Anxiety and Depressive Symptoms Correlated to Patient-Reported Outcome Measures after Rotator Cuff Repair: A Prospective Study in the Perioperative Period
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lau, B.C.; Scribani, M.; Wittstein, J. The Effect of Preexisting and Shoulder-Specific Depression and Anxiety on Patient-Reported Outcomes After Arthroscopic Rotator Cuff Repair. Am. J. Sports Med. 2019, 47, 3073–3079. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.H.; Song, K.S.; Hwang, I.; Warner, J.J. Does Rotator Cuff Repair Improve Psychologic Status and Quality of Life in Patients with Rotator Cuff Tear? Clin. Orthop. Relat. Res. 2015, 473, 3494–3500. [Google Scholar] [CrossRef] [PubMed]
- Lau, B.C.; Scribani, M.; Wittstein, J. Patients with depression and anxiety symptoms from adjustment disorder related to their shoulder may be ideal patients for arthroscopic rotator cuff repair. J. Shoulder Elb. Surg. 2020, 29, S80–S86. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Gougoulias, N.; Caine, D.; Denaro, V. Sport injuries: A review of outcomes. Br. Med. Bull. 2011, 97, 47–80. [Google Scholar] [CrossRef] [PubMed]
- Cronin, K.J.; Mair, S.D.; Hawk, G.S.; Thompson, K.L.; Hettrich, C.M.; Jacobs, C.A. Increased Health Care Costs and Opioid Use in Patients with Anxiety and Depression Undergoing Rotator Cuff Repair. Arthroscopy 2020, 36, 2655–2660. [Google Scholar] [CrossRef] [PubMed]
- Panattoni, N.; Longo, U.G.; De Salvatore, S.; Castaneda, N.S.C.; Ambrogioni, L.R.; Piredda, M.; De Marinis, M.G.; Denaro, V. The influence of psychosocial factors on patient-reported outcome measures in rotator cuff tears pre- and post-surgery: A systematic review. Qual. Life Res. 2022, 31, 91–116. [Google Scholar] [CrossRef]
- Johnson, A.H.; York, J.J.; Lashgari, C.J.; Petre, B.M.; Turcotte, J.J.; Redziniak, D.E. Effects of preexisting depression and anxiety on postoperative outcomes following arthroscopic rotator cuff repair. JSES Int. 2022, 6, 984–988. [Google Scholar] [CrossRef]
- Longo, U.G.; Risi Ambrogioni, L.; Candela, V.; Berton, A.; Carnevale, A.; Schena, E.; Denaro, V. Conservative versus surgical management for patients with rotator cuff tears: A systematic review and META-analysis. BMC Musculoskelet. Disord. 2021, 22, 50. [Google Scholar]
