Appendiceal Mucinous Neoplasms and Inflammatory Bowel Disease: Systematic Review of the Literature
Abstract
:1. Introduction
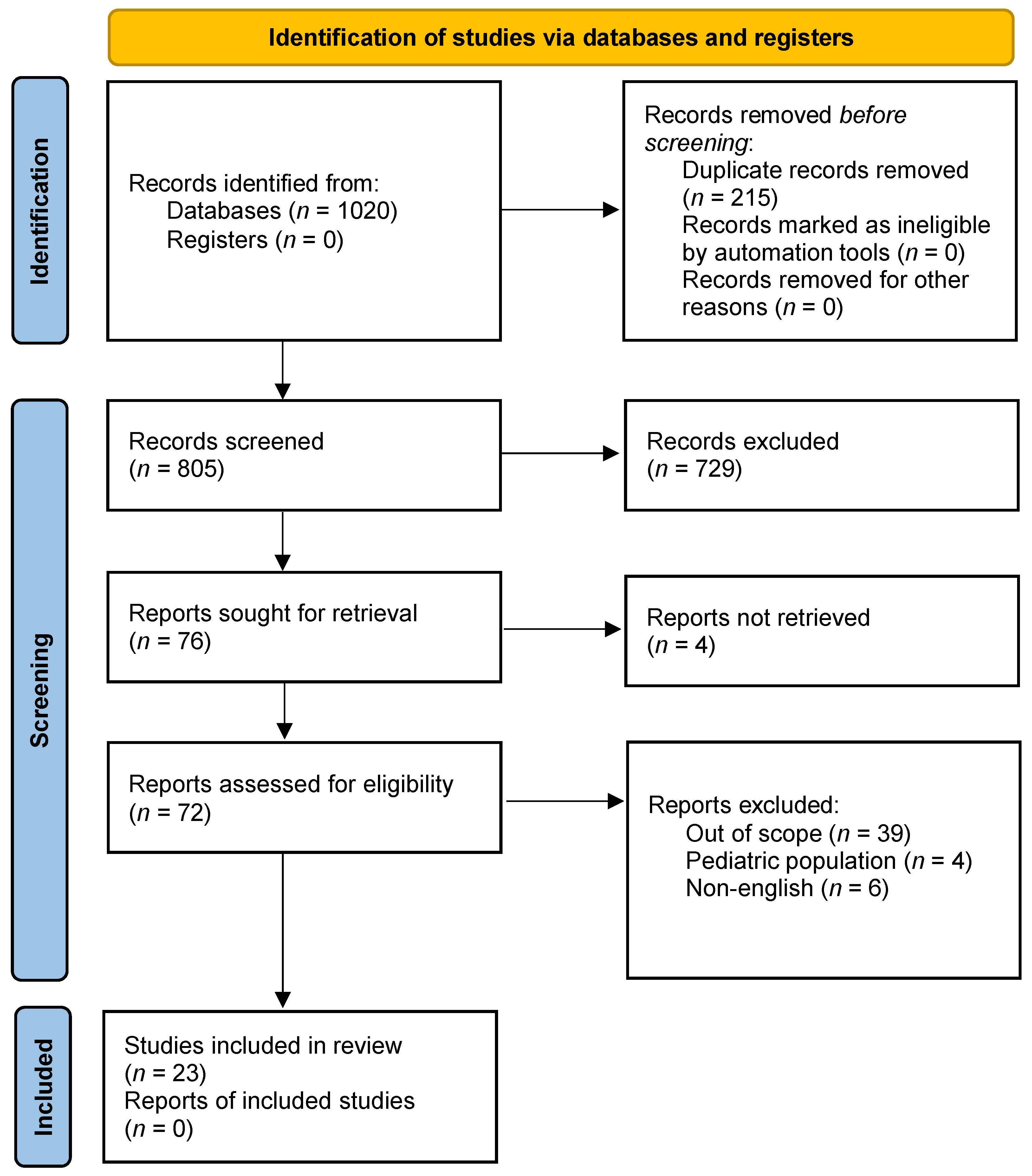
2. Materials and Methods
2.1. Protocol Registration
2.2. Study Characteristics
2.3. Information Sources, Study Selection and Data Extraction
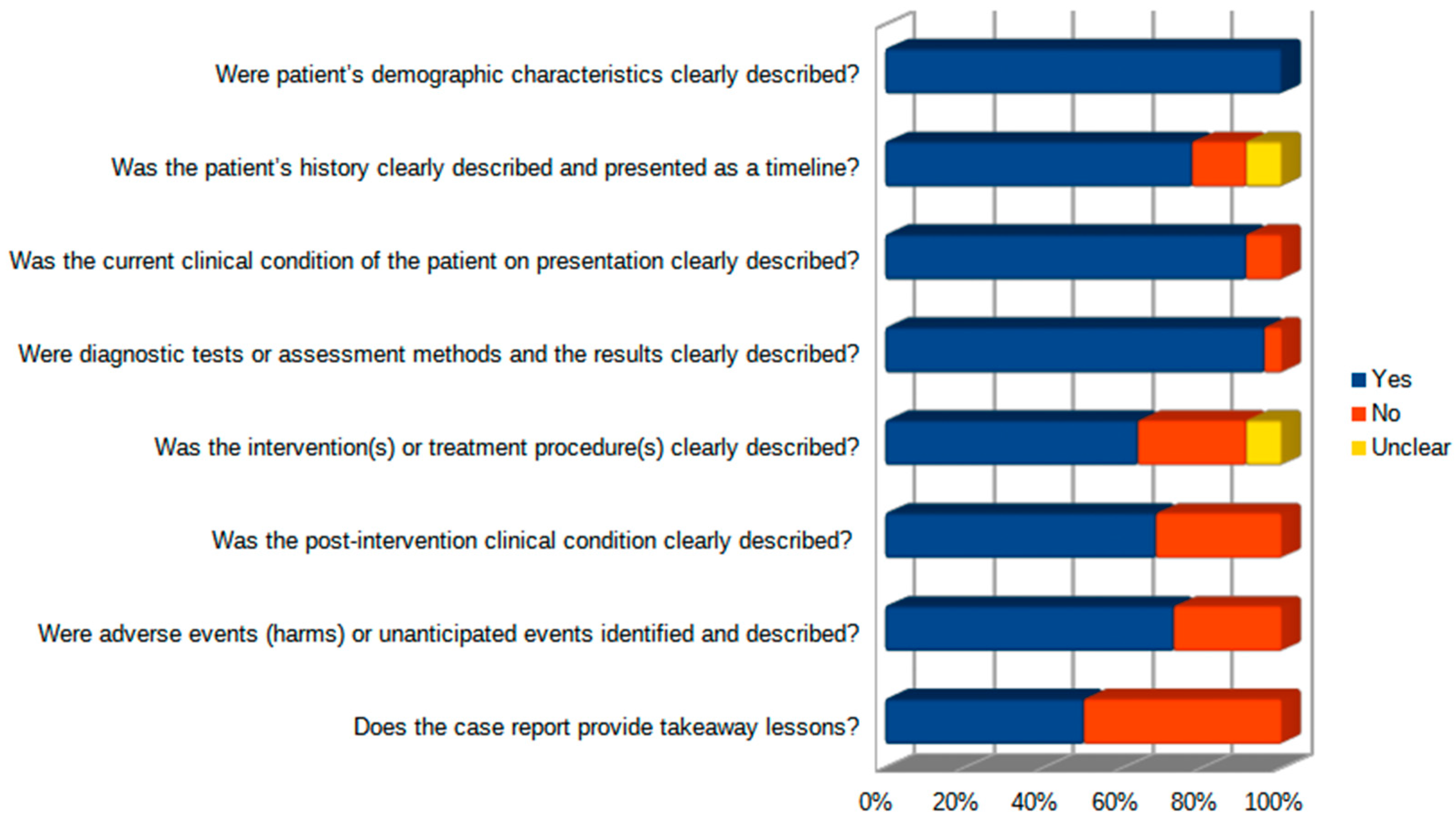
3. Results
3.1. Patients’ Characteristics
3.2. Surgical Management
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glasgow, S.C.; Gaertner, W.; Stewart, D.; Davids, J.; Alavi, K.; Paquette, I.M.; Steele, S.R.; Feingold, D.L. The American Society of Colon and Rectal Surgeons, Clinical Practice Guidelines for the Management of Appendiceal Neoplasms. Dis. Colon Rectum 2019, 62, 1425. [Google Scholar] [CrossRef] [PubMed]
- Stopenski, S.J.; Grigorian, A.; Carmichael, J.; Mills, S.; Brady, M.; Dolich, M.; Kuza, C.M.; Nguyen, N.T.; Nahmias, J. Risk Factors for Appendiceal Cancer after Appendectomy. Am. Surg. 2021, 87, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Carr, N.J.; Cecil, T.D.; Mohamed, F.; Sobin, L.H.; Sugarbaker, P.H.; González-Moreno, S.; Taflampas, P.; Chapman, S.; Moran, B.J. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am. J. Surg. Pathol. 2016, 40, 14. [Google Scholar] [CrossRef] [PubMed]
- Morano, W.F.; Gleeson, E.M.; Sullivan, S.H.; Padmanaban, V.; Mapow, B.L.; Shewokis, P.A.; Esquivel, J.; Bowne, W.B. Clinicopathological Features and Management of Appendiceal Mucoceles: A Systematic Review. Am. Surg. 2018, 84, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.J.; Thacker, P.G.; Grotz, T.E.; Graham, R.P.; Fletcher, J.G.; VanBuren, W.M.; Iyer, V.R.; Fidler, J.L.; Menias, C.O.; Wasif, N.; et al. Mucinous Appendiceal Neoplasms: Classification, Imaging, and HIPEC. Abdom. Radiol. 2019, 44, 1686–1702. [Google Scholar] [CrossRef]
- Leonards, L.M.; Pahwa, A.; Patel, M.K.; Petersen, J.; Nguyen, M.J.; Jude, C.M. Neoplasms of the Appendix: Pictorial Review with Clinical and Pathologic Correlation. Radiographics 2017, 37, 1059–1083. [Google Scholar] [CrossRef]
- Lien, W.-C.; Huang, S.-P.; Chi, C.-L.; Liu, K.-L.; Lin, M.-T.; Lai, T.-I.; Liu, Y.-P.; Wang, H.-P. Appendiceal Outer Diameter as an Indicator for Differentiating Appendiceal Mucocele from Appendicitis. Am. J. Emerg. Med. 2006, 24, 801–805. [Google Scholar] [CrossRef]
- Axelrad, J.E.; Lichtiger, S.; Yajnik, V. Inflammatory Bowel Disease and Cancer: The Role of Inflammation, Immunosuppression, and Cancer Treatment. World J. Gastroenterol. 2016, 22, 4794–4801. [Google Scholar] [CrossRef]
