Anatomical Analysis of the Gonadal Veins and Spine in Lateral Lumbar Interbody Fusion
Abstract
1. Introduction
2. Materials and Methods
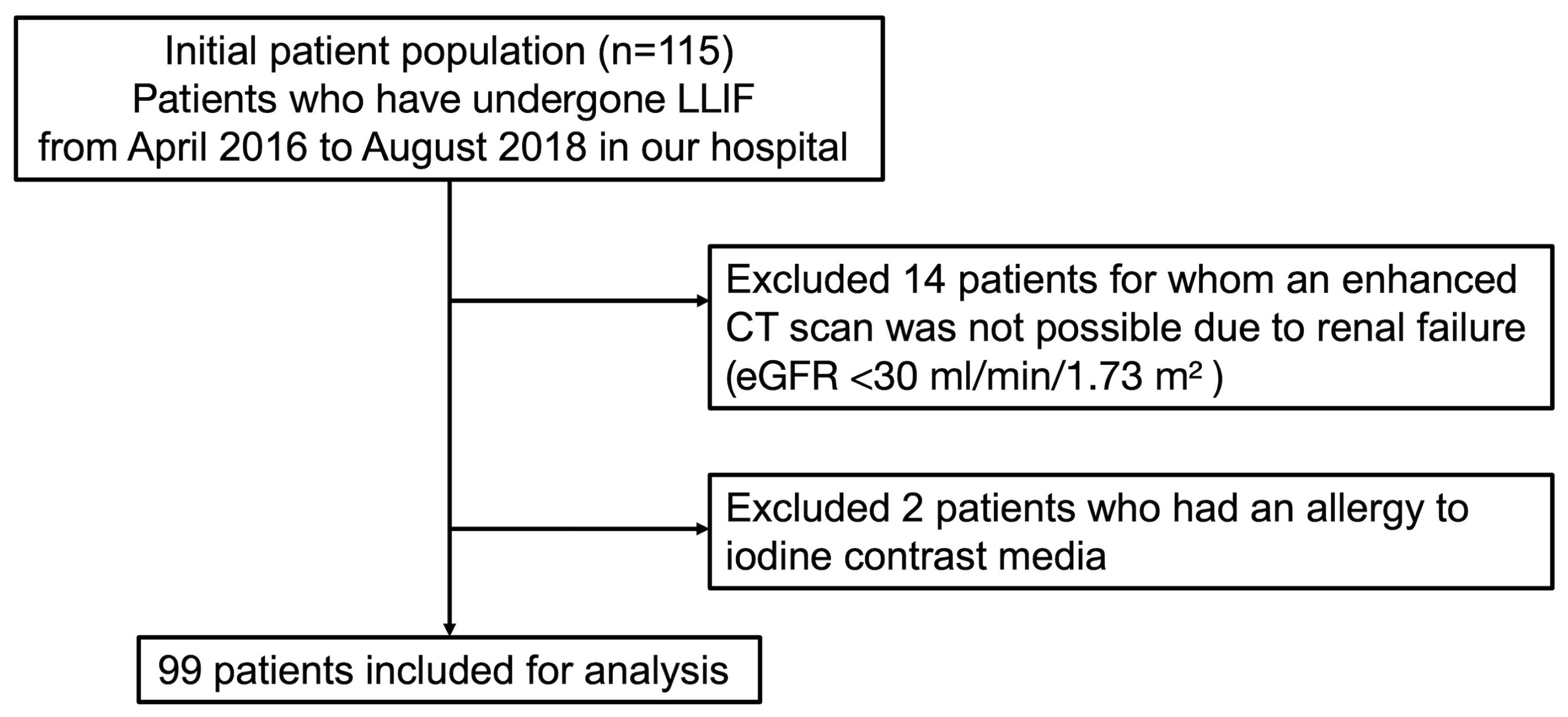
2.1. Study Design and Setting
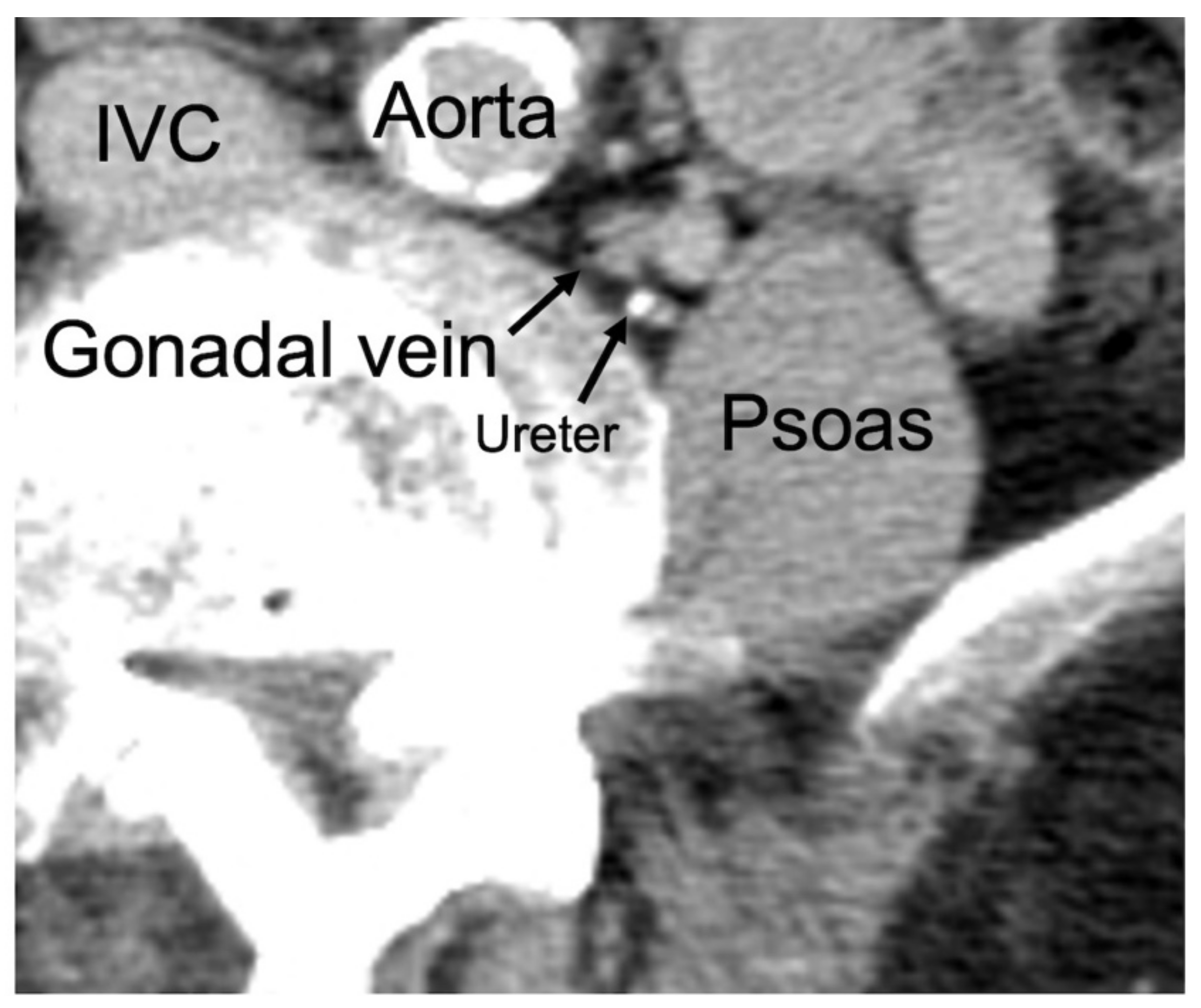
2.2. Classification of GV Location
2.3. Patients with GV in the DM Region
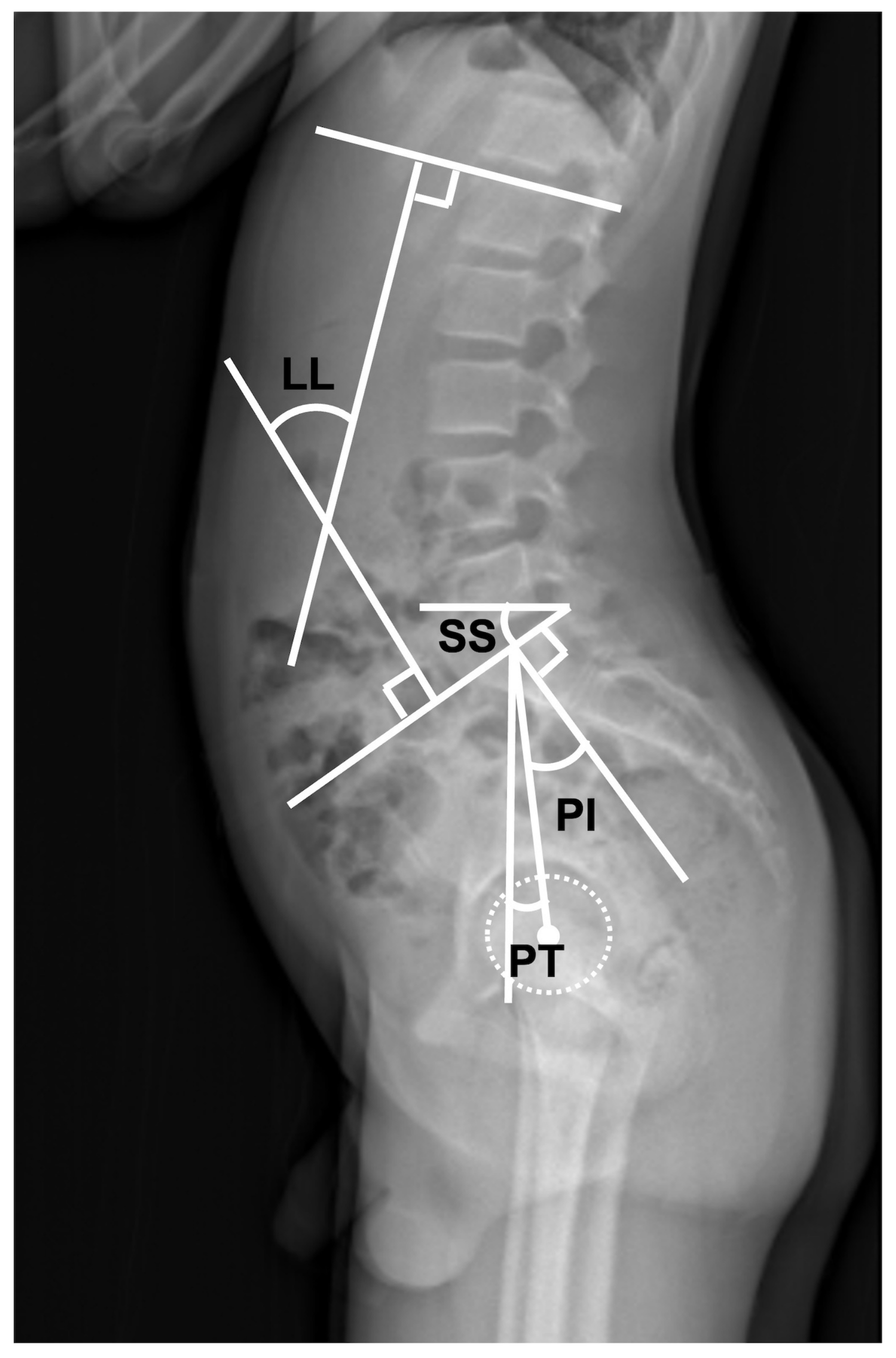
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Patients
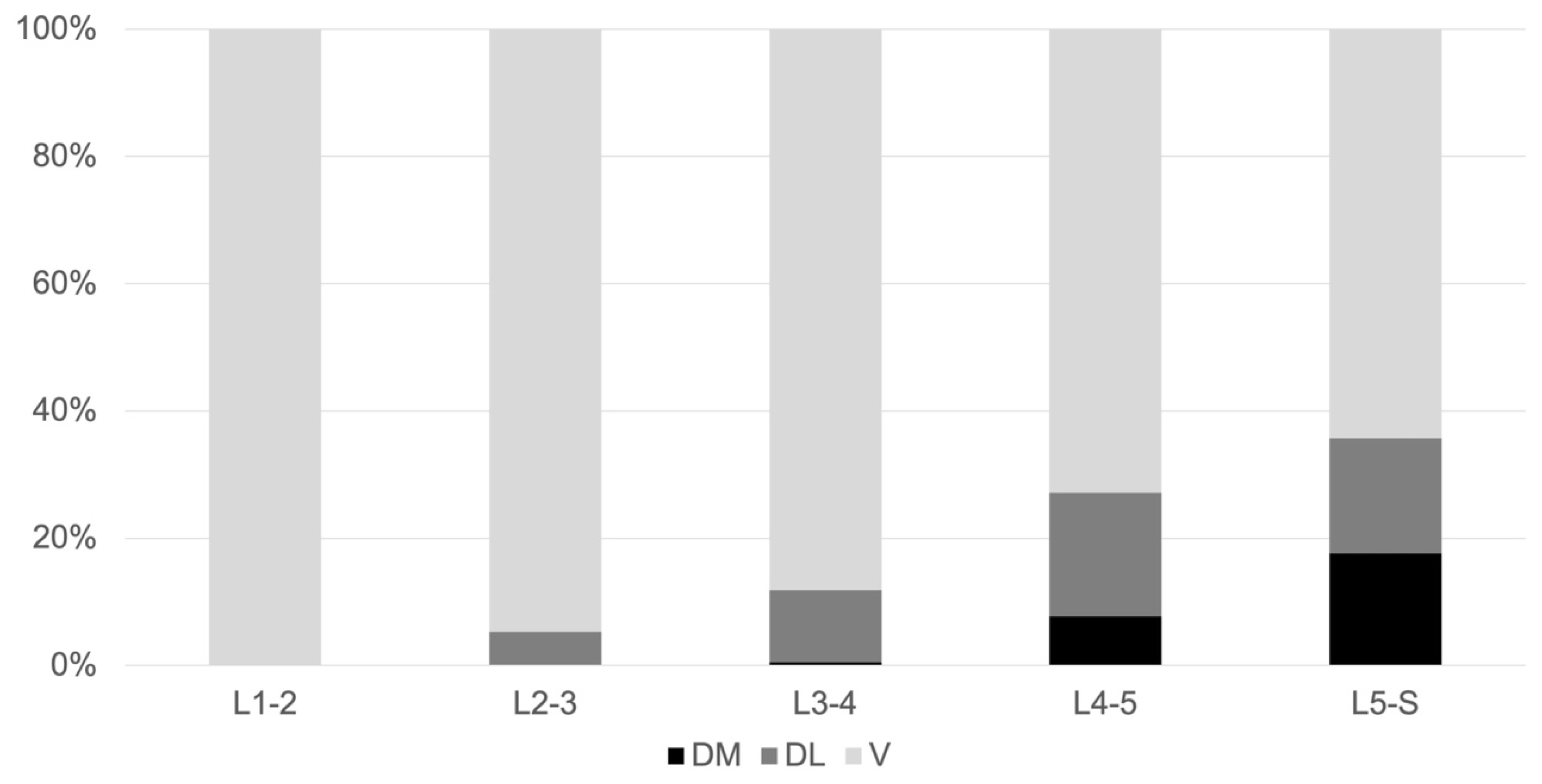
3.2. GV Location at the Lumbar Disc Level
3.3. Differences in the Right and Side and in Terms of Sex
3.4. Comparison between Group M and Group O
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moller, D.J.; Slimack, N.P.; Acosta, F.L., Jr.; Koski, T.R.; Fessler, R.G.; Liu, J.C. Minimally invasive lateral lumbar interbody fusion and transpsoas approach–related morbidity. Neurosurg. Focus 2011, 31, E4. [Google Scholar] [CrossRef]
- Ozgur, B.M.; Aryan, H.E.; Pimenta, L.; Taylor, W.R. Extreme Lateral Interbody Fusion (XLIF): A novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006, 6, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.B.; Marchi, L.M.; Coutinho, E.; Pimenta, L. A Radiographic Assessment of the Ability of the Extreme Lateral Interbody Fusion Procedure to Indirectly Decompress the Neural Elements. Spine 2010, 35 (Suppl. S26), S331–S337. [Google Scholar] [CrossRef]