- Chung, S.W.; Park, J.S.; Kim, S.H.; Shin, S.H.; Oh, J.H. Quality of life after arthroscopic rotator cuff repair: Evaluation using SF-36 and an analysis of affecting clinical factors. Am. J. Sport. Med. 2012, 40, 631–639. [Google Scholar] [CrossRef]
- Teunis, T.; Lubberts, B.; Reilly, B.T.; Ring, D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J. Shoulder Elb. Surg. 2014, 23, 1913–1921. [Google Scholar] [CrossRef]
- Razmjou, H.; Bean, A.; MacDermid, J.C.; Van Osnabrugge, V.; Travers, N.; Holtby, R. Convergent Validity of the Constant-Murley Outcome Measure in Patients with Rotator Cuff Disease. Physiother. Can. 2008, 60, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Salvatore, G.; Rizzello, G.; Berton, A.; Ciuffreda, M.; Candela, V.; Denaro, V. The burden of rotator cuff surgery in Italy: A nationwide registry study. Arch. Orthop. Trauma Surg. 2017, 137, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Berton, A.; De Salvatore, S.; Candela, V.; Cortina, G.; Presti, D.L.; Massaroni, C.; Petrillo, S.; Denaro, V. Delayed Rehabilitation Protocol after Rotator Cuff Repair. Osteology 2021, 1, 29–38. [Google Scholar] [CrossRef]
- Coronado, R.A.; Seitz, A.L.; Pelote, E.; Archer, K.R.; Jain, N.B. Are Psychosocial Factors Associated with Patient-reported Outcome Measures in Patients with Rotator Cuff Tears? A Systematic Review. Clin. Orthop. Relat. Res. 2018, 476, 810–829. [Google Scholar] [CrossRef]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B.; New England Medical Center Hospital. SF-36 Health Survey: Manual and Interpretation Guide; Health Institute New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- Sahoo, S.; Ricchetti, E.T.; Zajichek, A.; Evans, P.J.; Farrow, L.D.; McCoy, B.W.; Jones, M.H.; Miniaci, A.A.; Sabesan, V.J.; Schickendantz, M.S.; et al. Associations of Preoperative Patient Mental Health and Sociodemographic and Clinical Characteristics with Baseline Pain, Function, and Satisfaction in Patients Undergoing Rotator Cuff Repairs. Am. J. Sports Med. 2020, 48, 432–443. [Google Scholar] [CrossRef]