- Park, S.H.; Loftus, E.V.; Yang, S.-K. Appendiceal Skip Inflammation and Ulcerative Colitis. Dig. Dis. Sci. 2014, 59, 2050–2057. [Google Scholar] [CrossRef]
- Stangl, P.C.; Herbst, F.; Birner, P.; Oberhuber, G. Crohn’s Disease of the Appendix. Virchows Arch. 2002, 440, 397–403. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Miami, FL, USA, 2020; ISBN 9780648848806. [Google Scholar]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.E.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2000. [Google Scholar]
- Orta, L.; Trindade, A.J.; Luo, J.; Harpaz, N. Appendiceal Mucinous Cystadenoma Is a Neoplastic Complication Of IBD: Case-Control Study of Primary Appendiceal Neoplasms. Inflamm. Bowel Dis. 2009, 15, 415–421. [Google Scholar] [CrossRef]
- Matsushita, M.; Tanaka, T.; Omiya, M.; Okazaki, K. Significant Association of Appendiceal Neoplasms and Ulcerative Colitis Rather than Crohn’s Disease. Inflamm. Bowel Dis. 2010, 16, 735. [Google Scholar] [CrossRef] [PubMed]
- Uchino, M.; Ikeuchi, H.; Hata, K.; Minagawa, T.; Horio, Y.; Kuwahara, R.; Nakamura, S.; Watanabe, K.; Saruta, M.; Fujii, T.; et al. Intestinal Cancer in Patients with Crohn’s Disease: A Systematic Review and Meta-Analysis. J. Gastroenterol. Hepatol. 2021, 36, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, F.J.R.; do Couto Netto, S.D.; Akaishi, E.H.; Utiyama, E.M.; Menegozzo, C.A.M.; Rocha, M.C. Acute Appendicitis, Inflammatory Appendiceal Mass and the Risk of a Hidden Malignant Tumor: A Systematic Review of the Literature. World J. Emerg. Surg. 2017, 12, 12. [Google Scholar] [CrossRef] [PubMed]
- Nehme, F.; Schneider, A.; Hamid, F. Appendiceal Adenocarcinoma Associated with Ulcerative Colitis. ACG Case Rep. J. 2019, 6, e00255. [Google Scholar] [CrossRef] [PubMed]
- Wong, U.; Darwin, P. Appendiceal Mucocele Diagnosed in Patients with Inflammatory Bowel Disease Using Endoscopic Ultrasound. Case Rep. Med. 2012, 2012, 849892. [Google Scholar] [CrossRef]
- Kim, T.K.; Park, J.H.; Kim, J.Y.; Kim, B.C.; Kang, B.M.; Min, S.K.; Kim, J.W. Safety and Feasibility of Laparoscopic Surgery for Appendiceal Mucocele: A Multicenter Study. Surg. Endosc. 2018, 32, 4408–4414. [Google Scholar] [CrossRef]
- Takeda, Y.; Nakase, H.; Mikami, S.; Inoue, T.; Satou, S.; Sakai, Y.; Chiba, T. Possible Link between Ulcerative Colitis and in Situ Adenocarcinoma of an Appendiceal Mucocele: Importance of Inflammation in the Appendiceal Orifice Related to UC. Inflamm. Bowel Dis. 2008, 14, 873–874. [Google Scholar] [CrossRef]
