The Two Substrate Reduction Therapies for Type 1 Gaucher Disease Are Not Equivalent. Comment on Hughes et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hughes, D.A.; Deegan, P.; Giraldo, P.; Göker-Alpan, Ö.; Lau, H.; Lukina, E.; Revel-Vilk, S.; Scarpa, M.; Botha, J.; Gadir, N.; et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158. [Google Scholar] [CrossRef] [PubMed]
- Peterschmitt, M.J.; Cox, G.F.; Ibrahim, J.; MacDougall, J.; Underhill, L.H.; Patel, P.; Gaemers, S.J.M. A pooled analysis of adverse events in 393 adults with Gaucher disease type 1 from four clinical trials of oral eliglustat: Evaluation of frequency, timing, and duration. Blood Cells Mol. Dis. 2018, 68, 185–191. [Google Scholar] [CrossRef] [PubMed]
- CERDELGA™ (Eliglustat) [Package Insert]; Genzyme Ireland, Ltd.: Waterford, Ireland, 2018; Available online: http://www.cerdelga.com/pdf/cerdelga_prescribing_information.pdf (accessed on 27 October 2022).
- CERDELGA™ 84 mg Capsules. In Summary of Product Characteristics; Genzyme Therapeutics: Oxfordshire, UK; Available online: https://www.medicines.org.uk/emc/product/2615/smpc2018 (accessed on 27 October 2022).
- Zavesca (Miglustat) US Prescribing Information; Actelion Pharmaceuticals US, Inc: South San Francisco, CA, USA, 2017; Available online: https://www.zavesca.com/pdf/ZAVESCA-Full-Prescribing-Information.pdf (accessed on 27 October 2022).
- Zavesca (Miglustat) Summary of Product Characteristics; Janssen Pharmaceutica NV: Beerse, Belgium, 2012.
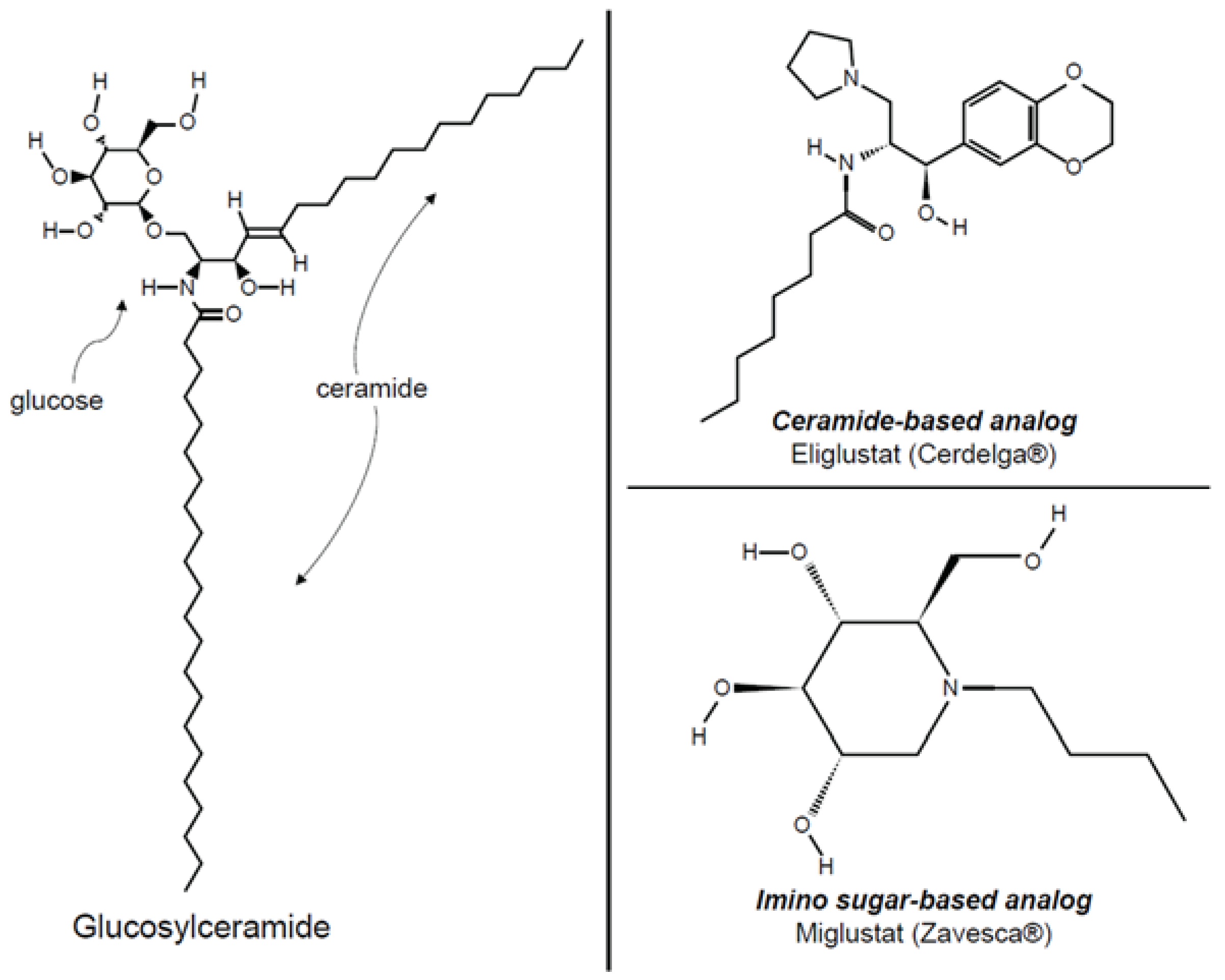
- Shayman, J.A. Eliglustat tartrate: Glucosylceramide synthase inhibitor treatment of type 1 Gaucher disease. Drugs Future 2010, 35, 613–620. [Google Scholar] [CrossRef] [PubMed]
- McEachern, K.A.; Fung, J.; Komarnitsky, S.; Siegel, C.; Chuang, W.L.; Hutto, E.; Shayman, J.A.; Grabowski, G.A.; Aerts, J.M.; Cheng, S.H.; et al. A specific and potent inhibitor of glucosylceramide synthase for substrate inhibition therapy of Gaucher disease. Mol. Genet. Metab. 