- Thorpe, A.M.; O’Sullivan, P.B.; Mitchell, T.; Hurworth, M.; Spencer, J.; Booth, G.; Goebel, S.; Khoo, P.; Tay, A.; Smith, A. Are Psychologic Factors Associated with Shoulder Scores After Rotator Cuff Surgery? Clin. Orthop. Relat. Res. 2018, 476, 2062–2073. [Google Scholar] [CrossRef]
- Rosenberger, P.H.; Jokl, P.; Ickovics, J. Psychosocial factors and surgical outcomes: An evidence-based literature review. J. Am. Acad. Orthop. Surg. 2006, 14, 397–405. [Google Scholar] [CrossRef]
- Ravindra, A.; Barlow, J.D.; Jones, G.L.; Bishop, J.Y. A prospective evaluation of predictors of pain after arthroscopic rotator cuff repair: Psychosocial factors have a stronger association than structural factors. J. Shoulder Elb. Surg. 2018, 27, 1824–1829. [Google Scholar] [CrossRef]
- Lädermann, A.; Burkhart, S.S.; Hoffmeyer, P.; Neyton, L.; Collin, P.; Yates, E.; Denard, P.J. Classification of full-thickness rotator cuff lesions: A review. EFORT Open Rev. 2016, 1, 420–430. [Google Scholar] [CrossRef]
- Churruca, K.; Pomare, C.; Ellis, L.A.; Long, J.C.; Henderson, S.B.; Murphy, L.E.; Leahy, C.J.; Braithwaite, J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect. 2021, 24, 1015–1024. [Google Scholar] [CrossRef]
- Longo, U.G.; Panattoni, N.; De Salvatore, S.; Marchetti, A.; De Marinis, M.G.; Denaro, V. A qualitative assessment of experiences and perception during pre-admission for rotator cuff repair surgery. BMC Musculoskelet. Disord. 2023, 24, 259. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, F.; Alarabi, A.; Alharthi, M.; Alanazi, T.; Alohali, A.; Alsaleem, M. Use of patient-reported outcome measures (PROMs) by orthopedic surgeons in Saudi Arabia. J. Orthop. Surg. Res. 2020, 15, 598. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Candela, V.; De Salvatore, S.; Piergentili, I.; Panattoni, N.; Casciani, E.; Faldetta, A.; Marchetti, A.; De Marinis, M.G.; Denaro, V. Arthroscopic Rotator Cuff Repair Improves Sleep Disturbance and Quality of Life: A Prospective Study. Int. J. Environ. Res. Public Health 2021, 18, 3797. [Google Scholar] [CrossRef] [PubMed]
- Green, A.; Loyd, K.; Molino, J.; Evangelista, P.; Gallacher, S.; Adkins, J. Long-term functional and structural outcome of rotator cuff repair in patients 60 years old or less. JSES Int. 2023, 7, 58–66. [Google Scholar] [CrossRef]