- Guaglio, M.; Sinukumar, S.; Kusamura, S.; Milione, M.; Pietrantonio, F.; Battaglia, L.; Guadagni, S.; Baratti, D.; Deraco, M. Correction to: Clinical Surveillance After Macroscopically Complete Surgery for Low-Grade Appendiceal Mucinous Neoplasms (LAMN) with or Without Limited Peritoneal Spread: Long-Term Results in a Prospective Series. Ann. Surg. Oncol. 2018, 25, 987. [Google Scholar] [CrossRef]
- Foster, J.M.; Sleightholm, R.L.; Wahlmeier, S.; Loggie, B.; Sharma, P.; Patel, A. Early Identification of DPAM in At-Risk Low-Grade Appendiceal Mucinous Neoplasm Patients: A New Approach to Surveillance for Peritoneal Metastasis. World J. Surg. Oncol. 2016, 14, 243. [Google Scholar] [CrossRef] [PubMed]
- Fournier, K.; Rafeeq, S.; Taggart, M.; Kanaby, P.; Ning, J.; Chen, H.-C.; Overman, M.; Raghav, K.; Eng, C.; Mansfield, P.; et al. Low-Grade Appendiceal Mucinous Neoplasm of Uncertain Malignant Potential (LAMN-UMP): Prognostic Factors and Implications for Treatment and Follow-Up. Ann. Surg. Oncol. 2017, 24, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Honoré, C.; Caruso, F.; Dartigues, P.; Benhaim, L.; Chirica, M.; Goéré, D.; Elias, D. Strategies for Preventing Pseudomyxoma Peritonei After Resection of a Mucinous Neoplasm of the Appendix. Anticancer Res. 2015, 35, 4943–4947. [Google Scholar] [PubMed]
- McDonald, J.R.; O’Dwyer, S.T.; Rout, S.; Chakrabarty, B.; Sikand, K.; Fulford, P.E.; Wilson, M.S.; Renehan, A.G. Classification of and Cytoreductive Surgery for Low-Grade Appendiceal Mucinous Neoplasms. Br. J. Surg. 2012, 99, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Smeenk, R.M.; van Velthuysen, M.L.F.; Verwaal, V.J.; Zoetmulder, F. Appendiceal Neoplasms and Pseudomyxoma Peritonei: A Population Based Study. Eur. J. Surg. Oncol. 2008, 34, 196–201. [Google Scholar] [CrossRef]
- Moniakis, A.A.; Flamourakis, M.E.; Gkionis, I.G.; Giakoumakis, M.I.; Tsagkataki, E.S.; Kazamias, G.M.; Spiridakis, K.G.; Christodoulakis, M.S. Ileocolic Intussusception in a Woman: A Case Report and Literature Review. Am. J. Case Rep. 2021, 22, e933341-1–e933341-9. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.G.; Conlon, E.T.; Forde, G.; Byrnes, V.M.; Carroll, P.A. Adult Intussusception Secondary to an Appendiceal Tumour in a Patient with Ulcerative Colitis: A Case Report. Surg. Case Rep. 2020, 6, 234. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, T.; Chalmers, A.; Verbeke, C.; Saunders, R.; Everett, S. Appendiceal Mucocele in Ulcerative Colitis. Endoscopy 2010, 42, E105–E106. [Google Scholar] [CrossRef]