2007, 91, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Wennekes, T.; Meijer, A.J.; Groen, A.K.; Boot, R.G.; Groener, J.E.; van Eijk, M.; Ottenhoff, R.; Bijl, N.; Ghauharali, K.; Song, H.; et al. Dual-action lipophilic iminosugar improves glycemic control in obese rodents by reduction of visceral glycosphingolipids and buffering of carbohydrate assimilation. J. Med. Chem. 2010, 53, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Belmatoug, N.; Burlina, A.; Giraldo, P.; Hendriksz, C.J.; Kuter, D.J.; Mengel, E.; Pastores, G.M. Gastrointestinal disturbances and their management in miglustat-treated patients. J. Inherit. Metab. Dis. 2011, 34, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Champion, H.; Ramaswami, U.; Imrie, J.; Lachmann, R.H.; Gallagher, J.; Cox, T.M.; Wraith, J.E. Dietary modifications in patients receiving miglustat. J. Inherit. Metab. Dis. 2010, 33, S379–S383. [Google Scholar] [CrossRef] [PubMed]
- Peterschmitt, M.J.; Freisens, S.; Underhill, L.H.; Foster, M.C.; Lewis, G.; Gaemers, S.J.M. Long-term adverse event profile from four completed trials of oral eliglustat in adults with Gaucher disease type 1. Orphanet J. Rare Dis. 2019, 14, 128. [Google Scholar] [CrossRef] [PubMed]
- Schiffmann, R.; Fitzgibbon, E.J.; Harris, C.; DeVile, C.; Davies, E.H.; Abel, L.; van Schaik, I.N.; Benko, W.; Timmons, M.; Ries, M.; et al. Randomized, controlled trial of miglustat in Gaucher’s disease type 3. Ann. Neurol. 2008, 64, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Ruskin, J.N.; Ortemann-Renon, C.; Msihid, J.; Ross, L.; Puga, A.C.; Peterschmitt, M.J.; Cox, G.F.; Maison-Blanche, P. How a concentration-effect analysis of data from the eliglustat thorough electrocardiographic study was used to support dosing recommendations. Mol. Genet. Metab. 2020, 131, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Granovsky-Grisaru, S.; Belmatoug, N.; vom Dahl, S.; Mengel, E.; Morris, E.; Zimran, A. The management of pregnancy in Gaucher disease. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 156, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Mistry, P.K.; Balwani, M.; Baris, H.N.; Turkia, H.B.; Burrow, T.A.; Charrow, J.; Cox, G.F.; Danda, S.; Dragosky, M.; Drelichman, G.; et al. Safety, efficacy, and authorization of eliglustat as a first-line therapy in Gaucher disease type 1. Blood Cells Mol. Dis. 2018, 71, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Cox, T.; Lachmann, R.; Hollak, C.; Aerts, J.; van Weely, S.; Hrebicek, M.; Platt, F.; Butters, T.; Dwek, R.; Moyses, C.; et al. Novel oral treatment of Gaucher’s disease with N-butyldeoxynojirimycin (OGT 918) to decrease substrate biosynthesis. Lancet 2000, 355, 1481–1485. [Google Scholar] [CrossRef]