- Lavoie-Gagne, O.; Huddleston, H.P.; Fu, M.C.; Mehta, N.; Nwachukwu, B.; Forlenza, E.M.; Yanke, A.; Cole, B.J.; Verma, N.N.; Forsythe, B. PROMIS Upper Extremity underperforms psychometrically relative to American Shoulder and Elbow Surgeons score in patients undergoing primary rotator cuff repair. J. Shoulder Elb. Surg. 2022, 31, 718–725. [Google Scholar] [CrossRef]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Gagnier, J.J. Patient reported outcomes in orthopaedics. J. Orthop. Res. 2017, 35, 2098–2108. [Google Scholar] [CrossRef]
- Cho, C.-H.; Seo, H.-J.; Bae, K.-C.; Lee, K.-J.; Hwang, I.; Warner, J.J. The impact of depression and anxiety on self-assessed pain, disability, and quality of life in patients scheduled for rotator cuff repair. J. Shoulder Elb. Surg. 2013, 22, 1160–1166. [Google Scholar] [CrossRef]
- Somerson, J.S.; Hsu, J.E.; Gorbaty, J.D.; Gee, A.O. Classifications in Brief: Goutallier Classification of Fatty Infiltration of the Rotator Cuff Musculature. Clin. Orthop. Relat. Res. 2016, 474, 1328–1332. [Google Scholar] [CrossRef]
- Woollard, J.D.; Bost, J.E.; Piva, S.R.; Kelley Fitzgerald, G.; Rodosky, M.W.; Irrgang, J.J. The ability of preoperative factors to predict patient-reported disability fol-lowing surgery for rotator cuff pathology. Disabil. Rehabil. 2017, 39, 2087–2096. [Google Scholar] [CrossRef]
- Pallant, J.F.; Bailey, C.M. Assessment of the structure of the Hospital Anxiety and Depression Scale in musculoskeletal patients. Heal. Qual. Life Outcomes 2005, 3, 82. [Google Scholar] [CrossRef]
- Cho, C.-H.; Jung, S.-W.; Park, J.-Y.; Song, K.-S.; Yu, K.-I. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J. Shoulder Elb. Surg. 2013, 22, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Traki, L.; Rostom, S.; Tahiri, L.; Bahiri, R.; Harzy, T.; Abouqal, R.; Hajjaj-Hassouni, N. Responsiveness of the EuroQol EQ-5D and Hospital Anxiety and Depression Scale (HADS) in rheumatoid arthritis patients receiving tocilizumab. Clin. Rheumatol. 2014, 33, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Rhee, S.M.; Kim, H.S.; Oh, J.H. Effects of Anxiety and Depression Measured via the Hospital Anxiety and Depres-sion Scale on Early Pain and Range of Motion After Rotator Cuff Repair. Am. J. Sport. Med. 2021, 49, 314–320. [Google Scholar] [CrossRef] [PubMed]