- Lakatos, P.L.; Gyori, G.; Halasz, J.; Fuszek, P.; Papp, J.; Jaray, B.; Lukovich, P.; Lakatos, L. Mucocele of the Appendix: An Unusual Cause of Lower Abdominal Pain in a Patient with Ulcerative Colitis-. A Case Report and Review of Literature. World J. Gastroenterol. WJG 2005, 11, 457–459. [Google Scholar] [CrossRef]
- Lyda, M.H.; Noffsinger, A.; Belli, J.; Fischer, J.; Fenoglio-Preiser, C.M. Multifocal Neoplasia Involving the Colon and Appendix in Ulcerative Colitis: Pathological and Molecular Features. Gastroenterology 1998, 115, 1566–1573. [Google Scholar] [CrossRef]
- Noaki, R.; Kawahara, H.; Watanabe, K.; Kobayashi, S.; Uchiyama, K.; Yanaga, K. Appendiceal Mucocele Detected under Treatment of Ulcerative Colitis. Case Rep. Gastroenterol. 2009, 3, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Kuester, D.; Dalicho, S.; Mönkemüller, K.; Benedix, F.; Lippert, H.; Guenther, T.; Roessner, A.; Meyer, F. Synchronous Multifocal Colorectal Carcinoma in a Patient with Delayed Diagnosis of Ulcerative Pancolitis. Pathol. Res. Pract. 2008, 204, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Lipka, S.; Katz, S. Appendiceal Adenocarcinoma in a Patient with Chronic Ulcerative Colitis: What Is the Appropriate Surgical Procedure? J. Crohns Colitis 2014, 8, 334–335. [Google Scholar] [CrossRef]
- Sonwalkar, S.A.; Denyer, M.E.; Verbeke, C.S.; Guillou, P.J. Cancer of Appendix as a Presenting Feature of Crohn’s Disease. Eur. J. Gastroenterol. Hepatol. 2002, 14, 1029. [Google Scholar] [CrossRef] [PubMed]
- Tonolini, M. Appendiceal Mucocele in Ulcerative Colitis: A Rare Association and a Crucial Preoperative Diagnosis. J. Gastrointest. Liver Dis. 2015, 24, 125–130. [Google Scholar]
- Pérez-Aguirre, J.; Villanueva Saenz, E.; Belmonte, M.C.; Martínez, P.H.M.; Márquez, R.M.L.; Carranza, R.J.M. Appendix Adenocarcinoma Associated with Ulcerative Colitis: A Case Report and Literature Review. Tech. Coloproctol. 2006, 10, 54–56. [Google Scholar] [CrossRef]
- Vukovic, J.; Vrebalov Cindro, P.; Tomic, S.; Tonkic, A. Signet Ring Carcinoma of the Appendix Presenting as Crohn’s Disease in a Young Male. Case Rep. Gastroenterol. 2018, 12, 277–285. [Google Scholar] [CrossRef]
- Zannoni, U.; Masci, C.; Bazzocchi, R.; Gandolfo, F.; Pezzi, A.; Alampi, G.; Biasco, G. Cancer of the Appendix in Long-Standing Ulcerative Colitis: A Case Report. Tumori J. 1997, 83, 958–959. [Google Scholar] [CrossRef]