- Rodgers, W.B.; Gerber, E.J.P.-C.; Patterson, J.B. Intraoperative and Early Postoperative Complications in Extreme Lateral Interbody Fusion: An analysis of 600 cases. Spine 2011, 36, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Allain, J.; Dufour, T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop. Traumatol. Surg. Res. 2019, 106, S149–S157. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 2015, 1, 2–18. [Google Scholar]
- Isaacs, R.E.; Sembrano, J.N.; Tohmeh, A.G.; SOLAS Degenerative Study Group. Two-Year Comparative Outcomes of MIS Lateral and MIS Transforaminal Interbody Fusion in the Treatment of Degenerative Spondylolisthesis. Part II: Radiographic findings. Spine 2016, 41 (Suppl. S8), S133–S144. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.H.; Samartzis, D.; Khanna, A.J.; Anderson, D.G. Minimally Invasive Techniques for Lumbar Interbody Fusions. Orthop. Clin. N. Am. 2007, 38, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, A.O.; Soliman, M.A.R.; Azmy, S.; Khan, A.; Jowdy, P.K.; Mullin, J.P.; Pollina, J. Incidence of major and minor vascular injuries during lateral access lumbar interbody fusion procedures: A retrospective comparative study and systematic literature review. Neurosurg. Rev. 2021, 45, 1275–1289. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.-Y.; Xu, Z.-W.; He, D.-W.; Zhao, X.; Ma, W.-H.; Ni, W.-F.; Song, Y.-X.; Zhang, J.-Q.; Yu, W.; Fang, X.-Q.; et al. Complications and Prevention Strategies of Oblique Lateral Interbody Fusion Technique. Orthop. Surg. 2018, 10, 98–106. [Google Scholar] [CrossRef]
- Kagami, Y.; Nakashima, H.; Satake, K.; Ito, K.; Tanaka, S.; Segi, N.; Ouchida, J.; Morita, M.; Ando, K.; Kobayashi, K.; et al. Assessment of Ureters at Dangerous Locations in Lateral Lumbar Interbody Fusion. Spine Surg. Relat. Res. 2022, 6, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Regev, G.J.; Chen, L.; Dhawan, M.; Lee, Y.P.; Garfin, S.R.; Kim, C.W. Morphometric Analysis of the Ventral Nerve Roots and Retroperitoneal Vessels with Respect to the Minimally Invasive Lateral Approach in Normal and Deformed Spines. Spine 2009, 34, 1330–1335. [Google Scholar] [CrossRef]
- Deschênes, S.; Charron, G.; Beaudoin, G.; Labelle, H.; Dubois, J.; Miron, M.-C.; Parent, S. Diagnostic Imaging of Spinal Deformities: Reducing patients radiation dose with a new slot-scanning X-ray imager. Spine 2010, 35, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Whittle, M.; Evans, M. Instrument for measuring the cobb angle in scoliosis. Lancet 1979, 313, 414. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Karaosmanoglu, D.; Karcaaltincaba, M.; Karcaaltincaba, D.; Akata, D.; Ozmen, M. MDCT of the Ovarian Vein: Normal Anatomy and Pathology. Am. J. Roentgenol. 2009, 192, 295–299. [Google Scholar] [CrossRef]
- Szpinda, M.; Elminowska-Wenda, G.; Wiśniewski, M.; Frąckiewicz, P. Morphometric analysis of the gonadal veins in human foetuses. Ann. Anat. 2005, 187, 399–403. [Google Scholar] [CrossRef]
- Pai, M.; Vadgaonkar, R.; Rai, R.; Nayak, S.R.; Jiji, P.J.; Ranade, A.; Prabhu, L.; Madhyastha, S. A cadaveric study of the testicular artery in the South Indian population. Singap. Med. J. 2008, 49, 551–555. [Google Scholar]
- Barber, B.; Horton, A.; Patel, U. Anatomy of the Origin of the Gonadal Veins on CT. J. Vasc. Interv. Radiol. 2012, 23, 211–215. [Google Scholar] [CrossRef]
- Makanji, H.S.; Le, H.; Wood, K.B.; Jenis, L.G.; Cha, T.D. Morphometric Analysis of the Retroperitoneal Vessels with Respect to Lateral Access Surgery in Adult Scoliosis. Clin. Spine Surg. 2017, 30, E1010–E1014. [Google Scholar] [CrossRef]
- Hsu, C.-W.; Chang, M.-C.; Wang, J.-H.; Wu, C.-C.; Chen, Y.-H. Incidence and Clinical Outcomes of Gonadal Artery Injury during Colorectal Surgery in Male Patients. J. Gastrointest. Surg. 2019, 23, 2075–2080. [Google Scholar] [CrossRef] [PubMed]