| Time | N | Mean | SD | Minimum | Maximum | p-Value, Friedman Test | |
|---|---|---|---|---|---|---|---|
| HADS | Pre-operative | 43 | 11.7 | 8.7 | 0 | 32 | <0.001 * |
| 1 month | 43 | 9.2 | 7.4 | 0 | 29 | ||
| 3 months | 43 | 6.1 | 6.8 | 0 | 27 | ||
| 6 months | 43 | 5.4 | 6.9 | 0 | 27 | ||
| HADS-A | Pre-operative | 43 | 6.7 | 4.6 | 0 | 16 | <0.001 * |
| 1 month | 43 | 5.4 | 3.8 | 0 | 14 | ||
| 3 months | 43 | 3.6 | 3.4 | 0 | 13 | ||
| 6 months | 43 | 3.2 | 3.5 | 0 | 13 | ||
| HADS-D | Pre-operative | 43 | 5.0 | 4.5 | 0 | 18 | <0.001 * |
| 1 month | 43 | 3.8 | 4.3 | 0 | 17 | ||
| 3 months | 43 | 2.5 | 3.7 | 0 | 16 | ||
| 6 months | 43 | 2.2 | 3.7 | 0 | 16 | ||
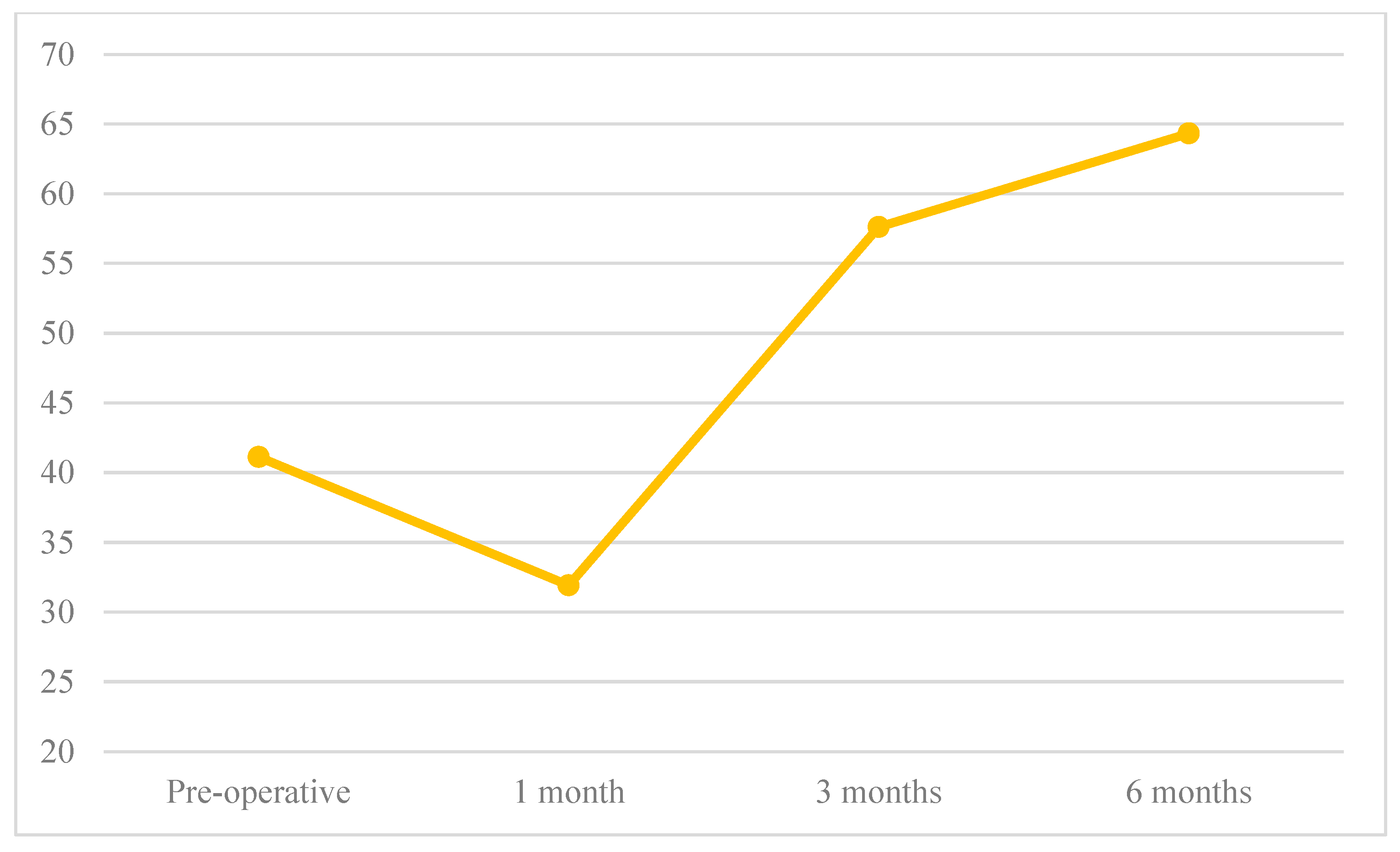
| CONSTANT SCORE | Pre-operative | 43 | 41.1 | 16.7 | 4 | 70 | <0.001 * |
| 1 month | 43 | 31.9 | 10.3 | 9.5 | 60 | ||
| 3 months | 43 | 57.6 | 12.9 | 23.5 | 75 | ||
| 6 months | 43 | 64.3 | 9.9 | 41.5 | 77 | ||
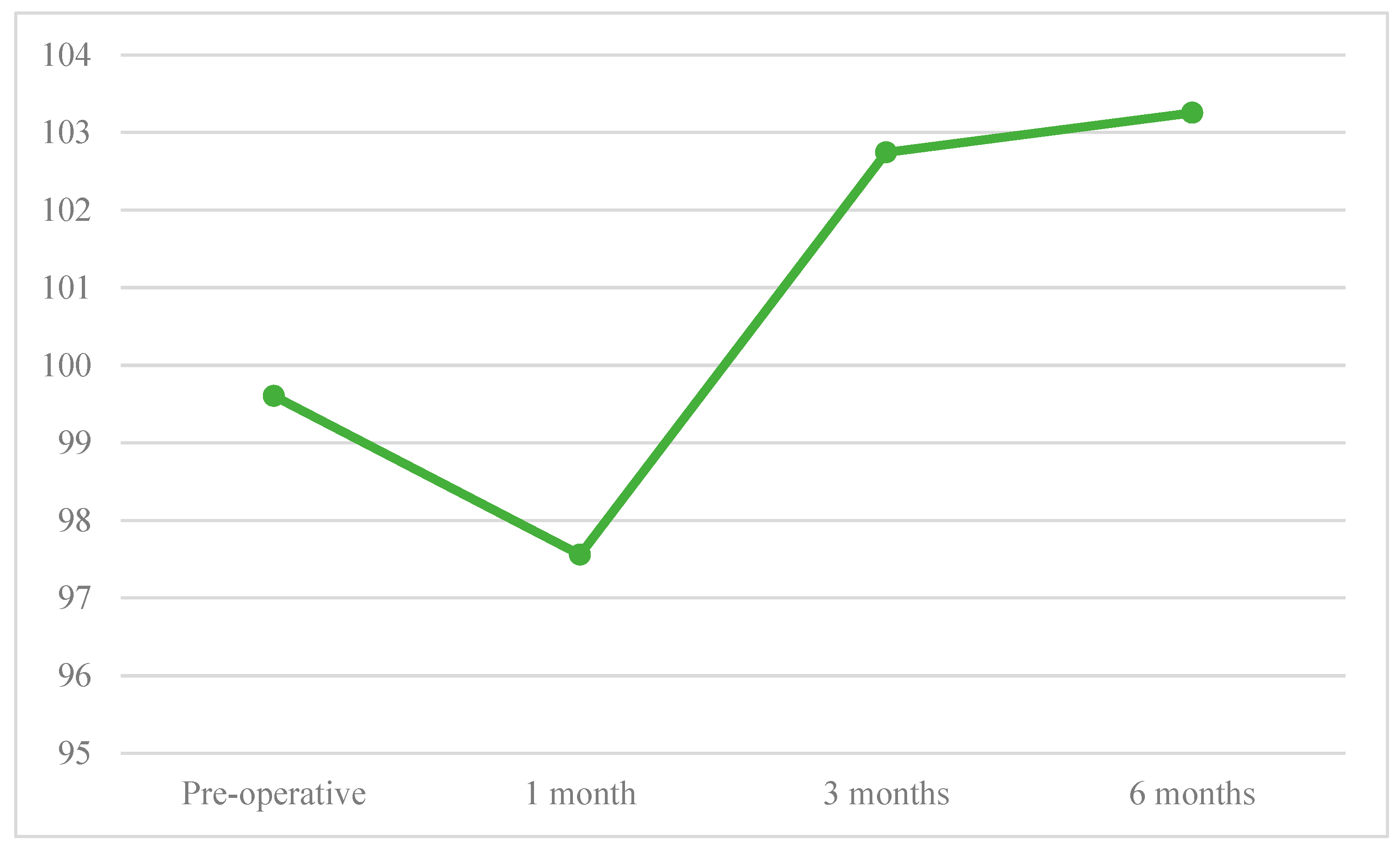
| SF-36 | Pre-operative | 43 | 99.6 | 8.5 | 85 | 116 | <0.001 * |
| 1 month | 43 | 97.6 | 7.7 | 79 | 111 | ||
| 3 months | 43 | 102.7 | 7.5 | 80 | 116 | ||
| 6 months | 43 | 103.3 | 6.9 | 80 | 116 |
| Score | Pre-op vs. 1 Month | Pre-op vs. 3 Months | Pre-op vs. 6 Months | 1 Month vs. 3 Months | 1 Months vs. 6 Months | 3 Months vs. 6 Months |
|---|---|---|---|---|---|---|
| HADS | 0.012 * | <0.001 * | <0.001 * | 0.001 * | <0.001 * | 0.146 |
| HADS-A | 0.040 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | 0.140 |
| HADS-D | 0.021 * | <0.001 * | <0.001 * | 0.006 * | <0.001 * | 0.268 |
| CONSTANT SCORE | 0.004 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| SF-36 | 0.061 | 0.033 * | 0.014 * | <0.001 * | <0.001 * | 0.495 |
| HADS Pre | HADS 1 mo | HADS 3 mo | HADS 6 mo | |||||
|---|---|---|---|---|---|---|---|---|
| rho | Constant score Pre | −0.4 | Constant score 1 mo | −0.2 | Constant score 3 mo | −0.5 | Constant score 6 mo | −0.4 |
| p-value | 0.008 * | 0.152 | 0.002 * | 0.007 * | ||||
| rho | SF-36 Pre | −0.6 | SF-36 1 mo | −0.5 | SF-36 3 mo | −0.4 | SF-36 6 mo | −0.6 |
| p-value | <0.001 * | 0.001 * | 0.008* | <0.001 * | ||||