- Simsek, M.; Linn, A.J.; de Boer, N.K.H. Pseudomyxoma Peritonei of the Appendix after Ileocecal Resection: Expect the Unexpected. Dig. Liver Dis. 2019, 51, 1486. [Google Scholar] [CrossRef]
- Abdulghaffar, S.; Badrawi, N.; Khairi, T.E.; Keloth, T.R.; Businge, P.E. Giant Appendiceal Mucocele as a First Manifestation in a Patient with Silent Ulcerative Colitis: A Case Report. Radiol. Case Rep. 2022, 17, 1335–1339. [Google Scholar] [CrossRef]
- Almogy, G.; Fellig, Y.; Paz, K.; Durst, A.; Eid, A. Adenocarcinoma of the Appendix Associated with Long-Standing Crohns Disease. Int. J. Color. Dis. 2001, 16, 408–409. [Google Scholar] [CrossRef] [PubMed]
- Fukumoto, Y.; Kobayashi, Y.; Takemura, S.; Maeda, K.; Nakamura, F.; Inatomi, O.; Andoh, A.; Ban, H. A Case of Appendix Adenocarcinoma Associated with Ulcerative Colitis. Clin. Case Rep. 2021, 9, e04768. [Google Scholar] [CrossRef] [PubMed]
- Klag, T.; Wehkamp, J.; Bösmüller, H.; Falch, C.; Johannink, J.; Malek, N.P.; Kirschniak, A.; Goetz, M. Low-Grade Appendiceal Mucinous Neoplasm (LAMN)—3-Year Endoscopic Follow-up Underlines Benign Course of LAMN Type 1. Z. Gastroenterol. 2017, 55, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Fakheri, H.; Bari, Z.; Yaghoobi, M.; Rabiee, P. Concomitant Occurrence of Appendiceal Mucocele and Ulcerative Colitis: Case Reports. Caspian J. Intern. Med. 2023, 14, 391–395. [Google Scholar] [CrossRef]
| Author | Year of Publication | Years of Enrollment | Type of Study | No. of Surgically Treated Patients | Age | Male/Female | Etiology | Associated Disease Activity | Description of Disease Activity |
|---|---|---|---|---|---|---|---|---|---|
| Moniakis | 2021 | Case report | 1 | 65 | F | CD | Yes | Remission | |
| Davey | 2020 | Case report | 1 | 42 | M | UC | Yes | Proctitis | |
| Ghosh | 2010 | Case report | 1 | 55 | F | UC | NR | NR | |
| Lakatos | 2005 | Case report | 1 | 60 | M | UC | Yes | Proctosigmoiditis | |
| Lyda | 1998 | Case report | 1 | 48 | M | UC | NR | NR | |
| Nehme | 2019 | Case report | 1 | 42 | M | UC | Yes | Pancolitis | |
| Noaki | 2009 | Case report | 1 | 33 | F | UC | No | Proctosigmoiditis | |
| Orta | 2009 | 2002–2006 | Retrospective | 9 | 46.2 (mean) | 6M/3F | 6 UC 3 CD | NR | 4 pancolitis (UC); 2 left colitis (UC); 3 ileocolic (CD) |
| Kuester | 2008 | Case report | 1 | 36 | M | UC | Yes | Pancolitis | |
| Shen | 2014 | Case report | 1 | 68 | M | UC | No | Remission | |
