee (Right/Left) | Modified implant group | 5/5 | |
| PEEK group | 6/4 | ||
| Bioabsorable group | 9/4 | ||
| Follow up time (month) | 12.30 ± 0.24 | ||
| Lysholm Score (Mean ± SD) | IKDC Score (Mean ± SD) | |||
|---|---|---|---|---|
| 6 months | 12 months | 6 months | 12 months | |
| Modified implant group | 80.50 ± 9.50 | 87.90 ± 5.50 | 79.90 ± 9.82 | 90.00 ± 5.60 |
| PEEK group | 85.3 ± 4.42 | 89.70 ± 2.75 | 82.60 ± 5.91 | 94.00 ± 4.37 |
| Bioabsorbable group | 78.85 ± 7.96 | 89.07 ± 2.75 | 76.46 ± 6.04 | 90.85 ± 5.41 |
| p-value | 0.140 | 0.770 | 0.150 | 0.200 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakti, M.; Wawolumaja, A.F.I.; Saleh, R.; Usman, M.A.; Arifin, J.; Johan, M.P. Modified Implant Fixation Technique Is an Alternative for Patients with an Anterior Cruciate Ligament Tear in Limited Resource Settings: A Comparison Functional Outcome Study with Polyether Ether Ketone and Bioabsorbable Screws. J. Clin. Med. 2024, 13, 2964. https://doi.org/10.3390/jcm13102964
Sakti M, Wawolumaja AFI, Saleh R, Usman MA, Arifin J, Johan MP. Modified Implant Fixation Technique Is an Alternative for Patients with an Anterior Cruciate Ligament Tear in Limited Resource Settings: A Comparison Functional Outcome Study with Polyether Ether Ketone and Bioabsorbable Screws. Journal of Clinical Medicine. 2024; 13(10):2964. https://doi.org/10.3390/jcm13102964
Chicago/Turabian StyleSakti, Muhammad, Arian Fardin Ignatius Wawolumaja, Ruksal Saleh, Muhammad Andry Usman, Jainal Arifin, and Muhammad Phetrus Johan. 2024. "Modified Implant Fixation Technique Is an Alternative for Patients with an Anterior Cruciate Ligament Tear in Limited Resource Settings: A Comparison Functional Outcome Study with Polyether Ether Ketone and Bioabsorbable Screws" Journal of Clinical Medicine 13, no. 10: 2964. https://doi.org/10.3390/jcm13102964
APA StyleSakti, M., Wawolumaja, A. F. I., Saleh, R., Usman, M. A., Arifin, J., & Johan, M. P. (2024). Modified Implant Fixation Technique Is an Alternative for Patients with an Anterior Cruciate Ligament Tear in Limited Resource Settings: A Comparison Functional Outcome Study with Polyether Ether Ketone and Bioabsorbable Screws. Journal of Clinical Medicine, 13(10), 2964. https://doi.org/10.3390/jcm13102964