| HADS-A Pre | HADS-A 1 mo | HADS-A 3 mo | HADS-A 6 mo | |||||
| rho | Constant score Pre | −0.3 | Constant score 1 mo | −0.2 | Constant score 3 mo | −0.4 | Constant score 6 mo | −0.4 |
| p-value | 0.032 * | 0.255 | 0.003 * | 0.016 * | ||||
| rho | SF-36 Pre | −0.5 | −0.5 | SF-36 3 mo | −0.4 | SF-36 6 mo | −0.6 | |
| p-value | <0.001 * | SF-36 1 mo | 0.001 * | 0.006 * | <0.001 * | |||
| HADS-D Pre | HADS-D 1 mo | HADS-D 3 mo | HADS-D 6 mo | |||||
| rho | Constant score Pre | −0.5 | Constant score 1 mo | −0.3 | Constant score 3 mo | −0.5 | Constant score 6 mo | −0.5 |
| p-value | 0.001 * | 0.099 | 0.001 * | 0.002 * | ||||
| rho | SF-36 Pre | −0.6 | SF-36 1 mo | −0.4 | SF-36 3 mo | −0.5 | SF-36 6 mo | −0.5 |
| p-value | <0.001 * | 0.014 * | 0.001 * | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; De Salvatore, S.; Piergentili, I.; Panattoni, N.; Marchetti, A.; De Marinis, M.G.; Denaro, V. Anxiety and Depressive Symptoms Correlated to Patient-Reported Outcome Measures after Rotator Cuff Repair: A Prospective Study in the Perioperative Period. J. Clin. Med. 2023, 12, 2999. https://doi.org/10.3390/jcm12082999
Longo UG, De Salvatore S, Piergentili I, Panattoni N, Marchetti A, De Marinis MG, Denaro V. Anxiety and Depressive Symptoms Correlated to Patient-Reported Outcome Measures after Rotator Cuff Repair: A Prospective Study in the Perioperative Period. Journal of Clinical Medicine. 2023; 12(8):2999. https://doi.org/10.3390/jcm12082999
Chicago/Turabian StyleLongo, Umile Giuseppe, Sergio De Salvatore, Ilaria Piergentili, Nicolò Panattoni, Anna Marchetti, Maria Grazia De Marinis, and Vincenzo Denaro. 2023. "Anxiety and Depressive Symptoms Correlated to Patient-Reported Outcome Measures after Rotator Cuff Repair: A Prospective Study in the Perioperative Period" Journal of Clinical Medicine 12, no. 8: 2999. https://doi.org/10.3390/jcm12082999
APA StyleLongo, U. G., De Salvatore, S., Piergentili, I., Panattoni, N., Marchetti, A., De Marinis, M. G., & Denaro, V. (2023). Anxiety and Depressive Symptoms Correlated to Patient-Reported Outcome Measures after Rotator Cuff Repair: A Prospective Study in the Perioperative Period. Journal of Clinical Medicine, 12(8), 2999. https://doi.org/10.3390/jcm12082999