- Pastuszak, A.W.; Wang, R. Varicocele and testicular function. Asian J. Androl. 2015, 17, 659. [Google Scholar] [CrossRef] [PubMed]
- Joh, M.; Grewal, S.; Gupta, R. Ovarian Vein Embolization: How and When Should It Be Done? Tech. Vasc. Interv. Radiol. 2021, 24, 100732. [Google Scholar] [CrossRef] [PubMed]
- Ouchida, J.; Kanemura, T.; Satake, K.; Nakashima, H.; Segi, N. Anatomic evaluation of retroperitoneal organs for lateral approach surgery: A prospective imaging study using computed tomography in the lateral decubitus position. Eur. Spine J. 2019, 28, 835–841. [Google Scholar] [CrossRef] [PubMed]

| L1–L2 Levels (%) | L2–L3 Levels (%) | L3–L4 Levels (%) | L4–L5 Levels (%) | L5–S Levels (%) | |
|---|---|---|---|---|---|
| V | 31 (100) | 160 (94.6) | 172 (88.2) | 133 (72.9) | 124 (64.3) |
| DM | 0 | 0 | 1 (0.5) | 15 (7.7) | 34 (17.6) |
| DL | 0 | 9 (5.3) | 22 (11.3) | 38 (19.5) | 35 (18.1) |
| Left Side (%) | Right Side (%) | p Value | |
|---|---|---|---|
| L1–L2 level | 1.0 | ||
| V | 21 (100) | 10 (100) | |
| DM | 0 | 0 | |
| DL | 0 | 0 | |
| L2–L3 level | 0.54 | ||
| V | 83 (93.3) | 77 (96.2) | |
| DM | 0 | 0 | |
| DL | 6 (6.7) | 3 (3.8) | |
| L3–L4 level | <0.01 | ||