- Cox, T.M.; Drelichman, G.; Cravo, R.; Balwani, M.; Burrow, T.A.; Martins, A.M.; Lukina, E.; Rosenbloom, B.; Ross, L.; Angell, J.; et al. Eliglustat compared with imiglucerase in patients with Gaucher’s disease type 1 stabilised on enzyme replacement therapy: A phase 3, randomised, open-label, non-inferiority trial. Lancet 2015, 385, 2355–2362. [Google Scholar] [CrossRef]
- Cox, T.M.; Amato, D.; Hollak, C.E.; Luzy, C.; Silkey, M.; Giorgino, R.; Steiner, R.D. Evaluation of miglustat as maintenance therapy after enzyme therapy in adults with stable type 1 Gaucher disease: A prospective, open-label non-inferiority study. Orphanet J. Rare Dis. 2012, 7, 102. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mistry, P.K.; Kishnani, P.S.; Balwani, M.; Charrow, J.M.; Hull, J.; Weinreb, N.J.; Cox, T.M. The Two Substrate Reduction Therapies for Type 1 Gaucher Disease Are Not Equivalent. Comment on Hughes et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158. J. Clin. Med. 2023, 12, 3269. https://doi.org/10.3390/jcm12093269
Mistry PK, Kishnani PS, Balwani M, Charrow JM, Hull J, Weinreb NJ, Cox TM. The Two Substrate Reduction Therapies for Type 1 Gaucher Disease Are Not Equivalent. Comment on Hughes et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158. Journal of Clinical Medicine. 2023; 12(9):3269. https://doi.org/10.3390/jcm12093269
Chicago/Turabian StyleMistry, Pramod K., Priya S. Kishnani, Manisha Balwani, Joel M. Charrow, Judy Hull, Neal J. Weinreb, and Timothy M. Cox. 2023. "The Two Substrate Reduction Therapies for Type 1 Gaucher Disease Are Not Equivalent. Comment on Hughes et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158" Journal of Clinical Medicine 12, no. 9: 3269. https://doi.org/10.3390/jcm12093269
APA StyleMistry, P. K., Kishnani, P. S., Balwani, M., Charrow, J. M., Hull, J., Weinreb, N. J., & Cox, T. M. (2023). The Two Substrate Reduction Therapies for Type 1 Gaucher Disease Are Not Equivalent. Comment on Hughes et al. Switching between Enzyme Replacement Therapies and Substrate Reduction Therapies in Patients with Gaucher Disease: Data from the Gaucher Outcome Survey (GOS). J. Clin. Med. 2022, 11, 5158. Journal of Clinical Medicine, 12(9), 3269. https://doi.org/10.3390/jcm12093269