| Sonwalkar | 2002 | Case report | 1 | 68 | F | CD | Yes | Caecum | |
| Takeda | 2008 | Case report | 1 | 42 | M | UC | No | NR | |
| Tonolini | 2015 | Case report | 1 | 71 | M | UC | Yes | Pancolitis | |
| Villanueva Saenz | 2006 | Case report | 1 | 60 | F | UC | Yes | Left colitis | |
| Vukovic | 2018 | Case report | 1 | 22 | M | CD | Yes | Ileocolic | |
| Zannoni | 1997 | Case report | 1 | 69 | F | UC | No | Remission | |
| Wong | 2012 | Case report | 2 | 48 (mean) | 2F | 2 UC | No/Yes | Remission/Pancolitis | |
| Simsek | 2019 | Case report | 1 | 22 | F | CD | Yes | Ileocolic | |
| Abdulghaffar | 2022 | Case report | 1 | 48 | F | UC | Yes | Proctosigmoiditis | |
| Almogy | 2001 | Case report | 1 | 38 | M | CD | Yes | Ileocolic | |
| Fukumoto | 2021 | Case report | 1 | 52 | M | UC | Yes | Left colitis | |
| Klag | 2016 | Case report | 1 | 63 | M | UC | Yes | Remission | |
| Fakheri | 2023 | Case report | 3 | 55.7 (mean) | 2F; 1M | 3 UC | Yes | 2 pancolitis; 1 left colitis |
| Author | Publication Year | Surgical Approach | Timing | Surgical Procedure | Reason for Extended Resection (Other than Appendectomy) | Histologic Report | Pathological Stage + Extra-Appendiceal Mucin | Synchronous Colon Dysplasia/Carcinoma |
|---|---|---|---|---|---|---|---|---|
| Moniakis | 2021 | Laparotomy | Urgent | right hemicolectomy | NR | LAMN | No mucin | 0 |
| Davey | 2020 | Open | Urgent | right hemicolectomy | no clear margin | LAMN | TisN0, no mucin | 0 |
| Ghosh | 2010 | Laparoscopic | Elective | right hemicolectomy | no clear margin | LAMN | No mucin | 0 |
| Lakatos | 2005 | Open | Elective | cecal resection | no clear margin | LAMN | No mucin | 0 |
| Lyda | 1998 | Open | Elective | proctocolectomy | dysplasia in UC | LAMN | No mucin | 1 |
| Nehme | 2019 | NR | Urgent | proctocolectomy with ileostomy | dysplasia in UC | Mucinous adenocarcinoma | TNM NR, no mucin | 1 |
| Noaki | 2009 | Open | Elective | cecal resection | no clear margin | LAMN | No mucin | 1 |
| Orta | 2009 | NR | NR | colectomy | NR | LAMN | NR | 4 UC |
| Kuester | 2008 | NR | Elective | proctocolectomy with ileostomy | dysplasia in UC | LAMN | No mucin | 1 |
| Shen | 2014 | Laparoscopic | Urgent | right hemicolectomy | no clear margin | Mucinous adenocarcinoma | T2, N not reported No mucin | 0 |
| Sonwalkar | 2002 | Open | Elective | right hemicolectomy | colon cancer (caecum) | Mucinous adenocarcinoma | T4N1M0, no mucin | 1 |