| V | 80 (82.4) | 92 (93.9) | |
| DM | 0 | 1 (1.0) | |
| DL | 17 (17.5) | 5 (5.1) | |
| L4–L5 level | 0.07 | ||
| V | 66 (67.3) | 76 (78.3) | |
| DM | 7 (7.1) | 8 (8.2) | |
| DL | 25 (25.5) | 13 (13.4) | |
| L5–S level | 0.12 | ||
| V | 56 (57.2) | 68 (71.6) | |
| DM | 20 (20.4) | 14 (14.7) | |
| DL | 22 (22.4) | 13 (13.7) |
| Men (%) | Women (%) | p Value | |
|---|---|---|---|
| L3–L4 level | 0 | 1 (0.7) | <0.01 |
| L4–L5 level | 0 | 15 (7.7) | <0.01 |
| L5–S level | 1 (0.5) | 33 (17.1) | <0.01 |
| Group M n = 27 | Group O n = 72 | p Value | |
|---|---|---|---|
| Age, years, mean (SD) | 70.3 (6.2) | 70.4 (9.2) | 0.95 |
| Sex, male/female, n | 1/26 | 37/35 | <0.01 * |
| BMI, kg/m2, mean (SD) | 22.9 (3.8) | 24.3(3.5) | 0.06 |
| Cobb angle (°) (SD) | 16.0 (16.4) | 5.1 (11.3) | <0.01 * |
| LL (L1–S1 level) (°) (SD) | 22.0 (18.4) | 29.7 (14.6) | 0.03 * |
| PI (°) (SD) | 51.5 (10.5) | 46.6 (9.6) | 0.03 * |
| PI–LL (°) (SD) | 29.5 (18.6) | 16.2 (15.5) | <0.01 * |
| PT (°) (SD) | 30.6 (9.3) | 21.2 (9.1) | <0.01 * |
| SS (°) (SD) | 20.9 (11.0) | 25.2 (9.4) | 0.06 |
| Disease, n (%) | <0.01 * | ||
| Degenerative scoliosis | 20 (74.1) | 21 (29.2) | |
| Degenerative spondylolisthesis | 5 (18.5) | 34 (47.2) | |
| Fracture | 2 (7.4) | 13 (18.1) | |