| Takeda | 2008 | NR | Urgent | appendectomy | appendectomy | Mucinous adenocarcinoma | TNM NR, no mucin | 0 |
| Tonolini | 2015 | Laparoscopic | Elective | appendectomy | appendectomy | LAMN | No mucin | 0 |
| Villanueva Saenz | 2006 | NR | Elective | proctocolectomy with ileostomy | severe pancolitis | Mucinous adenocarcinoma | TNM NR, no mucin | 0 |
| Vukovic | 2018 | NR | Urgent | right hemicolectomy | IBD relapse | Mucinous adenocarcinoma + signet ring cells | TNM NR, no mucin | 0 |
| Zannoni | 1997 | Open | Elective | right hemicolectomy | no clear margin | Mucinous adenocarcinoma | TNM NR, no mucin | 0 |
| Wong | 2012 | Laparoscopic | Elective | appendectomy | appendectomy | LAMN | No mucin | 0 |
| Simsek | 2019 | Open | Elective | ileocecal resection | IBD relapse | LAMN | PMP, TNM NR | 0 |
| Abdulghaffar | 2022 | Open | Elective | appendectomy | appendectomy | LAMN | No mucin | 0 |
| Almogy | 2001 | Open | Urgent | subtotal colectomy | colon perforation | Mucinous adenocarcinoma | TNM NR, no mucin | 0 |
| Fukumoto | 2021 | Laparoscopic | Urgent | right hemicolectomy | suspected cancer of right colon | Mucinous adenocarcinoma | T4bN1aM0, no mucin | 0 |
| Klag | 2016 | Laparoscopic | Elective | cecal resection | no clear margin | LAMN | No mucin | 0 |
| Fakheri | 2023 | NR | Elective | 2 right hemicolectomies + appendectomy | no clear margin | 3 LAMN | No mucin | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonomi, A.M.; Ferrario, L.; Frontali, A.; Danelli, P.; Colombo, F. Appendiceal Mucinous Neoplasms and Inflammatory Bowel Disease: Systematic Review of the Literature. J. Clin. Med. 2024, 13, 191. https://doi.org/10.3390/jcm13010191
Bonomi AM, Ferrario L, Frontali A, Danelli P, Colombo F. Appendiceal Mucinous Neoplasms and Inflammatory Bowel Disease: Systematic Review of the Literature. Journal of Clinical Medicine. 2024; 13(1):191. https://doi.org/10.3390/jcm13010191
Chicago/Turabian StyleBonomi, Alessandro Michele, Luca Ferrario, Alice Frontali, Piergiorgio Danelli, and Francesco Colombo. 2024. "Appendiceal Mucinous Neoplasms and Inflammatory Bowel Disease: Systematic Review of the Literature" Journal of Clinical Medicine 13, no. 1: 191. https://doi.org/10.3390/jcm13010191
APA StyleBonomi, A. M., Ferrario, L., Frontali, A., Danelli, P., & Colombo, F. (2024). Appendiceal Mucinous Neoplasms and Inflammatory Bowel Disease: Systematic Review of the Literature. Journal of Clinical Medicine, 13(1), 191. https://doi.org/10.3390/jcm13010191