| Others | 0 | 4 (5.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kagami, Y.; Nakashima, H.; Satake, K.; Ito, K.; Tsushima, M.; Segi, N.; Tomita, H.; Ouchida, J.; Morita, Y.; Ode, Y.; et al. Anatomical Analysis of the Gonadal Veins and Spine in Lateral Lumbar Interbody Fusion. J. Clin. Med. 2023, 12, 3041. https://doi.org/10.3390/jcm12083041
Kagami Y, Nakashima H, Satake K, Ito K, Tsushima M, Segi N, Tomita H, Ouchida J, Morita Y, Ode Y, et al. Anatomical Analysis of the Gonadal Veins and Spine in Lateral Lumbar Interbody Fusion. Journal of Clinical Medicine. 2023; 12(8):3041. https://doi.org/10.3390/jcm12083041
Chicago/Turabian StyleKagami, Yujiro, Hiroaki Nakashima, Kotaro Satake, Kenyu Ito, Mikito Tsushima, Naoki Segi, Hiroyuki Tomita, Jun Ouchida, Yoshinori Morita, Yukihito Ode, and et al. 2023. "Anatomical Analysis of the Gonadal Veins and Spine in Lateral Lumbar Interbody Fusion" Journal of Clinical Medicine 12, no. 8: 3041. https://doi.org/10.3390/jcm12083041
APA StyleKagami, Y., Nakashima, H., Satake, K., Ito, K., Tsushima, M., Segi, N., Tomita, H., Ouchida, J., Morita, Y., Ode, Y., Imagama, S., & Kanemura, T. (2023). Anatomical Analysis of the Gonadal Veins and Spine in Lateral Lumbar Interbody Fusion. Journal of Clinical Medicine, 12(8), 3041. https://doi.org/10.3390/jcm12083041







